Abstract
Purpose of review
Injuries to the great toe are common in athletes. While most are managed nonoperatively and allow return to sports activity, some great toe injuries are highly problematic and can impact function. The purpose of this review is to highlight several specific injuries and disease processes involving the hallux and to detail current recommendations and management options in order to help raise suspicion for injuries that can result in long-term dysfunction.
Recent findings
Toe injuries have been found to represent nearly 10% of injuries presenting to fracture clinics. While most injuries can be treated nonsurgically, there are a number of specific injuries that require a high index of suspicion, careful management, and in some cases, surgical intervention. Injuries detailed in this review include turf toe, traumatic bunion, and hallux and sesamoid fractures. Additional pathologies that are covered include sesamoiditis and sesamoid avascular necrosis as well as hallux rigidus. Appropriate workup and current treatment recommendations are discussed.
Summary
Injuries to the hallux can result in long-term pain and disability if not properly diagnosed and treated. A high index of suspicion is required.
Keywords: Hallux injury, Sesamoids, Fracture, Turf toe, Traumatic bunion
Introduction
Injuries to the hallux are common in athletes of nearly every age group and level of participation. These can range from mild toe stubbing injuries with minimal soft tissue disruption to severe fracture dislocations resulting in long-term pain and dysfunction. One of the challenges in treating these injuries is expeditiously differentiating mild injuries that will do well with conservative management from those which will require surgical reconstruction to restore function and avoid long-term complications. Given that many of these patients will present to urgent care facilities or primary care offices, providers must maintain a high index of suspicion and an understanding of the workup and management for these injuries. This review is intended to provide an overview of common and/or commonly missed injuries to the hallux in order to provide guidance regarding recent treatment principles.
Anatomy
The hallux metatarsophalangeal (MTP) joint is a ginglymoarthrodial joint, meaning a ball and socket hinged joint with a sliding component. The proximal articular surface of the proximal phalanx has a concave shape that matches the transversely oriented metatarsal head, which is larger in the transverse plane than in the dorsoplantar plane. Stability is provided mainly by the ligamentous and soft tissue structures spanning the joint with little stability provided by the shallow articulation. An intraarticular meniscus is commonly seen and is believed to enhance stability [1]. There are two tubercles on the plantar aspect of the proximal phalanx, adjacent to the articular surface, allowing muscular attachments (extensor and flexor hallucis brevis, intrinsics, and the adductor and abductor halluces). The extensor hallucis longus (EHL) and the flexor hallucis longus (FHL) cross the joint at the midpoint directly dorsal and plantar and insert on the distal phalanx.
The plantar plate capsuloligamentous complex contains the larger medial/tibial sesamoid and the smaller, rounder, and slightly more proximal lateral/fibular sesamoid. The sesamoids form through multiple ossification centers and are supplied by the sesamoid artery, which is a terminal branch of the medial plantar artery. The sesamoids act to increase the lever arm of the flexor hallucis brevis (FHB) and provide protection to the FHL tendon, which runs plantar between the sesamoids on the plantar aspect of the great toe. The sesamoids are embedded within the FHB tendon slips and articulate with the plantar metatarsal head. This articulation also acts to off-load some of the forces through the MTP joint. The fibrocartilaginous plantar plate allows for smooth gliding of the sesamoids and also provides stability through its connections with the deep transverse metatarsal ligament, the flexor tendon sheaths, and the plantar aponeurosis.
The medial and lateral proper digital nerves arise from the medial plantar nerve and run deep to the transverse metatarsal ligament. The dorsomedial cutaneous nerve is an extension of the superficial peroneal nerve whereas the dorsolateral cutaneous nerve is an extension of the deep peroneal nerve. These nerves lie on their respective side of the EHL tendon and have been shown in cadaver studies to be, on average, 3.4 and 4 mm from standard dorsolateral and dorsomedial metatarsophalangeal joint arthroscopy portal sites, respectively [2].
The MTP joint provides balance during standing as well as essential power in the toe-off phase during activities from normal walking to jumping. This small joint has been shown biomechanically to have joint reaction forces of up to 80% of the body weight through the toe-off phase of normal walking. This force can increase up to 200–300% of the body weight with athletic activity and up to 800% with jumping [3]. Injury to this complex can result in pain, weakness, and instability which can impact performance considerably.
