Abstract
Veterans from conflicts such as the wars in Iraq and Afghanistan commonly return with behavioral health problems, including Post-Traumatic Stress Disorder (PTSD) and hazardous or harmful substance use. Unfortunately, many veterans experience significant barriers to receiving evidence-based treatment, including poor treatment motivation, concerns about stigma, and lack of access to appropriate care. To address this need, the current study developed and evaluated a web-based self-management intervention based on cognitive behavioral therapy (CBT), targeting PTSD symptoms and hazardous substance use in a group of symptomatic combat veterans enrolled in VA primary care. Veterans with PTSD/subthreshold PTSD and hazardous substance use were randomized to primary care treatment as usual (TAU; n=81) or to TAU plus a web-based CBT intervention called Thinking Forward (n=81). Thinking Forward consisted of 24 sections (approximately 20 minutes each), accessible over 12 weeks. Participants completed baseline and 4-, 8-, 12-, 16- and 24-week follow-up assessments. Three primary outcomes of PTSD, alcohol and other drug use, and quality of life were examined. Significant treatment effects were found for heavy drinking, but not for PTSD or quality of life. The effect of the intervention on heavy drinking was mediated by intervening increases in coping, social support, self-efficacy, and hope for the future. These results demonstrate the promise of a web-based, self-management intervention for difficult-to-engage OEF/OIF veterans with behavioral health and substance use concerns.
Keywords: technology, intervention, veterans, PTSD, alcohol, substance abuse, CBT
Introduction
Over 2.5 million US soldiers have served in military efforts in or near Afghanistan (Operation Enduring Freedom; OEF) or Iraq (Operation Iraqi Freedom; OIF; Operation New Dawn, OND). Often, soldiers experience significant stressors during deployment that result in mental health or substance use problems. In fact, over two thirds (69%) of OEF/OIF veterans seeking services at Veterans’ Administration (VA) medical centers screened positive for a behavioral health problem (Seal et al., 2009), with over half (53%) of OEF/OIF veterans screening positive for PTSD (Helmer et al., 2009) and 23-27% screening positive for hazardous alcohol use (Jakupcak, et al., 2008; McDevitt-Murphy et al., 2010). Rates of comorbidity are high in OEF/OIF veterans; 63% of recent combat veterans with alcohol use disorder also have PTSD (Seal et al., 2010). Drug misuse (particularly opioids), depression, and chronic pain also are elevated among OEF/OIF veterans (Helmer et al., 2009; Seal et al., 2009). Further, the presence of these behavioral health concerns is associated with significant impairment in multiple areas, including increased suicide risk, poorer psychosocial functioning, poorer physical health, and poorer work productivity, all of which are associated with significant public health costs (Hoge, et al., 2007; Jakupcak et al., 2008; McDevitt-Murphy et al., 2010).
The high comorbidity of PTSD and hazardous substance use in OEF/OIF veterans is complicated by their reciprocal effect on each other. Individuals may self-medicate PTSD symptoms and hazardous alcohol or other drug use may place individuals at higher risk for exposure to trauma, hinder their ability to process or resolve trauma, or exacerbate certain PTSD symptoms (Jacobsen, Southwick, & Kosten, 2001; Khantzian, 1997). Given the complexity of the relationship between PTSD and substance use and the high levels of comorbidity, integrated treatment approaches are indicated. In addition, a large portion of veterans with comorbid PTSD and substance use disorders (SUD) report that they would prefer an integrated, rather than a sequential or separate, treatment approach (Back, Brady, Jaanimagi, & Jackson, 2006). Several face-to-face integrated approaches have been developed and tested, with some positive results (see McCauley, et al., 2012; McGovern, et al., 2011; Prins, Cimpean, & Schnurr, 2009) for a review.
An additional challenge in providing treatment for co-occurring PTSD and hazardous substance use is that many OEF/OIF veterans do not seek behavioral health treatment: only half who screened positive for PTSD and 18% who screened positive for hazardous alcohol use report using any type of behavioral health treatment (Erbes, Westermeyer, Engdahl, & Johnsen, 2007). Veterans have identified many treatment barriers, including poor confidence in treatment effectiveness, fear of increasing symptoms, stigma, practical barriers (e.g., transportation, treatment availability), and avoidance symptoms characteristic of PTSD (Hoge et al., 2004; Pietrzak, et al., 2009b; Stecker, McGovern, & Herr, 2012).
