Abstract
Purpose of the review
Scapholunate and perilunate injuries can be difficult to diagnose and treat in the athlete. In this review article, we present the mechanism of injury, evaluation, management, and outcomes of treatment for these injuries.
Recent findings
Acute repair of dynamic scapholunate ligament injuries remains the gold standard, but judicious use of a wrist splint can be considered for the elite athlete who is in season. The treatment of static scapholunate ligament injury remains controversial. Newer SL reconstructive techniques that aim to restore scapholunate function without compromising wrist mobility as much as tenodesis procedures show promise in athlete patients.
Summary
Acute injuries to the scapholunate ligament are best treated aggressively in order to prevent the sequelae of wrist arthritis associated with long-standing ligamentous injury. Acute repair is favored. Reconstructive surgical procedures to manage chronic scapholunate injury remain inferior to acute repair. The treatment of lunotriquetral ligament injuries is not well defined.
Keywords: Scapholunate ligament, Lunotriquetral ligament, Wrist instability, Wrist sprain, Athletic injury, DISI
Introduction
The scaphoid, lunate, and triquetrum constitute the proximal carpal row of the wrist, commonly referred to as the intercalary segment. These three bones are linked via the scapholunate (SL) and lunotriquetral (LT) interosseous ligaments, respectively. The lunate is held in balance between a flexion-moment provided by the scaphoid and an extension moment provided by the triquetrum [1]. Both the SL and LT ligaments have three main components: dorsal, proximal (or membranous), and volar segments. Biomechanical studies have shown that the dorsal aspect of the SL ligament and the volar aspect of the LT ligament are the primary functional components of these interosseous ligaments [2, 3]. These ligaments do not function in isolation. There is an extensive extrinsic ligamentous complex that consists of volar and dorsal radiocarpal and ulnocarpal ligaments that provides additional stability to the proximal row. Injuries to the wrist vary in severity by the degree and number of stabilizing ligaments disrupted [4, 5].
The mechanism responsible for most scapholunate and perilunate injuries is wrist extension, ulnar deviation, and carpal supination [6]. Mayfield described a progression of perilunate instability, traveling from radial to ulnar around the lunate: stage I involves disruption of the scapholunate articulation, stage II adds lunocapitate disruption, stage III adds lunotriquetral disruption, and finally, stage IV involves dislocation of the lunate from the radius [6] (Fig. 1). Conversely, wrist extension, radial deviation, and intercarpal pronation create a reverse-progression of intercarpal disruption, starting with lunotriquetral disruption and working from ulnar to radial [7]. A three stage progression has been described [7] (Fig. 2). As such, isolated scapholunate and lunotriquetral ligament injuries are within the greater perilunate spectrum.
Fig. 1.
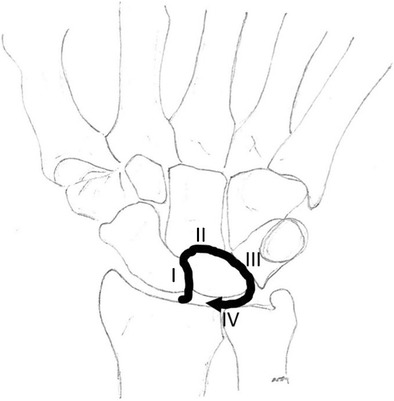
The Mayfield classification of perilunate injury. The initial injury is initiated with extension and ulnar deviation of the carpus and portends a circle around the lunate. In stage I, the scapholunate ligament is torn. Stage 2, the dorsal capsule is disrupted at the midcarpal joint. Stage 3, the lunotriquetral ligament is torn. Stage 4, the lunate is dislocated out of the proximal row in a volar direction, flipped 180 degrees, tethered by the long and short radiolunate ligaments. Adapted with permission from Mayfield JK, Johnson RP, Kilcoyne RK. Carpal dislocations: pathomechanics and progressive perilunar instability. J Hand Surg Am. 1980;5(3):226-41
Fig. 2.
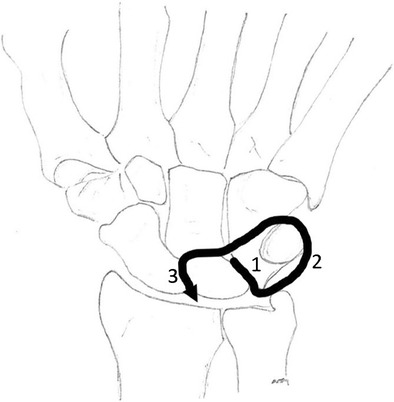
Reverse perilunate injury. Another proposed mechanism for perilunate injury where the carpus is placed into forced extension, radial deviation, and pronation. Stage 1: the lunotriquetral ligament is torn. Stage 2: the dorsal ulnar midcarpal capsule is torn. Stage 3: the scapholunate ligament is torn. Adapted with permission from Murray PM, Palmer CG, Shin AY. The mechanism of ulnar-sided perilunate instability of the wrist: a cadaveric study and six clinical cases. J Hand Surg Am. 2012;37(4):721-8. doi:10.1016/j.jhsa.2012.01.015
Forceful wrist extension is a common mechanism for a variety of other wrist injuries, including distal radius and scaphoid fractures, which are much more common than scapholunate or perilunate ligamentous injuries [8]. While intercarpal ligamentous injuries may occur in concert with bony injuries at the wrist [9], a detailed discussion of these concordant injuries is beyond the scope of this review. The treating physician must consider these more common diagnoses in the injured athlete.