Turf toe injuries
Background
Originally described in the 1970s, turf toe injuries were first recognized due to the use of artificial turf in the American football league [4]. This was due to increasingly flexible shoes on a surface that did not give way like natural grass. The mechanism of injury was determined to be hyperdorsiflexion of the hallux combined with an axial load such as when a player falls back onto his own heel with his toe hyperextended and heel in equinus or steps out onto another players foot resulting in toe hyperextension [5] (Fig. 1). A recent retrospective review among NCAA football athletes suggested that the incidence has decreased in this population due to changes in shoe wear as well as improvements in artificial turf [6]. In the 1970s, the incidence was reported to be as high as 5–6 players per team each season with 30–45% of NFL players reporting a history of such injury and up to 83% of these injuries occurring on artificial turf. While it is still suggested that artificial turf results in a significant increase in risk of the injury, the recently reported incidence of turf toe injury is around 0.45–0.53 players per team each season [6].
Fig. 1.
Illustrations of common turf to injury mechanisms, including a MTP joint hyperdorsiflexion when the forefoot collides with another shoe. b MTP is hyperdorsiflexed as the player lands with the great toe dorsiflexed with impact on the heel from self or another player
The pathoanatomy of turf toe injury involves disruption of the plantar capsuloligamentous structures of the hallux MTP joint including the plantar plate, intersesamoid ligament, phalangeal sesamoid ligaments, and collateral ligaments. The degrees of injury can range from simple sprains of the capsuloligamentous complex to frank dislocations of the MTP joint. A recent biomechanical study found that forceful dorsiflexion of the MTP joint past 78° resulted in a 50% probability of injury [7].
Presentation
Turf toe injuries are now known to be caused by a variety of mechanisms. Patients can present after an acute high-energy mechanism with significant swelling and ecchymosis. Others may be more subtle injuries with insidious onset and lacking overwhelming clinical findings. These situations may result in failure to recognize the injury and ultimately a prolonged recovery due to inadequate treatment [8]. Therefore, a high index of suspicion is key to recognizing and appropriately managing these injuries.
While previous reports suggest that these injuries require a significant amount of force, recently, it has been suggested that there may be cases where the injury occurs more insidiously, possibly due to a stress-related phenomenon. Roche et al. recently described a case involving a 31-year-old professional soccer player who developed significant pain with MTP dorsiflexion and was found to have complete rupture of his lateral plantar plate with diastasis of a bipartite sesamoid in the absence of overt injury [9].
Workup
Significant injury is suggested by ecchymosis, dorsal or medial joint line tenderness, or even intrinsic minus positioning of the hallux suggesting disruption of FHB or its insertion [1]. In cases of MTP dislocation, those that are easily reduced tend to have more extensive injuries since the intersesamoid ligament is usually disrupted, whereas those that are more difficult to reduce might include the metatarsal head buttonholed around the ligament. Immediately following a complete injury, dorsiflexion range of motion might be increased due to loss of plantar restraints. However, after swelling ensues, these injuries usually result in relative stiffness of the MTP joint. Stability of the MTP joint can be tested similar to a Lachman’s test of the knee, with a dorsally applied stress on the proximal phalanx while stabilizing the metatarsal and comparing the exam to the contralateral side. Pain and laxity are positive tests.
AP and lateral x-rays alone can be sufficient in some cases to identify proximal migration or fracture of the sesamoids compared to the contralateral side in severe injuries. Additionally, views include 40° medial and lateral oblique x-rays and a sesamoid view to better visualize the sesamoids. In cases of bipartite sesamoids, particular attention needs to be drawn to whether or not there is diastasis [10]. Live fluoroscopy can be helpful in distinguishing an intact bipartite sesamoid versus an acute diastasis or fracture as the proximal sesamoid would lag behind the distal sesamoid with increasing dorsiflexion of the hallux [11].
In a cadaveric biomechanical study, Waldrop et al. sequentially sectioned the medial collateral ligament, lateral collateral ligament, and the tibial and fibular phalangeal sesamoid ligaments. They then used a standardized method to dorsiflex the toe and obtain a lateral radiograph to measure the distance between the proximal phalanx and the sesamoids. They found that in any of the various combinations, sectioning any two ligaments did not cause a significant increase in distance; however, sectioning any three of the ligaments caused an average of 3 mm of separation from baseline. They suggested that dorsiflexion stress views can be utilized to determine the severity of injury and suggested that >3 mm of separation compared to the contralateral side was an indication of a complete injury and that surgical intervention was warranted [8].