Two strategies to help engage veterans in care are to provide behavioral health services within easy to access settings, such as primary care, and to use technology to allow veterans to engage outside of formal treatment settings. Veterans with mental health problems often present in primary care clinics for routine care providing an opportunity for intervention at this level of care (Zlotnick et al., 2004). Technology-delivered interventions have demonstrated feasibility and are acceptable within a variety of populations, including those with PTSD, hazardous substance use, and military personnel (Grubaugh, et al., 2008; Marsch, 2011; Wilson, et al., 2008). Developing novel treatments that can be delivered remotely may be of particular importance in addressing PTSD, as individuals with this diagnosis may be more likely to reside in more remote, less populated areas in order to reduce overstimulation, hyperarousal, and interpersonal conflict (Morland, Frueh, Pierce, & Miyahira, 2003). Computer-delivered CBT interventions to target PTSD (Klein et al., 2010; Roy-Byrne et al., 2010) and SUD (Bickel, Marsch, Buchhalter, & Badger, 2008; Carroll et al., 2009) have been found to be efficacious, including interventions targeting hazardous alcohol use (Riper et al., 2011) and PTSD (Litz et al., 2007) among veterans.
One published study reported on an 8-session, web-based CBT intervention for veterans who reported hazardous drinking; Brief and colleagues (2013) reported that participants in the VetChange intervention showed significant decreases in self-reported drinking and PTSD symptoms. Although the Brief et al. study suggests that a web-based CBT intervention holds promise for veterans with hazardous substance use and PTSD, it is important to note that the VetChange intervention targeted hazardous drinking in veterans and did not specifically address PTSD, either for inclusion in the study or in the intervention content, whereas the current intervention is meant to fill the need for an integrated treatment of hazardous alcohol and other drug use and PTSD symptoms among OEF/OIF veterans. In addition, Brief et al. recruited participants from the internet and relied solely on online self-report assessments for data collection, while the current study used rigorous in-person interviews for data collection (including self-reports from collaterals as a validity check) and recruited non-treatment seeking persons with clinically elevated levels of PTSD and substance use from primary care settings.
The primary aim of this clinical trial was to test an intervention designed to increase access to and engagement in CBT, as well as deliver a reliable and low cost treatment that did not increase demand on providers’ time or training. A detailed description of our iterative development process involving both veteran and behavioral health clinician input has been reported (Possemato et al., 2015). Due to name overlap with another web-based program for veterans, we have changed the name of the program from “Coming Home and Moving Forward” to “Thinking Forward”. The current article describes the evaluation of the Thinking Forward intervention in a randomized clinical trial.
A secondary aim of our research was to investigate theorized mediators of treatment outcome. It was hypothesized that deficits in the ability to cope with life stress maintain hazardous alcohol and drug use and psychiatric symptoms. CBT teaches coping skills and aims to increase self-efficacy for positive coping, helping people more successfully manage stressors, including high-risk situations for substance use. The acquisition of coping skills and self-efficacy has often been shown to be mechanisms of change in CBT (Hendricks, Delucchi, & Hall, 2010; Litt, Kadden, Kabela-Cormier, & Petry, 2008), including one study that showed that coping mediated the effect of a computer-delivered CBT intervention on substance use outcomes (Kiluk, Nich, Babuscio, & Carroll, 2010). In addition to improving coping, CBT also focuses on restructuring dysfunctional cognitions (e.g., Beck, 1997). Research has shown that changes in dysfunctional cognitions mediate the effects of CBT on PTSD (Kleim et al., 2013; Muresan et al., 2012).
In addition to CBT-specific mediators, we also were interested in testing purported mechanisms of change, such as positive social support, hope for the future, readiness to change, and therapeutic alliance, that have been shown to correlate with treatment outcomes across a number of different treatment modalities targeting both substance use and psychiatric symptoms (e.g., Dunn, Deroo, & Rivara, 2001; Stein et al., 2009; Kaskutas, Bond, & Humphreys, 2002; Magura et al., 2003; Morgenstern, Labouvie, McCrady, Kahler, & Frey, 1997; Knaevelsrud & Maercker, 2007). One possible mediator that has recently received attention in treatments focused on combat veterans is resilience. Resilience is often defined as having the coping resources to thrive in the face of adversity. CBT is thought to foster resilience by teaching skills that enable emotional awareness and stability, positive social interactions, and effective coping strategies (Lee, Sudom, & Zamorski, 2013). Resilience has been found to mediate the association between post-deployment stressors and behavioral health outcomes (Wooten, 2012).
