Abstract
Purpose of review
The purposes of this review are to discuss the diagnosis and management of mallet and jersey finger injuries in athletes and to highlight how treatment impacts return to play.
Recent findings
Mallet finger: although numerous non-operative and operative techniques have been described, there continues to be little consensus regarding the optimal procedure. Jersey finger: ultrasound appears to be a cost-effective imaging modality that may be useful for preoperative planning. Wide-awake surgery offers optimal intraoperative assessment of the tendon repair. Tendon repair with volar plate augmentation has been shown to improve the strength of the repair in the laboratory, and early clinical results are encouraging.
Summary
Most mallet finger injuries will heal with non-operative treatment over a period of 8–12 weeks, even when treatment is delayed up to 3–4 months. An acute diagnosis of jersey finger requires surgical treatment and generally means 8–12 weeks of inability to compete in most contact sports.
Keywords: Athlete, Distal phalanx, Jersey finger, Mallet finger, Tendon avulsion
Introduction
Finger injuries make up approximately 38% of all upper extremity injuries presenting to emergency departments in the USA [1]. The distal phalanx in particular is prone to sports-related injury due to its location and function. Injuries to the distal phalanx are variable, consisting of isolated or combined soft tissue and bony injuries. The functional consequences of loss of distal interphalangeal joint (DIPJ) motion depend on whether flexion or extension capabilities are lost and generally include decreased dexterity, decreased pinch strength, and decreased grasp capability. Although many patients can adapt to these deficits, pain related to soft tissue injury or post-traumatic arthritis may further limit function and potentially athletic performance. In addition, some patients find a distal interphalangeal extensor lag or a dorsal prominence cosmetically unsightly and will actively seek treatment for esthetic concerns. Therefore, injuries of the distal finger should be scrutinized and managed meticulously in order to limit undesirable outcomes.
These injuries may be dismissed as minor sprains, however, and depending on the sport, some athletes may be capable of “playing through” the injury at a competitive level. It is not uncommon for competitive athletes to present in delayed fashion or once the season has ended. Treatment of athletes should take into account the sport, the playing position, the timing of the season, the level of competition (high school, college, professional), and the patient’s goals. Furthermore, overzealous parents of adolescent and high school athletes, eager for their children to return to play, must be educated and counseled appropriately about the complications of return to play prior to sufficient healing, as well as the complications of delayed or neglected treatment.
In this manuscript, the diagnosis and treatment of mallet finger and jersey finger injuries are discussed with a focus on athletes. Special considerations are given to more recently described treatment techniques and areas of controversy.
Pertinent anatomy
The anatomy of the distal phalanx is unique and complex. The normal range of motion at the DIPJ is between 0° and 85°, although the functional flexion posture has been reported to be 39° [2]. Substantial stability to the DIPJ is provided by the combination of the extensor and flexor tendons, a thick volar plate and stout collateral ligaments. The dorsal portion of the collateral ligaments provides rebound extension of the flexed DIPJ, protecting the joint from greater than 45° of volar subluxation despite a complete disruption of the extensor tendon [3, 4]. The short lever arm of the DIPJ further contributes to its stability, as evidenced by the rarity of simple DIPJ dislocations [5].
The extensor tendon to each digit trifurcates just proximal to the proximal interphalangeal joint (PIPJ) into one central slip and two lateral slips. The central slip inserts onto the middle phalanx while the lateral slips coalesce with the tendons of the interosseous and lumbrical muscles to form the lateral bands. The lateral bands then cross the DIPJ to insert as the terminal tendon on the dorsal epiphysis of the distal phalanx. The proximal extent of the germinal matrix is very close to the insertion of the terminal tendon and lies on average 1.2 mm distally [6].
The flexor digitorum superficialis (FDS) tendons lie superficial (palmar) to the flexor digitorum profundus (FDP) at the carpal tunnel and the palm. At the level of the proximal phalanx, however, the FDS tendon bifurcates and courses dorsally, allowing the FDP to become superficial at the level of the PIPJ. Shortly after they bifurcate, the two FDS slips coalesce to form Camper’s chiasm, before splitting up a second time and inserting on the volar aspect of the middle phalanx just distal to the PIPJ. The FDP, travels distally and attaches on the volar metaphysis of the distal phalanx. Long and short vincula, which are folds of the mesotenon that contain blood vessels, are a major source of nutrition to both FDP and FDS tendons and become clinically relevant structures in jersey finger injuries.