Magnetic resonance imaging (MRI) can be useful in ambiguous cases; however, it needs to be interpreted with caution as they have been shown to overestimate the degree of injury. Dietrich et al. obtained MRIs in 30 asymptomatic volunteers and found that the collateral ligaments frequently contained hyperintense areas on fluid-weighted sequences with fat suppression and on intermediate weighted sequences [12].
Classification
Turf toe injuries are most commonly graded as 1 (stretching), grade 2 (partial ligament injury), or grade 3 (complete ligament injury). Clinical findings for each grade of injury are outlined in Table 1.
Table 1.
Classifications of turf toe injuries [13]
| Hyperextension injuries (turf toe) | Grade | Description |
|---|---|---|
| I | • Local tenderness • Minimal swelling • No ecchymosis • Mild restriction in range of motion • Performance mildly inhibited |
|
| II | • Intense and more diffuse tenderness • Moderate swelling • Ecchymosis may be present • Moderate restriction in range of motion • Performance inhibited |
|
| III | • Severe pain with both plantar and dorsal tenderness • Marked swelling and ecchymosis • Severely limited range of motion |
Treatment
In cases of low-grade sprains, conservative management is recommended with rest, ice, and gradual return to sport activities after 2–6 weeks once painless dorsiflexion to 50°–60° can be performed [6]. Casting in plantar flexion is a conservative modality used at our institution that can provide soft tissue rest and allow the plantar structures to heal in appropriate tension in moderate injuries. Morton’s extension insoles or walking cam boots with a sesamoid recess can be beneficial [14] to reduce forces and extremes of motion during normal gait and return to activities. Corticosteroid injections are discouraged as these can increase the risk of further injury by masking symptoms.
In complete ligament injury cases (grade 3), direct repair of the injured structures has been reported with good results. Operative indications include large capsular avulsions with an unstable joint, sesamoid fracture or bipartite sesamoid with diastasis or retraction of the sesamoids, vertical instability on examination, traumatic hallux valgus, chondral injury with intraarticular loose body, or failure of nonsurgical management [1]. The typical approach is via a medially based incision at the 1st metatarsal that is then angled 90° at the plantar MTP crease. Direct repair of intrasubstance tears can be performed versus suture anchor repair if the structures have avulsed from the proximal phalanx [15].
Post-operatively, the toe is placed into a toe spica splint in approximately 10°–20° of plantar flexion. Gentle, protected active assisted range of motion is initiated at 1 week post-op to avoid MTP joint arthrofibrosis. It is critical that passive dorsiflexion and resisted plantar flexion be avoided early on. Nonweight bearing in a short boot should be continued until 4 weeks post-op. At 4 weeks, weight bearing may be initiated as well as passive and active range of motion of the toe. At 8 weeks, the boot is discontinued and replaced with accommodative shoes reinforced with a turf toe plate or Morton’s extension. Gradual progression can begin with therapy with return to sport expected at 12 to 16 weeks. Patient expectations must be tempered with the understanding that full participation may take up to a year and that residual pain and stiffness are common.
Sesamoid fracture
Due to the high loads placed on the plantar 1st metatarsal head along with the significant stresses placed across the 1st MTP joint during sports activities, the sesamoids are highly susceptible to fracture. Fractures can be classified as being either acute or stress with acute fractures typically occurring in the setting of significant turf toe injury (discussed above). Cases of acute fracture more commonly involve the tibial sesamoid, and fractures are often transverse. The fibular sesamoid can be involved but is relatively protected due to its ability to slip between the 1st and 2nd metatarsal heads during the injury. While displaced fractures suggest a disruption in the plantar plate and sesamoid complex requiring surgical repair, in most cases, the abundant soft tissue connections hold the fragments in relative apposition. In these nondisplaced or minimally displaced fractures, conservative treatment is the first line in management. The typical protocol involves 4–6 weeks of rigid immobilization with the toe in plantar flexion with an additional period of protected weight bearing and gradual return to normal activity. However, nondisplaced sesamoid fractures can be difficult to distinguish from bipartite sesamoids. Criteria for diagnosing an acute fracture include irregular separation of the sesamoid with serrated edges, evidence of callous formation on repeat radiographs, normal appearance of the contralateral sesamoid (bipartite sesamoids are present in 85% of cases [16]), extensive edema on MRI, or evidence of fracture upon surgical visualization [17] (Fig. 2).