Diagnosis
Scapholunate injuries, and other perilunate injuries, are likely under-appreciated injuries, commonly dismissed as simple “sprains,” especially in athletes [10]. Delays in appropriate treatment can significantly affect outcome as treatment of acute scapholunate and perilunate injuries have better results than treatment for chronic injuries [11, 12]. As such, prompt and accurate diagnosis is paramount.
Higher stage perilunate injuries occur most frequently from high-energy trauma [13]. Lower stage injuries, such as isolated scapholunate or lunotriquetral ligament tears, are more likely to occur in an athlete who collides with another athlete or the ground [11]. Accurate diagnosis of scapholunate and lunotriquetral injuries can be challenging in the acute setting. Localized pain over the scapholunate or lunotriquetral intervals, or instability on examination, which may include a positive Watson’s shift, laxity on lunotriquetral shuck, or a positive Kleinman’s shear test, should alert the physician to consider injury to the SL or LT ligaments and initiate additional diagnostic testing [14, 15]. A high index of suspicion is essential so as not to delay the initiation of appropriate treatment.
Investigation includes plain radiographs with a neutral posterior-anterior (PA) and lateral view. SL interval widening >3 mm on the PA view, or a scapholunate angle >70° on the lateral, is concerning for a SL ligament injury [11]. A 20° tangential PA view as described by Moneim is also recommended as it allows direct viewing of the SL interval and does not require painful contraction or positioning by the patient [16]. Multiple stress views have been proposed including: PA clenched fist-neutral, PA clenched fist-radial deviation, PA clenched fist-ulnar deviation, PA finger traction-pronation, PA thumb traction, anteroposterior (AP) clenched fist-neutral, AP clenched fist-radial deviation, PA clenched pencil, and AP clenched fist-ulnar deviation (UD) [5]. As obtaining these stress views can cause pain for the patient and patient effort is required, caution must be used when evaluating these studies. In a cadaveric model, the PA clenched pencil view, which allows viewing of both wrists simultaneously, was the most reproducible and consistently showed the widest SL gaps [5]. Contralateral wrist comparison radiographs are strongly recommended as some SL widening may be physiologic rather than pathologic.
Scapholunate ligament injuries are further classified as “pre-dynamic,” “dynamic,” or “static” based on imaging. Pre-dynamic instability occurs when no abnormalities can be determined on standard radiographs though a ligament tear is found using advanced imaging or at the time of surgery. Dynamic instability is noted when normal measurements are found on neutral, non-stress radiographs, but pathologic widening is seen on stress views. Static instability is noted when a widened scapholunate interval and a dorsiflexion intercalated segment instability (DISI) pattern are observed on neutral, non-stress radiographs. Static scapholunate dissociation correlates with a more involved injury to the secondary stabilizing extrinsic ligaments, in addition to the SL ligament itself [4, 5].
Advanced imaging may be used to evaluate for scapholunate or perilunate injuries. A wide range of modalities has been described, from computed tomography (CT) to magnetic resonance imaging (MRI), MR-arthrogram (MRA) to cine-MRI, cine-fluoroscopy to 4D-CT [17–19]. MRI and MR-arthrograms are most commonly performed. As with radiographs, traction during imaging may facilitate recognition of pathology. Compared to conventional MRA, traction MRA demonstrates improved sensitivity, specificity, and accuracy when evaluating for full-thickness tears of the SL and LT ligaments [20].
While advanced imaging may be helpful, diagnostic arthroscopy remains the gold standard to diagnose intercarpal ligament tears [21]. In 1996, Geissler et al. proposed an arthroscopic staging system for SL injuries that has been widely applied, including to LT injuries [9]. Stage I involves attenuation of the ligament as seen from the radiocarpal joint, without malalignment in the midcarpal joint; stage II involves incongruence as seen in the midcarpal joint though a probe may not be passed between the respective bones; stage III involves increased incongruence such that a probe may be passed between the respective bones; and stage IV involves gross instability and incongruence such that a 2.7 mm arthroscope may be “driven” between the respective carpal bones [9] (Table 1).
Table 1.