Although a disruption of the extensor tendon at the level of the DIPJ does not typically lead to proximal retraction [7], the extensor tone is increased at the level of the PIPJ. Over time, an imbalance of the flexor and extensor tendons may develop, leading to a swan-neck deformity, characterized by a hyperextended PIPJ and flexed DIPJ. This is particularly apparent when there is excess laxity or injury at the palmar plate of the PIPJ. On the other hand, injury to the FDP usually results in proximal tendon retraction [8]. Therefore, early diagnosis and treatment of both mallet finger and jersey finger injuries result in better outcomes in most clinical scenarios.
Mallet finger
Description and background
Mallet finger is a term used to describe traumatic loss of terminal extensor function at the level of the DIPJ of the fingers or thumb. The usual mechanism of injury involves an axial, or jamming, force directed at the fingertip while the DIPJ is in active extension. The axial load forces the DIPJ into flexion resulting in avulsion of the extensor tendon. Less common mechanisms of injury include hyperextension injuries [9] and sharp lacerations. Mallet fingers can occur during any contact sports such as softball, baseball, football, basketball, or soccer, in which the hand is subjected to force from a ball, a fall, or another player.
Diagnosis of the injury
Patients present with a painful or painless deformity and inability to fully extend the DIPJ. Other conditions that mimic a mallet finger include a bony exostosis or a Seymour fracture in the pediatric and adolescent populations [10]. The lateral X-ray will usually confirm the diagnosis and will reveal whether the injury is purely tendinous or if there is a bony component (Fig. 1). Mallet injuries have been classified by several authors including Doyle [11] and Wehbé and Schneider [12]. The Burton classification is reserved for chronic mallet injuries and takes into account the flexibility of the deformity [13] (Table 1).
Fig. 1.

a A 49-year-old male with a purely tendinous mallet finger and noticeable extensor lag. There is also noticeable hyperextension at the level of the PIPJ, resulting in a swan-neck deformity b A 16-year old male with a bony mallet finger involving a fleck of bone and minimal extensor lag as the finger is in a cylinder cast. The shadow of the cast can be appreciated on the radiograph
Table 1.
Commonly referenced classifications of mallet finger injuries
| Doyle [11] | |
| Type I | Closed injury, with or without small dorsal avulsion fracture |
| Type II | Open injury, laceration of tendon |
| Type III | Open injury with loss of skin, subcutaneous cover, and tendon substance |
| Type IV | Mallet fracture |
| A | Transepiphyseal plate fracture in children |
| B | Hyperflexion injury with fracture of articular surface of 20 to 50% |
| C | Hyperextension injury with fracture of the articular surface >50% and with early or late volar subluxation of distal phalanx |
| Wehbé and Schneider [12] (for bony mallet injuries) | |
| Type Ia | Fractures without subluxation of the distal interphalangeal joint |
| Type IIa | Fractures with subluxation of the distal interphalangeal joint |
| Type IIIa | Epiphyseal and physeal injuries |
| Subtype A | Fracture fragment involving less than one-third of the articular surface of the distal phalanx |
| Subtype B | Fracture fragment involving one-third to two-thirds of the articular surface |
| Subtype C | Fragment that includes more than two thirds of the articular surface |
| Burton [13] (for chronic mallet injuries) | |
| Stage I | Supple, passively correctable deformity |
| Stage II | Fixed contracture, contracted lateral bands |
| Stage III | Fixed contracture, joint fibrosis, collateral ligament and palmar plate contractures |
aEach of these fracture types may be divided into three subtypes. Any of these fractures may be accompanied by hyperextension of the proximal interphalangeal joint.
Non-operative treatment
Conservative treatment involves splint immobilization of the DIPJ in a neutral position, typically without immobilization of the PIPJ [5, 14]. Katzman et al. recreated tendinous mallet fingers in a study of 32 cadaveric digits and noted no differences in the amount of extensor tendon gapping at the DIPJ whether or not the PIPJ was immobilized [7]. If a substantial portion of the articular surface is involved and there is marked volar subluxation of the DIPJ, collateral ligament injury at the DIPJ and volar plate injury at the PIPJ may coexist. Under these circumstances, the PIPJ may be immobilized along with the DIPJ. Ideally using a cylinder cast or static splint, the DIPJ is held in neutral to slight hyperextension and the PIPJ in 20–30° of flexion.