Given the existing theory and research described above, we selected several variables to test as potential mediators of our novel intervention. Coping responses and self-efficacy were selected based on our use of core CBT strategies, including cognitive restructuring, functional analysis of substance use, and problem solving. Thinking Forward also has a specific focus on readiness for change (module 2) and social support (Communicating with Others Module and Preventing Stress from Ruining Relationships Module). Additionally, hope for the future and resilience were selected as potential mediators, consistent with the overarching theme of Thinking Forward being a strength-based approach focused on healthy re-integration, and therapeutic alliance has been shown to mediate the effects of a variety of interventions (Maisto, et al., 2015).
Method
Participants
The trial was registered at ClinicalTrials.gov (NCT01710943) and was approved by the Syracuse VAMC, Western New York VAMC, Syracuse University, and National Development Research Institutes Institutional Review Boards. Veterans (N= 162) were recruited from primary care clinics in four VA facilities. To be included in the trial, participants needed to be OEF/OIF/OND veterans; report hazardous alcohol on the AUDIT (score ≥ 8 for men, ≥ 7 for woman; Babor, Higgins-Biddle, Saunders, & Monteiro, 2001) or substance misuse on the DAST-10 (score ≥ 2; Skinner, 1982); and report symptoms consistent with at least subthreshold PTSD (a military-related traumatic life event plus, at least, 1 re-experiencing symptom, 3 avoidance symptoms or 2 hyperarousal symptoms) on the Clinician Administered PTSD Scale (Blake et al., 1995). Participants who were currently receiving psychotherapy for PTSD or had incurred a change in dose or type of a psychiatric medication that treats PTSD or a substance use disorder in the last two months were excluded from participation. Also, veterans in need of inpatient substance detoxification, who had a plan to harm themselves, or who had documentation of a psychotic disorder or moderate to severe traumatic brain injury in their VA medical chart were excluded.
Veterans were referred to the study by primary care providers or OEF/OIF/OND case managers. Referrals were facilitated by a case-finding protocol: using the electronic medical records, study staff generated lists of OEF/OIF/OND veterans who had screened positive on the standard screens delivered in VA primary care for hazardous alcohol use and PTSD (i.e., Audit-C and PC-PTSD). Research staff asked primary care providers to refer patients who screened positive. Referred patients were sent a letter in the mail introducing the study then telephoned and screened for combat stress reactions and current substance use. Recruitment letters and phone screens described the treatment as focusing on PTSD symptoms and hazardous substance use. Interested veterans were invited to come their local VA to complete the baseline interview.
Procedure
At the baseline interview, informed consent was administered. Then, participants were assessed for suicidality, hazardous alcohol or other drug use, and PTSD symptoms to determine eligibility. Eligible participants then completed the rest of the baseline assessment (described next) and were randomly assigned to Treatment as Usual (TAU) or TAU plus Thinking Forward. Permuted-block randomization was used to randomize participants based on whether or not they met DSM-IV criteria for a current alcohol or other drug abuse or dependence (as measured by the MINI) and diagnostic or subthreshold PTSD (as measured by the CAPS). Participants were assessed at baseline, weeks 4, 8 and 12 during the active intervention phase, and at 16 and 24 weeks (i.e., 1 and 3 month post-intervention follow-ups). Participants were compensated for the time they spent completing assessments at a rate of approximately $25/ hour and could earn up to $290 for completing all assessments. Participants were not compensated for completing treatment modules.
Measures
Four measures were used to assess eligibility and baseline health status. The Clinical Administered PTSD Scale (CAPS) assessed the 17 core symptoms of PTSD as defined in the DSM-IV in an interview format (Blake et al., 1995). Each symptom was scored separately on a five-point scale for frequency and intensity. A rating of at least 1 for frequency and 2 for intensity of PTSD symptoms on the CAPS were defined as “endorsed”. The CAPS is reliable and has excellent diagnostic utility compared to the SCID PTSD module. This measure was used to verify the presence of a criterion A traumatic event and document rates of full and subthreshold PTSD. Subthreshold PTSD was defined as meeting DSM-IV criterion B (re-experiencing) and either criterion C (avoidance) or criterion D (arousal), plus meeting criterion E (duration) and F (functional impairment; Schnurr, Lunney, Sengupta, & Spiro, 2005). All interviewers were trained and received in-person supervision from a licensed clinical psychologist for every baseline CAPS interview. In supervision, endorsed symptoms and item ratings were discussed and interview ratings were changed if the original rating was considered to be not accurate by the supervisor. Because of this supervisor consensus method, inter-rater reliability ratings were not conducted for this study. The Alcohol Use Disorders Identification Test (AUDIT; (Babor et al., 2001) screened for hazardous alcohol use at baseline. Patients had to score 8 or higher for men and 7 or higher for women to be eligible for inclusion in the trial. The AUDIT is reliable, valid, and had acceptable internal consistency in this study (α=.75). The Drug Abuse Screening Test-10 (DAST-10; (Skinner, 1982) was used to determine if patients met criteria for hazardous drug use at baseline as defined by a score of 2 or higher. The DAST-10 discriminates between persons with or without drug use disorders and has acceptable internal consistency in this study (α=.73). The MINI International Neuropsychiatric Interview (MINI) assessed for DSM-IV substance use disorders and was administered in a computerized, self-report format. The MINI has comparable validity to well-established structured clinical interviews (Sheehan, 2004).