The Geissler classification of interacarpal ligament injury
| Arthroscopic classification of the tears of the intracarpal ligaments | |
|---|---|
| Grade | Description |
| I | Attenuation or hemorrhage of the interosseous ligament as seen from the radiocarpal space. No incongruency of carpal alignment in the midcarpal space. |
| II | Attenuation or hemorrhage of interosseous ligament as seen from the radiocarpal space. Incongruency or step-off of midcarpal space. There may be slight gap (less than width of probe) between carpal bones. |
| III | Incongruency or step-off of carpal alignment as seen from both radiocarpal and midcarpal space. Probe may be passed through gap between carpal bones. |
| IV | Incongruency or step-off of carpal alignment as seen from both radiocarpal and midcarpal spaces. There is gross instability with manipulation. A 2.7-mm arthroscope may be passed through the gap between carpal bones. |
This classification system depicts injury severity based upon arthroscopic findings. Grade 1 injuries are the least severe while grade 4 injuries have the highest level of damage. Reprinted with permission from Geissler WB, Freeland AE, Savoie FH, McIntyre LW, Whipple TL. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg Am. 1996;78(3):357-65
Uniqueness of athletes
Caring for athletes often presents a unique set of circumstances surrounding injury evaluation and treatment. These factors include personal demands and coaching expectations such that many physicians consider caring for athletes different from managing others in the general population [22]. One must not only consider the actual injury, but the athlete as a whole [10]. Scapholunate and perilunate injuries in the athlete require an important risk-benefit discussion between the athlete and the treating physician. One must understand that there may be incredible pressure from parents, coaches, teammates, agents, and/or trainers, but ultimately, the treating physician must do what is in the athlete’s best interest, while maintaining sound ethical principles. A recent survey of consultant hand surgeons managing professional athletes showed that there was significant variability in the management of hand and wrist injuries, a finding that demonstrates that treatments are very specifically individualized [22]. The management of these injuries in athletes depends on the age of the athlete, the sport, the position the athlete plays, and the timing in regard to the current season as well as future seasons [23].
The goal of treatment of scapholunate and perilunate injuries, from the surgeon’s perspective, is restoration of a stable and functional wrist with minimal morbidity. The goal of treatment from the athlete’s perspective may be different; it may simply be an expedited return to competition. The recovery of mobility, strength, and dexterity specific to the individual needs must be acknowledged in order to get the athlete back into competition as quickly as possible [24]. Both overtreatment (such as excessive dissection during surgery or unnecessarily prolonged immobilization) and under treatment (such as inadequate fixation or insufficient immobilization) can have devastating consequences and can result in season-ending or even career-ending outcomes [10].
Treatment options
Non-operative management
Non-operative treatment is primarily reserved for stable, partial SL ligament tears, and perilunate injuries. A period of immobilization for 4 to 6 weeks is curative in most patients [23]. Elite athletes may also benefit from their increased access to therapy as these athletes are often under close supervision of athletic trainers and physical therapy staff, whereas non-athletes may not have this benefit. Additionally, judicious use of a wrist splint or cast can be considered for the elite athlete that is in season, if their particular position allows.
Anderson and Hoy reported on a series of five patients with at least partial SL ligament tearing treated with an orthotic and rehabilitation program [25]. A custom splint was worn for a minimum 6 weeks limiting the patient to mid-range dart-throwers motion. Dart-throwers motion is defined as the arc traveling from radial deviation with extension to ulnar deviation with flexion. It had been shown to place very little stress on the SL ligament and therefore allows earlier motion to improve function of secondary wrist stabilizers [24, 25]. Rehabilitation afterward consisted of strengthening and proprioceptive exercises. Although the study was limited by a lack of baseline data and consistent implementation, patients reported improved pain and function at median 4-year follow-up [25].
Operative management
With a goal of returning to full activity and function, surgical treatment is a mainstay of SL ligament and perilunate injury treatment in the athlete [11]. Surgical indications vary based on the severity of the instability, the chronicity of the injury, and the presence of degenerative changes (Table 2). Salvage procedures (partial wrist fusions) are used to manage the sequelae of chronic scapholunate and perilunate injuries. Because such operations are likely to end an athlete’s career, however, they are not further discussed in this manuscript.
Table 2.
Treatment algorithm for scapholunate ligament injury
| Scapholunate interosseous ligament injury | |
|---|---|
| Injury pattern | Treatment strategy |
| Predynamic or occult instability (partial scapholunate ligament tear) | Immobilization Arthroscopic debridement/pinning |
| Acute complete injury with reparable scapholunate ligament | Primary soft tissue repair with or without capsulodesis |
| Complete injury with irreparable ligament and reducible scaphoid subluxation | Capsulodesis Reconstruction (tendon weaves, BRB reconstruction, and RASL) Tenodesis (Brunelli or modifications) SLAM |
| Complete injury with irreducible scaphoid subluxation and DISI | Capsular release and reconstruction Salvage (proximal row carpectomy, limited wrist fusion) |
| Scapholunate advanced collapse | Arthroscopic debridement Neurectomy Salvage (proximal row carpectomy, limited wrist fusion) |
The severity and injury type in the left column is shown with increasing severity from top to bottom. A proposed treatment for the injury diagnosed is listed in the right column. Adapted with permission from Paci GM, Yao J. Surgical techniques for the treatment of carpal ligament injury in the athlete. Clin Sports Med. 2015;34(1):11-35. doi:10.1016/j.csm.2014.09.010
In pre-dynamic injuries, in which partial ligament injuries are typical, arthroscopic treatment is indicated when immobilization is unsuccessful. In general, arthroscopic debridement is performed in concert with other techniques such as thermal shrinkage and k-wire fixation. Lee et al. demonstrated significant improvement in pain and grip strength in patients with Geissler stage I and II SL injuries after arthroscopic debridement and thermal shrinkage at mean follow-up of 52.8 months [26]. A recent study by Pirolo et al. found that electrothermal treatment of SL and LT ligament tears eliminated neuronal tissue within the ligament, suggesting that the improvement in pain is via a denervation effect [27].