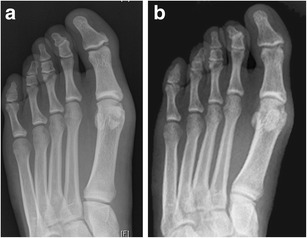
Fig. 2.

Images illustrating bipartite sesamoid intersesamoid sprain. a Initial AP radiograph suggesting bipartite sesamoid and MRI suggesting inter-bitartite sesamoid separation. b Contralateral foot radiographs revealing bitartite sesamoid. c Follow-up radiographs after 6 weeks of conservative treatment without improvement in symptoms. Callus formation suggests fracture
Stress fractures also occur more commonly in the tibial sesamoid. Diagnosis can be difficult as radiographs are often normal for months after the onset of symptoms. Radionucleotide scanning and MRI scans are more sensitive early, and CT scans are more specific for fracture. Additionally, if a high suspicion exists, stress radiographs with the hallux dorsiflexed may reveal separation in both acute or stress fractures.
While most sesamoid fractures will heal when diligently diagnosed and appropriately treated (Fig. 3, sesamoid nonop), a potential complication of nonoperatively treatment of sesamoid fractures is nonunion. While the true incidence is not known, this complication is often cited as a cause of persistent pain and inability of high level athletes with the injury to return to play. This is more likely to occur in displaced fractures and in fractures that are initially misdiagnosed. In these cases, autogenous bone grafting has been shown to result in high rates of fusion. Anderson and McBryde reported a 90% union rate with most of these patients obtaining relief of their symptoms and return to preinjury level of activity [18]. In cases of transverse fracture patterns, percutaneous screw fixation has been successful in small case series with less risk of wound complications that can plague open procedures on the plantar aspect of the foot (Fig. 4 sesamoid ORIF) [19].
Fig. 3.
Nonoperatively treated sesamoid fracture in collegiate football player. a Injury film. b Three months post-injury
Fig. 4.
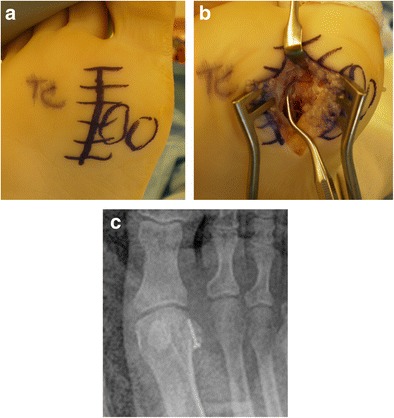
Photographs of surgically treated sesamoid fracture illustrating a plantar incision lateral to the fibular sesamoid and b the fracture site debrided of fibrous tissue (Images courtesy of Loretta Chou, MD)
Sesamoidectomy is a described treatment in cases of recalcitrant pain after conservative therapy, particularly in complex and comminuted fracture patterns, failed grafting, degenerative joint disease, and avascular necrosis (AVN). Risks include development of hallux valgus with medial sesamoidectomy or hallux varus with lateral sesamoidectomy (10–20% risk [20]), claw toe deformity due to disruption of the FHB, and transfer metatarsalgia in addition to risks such as wound complications and nerve injury. When done for cases of sesamoid fracture, the results are promising with most studies reporting improvement in pain and return to activities [21]. Bichara et al., in their study out of Massachusetts General Hospital, reported on 24 cases of sesamoidectomy performed in athletes who had failed conservative management. They reported a significant improvement in pain, and 22 of 24 patients returned to full activity at an average of approximately 12 weeks. Only one patient developed alignment deformity (hallux valgus after medial sesamoidectomy).
Sesamoiditis and avascular necrosis
The sesamoid complex acts as a pulley with the sesamoids acting to improve the moment arm of the flexor force on the MTP joint during the toe-off phase of normal walking and running. They play an intricate role in the windlass mechanism of the foot via their numerous attachments to the plantar plate and plantar fascia.
Sesamoiditis
The sesamoid region experiences substantial forces during running and jumping activities, which, when excessive or repetitive, can result in inflammation of one or both of the sesamoids or surrounding soft tissues. This repetitive trauma can be due to increased activity, poor shoe wear, or anatomic variations that place increased stress on the base of the 1st metatarsal head such as a pes cavus foot, hindfoot varus, or equinus. Sesamoiditis can also be caused by conditions such as infection, inflammatory arthropathies, and osteoarthritis in the absence of repetitive trauma [22].