Three measures were used to assess the primary study outcomes and were administered at each time point. The Timeline Follow-Back (TLFB) interview assessed self-reported substance use using calendars to record past daily alcohol use in standardized drink quantities and use of other drugs (e.g., cocaine, opiates, cannabis) for the previous 90 days at baseline and since the last assessment at follow-ups. Primary outcomes derived were percent of drinking days, percent of heavy drinking days, and percent of drug use days. “Heavy” drinking was defined according to U.S. National Institute on Alcohol Abuse and Alcoholism criteria of 4 or more standard drinks on an occasion for women and 5 or more for men, with a standard drink defined as a beverage containing the equivalent of .6 ounce of pure alcohol. The primary alcohol outcomes of frequency of alcohol use and the frequency of heavy use are based on the reasoning that both of these dimensions, which tend to be weakly correlated, when combined predict the occurrence of alcohol-related problems (Babor, Longabaugh, Zweben, Fuller, Stout, Anton, & Randall, 1994; Project MATCH Research Group, 1998). The TLFB has good psychometric properties, including test-retest reliability and high content, criterion, and construct validity across multiple related measures (Sobell & Sobell, 2000). Participants were asked to provide a collateral informant who was contacted once by phone to provide information about past daily alcohol and other drug use over the previous month. Collaterals were randomly assigned to be contacted at baseline or one of the follow-up points. These data were compared to the participants’ self-report of past alcohol and other drug use. The PTSD Checklist- Military (PCL-M) asked respondents to self-report how much they have been bothered by 17 PTSD symptoms in the past month on a 5-point scale. The PCL-M is reliable, valid, (Weathers, 1996) and had good internal consistency in this study (α=.76). The total score was used as the primary PTSD outcome. The WHOQOL-BREF was used to measure quality of life, life satisfaction, and personal well-being with 26-items assessing the broad domains of physical health, psychological health, social relationships and environmental factors (e.g., finances, safety) (Murphy, Herrman, Hawthorne, Pinzone, & Evert, 2000). This measure is reliable, valid, and has good internal consistency in this study (α=.85). The domain scores were used as the QOL outcome measures.
Several self-report measures were administered at pre and post treatment. Changes scores for each measure were computed as mediators of treatment outcome. The Coping Strategies Scale (CSS) – Brief Version (Litt, Kadden, Cooney, & Kabela, 2003) assesses change processes and skills taught in coping-skills treatment, such as problem solving and dealing with urges to use substances. Twenty-three items are rated on a 4-point scale for how often each strategy is used to help avoid substance use. This measure has good predictive validity, as total coping skills has been found to be related to reduced drinking (Litt et al., 2003) and good internal consistently reliability in this sample (.87). The total coping scale was used in this study. Medical Outcomes Study Social Support Scale (MOS-SSS) measures how often specific types of social support are available to participants, with 19 items rated on a 5-point scale. The measure has construct validity (Sherbourne & Stewart, 1991) and high internal consistency reliability in this sample (.96). The Brief Situational Confidence Questionnaire (BSCQ) (Breslin, Sobell, Sobell, & Agrawal, 2000) measures self-efficacy, that is how confident participants are in their ability to resist heavy drinking across eight high-risk situations on a 0% to 100% scale. The questionnaire has good test-retest reliability (Condiotte & Lichtenstein, 1981) and had good internal consistency reliability in our sample (.90). The Future Scale (Hellstrom, Jansson, & Carlsson, 1999) measures expectations about the future on two scales (Explicit and Implicit, 5-items each, rated on 7-point scales) representing the degree that the future is perceived to be comprehensible, manageable, and meaningful. Hellstrom, Jansson, and Carlsson (2000) found an internal consistency of 0.80 for the full Future Scale and the reliability (Cronbach's α) for each subscale was 0.52 and 0.75, respectively. The current study examined only the Explicit Future Scale. Readiness to Change Questionnaire (RTCQ) is a 12-item questionnaire for assignment of hazardous drinkers to pre-contemplation, contemplation, or action stages (Rollnick, Heather, Gold, & Hall, 1992). The measure has good predictive validity with drinking outcomes and adequate internal consistency reliability (.66) in the current sample. The Connor-Davidson Resilience Scale (CD-RISC) measures resiliency, with 25 items rated on a 5-point scale. The scale has high test-retest reliability, convergent validity, and discriminant validity (Connor & Davidson, 2003). Internal consistency reliability in this sample was good at .88.