In dynamic and reducible static injuries, treatment depends on the time passed from the trauma because the interosseous ligaments degenerate over time and are difficult to repair once chronic tears have developed [11, 12]. Rohman et al. compared outcomes of treatment for SL instability before and after 6 weeks from injury and found an increased failure rate and worse radiographic outcomes in patients treated after 6 weeks from the initial injury [12]. For the elite athlete, when treatment is considerably delayed, the treatment options are generally unfavorable. Therefore, direct repair of an acute injury offers the best conditions for a successful outcome. The importance of early surgery, preferably within 3 weeks from injury, cannot be over-emphasized [24]. In acute dynamic and reducible static injuries, the ligament can be repaired and a dorsal capsulodesis can be added to enhance the repair. Melone et al. demonstrated an average Mayo wrist score of 85 and full return to play in 100% of professional basketball players followed for more than 5 years who were treated in this manner [24].
For patients with chronic injures, ligament reconstruction is generally superior to repair [12]. While reconstruction can favorably alter the deteriorating pattern of carpal instability, it remains limited in its capacity to restore sufficient function for the athlete as stability is achieved at the expense of mobility [24]. There are many described methods of ligament reconstruction, including tenodesis [28, 29], free tendon graft [30], bone-retinaculum-bone (BRB) [31, 32], reduction and association of the scaphoid and lunate ligament (RASL) [33, 34], and the scapholunate axis method (SLAM) [35]. As with acute repair, dorsal capsulodesis may be performed in conjunction with any of these procedures [36].
In 1995, Brunelli and Brunelli presented a technique for the treatment of SL tears in which a slip of the flexor carpi radialis (FCR) tendon was transferred from volar-to-dorsal in a scaphoid tunnel and secured to the dorsal aspect of the lunate and the distal radius [28]. There have been many recent modifications to this technique. One such modification, commonly referred to as a “three-ligament tenodesis” or “modified Brunelli,” has been popularized by Garcia-Elias et al. [29]. Pauchard et al. found that patients with static instability who underwent the “three-ligament tenodesis” procedure had a statistically significant improvement in pain, grip strength, and wrist function at 2-year follow-up, despite no difference in pre- versus post-operative radiographs, although they also had a significant complication rate and progression of arthritis; as such, they argued that the use of this procedure may need to be re-evaluated. Williams et al. reported that 79% of professional athletes (mostly rugby players) were able to return to play within 4 months after undergoing modified Brunelli SL reconstruction, though ultimately only 64% were able to return to their previous level of competition [37].
Elsaftawy et al. proposed a technique for SL reconstruction in which a free tendon graft is routed through parallel tunnels in the scaphoid and lunate and secured back onto itself at the proximal pole of the scaphoid to recreate the anatomic relationship between the scaphoid and lunate, without involving the dorsal extrinsic ligaments [30]. They also described a modification to the Brunelli technique using a similar course for the FCR tendon. In a cadaveric study, they found improved anatomic alignment and rotatory stability of the scaphoid, without the loss of motion typical of other tenodesis techniques, and thus concluded that their techniques could be options in the future for dynamic and static SLIL instability [30]. Such a technique is appealing in the athlete where preservation of wrist motion may be critical.
As no reconstructive technique to date has proven to provide optimal results, some have directed efforts toward replacement of the dorsal aspect of the SL ligament, the most structurally and functionally important aspect of the ligament [31, 38]. Based on the use of bone-patellar tendon-bone autograft for anterior cruciate ligament reconstruction of the knee, Weiss described the use of bone-retinaculum-bone (BRB) autograft for the treatment of SLIL injuries [32]. Soong et al. published long-term outcomes of patients who underwent BRB reconstruction for dynamic SL instability and found that results were comparable to those of other SL ligament reconstruction procedures [39]. A variety of bone-tissue-bone (BTB) autografts have been proposed, although the exact indication for composite tissue replacement remains to be determined [38].