Various splints have been used including volar-based Stack splints, dorsal Alumafoam splints, or cylinder casts (Fig. 2). Splints need to be worn 24 h a day. Immobilization for 6 to 8 weeks is recommended for bony mallets, while 8 to 12 weeks of immobilization is recommended for purely tendinous injuries. Patients are instructed on how to safely remove and replace the splints. Complications of non-operative treatment include skin sloughing, blistering, or maceration as a result of prolonged splinting or splinting in hyperextension [5, 15•] (Fig. 3). Other complications of non-operative treatment include recurrence of the mallet deformity and the subsequent development of a swan-neck deformity, both usually the result of poor patient compliance. The development of swan-neck deformity has also been associated with a bony fragment 1/3 to 2/3 the size of the articular surface with DIPJ subluxation [16].
Fig. 2.

Various splints have been used including stack splints (a) and dorsal Alumafoam splints (b)
Fig. 3.

An example of skin maceration over the DIPJ. This rarely leads to long-term complications unless full-thickness skin loss occurs
The literature has consistently demonstrated excellent outcomes in terms of pain relief and restoration of active extension with non-operative treatment of purely tendinous, or bony mallet injuries with less than 30% articular involvement, and no volar subluxation of the distal phalanx [12, 15•, 17]. Large fragments without significant displacement or volar subluxation may also be treated successfully non-surgically [12]. Although controversial, Wehbé and Schneider reported successful non-operative treatment of bony mallets with large articular fragments and volar subluxation, noting open reduction and internal fixation to be a technically demanding procedure and the DIP joint’s remarkable ability to remodel [4, 12]. Good outcomes are usually achieved despite a treatment delay of 3–4 months [15•, 17].
Operative treatment
Traditionally, involvement of greater than 30% of the articular surface, with volar subluxation of the distal phalanx has been an indication for operative treatment [4]. It should be stressed, however, that non-operative treatment of these injuries has resulted in acceptable clinical outcomes. A predictable dorsal prominence and minor loss of motion appear to be the major concerns, but these limitations are generally well accepted by patients [12, 18]. Other factors that may guide the decision-making when considering operative treatment include the patient’s age, hand dominance, type of sport, position, season duration, and the goals of the athlete. The index finger may take priority due to the need for full extension in activities such as pointing or holding a pen or pencil. Open injuries require adequate irrigation and debridement, and this may be performed in the emergency room or operating room, but actual suturing of the tendon and k-wire stabilization of the joint may not be necessary as the terminal tendon does not retract like a flexor tendon would [7].
If the injury is reducible by closed means, pinning of the DIPJ in extension should be attempted as this is a simple, cost-effective, and less morbid procedure relative to open treatment. Numerous variants of percutaneous pinning have been described, including the popular extension block pinning for large bony mallets or simple retrograde pinning for tendinous or small bony mallets [5, 19–21] (Fig. 4).
Fig. 4.
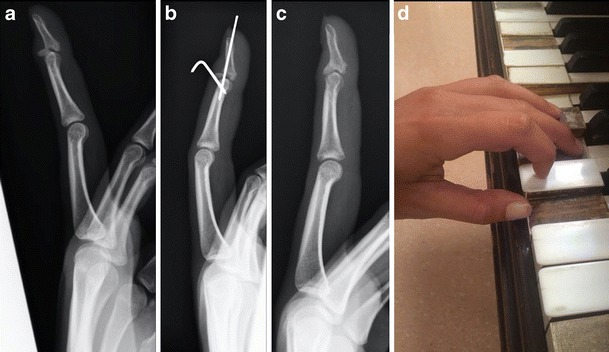
Left middle bony mallet involving a large portion of the articular surface (a). Treated with extension block pinning (b). Radiographic evidence of healing 10 weeks postoperatively (c). The patient was able to resume piano without any difficulties (d)
Open treatment may be warranted on occasion, when the benefits of anatomic healing outweigh the complication risks. Relative to non-operative treatment, successful open treatment has been found to result in improved active DIPJ range of motion and better cosmesis [18]. A dorsal H or Y shaped incision over the DIPJ is typically used. Adequate exposure is necessary, and this is usually achieved by release of the dorsal 20% of the collateral ligaments. The dorsal cortex of the DIPJ is then manually aligned and fixation proceeds with 0.028-in. k-wires, as larger k-wires may lead to fragment comminution. The more invasive nature of open procedures may lead to nail growth deformity, increased scarring, and infection. These potential complications should be thoroughly considered and discussed with the patient prior to proceeding with open treatment. A recent study by Toker et al. [22•] described the use of open reduction and hook plate fixation. The rationale was based on the theoretical advantages of maintenance of anatomic reduction, rigid fixation, and early motion. In comparison to percutaneous extension block pinning, no significant differences in post-operative pain or extensor lag were noted, but hook plate fixation was more expensive and required more soft tissue dissection [22•].