Intervention
Treatment as Usual (TAU) consisted of the usual VA primary care services, including medical, behavioral health, pharmacy, weight management and social work services. Behavioral health providers are integrated into the primary care team to provide consultation to medical staff and brief assessment and interventions to referred patients. Treatment utilization among the participants was quite low overall, so we compared treatment visits and prescribed psychiatric medications for participants in the web-based intervention group to visits and medications for participants in TAU across the 24-week study period. On average, participants received less than one primary care visit, slightly more than one mental health visit, and less than one psychiatric medication. The experimental and control conditions did not significantly differ in the amount of care they received. Table A1 is a summary of the number of primary care and mental health visits and psychiatric medications participants received as part of treatment as usual during their six months of active study participation.
TAU Plus Thinking Forward
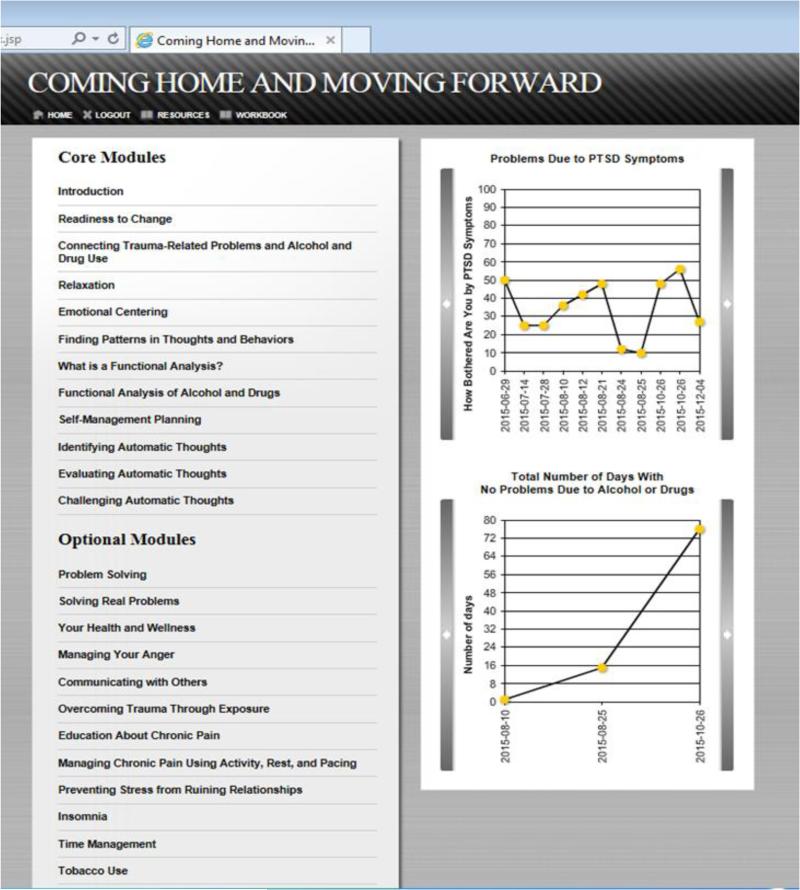
Participants randomized to the enhanced condition were shown how to access the Thinking Forward web-based program at the end of the baseline assessment session. The program was self-directed, with the first module teaching participants how to use it. The program contained 24 modules housed within a homepage (Figure 1). Modules were self-paced, with each module taking approximately 20 minutes to complete. Participants were asked to complete the 12 “core modules” in the first six weeks of treatment then to re-visit important modules and complete additional modules of their choice during weeks 7-12. Modules included interactive exercises and veteran stories that illustrate common symptoms and coping strategies. They were designed to teach a variety of cognitive behavioral skills, such as identifying, evaluating and challenging negative automatic thoughts related to PTSD symptoms and doing a functional analysis of problematic alcohol or other drug use. Relaxation and emotional centering modules were included to provide specific skills for managing trauma-related distress. Other modules, although not specific to trauma, drew connections between trauma and conditions such as insomnia, pain, and communications problems, and used examples of veterans with PTSD symptoms. Also, included in the program are recurring queries assessing problematic substance use and trauma symptoms, graphs showing progress made in these areas, a printable workbook containing key points and fillable copies of exercises from each program modules, and a resources page see Possemato et al. (2015) for more detail). Participants accessed the program using a unique login and password. Modules were typically completed at home but participants could opt to complete them in a private room at their local VA. The program also had a back-end system, which allowed research staff to track module completion. Participants who did not complete at least one module per week were contacted by research staff once per week for the first 4 weeks and twice per month for weeks 5-12. Participants were prompted to engage in the treatment via phone calls, text messages, and in-person reminders when they were meeting with research staff to complete study assessments. In an attempt to increase participants’ use of the modules, this strategy was changed after enrolling 24 participants to add a daily reminder call for the first three days to complete the first module.
Figure 1.
Web-based CBT homepage and list of program sections/modules
Analytic Plan