Based on observations that patients with pseudoarthrosis associated with failed scapholunate arthrodesis tend to do better than those who achieve fusion, reduction, and association of the scaphoid and lunate (RASL) was developed as a procedure that utilizes a Herbert screw to create a fibrous union between the scaphoid and lunate [33]; it can be performed with or without concomitant SL ligament repair [33, 34, 40]. While outcomes have been favorable, the procedure typically requires screw removal at a later date because the screw often loosens [40]. The scapholunate intercarpal (SLIC) screw (Acumed, Hillsboro, OR) has been developed to address issues with the rigid Herbert screw; this screw allows an “anatomic toggle” of 15–22°, allowing the scaphoid and lunate to move anatomically while the soft tissue heals [23]. Geissler and Burkett report a return to play at 1–2 weeks post-op when the SLIC screw is used [23].
The scapholunate axis method (SLAM) is another technique that is used to reconstruct the SL ligament in patients with dynamic or reducible static SL instability [35]. Yao et al. reported an improvement in radiographic SL gap and angle, grip strength, and pain scores in patients undergoing the SLAM procedure [35]. They believe the SLAM technique is superior to other reconstructive options because no other method has been proven to restore scaphoid extension, decrease the SL gap, and correct scaphoid pronation using a multi-planar biologic tether; in addition, there is no need for screw removal and the graft is less rigid than with a metal screw [35].
Similar to the SLAM, Ross et al. proposed a new ligament reconstruction technique in which a portion of the FCR tendon is rerouted through a transosseous tunnel across the scaphoid, lunate, and triquetrum [41]. This technique is different from the SLAM in that it can also be used for lunotriquetral ligament injuries. Having used the technique in more the 40 patients since 2009, Ross et al. reported improved quickDASH and PRWE scores, grip strength, pain, similar ROM, and a maintained SL interval on radiographs [41]. They compared their outcomes to other ligament reconstructions and determined that their clinical and radiographic outcomes were similar, if not superior. Therefore, they concluded that the technique is effective but expressed caution because of the small number of patients studied and complexity of the procedure [41].
Treatment of LT injuries
Isolated LT ligament injury is not as common or as well described as SL injuries. Patients with non-dissociative LT injuries rarely present for treatment, unless they have continued intermittent ulnar-sided wrist pain. Interestingly, patients with acute LT injuries tend to present after more significant, traumatic perilunate injuries [42]. The grading and treatment of LT injuries have been extrapolated from the SL literature (Table 3). Similar to SL injuries, the Geissler grading system is utilized for classification [9]. Recent review articles highlight the limited amount of research available [11, 42, 43]. In general, LT injuries are treated non-operatively with immobilization for 4–6 weeks and may be supplemented with intra-articular steroid injections or NSAIDS [42]. The success of non-operative management has rarely been described, and there are no current studies comparing operative versus non-operative management of this type of injury.
Table 3.
Treatment algorithm for lunotriquetral ligament injury
| Lunotriquetral interosseous ligament injury | |
|---|---|
| Injury pattern | Treatment strategy |
| Predynamic or occult instability (partial LTIL injury) | Immobilization Arthroscopic debridement ± pinning |
| Acute complete injury with reparable LTIL | Primary soft tissue repair with or without capsulodesis |
| Complete injury with irreparable ligament or VISI | Capsulodesis Reconstruction with tenodesis Lunotriquetral arthrodesis Ulnar shortening osteotomy |
| Ulnocarpal impaction syndrome | Ulnar shortening osteotomy |
The severity and injury type in the left column is shown with increasing severity from top to bottom. A proposed treatment for the injury diagnosed is listed in the column to the right. Adapted with permission from Paci GM, Yao J. Surgical techniques for the treatment of carpal ligament injury in the athlete. Clin Sports Med. 2015;34(1):11-35. doi:10.1016/j.csm.2014.09.010
In high-demand athletes, surgical management may be beneficial to return them to their previous level of play [11]. If the athlete has a partial LT injury, arthroscopic debridement may be considered, with or without electrothermal treatment. Reported outcomes are overall encouraging, with good to excellent pain relief in 20–100% and post-operative grip strength of 67–97% compared to the non-injured side [42, 43]. When the athlete has a complete LT ligament tear, acute repair or reconstruction, with or without capsulodesis, may be performed. High level of evidence studies are lacking, though reports have quoted the outcomes with range of motion from 62–100% of normal, grip strength 67–100% of normal, and patients with good to excellent results in 50–87% of cases [11]. Studies based on repair alone demonstrated a 77% reoperation rate whereas reconstruction had a 31% reoperation rate at 5 years [11].
Chronic LT tears can occur from ulnar positive variance. A recent study by Mirza et al. examined ulnar shortening osteotomies (USO) for isolated LTIL injuries that have failed non-operative management [44]. They postulated that USO may decrease ulnar-sided wrist pain with fewer complications compared to other treatments by tightening the triangular fibrocartilage complex (TFCC) and extrinsic ligaments [44]. They retrospectively examined 53 cases with a minimum follow-up of 1 year and determined that 83% had good to excellent outcomes on Gartland Werley score, grip strength increased 41% of the preoperative value, and all patients had clinical and radiographic union by 10 months [44]. The authors concluded that USO may be an effective primary treatment in addressing traumatic LTIL tears, but further studies are needed.