Patients can present with nonspecific complaints of forefoot or great toe pain. A careful history and physical exam is important to localize the site of maximal tenderness or the timing of the pain during the gait cycle. Weight-bearing radiographs of bilateral feet are the initial imaging modality of choice. If sesamoid pathology is suspected, then 40° medial and lateral oblique radiographs in addition to a weight-bearing axial sesamoid radiograph can be obtained to evaluate for sesamoid fractures or subluxation, respectively. CT and MRI can be helpful, and bone scan has been shown to detect cases in which there is pain in patients with otherwise normal x-rays [23]. Additionally, targeted injections can act as a diagnostic aid to help localize the pain generator.
Avascular necrosis of the sesamoid
Typically presenting as forefoot pain in the toe-off phase of gait, sesamoid AVN is most commonly seen in women between ages 18 and 29 years. The tibial sesamoid is more commonly involved. The disease process was initially described by Alex Renander in 1924 and is known as Morbus Renander [24]. Predisposing factors are similar to those for sesamoiditis (i.e. cavus foot, tight Achilles/equinus, high heel shoes, repetitive trauma).
On exam, patients typically have pain to direct palpation of the involved sesamoid with painful resisted plantar flexion of the hallux MTP. Radiographs may reveal fragmentation; however, MRI is the most sensitive diagnostic tool and can provide information regarding the stage of the AVN with early stages revealing low intensity on T1-weighted images and hyperintensity on T2- and STIR-weighted images (Fig. 5). In later stages, the T2 images will reveal hypointense areas where the necrotic bone has become sclerotic [25].
Fig. 5.
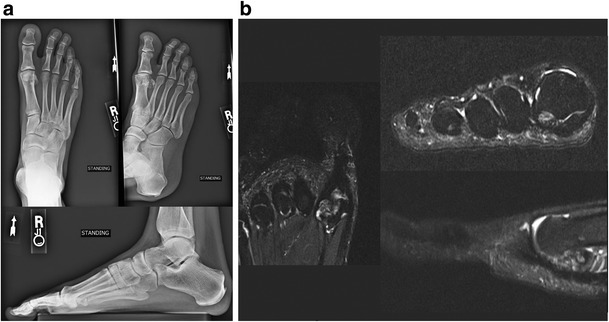
a Radiographs demonstrating fragmentation of the fibular sesamoid with early degenerative changes in the MTP joint. b T2-weighted MRI revealed heterogeneous, hyperintense signal within the sesamoid
Treatment
The first-line treatment for sesamoiditis and sesamoid AVN is conservative management with off-loading of the MTP joint, relative immobilization with rocker sole shoes or orthoses with or without metatarsal recess, avoidance of high heels, activity modification, and anti-inflammatory medications. If conservative management is unsuccessful, then surgical management should first attempt to correct any underlying cause such as gastrocnemius recession, first ray osteotomy, or correction of rigid cavus. Sesamoidectomy should only be considered in cases where there is normal alignment of the first ray, absence of toe clawing, and persistent pain despite a lengthy attempt at conservative management. For patients with AVN who fail conservative treatment, it is less likely to achieve resolution of the disease process with correction underlying anatomic causes and sesamoidectomy may be indicated with or without additional correction of malalignment or anatomic abnormalities.
Traumatic bunion deformity
Traumatic hallux valgus is rare but can occur following injury to the great toe. Traumatic injury to the medial capsule, the abductor hallucis or medial FHB tendons, or the ligamentous structures of the hallux result from a significant valgus force or hyperadduction injury. Avulsion fracture of the proximal phalanx can also occur (Fig. 6, hallux valgus) The resulting alteration in mechanics and joint reactive forces can limit power and lead to early-onset arthritis and functional decline. Surgical correction is indicated in patients without significant MTP arthritis who have flexible interphalangeal (IP) and MTP joints. Surgery consists of repair of the medial structures and, when necessary, release of some lateral structures to restore normal hallux alignment (Fig. 7, hallux valgus post-op). If tissues are insufficient or degenerative (as can occur in chronic cases), the abductor hallucis tendon can be included in the repair.
Fig. 6.

Traumatic hallux valgus with avulsion fracture at the base of the proximal phalanx
Fig. 7.