Mallet fingers presenting a few months after injury are considered chronic. Treatment options are guided in part by the flexibility of the mallet or the swan-neck deformity and in part by the patient’s anticipated compliance and activities. The available options include prolonged extension splinting, tenodermodesis, central slip tenotomy, or spiral oblique retinacular ligament (SORL) reconstruction [23]. If the DIPJ becomes painful and arthritic, or if the swan-neck deformity is fixed, DIPJ fusion with palmar plate repair or sublimis tenodesis may be considered.
Return to play
Return to sport is allowed after 8–12 weeks of treatment to give sufficient time for healing and regain in strength. The involvement of a hand therapist enables the implementation of a demand/needs analysis of the given sport, and a series of tests and exercises can ensure readiness for return to play.
Author’s preferred treatment
Early treatment is generally recommended once the diagnosis is made. However, competitive athletes are generally reluctant to loss of play, and an informative discussion about the risks of delayed treatment is mandatory. For a mallet finger, a few weeks of delay in treatment may be acceptable if the athlete is in a critical phase of the season, with the caveat that a secondary injury or the development of a swan-neck deformity may complicate future treatment. If the patient elects to play with the injury, a cylinder cast immobilizing the DIPJ in extension is provided. It should be noted that some patients do well despite no treatment at all. In the senior author’s experience, closed reduction with extension block pinning has been successful in cases of delayed presentation up to 24 weeks. For patients with a secondary swan-neck deformity, SORL reconstruction with palmaris longus or extensor digiti quinti (EDQ) is performed (Fig. 5).
Fig. 5.

A 16-year old male wrestler with a mallet finger that progressed to a flexible swan-neck deformity secondary to concomitant palmar plate injury (a). Reconstruction of the flexible swan-neck deformity using SORL reconstruction with a slip of the EDQ as a tendon graft (b). The graft is fixed to the distal phalanx through a vertical bone tunnel, then rerouted proximally deep to the neurovascular bundle and fixed to the proximal phalanx through a transverse bone tunnel. Tension is adjusted such that passive PIPJ extension results in passive DIPJ extension, a so called dynamic tenodesis (c). Patient immobilized for 6 weeks in a static cast (d). At 4 weeks, the cast may be weaned and gentle active range of motion begun (e). Final follow-up 6 months, full active range of motion (f)
Jersey finger
Description and background
Jersey finger is defined as avulsion of the flexor digitorum profundus tendon off of the volar aspect of the distal phalanx due to forced hyperextension of the DIPJ while the finger is actively flexed. Technically, all jersey fingers are zone I flexor tendon injuries [24]. Similar to mallet finger, jersey finger may be a purely tendinous injury or may be associated with a variably sized bony fragment. Often this occurs while grasping the jersey of an opponent who quickly pulls away (Fig. 6). The FDP of the ring finger is most commonly involved. One potential explanation is that this digit is tethered on both the radial and ulnar sides by bipennate lumbrical muscles and as a consequence is more vulnerable to hyperextension injury [25]. Jersey finger occurs mainly during football and rugby.
Fig. 6.

A classic case of jersey finger in a 14-year-old boy who injured his ring finger following a football tackle
Diagnosis of the injury
Examination reveals inability to make a full fist and loss of active DIPJ flexion of the involved digit. A fleck of avulsed bone typically retracts proximally with the tendon and may be visualized radiographically at the level of the PIPJ. In such an instance, it is critical that a comprehensive clinical examination rules out a PIPJ injury and correctly identifies a profundus avulsion injury. Schneider noted a case of jersey finger with an associated distal phalanx avulsion that was visualized at the level of the PIPJ and was mistakenly treated as a chip fracture of the PIPJ [4].
Non-operative treatment
Non-operative treatment is generally not recommended for jersey finger unless the patient is unable or unwilling to comply with post-operative therapy. Jersey finger is treated surgically when diagnosed acutely.