Arthrodesis of the LT joint is another procedure advocated to treat patients with resistant LT instability because patients with congenital LT coalition generally have normal grip strength and ROM [11, 42]. LT fusion has been found to have a range of motion 59–85% of normal, grip strength 59–93% of normal, and patient-reported satisfaction 0 to 93% with 27 to 59% of patients still reporting pain [11, 42, 43].
Best practices and treatments for LT instability are not known. Paci and Yao concluded that 4 weeks of immobilization should be attempted in athletes for acute or chronic LTIL injuries. If this fails, early intervention with repair should follow as unpredictable outcomes exist with reconstructive procedures [11]. Overall, these injuries continue to be difficult to manage for the treating hand surgeon as there is very little evidence upon which treatments are based.
Conclusions
It is prudent to diagnose scapholunate and perilunate injuries expeditiously in athletes as treatment of chronic tears is less predictable than earlier treatments that often result in better outcomes. Treatment must be tailored to the individual athlete which includes a discussion of injury severity and goals of treatment. In athletes, acute repair or reconstruction of the injured ligament is preferred, as salvage procedures will likely lead to the end of their athletic career [11]. Techniques such as a free-tendon graft, BTB replacement, RASL with a SLIC screw, and SLAM may be more favorable in athletes; in theory, these techniques work to restore normal intercarpal ligament function, without compromising mobility as much as tenodesis reconstructions. While numerous techniques are available, none has proven superior, therefore, additional studies are needed to elucidate the ideal treatment for athletes.
Compliance with ethical standards
Conflict of interest
All of the authors declare that they have no conflict of interest.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Hand and Wrist Sports Medicine
References
- 1.Garcia-Elias M, Cooney WP. Kinematics of the radiocarpal joint. In: Cooney WP, Linscheid RL, Dobyns JH, editors. The wrist: diagnosis and operative treatment. St. Louis: Mosby; 1998. pp. 205–18. [Google Scholar]
- 2.Berger RA, Imeada T, Berglund L, An KN. Constraint and material properties of the subregions of the scapholunate interosseous ligament. J Hand Surg [Am] 1999;24(5):953–62. doi: 10.1053/jhsu.1999.0953. [DOI] [PubMed] [Google Scholar]
- 3.Ritt MJ, Bishop AT, Berger RA, Linscheid RL, Berglund LJ, An KN. Lunotriquetral ligament properties: a comparison of three anatomic subregions. J Hand Surg [Am] 1998;23(3):425–31. doi: 10.1016/S0363-5023(05)80460-5. [DOI] [PubMed] [Google Scholar]
- 4.Van Overstraeten L, Camus EJ. The role of extrinsic ligaments in maintaining carpal stability—a prospective statistical analysis of 85 arthroscopic cases. Hand Surg Rehabil. 2016;35(1):10–5. doi: 10.1016/j.hansur.2015.09.004. [DOI] [PubMed] [Google Scholar]
- 5.Lee SK, Desai H, Silver B, Dhaliwal G, Paksima N. Comparison of radiographic stress views for scapholunate dynamic instability in a cadaver model. J Hand Surg [Am] 2011;36(7):1149–57. doi: 10.1016/j.jhsa.2011.05.009. [DOI] [PubMed] [Google Scholar]
- 6.Mayfield JK, Johnson RP, Kilcoyne RK. Carpal dislocations: pathomechanics and progressive perilunar instability. J Hand Surg [Am] 1980;5(3):226–41. doi: 10.1016/S0363-5023(80)80007-4. [DOI] [PubMed] [Google Scholar]
- 7.Murray PM, Palmer CG, Shin AY. The mechanism of ulnar-sided perilunate instability of the wrist: a cadaveric study and 6 clinical cases. J Hand Surg [Am] 2012;37(4):721–8. doi: 10.1016/j.jhsa.2012.01.015. [DOI] [PubMed] [Google Scholar]
- 8.Karl JW, Olson PR, Rosenwasser MP. The epidemiology of upper extremity fractures in the United States, 2009. J Orthop Trauma. 2015;29(8):e242–4. doi: 10.1097/BOT.0000000000000312. [DOI] [PubMed] [Google Scholar]