Post-op radiograph demonstrating correction of hallux valgus after removal of the fragment, medial tissue repair with abductor advancement
Fractures of the hallux
Toe phalangeal fractures are common, comprising 3.6–8% of injuries to the lower extremity [26, 27]. Among children, 5–13% of fractures occur in the foot and, of these, fractures of the toes are the most common. Most fractures of the hallux occur at the distal phalanx and are most commonly a result of a direct crushing type of injury. Stubbing injuries, on the other hand, generally impact the IP joint and can result in dislocations with or without intraarticular fractures [28]. While fractures of the 2nd through 5th toes are generally of little consequence and can typically be treated successfully with conservative measures, fractures of the hallux can lead to significant long-term pain and disability [29]. Unfortunately, the hallux is the most commonly injured toe, representing the greatest proportion of all toe phalangeal fractures (38–56%) [30, 31] (Fig. 8).
Fig. 8.

a Injury radiographs illustrating displaced proximal phalanx fracture of the great toe following direct impact trauma. b Post-operative radiographs following closed reduction with percutaneous pin fixation
Even with the injuries being relatively common, there are no evidence-based guidelines regarding the acceptable alignment or indications for surgical intervention in closed phalangeal fractures in the literature [31]. A recent review of all patients referred to a fracture clinic in London found that of 707 patients seen over a 1-year period, 65 (9%) were seen for toe phalangeal fractures. They reported that only two of these patients required surgery for loss of articular congruency or deformity. They recommended that only fractures with an intraarticular component, ones displaced more than 2 mm, physeal fractures, or open fractures require referral to an orthopedic specialist [31].
Mallet injuries are a specific pattern of fracture that occur due to a hyperflexion injury of the hallux IP joint that results in either a disruption of the extensor hallucis insertion or an avulsion of a dorsal lip of the proximal distal phalanx. Most literature on the topic is in the form of case reports, and treatment algorithms typically follow operative principles published for mallet injuries in the hand [32]. In most reported cases, successful treatment can be obtained via immobilization with extension splinting for 6–10 weeks with the most commonly reported complications including palpable dorsal deformity, mild flexion deformity, and decreased range of motion of the IP joint [28, 33]. Immobilization can be done with a small, custom thermoplast splint placed dorsally that keeps the toe hyperextended and allows the patient to wear most shoes. Operative indications include fractures that involve greater than a third of the joint surface or an unstable joint with plantar subluxation in addition to inability to tolerate, or failure of, nonsurgical management. The rare case reports of operative management in the literature do report improved outcomes in terms of range of motion, pain, and deformity compared to reports of nonoperative management [34, 35]. The typical algorithm involves attempted closed reduction with extension block pinning if there is a larger dorsal fracture or avulsion fragment followed by transarticular pinning with the IP joint in extension or even direct pinning of the fragment. If adequate reduction cannot be achieved, then a dorsal approach can be undertaken with direct visualization and reduction of the fragment. Tendon disruptions or those injuries with small avulsion fragments can usually be treated conservatively with extension splinting. Cases where compliance is difficult due to discomfort from the splint can be successfully treated with transarticular pinning for 5–6 weeks followed by a short period of night splinting [35].
Conclusion
While most injuries to the hallux can be treated with conservative measures such as off-loading, brief immobilization, and other modalities, a high index of suspicion is required when considering treatment strategies. Significant injuries such as turf toe and sesamoid fractures as well as chronic problems of the hallux, the MTP joint, or the sesamoids should be given adequate consideration. In cases that present with out-of-proportion pain, or when reasonable pain continues for an unreasonable amount of time, additional workup is often indicated. While the first step is often obtaining the appropriate radiographs with or without stress views or oblique views to analyze the sesamoids, advanced imaging can often be helpful in determining an underlying diagnosis. The hallux and its related articulations and adjacent structures cannot be ignored especially in light of the significant demands we place on it during normal and athletic activities. It is, therefore, important for providers who interact with these patients to have a high index of suspicion and to be ready to make a referral to a specialist in any case that may require surgical intervention.
Compliance with ethical standards
Conflict of interest
Philip J York and Frank B Wydra declare that they have no conflict of interest.