Operative treatment
The Leddy and Packer classification system for jersey finger injuries describes three injury types and is useful for prognostic and therapeutic considerations [8]. In type I injuries, the tendon retracts into the palm, the long and short vincula are both ruptured, leading to compromised tendon nutrition. These injuries have a worse prognosis if not diagnosed and treated within 7–10 days as the tendon contracts and becomes less viable. Type II injury is the most common type. The tendon retracts to the level of the PIPJ, preserving the long vinculum and retaining more of its blood supply (Fig. 7). Due to maintenance of tendon length and blood supply, type 2 injuries may be successfully repaired up to a few months following injury. In type III injuries, a large bony fragment is avulsed off the distal phalanx. The distal pulley prevents retraction beyond the middle phalanx [8].
Fig. 7.
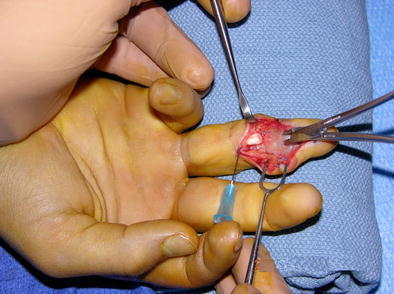
The avulsed tendon is seen to be retracted to the level of the PIP joint and proximal to the A4 pulley. This is the most common variant of jersey finger
Routine radiographic imaging will aid in ruling out concomitant osseous injuries and may reveal the location of tendon retraction if there is a bony avulsion. The use of MRI or ultrasound to confirm the diagnosis and aid in accurate preoperative localization has become more popular over the last several years [26, 27]. Accurate preoperative determination of the level of tendon retraction may limit intraoperative surprises and patient morbidity due to unnecessary dissection. Although uncommon, zone II or zone III intra-tendinous ruptures of the FDP mimic a jersey finger and have been well described (Fig. 8) [28].
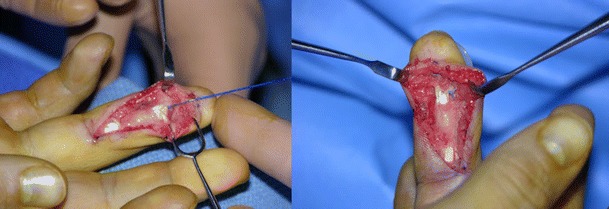
Fig. 8.

This patient was diagnosed intra-operatively with a zone III intra-tendinous FDP rupture. He presented clinically with inability to actively flex the DIPJ. Jersey finger was suspected and dissection proceeded from the DIPJ proximally until the site of rupture was identified. Preoperative imaging with ultrasound or MRI may have localized the site of rupture and limited unnecessary dissection
Over the last several years, Lalonde has published extensively on the benefits of wide-awake flexor tendon surgery and popularized this technique, particularly in zone I and zone II flexor tendon injuries [29••]. Lalonde describes the use of lidocaine with epinephrine and no tourniquet to obtain a bloodless field. At the conclusion of the repair, the patient is asked to actively flex the repaired tendon. Active flexion offers the optimal method of intrasurgical inspection and the best understanding of translation, gliding, and tension [29••].
A number of surgical techniques are used to treat avulsion injuries of the FDP, including the following: (1) the Bunnell pull-out suture technique [30], (2) suture anchor repair, and (3) repair of the tendon with incorporation of the volar plate. The latter is the most recent of the described techniques, and clinical outcome studies are still in development [31, 32•].
The pull-out suture procedure has traditionally been the most commonly used technique. A Bunnell stitch is initially passed through the tendon. The tendon is then attached to the distal phalanx by passing the suture through the distal phalanx with Keith needles, and tying the sutures over a button on the dorsum of the finger, usually over the nail plate (Fig. 9). The disadvantages include susceptibility to infections and skin necrosis, as well as nail bed injury.
Fig. 9.
The pull-out suture technique is depicted in this figure. The tendon is initially sutured with a Bunnell stitch and passed through the A4 pulley and then attached to the distal phalanx and tied to a dorsal button
The use of a suture anchor is desirable because it avoids the problems associated with a pullout suture. However, suture anchors have their own unique risks. For example, the anchor may cause nail bed problems and joint penetration, not to mention the additional cost. Suture anchor failure in laboratory studies has been attributed to suture breakage or anchor pull-out in elderly cadaveric bone, echoing the importance of healthy bone for a strong bone-implant construct [33, 34]. Importantly, laboratory studies have found that incorporation of the volar plate into a suture anchor tendon repair significantly decreases repair gapping and increases the load to failure [35•].