- 9.Geissler WB, Freeland AE, Savoie FH, McIntyre LW, Whipple TL. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg Am. 1996;78(3):357–65. doi: 10.2106/00004623-199603000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Gaston RG, Loeffler BJ. Sports-specific injuries of the hand and wrist. Clin Sports Med. 2015;34(1):1–10. doi: 10.1016/j.csm.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 11.Paci GM, Yao J. Surgical techniques for the treatment of carpal ligament injury in the athlete. Clin Sports Med. 2015;34(1):11–35. doi: 10.1016/j.csm.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 12.Rohman EM, Agel J, Putnam MD, Adams JE. Scapholunate interosseous ligament injuries: a retrospective review of treatment and outcomes in 82 wrists. J Hand Surg [Am] 2014;39(10):2020–6. doi: 10.1016/j.jhsa.2014.06.139. [DOI] [PubMed] [Google Scholar]
- 13.Krief E, Appy-Fedida B, Rotari V, David E, Mertl P, Maes-Clavier C. Results of perilunate dislocations and perilunate fracture dislocations with a minimum 15-year follow-up. J Hand Surg [Am] 2015;40(11):2191–7. doi: 10.1016/j.jhsa.2015.07.016. [DOI] [PubMed] [Google Scholar]
- 14.Watson HK, Ashmead D, Makhlouf MV. Examination of the scaphoid. J Hand Surg [Am] 1988;13(5):657–60. doi: 10.1016/S0363-5023(88)80118-7. [DOI] [PubMed] [Google Scholar]
- 15.Kleinman WB. Physical examination of the wrist: useful provocative maneuvers. J Hand Surg [Am] 2015;40(7):1486–500. doi: 10.1016/j.jhsa.2015.01.016. [DOI] [PubMed] [Google Scholar]
- 16.Moneim MS. The tangential posteroanterior radiograph to demonstrate scapholunate dissociation. J Bone Joint Surg Am. 1981;63(8):1324–6. doi: 10.2106/00004623-198163080-00016. [DOI] [PubMed] [Google Scholar]
- 17.Langner I, Fischer S, Eisenschenk A, Langner S. Cine MRI: a new approach to the diagnosis of scapholunate dissociation. Skeletal Radiol. 2015;44(8):1103–10. doi: 10.1007/s00256-015-2126-4. [DOI] [PubMed] [Google Scholar]
- 18.Demehri S, Hafezi-Nejad N, Morelli JN, Thakur U, Lifchez SD, Means KR, et al. Scapholunate kinematics of asymptomatic wrists in comparison with symptomatic contralateral wrists using four-dimensional CT examinations: initial clinical experience. Skeletal Radiol. 2016;45(4):437–46. doi: 10.1007/s00256-015-2308-0. [DOI] [PubMed] [Google Scholar]
- 19.Sulkers GS, Schep NW, Maas M, Strackee SD. Intraobserver and interobserver variability in diagnosing scapholunate dissociation by cineradiography. J Hand Surg [Am] 2014;39(6):1050–4. doi: 10.1016/j.jhsa.2014.03.014. [DOI] [PubMed] [Google Scholar]
- 20.Lee RK, Griffith JF, Ng AW, Nung RC, Yeung DK. Wrist traction during MR arthrography improves detection of triangular fibrocartilage complex and intrinsic ligament tears and visibility of articular cartilage. AJR Am J Roentgenol. 2016;206(1):155–61. doi: 10.2214/AJR.15.14948. [DOI] [PubMed] [Google Scholar]
- 21.Andersson JK, Andernord D, Karlsson J, Friden J. Efficacy of magnetic resonance imaging and clinical tests in diagnostics of wrist ligament injuries: a systematic review. Arthroscopy. 2015;31(10):2014–20. doi: 10.1016/j.arthro.2015.04.090. [DOI] [PubMed] [Google Scholar]
- 22.Dy CJ, Khmelnitskaya E, Hearns KA, Carlson MG. Opinions regarding the management of hand and wrist injuries in elite athletes. Orthopedics. 2013;36(6):815–9. doi: 10.3928/01477447-20130523-30. [DOI] [PubMed] [Google Scholar]
- 23.Geissler WB, Burkett JL. Ligamentous sports injuries of the hand and wrist. Sports Med Arthrosc. 2014;22(1):39–44. doi: 10.1097/JSA.0000000000000013. [DOI] [PubMed] [Google Scholar]
- 24.Melone CP, Jr, Polatsch DB, Flink G, Horak B, Beldner S. Scapholunate interosseous ligament disruption in professional basketball players: treatment by direct repair and dorsal ligamentoplasty. Hand Clin. 2012;28(3):253–60. doi: 10.1016/j.hcl.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 25.Anderson H, Hoy G. Orthotic intervention incorporating the dart-thrower’s motion as part of conservative management guidelines for treatment of scapholunate injury. J Hand Ther. 2016;29(2):199–204. doi: 10.1016/j.jht.2016.02.007. [DOI] [PubMed] [Google Scholar]
- 26.Lee JI, Nha KW, Lee GY, Kim BH, Kim JW, Park JW. Long-term outcomes of arthroscopic debridement and thermal shrinkage for isolated partial intercarpal ligament tears. Orthopedics. 2012;35(8):e1204–9. doi: 10.3928/01477447-20120725-20. [DOI] [PubMed] [Google Scholar]