Kenneth J Hunt reports grants from Acumed and ISAKOS outside of the submitted work.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Foot and Ankle Sports Medicine
Contributor Information
Philip J. York, Email: philip.york@ucdenver.edu
Frank B. Wydra, Email: frank.wydra@ucdenver.edu
Kenneth J. Hunt, Email: kenneth.j.hunt@ucdenver.edu
References
- 1.Mason LW, Molloy AP. Turf toe and disorders of the sesamoid complex. Clin Sports Med. 2015;34:725–739. doi: 10.1016/j.csm.2015.06.008. [DOI] [PubMed] [Google Scholar]
- 2.Vaseenon T, Phisitkul P. Arthroscopic debridement for first metatarsophalangeal joint arthrodesis with a 2- versus 3-portal technique: a cadaveric study. Arthrosc—J Arthrosc Relat Surg. 2010;26:1363–1367. doi: 10.1016/j.arthro.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 3.McBride ID, Wyss UP, Cooke TD, et al. First metatarsophalangeal joint reaction forces during high-heel gait. Foot Ankle. 1991;11:282–288. doi: 10.1177/107110079101100505. [DOI] [PubMed] [Google Scholar]
- 4.Bowers KD, Martin RB. Turf-toe: a shoe-surface related football injury. Med Sci Sports. 1976;8:81–83. [PubMed] [Google Scholar]
- 5.Watson TS, Anderson RB, Davis WH. Periarticular injuries to the hallux metatarsophalangeal joint in athletes. Foot Ankle Clin. 2000;5:687–713. [PubMed] [Google Scholar]
- 6.George E, Harris AHS, Dragoo JL, Hunt KJ. Incidence and risk factors for turf toe injuries in intercollegiate football: data from the National Collegiate Athletic Association Injury Surveillance System. Foot Ankle Int. 2014;35:108–115. doi: 10.1177/1071100713514038. [DOI] [PubMed] [Google Scholar]
- 7.Frimenko RE, Lievers WB, Riley PO, et al. Development of an injury risk function for first metatarsophalangeal joint sprains. Med Sci Sports Exerc. 2013;45:2144–2150. doi: 10.1249/MSS.0b013e3182994a10. [DOI] [PubMed] [Google Scholar]
- 8.Waldrop NE, Zirker CA, Wijdicks CA, et al. Radiographic evaluation of plantar plate injury: an in vitro biomechanical study. Foot ankle Int. 2013;34:403–408. doi: 10.1177/1071100712464953. [DOI] [PubMed] [Google Scholar]
- 9.Roche AJ, Calder JD. An atraumatic turf toe in an elite soccer player—a stress related phenomenon? Foot Ankle Surg. 2014;20:71–73. doi: 10.1016/j.fas.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 10.Rodeo SA, Warren RF, O’Brien SJ, et al. Diastasis of bipartite sesamoids of the first metatarsophalangeal joint. Foot Ankle. 1993;14:425–434. doi: 10.1177/107110079301400801. [DOI] [PubMed] [Google Scholar]
- 11.Hsu AR, Anderson RB. Foot and ankle injuries in American football. Am J Orthop (Belle Mead NJ) 2016;45:358–367. [PubMed] [Google Scholar]
- 12.Dietrich TJ, da Silva FLF, de Abreu MR, et al. First metatarsophalangeal joint- MRI findings in asymptomatic volunteers. Eur Radiol. 2015;25:970–979. doi: 10.1007/s00330-014-3489-y. [DOI] [PubMed] [Google Scholar]
- 13.Anderson RB. Turf toe injuries of the hallux metatarsophalangeal joint. Tech Foot Ankle Surg. 2002;1:102–111. doi: 10.1097/00132587-200212000-00004. [DOI] [Google Scholar]
- 14.McCormick JJ, Anderson RB. Turf toe: anatomy, diagnosis, and treatment. Sport Heal A Multidiscip Approach. 2010;2:487–494. doi: 10.1177/1941738110386681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Doty J, Coughlin M. Turf toe repair. A technical note. Foot Ankle Spec. 2015;6:452–456. doi: 10.1177/1938640013507107. [DOI] [PubMed] [Google Scholar]
- 16.Jahss MH. The sesamoids of the hallux. Clin Orthop Relat Res. (1981); 88–97. [PubMed]
- 17.Dedmond BT, Cory JW, McBryde A. The hallucal sesamoid complex. J Am Acad Orthop Surg. 2006;14:745–753. doi: 10.5435/00124635-200612000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Anderson RB, McBryde AM., Jr Autogenous bone grafting of hallux sesamoid nonunions. Foot Ankle Int. 1997;18:293–296. doi: 10.1177/107110079701800509. [DOI] [PubMed] [Google Scholar]