Recently Al-Qattan described a technique where the avulsed profundus tendon is reattached to the distal phalanx by repairing it to a distally based volar plate flap in an end-to-end fashion [32•]. The advantages of this technique include its relative simplicity and the strength of the repair. Despite theoretical concerns about hyperextension instability of the DIPJ, the early clinical results indicate otherwise. This may be due to the stability offered by the preserved collateral ligaments and the new volar soft tissue buttress incorporating the flexor tendon [32•].
Injuries that present 4 to 6 weeks following injury are considered chronic. Similar to chronic mallet injuries, the treatment is often guided by a combination of patient factors and technical considerations. Delayed primary repair may be possible, in particular for type II or III injuries. If the DIPJ is supple, and the patient’s main concern is loss of dexterity, staged FDP reconstruction may be a reasonable option. DIPJ arthrodesis may be used to treat a painful or unstable joint. FDP repair is not necessary for all patients with Jersey finger, and the surgeon must remember that some patients can function well with a sublimis only finger for interphalangeal joint flexion and no active flexion at the DIPJ.
Other complications associated with zone I flexor tendon repairs include adhesion formation, joint contracture, and quadriga. The quadriga phenomenon occurs when distal advancement of a contracted FDP tendon causes inability of the adjacent digits to fully flex at the DIPJ. With the popularization of wide-awake flexor tendon surgery and direct assessment of tension after repair, the frequency of this complication is expected to decrease.
Return to play
Athletes can expect 8–12 weeks of loss of play following surgical treatment. Generally, patients are allowed to return to sport once they have demonstrated functional active range of motion, minimal to no pain, and a grip strength greater than 80% relative to the uninjured side. The assistance of a hand therapist in tailoring a sport-specific rehabilitation program will allow the surgeon to more confidently release the athlete back to play.
Author’s preferred treatment
The authors prefer the pull-out suture technique. Despite its inherent risks, excellent outcomes are obtainable when the surgical technique and post-operative rehabilitation are executed appropriately (Fig. 10).
Fig. 10.
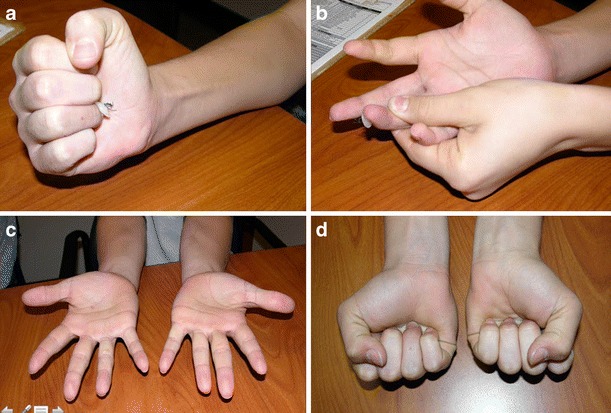
Care must be taken at all times to avoid damaging the germinal matrix with the Keith needles and pullout suture. This patient was able to regain nearly full active flexion following repair by 2 (a, b). Full flexion and extension demonstrated 6 months after surgery (c, d)
Non-surgical treatment is reserved for chronic injuries or in athletes unwilling or unable to comply with a strenuous postoperative rehabilitation regimen.
Conclusion
Multiple technical, patient-related, and sports-related factors must be considered during the management of injured athletes, with the aim of early, yet safe return to play. Most mallet finger injuries will heal with non-operative treatment over a period of 8–12 weeks, even when treatment is delayed up to 3–4 months.