- 27.Pirolo JM, Le W, Yao J. Effect of electrothermal treatment on nerve tissue within the triangular fibrocartilage complex, scapholunate, and lunotriquetral interosseous ligaments. Arthroscopy. 2016;32(5):773–8. doi: 10.1016/j.arthro.2015.11.050. [DOI] [PubMed] [Google Scholar]
- 28.Brunelli GA, Brunelli GR. A new technique to correct carpal instability with scaphoid rotary subluxation: a preliminary report. J Hand Surg [Am] 1995;20(3 Pt 2):S82–5. doi: 10.1016/S0363-5023(95)80175-8. [DOI] [PubMed] [Google Scholar]
- 29.Garcia-Elias M, Lluch AL, Stanley JK. Three-ligament tenodesis for the treatment of scapholunate dissociation: indications and surgical technique. J Hand Surg [Am] 2006;31(1):125–34. doi: 10.1016/j.jhsa.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 30.Elsaftawy A, Jablecki J, Jurek T, Domanasiewicz A, Gworys B. New concept of scapholunate dissociation treatment and novel modification of Brunelli procedure - anatomical study. BMC Musculoskelet Disord. 2014;15:172. doi: 10.1186/1471-2474-15-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Morrell NT, Weiss AP. Bone-retinaculum-bone autografts for scapholunate interosseous ligament reconstruction. Hand Clin. 2015;31(3):451–6. doi: 10.1016/j.hcl.2015.04.012. [DOI] [PubMed] [Google Scholar]
- 32.Weiss AP. Scapholunate ligament reconstruction using a bone-retinaculum-bone autograft. J Hand Surg [Am] 1998;23(2):205–15. doi: 10.1016/S0363-5023(98)80115-9. [DOI] [PubMed] [Google Scholar]
- 33.Filan SL, Herbert TJ. Herbert screw fixation for the treatment of scapholunate ligament rupture. Hand Surg. 1998;3:47–55. doi: 10.1142/S0218810498000088. [DOI] [Google Scholar]
- 34.Rosenwasser MP, Miyasajsa KC, Strauch RJ. The RASL procedure: reduction and association of the scaphoid and lunate using the Herbert screw. Tech Hand Up Extrem Surg. 1997;1(4):263–72. doi: 10.1097/00130911-199712000-00007. [DOI] [PubMed] [Google Scholar]
- 35.Yao J, Zlotolow DA, Lee SK. ScaphoLunate axis method. J Wrist Surg. 2016;5(1):59–66. doi: 10.1055/s-0035-1570744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Moran SL, Ford KS, Wulf CA, Cooney WP. Outcomes of dorsal capsulodesis and tenodesis for treatment of scapholunate instability. J Hand Surg [Am] 2006;31(9):1438–46. doi: 10.1016/j.jhsa.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 37.Williams A, Ng CY, Hayton MJ. When can a professional athlete return to play following scapholunate ligament delayed reconstruction? Br J Sports Med. 2013;47(17):1071–4. doi: 10.1136/bjsports-2013-092795. [DOI] [PubMed] [Google Scholar]
- 38.Harvey EJ, Berger RA, Osterman AL, Fernandez DL, Weiss AP. Bone-tissue-bone repairs for scapholunate dissociation. J Hand Surg [Am] 2007;32(2):256–64. doi: 10.1016/j.jhsa.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 39.Soong M, Merrell GA, Ortmann F, Weiss AP. Long-term results of bone-retinaculum-bone autograft for scapholunate instability. J Hand Surg [Am] 2013;38(3):504–8. doi: 10.1016/j.jhsa.2012.12.013. [DOI] [PubMed] [Google Scholar]
- 40.Fok MW, Fernandez DL. Chronic scapholunate instability treated with temporary screw fixation. J Hand Surg [Am] 2015;40(4):752–8. doi: 10.1016/j.jhsa.2014.12.004. [DOI] [PubMed] [Google Scholar]
- 41.Ross M, Loveridge J, Cutbush K, Couzens G. Scapholunate ligament reconstruction. J Wrist Surg. 2013;2(2):110–5. doi: 10.1055/s-0033-1341962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.van de Grift TC, Ritt MJ. Management of lunotriquetral instability: a review of the literature. J Hand Surg Eur Vol. 2016;41(1):72–85. doi: 10.1177/1753193415595167. [DOI] [PubMed] [Google Scholar]
- 43.Atkinson CT, Watson J. Lunotriquetral ligament tears. J Hand Surg [Am] 2012;37(10):2142–4. doi: 10.1016/j.jhsa.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 44.Mirza A, Mirza JB, Shin AY, Lorenzana DJ, Lee BK, Izzo B. Isolated lunotriquetral ligament tears treated with ulnar shortening osteotomy. J Hand Surg [Am] 2013;38(8):1492–7. doi: 10.1016/j.jhsa.2013.05.024. [DOI] [PubMed] [Google Scholar]