- 19.Blundell CM, Nicholson P, Blackney MW. Percutaneous screw fixation for fractures of the sesamoid bones of the hallux. J Bone Joint Surg Br. 2002;84:1138–1141. doi: 10.1302/0301-620X.84B8.13064. [DOI] [PubMed] [Google Scholar]
- 20.Pagenstert GI, Valderrabano V, Hintermann B. Medial sesamoid nonunion combined with hallux valgus in athletes: a report of two cases. Foot ankle Int / Am Orthop Foot Ankle Soc [and] Swiss Foot Ankle Soc. 2006;27:135–140. doi: 10.1177/107110070602700212. [DOI] [PubMed] [Google Scholar]
- 21.Aper RL, Saltzman CL, Brown TD. The effect of hallux sesamoid excision on the flexor hallucis longus moment arm. Clin Orthop Relat Res. (1996); 209–217. [DOI] [PubMed]
- 22.Taylor CF, Butler M, Parsons SW. Problems associated with the excision of the hallux sesamoids. Foot Ankle Clin. 2014;19:425–436. doi: 10.1016/j.fcl.2014.06.014. [DOI] [PubMed] [Google Scholar]
- 23.Yang R, Chu Y. Hallucal sesamoiditis manifested on bone scan. Clin Nucl Me. 2013;38:1019–1021. doi: 10.1097/RLU.0000000000000283. [DOI] [PubMed] [Google Scholar]
- 24.Ogata K, Sugioka Y, Urano Y, Chikama H. Idiopathic osteonecrosis of the first metatarsal sesamoid. Skelet Radiol. 1986;15:141–145. doi: 10.1007/BF00350208. [DOI] [PubMed] [Google Scholar]
- 25.Waizy H, Jäger M, Abbara-Czardybon M, et al. Surgical treatment of AVN of the fibular (lateral) sesamoid. Foot ankle Int / Am Orthop Foot Ankle Soc [and] Swiss Foot Ankle Soc. 2008;29:231–236. doi: 10.3113/FAI.2008.0231. [DOI] [PubMed] [Google Scholar]
- 26.Shibuya N, Davis ML, Jupiter DC. Epidemiology of foot and ankle fractures in the United States: an analysis of the National Trauma Data Bank (2007 to 2011) J Foot Ankle Surg. 2014;53:1–3. doi: 10.1053/j.jfas.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 27.Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37:691–697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 28.Hennessy MS, Saxby TS. Traumatic “mallet toe” of the hallux: a case report. Foot Ankle Int. 2001;22:977–978. doi: 10.1177/107110070102201209. [DOI] [PubMed] [Google Scholar]
- 29.Petnehazy T, Schalamon J, Hartwig C, et al. Fractures of the hallux in children. Foot ankle Int. 2015;36:60–63. doi: 10.1177/1071100714552482. [DOI] [PubMed] [Google Scholar]
- 30.Van Vliet-Koppert ST, Cakir H, Van Lieshout EMM, et al. Demographics and functional outcome of toe fractures. J Foot Ankle Surg. 2011;50:307–310. doi: 10.1053/j.jfas.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 31.Eves TB, Oddy MJ. Do broken toes need follow-up in the fracture clinic? J Foot Ankle Surg. 2016;55:488–491. doi: 10.1053/j.jfas.2016.01.034. [DOI] [PubMed] [Google Scholar]
- 32.Martin EA, Barske HL, DiGiovanni BF. Open surgical treatment of an acute, unstable bony mallet injury of the hallux. Foot Ankle Int. 2013;34:295–298. doi: 10.1177/1071100712465850. [DOI] [PubMed] [Google Scholar]
- 33.Rapoff AJ, Heiner JP. Avulsion fracture of the great toe: a case report. Foot ankle Int / Am Orthop Foot Ankle Soc [and] Swiss Foot Ankle Soc. 1999;20:337–339. doi: 10.1177/107110079902000514. [DOI] [PubMed] [Google Scholar]
- 34.Wada K, Yui M. Surgical treatment of mallet toe of the hallux with the extension block method: a case report. Foot Ankle Int. 2011;32:1086–1088. doi: 10.3113/FAI.2011.1086. [DOI] [PubMed] [Google Scholar]
- 35.Nakamura S. Temporary Kirschner wire fixation for a mallet toe of the hallux. J Orthop Sci. 2007;12:190–192. doi: 10.1007/s00776-006-1106-x. [DOI] [PubMed] [Google Scholar]