Over the last several years, improvements in soft-tissue imaging and the popularization of wide-awake flexor tendon surgery have been beneficial to the management of jersey finger injuries. Furthermore, newer surgical techniques including suture anchor repair and tendon repair with volar plate augmentation have demonstrated encouraging laboratory findings. An acute diagnosis of jersey finger, however, requires surgical treatment and generally means 8–12 weeks of inability to compete in most contact sports.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Hand and Wrist Sports Medicine
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Ootes D, Lambers KT, Ring DC. The epidemiology of upper extremity injuries presenting to the emergency department in the United States. Hand (N Y) 2012;7:18–22. doi: 10.1007/s11552-011-9383-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hume MC, Gellman H, McKellop H, Brumfield RH., Jr Functional range of motion of the joints of the hand. J Hand Surg [Am] 1990;15:240–3. doi: 10.1016/0363-5023(90)90102-W. [DOI] [PubMed] [Google Scholar]
- 3.Shrewsbury MM, Johnson RK. Ligaments of the distal interphalangeal joint and the mallet position. J Hand Surg [Am] 1980;5:214–6. doi: 10.1016/S0363-5023(80)80004-9. [DOI] [PubMed] [Google Scholar]
- 4.Schneider LH. Fractures of the distal interphalangeal joint. Hand Clin. 1994;10:277–85. [PubMed] [Google Scholar]
- 5.Lubahn JD, Hood JM. Fractures of the distal interphalangeal joint. Clin Orthop Relat Res. 1996;327:12–20. doi: 10.1097/00003086-199606000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Shum C, Bruno RJ, Ristic S, Rosenwasser MP, Strauch RJ. Examination of the anatomic relationship of the proximal germinal nail matrix to the extensor tendon insertion. J Hand Surg [Am] 2000;25:1114–7. doi: 10.1053/jhsu.2000.17865. [DOI] [PubMed] [Google Scholar]
- 7.Katzman BM, Klein DM, Mesa J, Geller J, Caligiuri DA. Immobilization of the mallet finger. Effects on the extensor tendon. J Hand Surg (Br) 1999;24:80–4. doi: 10.1016/S0266-7681(99)90041-4. [DOI] [PubMed] [Google Scholar]
- 8.Leddy JP, Packer JW. Avulsion of the profundus tendon insertion in athletes. J Hand Surg [Am] 1977;2:66–9. doi: 10.1016/S0363-5023(77)80012-9. [DOI] [PubMed] [Google Scholar]
- 9.Lange RH, Engber WD. Hyperextension mallet finger. Orthopedics. 1983;6:1426–31. doi: 10.3928/0147-7447-19831101-10. [DOI] [PubMed] [Google Scholar]
- 10.Seymour N. Juxta-epiphysial fracture of the terminal phalanx of the finger. J Bone Joint Surg (Br) 1966;48:347–9. [PubMed] [Google Scholar]
- 11.Doyle J. Extensor tendons-acute injuries. In: Green D, editor. Green’s operative hand surgery. 2. New York: Churchill Livingstone; 1993. [Google Scholar]
- 12.Wehbé MA, Schneider LH. Mallet fractures. J Bone Joint Surg Am. 1984;66:658–69. doi: 10.2106/00004623-198466050-00003. [DOI] [PubMed] [Google Scholar]
- 13.Burton RI. Extensor tendons—late reconstruction. In: Green DP, editor. Operative hand surgery. New York: Churchill Livingstone; 1988. [Google Scholar]
- 14.Bendre AA, Hartigan BJ, Kalainov DM. Mallet finger. J Am Acad Orthop Surg. 2005;13:336–44. doi: 10.5435/00124635-200509000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Altan E, Alp NB, Baser R, Yalçın L. Soft-tissue mallet injuries: a comparison of early and delayed treatment. J Hand Surg [Am] 2014;39:1982–5. doi: 10.1016/j.jhsa.2014.06.140. [DOI] [PubMed] [Google Scholar]
- 16.Kalainov DM, Hoepfner PE, Hartigan BJ, Carroll C, 4th, Genuario J. Nonsurgical treatment of closed mallet finger fractures. J Hand Surg [Am] 2005;30:580–6. doi: 10.1016/j.jhsa.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 17.Garberman SF, Diao E, Peimer CA. Mallet finger: results of early versus delayed closed treatment. J Hand Surg [Am] 1994;19:850–2. doi: 10.1016/0363-5023(94)90200-3. [DOI] [PubMed] [Google Scholar]
- 18.Lubahn JD. Mallet finger fractures: a comparison of open and closed technique. J Hand Surg [Am] 1989;14(2 Pt 2):394–6. doi: 10.1016/0363-5023(89)90121-4. [DOI] [PubMed] [Google Scholar]
- 19.Ishiguro T, Itoh Y, Yabe Y, Hashizume N. Extension block with Kirschner wire for fracture dislocation of the distal interphalangeal joint. Tech Hand Up Extrem Surg. 1997;1:95–102. doi: 10.1097/00130911-199706000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Tuttle HG, Olvey SP, Stern PJ. Tendon avulsion injuries of the distal phalanx. Clin Orthop Relat Res. 2006;445:157–68. doi: 10.1097/01.blo.0000205903.51727.62. [DOI] [PubMed] [Google Scholar]
- 21.Hofmeister EP, Mazurek MT, Shin AY, Bishop AT. Extension block pinning for large mallet fractures. J Hand Surg [Am] 2003;28:453–9. doi: 10.1053/jhsu.2003.50089. [DOI] [PubMed] [Google Scholar]
- 22.Toker S, Türkmen F, Pekince O, Korucu İ, Karalezli N. Extension block pinning versus hook plate fixation for treatment of mallet fractures. J Hand Surg [Am] 2015;40:1591–6. doi: 10.1016/j.jhsa.2015.04.027. [DOI] [PubMed] [Google Scholar]
- 23.Suh N, Wolfe SW. Soft tissue mallet finger injuries with delayed treatment. J Hand Surg [Am] 2013;38:1803–5. doi: 10.1016/j.jhsa.2013.03.050. [DOI] [PubMed] [Google Scholar]
- 24.Kleinert HE, Verdan C. Report of the committee on tendon injuries (International Federation of Societies for Surgery of the Hand) J Hand Surg [Am] 1983;8(5 Pt 2):794–8. doi: 10.1016/S0363-5023(83)80275-5. [DOI] [PubMed] [Google Scholar]
- 25.Lunn PG, Lamb DW. “Rugby finger”—avulsion of profundus of ring finger. J Hand Surg (Br) 1984;9:69–71. doi: 10.1016/0266-7681(84)90020-2. [DOI] [PubMed] [Google Scholar]
- 26.Goodson A, Morgan M, Rajeswaran G, Lee J, Katsarma E. Current management of Jersey finger in rugby players: case series and literature review. Hand Surg. 2010;15(2):103–7. doi: 10.1142/S0218810410004710. [DOI] [PubMed] [Google Scholar]
- 27.Cockenpot E, Lefebvre G, Demondion X, Chantelot C, Cotten A. Imaging of sports-related hand and wrist injuries: sports imaging series. Radiology. 2016;279:674–92. doi: 10.1148/radiol.2016150995. [DOI] [PubMed] [Google Scholar]
- 28.Bois AJ, Johnston G, Classen D. Spontaneous flexor tendon ruptures of the hand: case series and review of the literature. J Hand Surg [Am] 2007;32:1061–71. doi: 10.1016/j.jhsa.2007.06.012. [DOI] [PubMed] [Google Scholar]
- 29.Lalonde DH, Martin AL. Wide-awake flexor tendon repair and early tendon mobilization in zones 1 and 2. Hand Clin. 2013;29:207–13. doi: 10.1016/j.hcl.2013.02.009. [DOI] [PubMed] [Google Scholar]
- 30.Bunnell S. Surgery of the hand. 3. Philadelphia: JB Lippincott; 1948. [Google Scholar]
- 31.Al-Qattan MM, Al-Turaiki TM, Al-Zahrani AY, Al-Harbi MS, Al-Kahtani FS. A new technique of flexor profundus repair in the distal part of zone I: inclusion of the palmar plate. J Hand Surg Eur Vol. 2010;35:459–63. doi: 10.1177/1753193410365631. [DOI] [PubMed] [Google Scholar]
- 32.Al-Qattan MM. Use of the volar plate of the distal interphalangeal joint as a distally based flap in flexor tendon surgery. J Hand Surg [Am] 2016;41:287–90. doi: 10.1016/j.jhsa.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 33.Chu JY, Chen T, Awad HA, Elfar J, Hammert WC. Comparison of an all-inside suture technique with traditional pull-out suture and suture anchor repair techniques for flexor digitorum profundus attachment to bone. J Hand Surg [Am] 2013;38:1084–90. doi: 10.1016/j.jhsa.2013.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Halát G, Negrin L, Koch T, Erhart J, Platzer P, Hajdu S, et al. Biomechanical characteristics of suture anchor implants for flexor digitorum profundus repair. J Hand Surg [Am] 2014;39:256–61. doi: 10.1016/j.jhsa.2013.11.023. [DOI] [PubMed] [Google Scholar]
- 35.Brar R, Owen JR, Melikian R, Gaston RG, Wayne JS, Isaacs JE. Reattachment of flexor digitorum profundus avulsion: biomechanical performance of 3 techniques. J Hand Surg [Am] 2014;39:2214–9. doi: 10.1016/j.jhsa.2014.07.054. [DOI] [PubMed] [Google Scholar]