Treatment groups were compared for differences on demographic and other baseline characteristics using bivariate correlations, Wilcoxon Rank Sum Tests for non-normal variables, and chi-square tests for categorical measures. Baseline characteristics examined as potential covariates included age, gender, race, ethnicity, education, employment, and combat experiences. One baseline covariate, post-deployment life events was significantly different between treatment conditions and related to most of the outcomes, thus this covariate was included in both primary and mediation analyses as a control. Analyses included all randomized participants independent of early dropout, consistent with an intent-to-treat approach, and were performed using SAS statistical software.
To assess the intervention effects observed during the treatment period (baseline, 4, 8 and 12 weeks), and the durability or emergence of effects during 1- and 3-month post-intervention follow-up period, we used generalized mixed-effects piecewise regression models. Intervention type (Thinking Forward vs. TAU), two time variables (time 1 - effect of time during the treatment period, time 2 – effect of time during the post-intervention period), and their interaction terms (intervention condition-by-time 1 and intervention condition-by-time 2) were specified for the model. Significant time effects reflect an improvement for all participants on average, and significant interactions reflect an intervention effect (positive changes over time for participants in Thinking Forward relative to TAU). Random intercept and slope were included to account for across time correlations due to repeated measurements. Analyses were conducted with SAS PROC GLIMMIX (SAS Institute Inc., 2015). The current study attempted to address two empirical questions: 1) whether the intervention changed outcomes during the intervention period (baseline to 12 weeks); and 2) whether intervention effects differed between the intervention period and the post-intervention period. Specifically, we were interested in examining potential emergent (i.e., sleeper), or diminishing treatment effects after the active treatment period had ended. Our piecewise model, though less traditional than a straight longitudinal model, allowed us to address these two questions within one modeling framework.
Our mediation analyses focused on outcomes for which we found significant intervention effects during the in-treatment period. Although a significant intervention effect is not a prerequisite for mediation analysis because it is possible for an entire intervention effect to be “transmitted” to the outcome indirectly (Hayes, 2013; MacKinnon, 2008), we did not find this to be the case in our preliminary analyses. Moreover, because there were no significant differences for outcomes that showed intervention effects when comparing the in-treatment to post-treatment periods, our mediation analyses were conducted only for outcomes during the 12 week in-treatment study period. Lastly, because not all putative mediators were assessed at all assessment points, change scores from baseline to 12 weeks for both outcomes and the mediators were used for mediation analysis. We conducted univariate mediation analysis to assess mediated effect individually then multivariable mediation analyses to evaluate mediated effects by all mediators collectively. Significance of the mediated effects was tested using bias-corrected bootstrapping confidence intervals due to an asymmetric distribution. We also inferred mediated effects by comparing “total effect” (treatment effect without mediators) with “direct effect” (intervention effect when mediators were included in the model). If a total effect was significant and a direct effect was non-significant when the mediator was entered into the model, we assumed that this was a demonstration of complete mediation. If the magnitude of effect was smaller for the direct effect than for the total effect, we considered this to be partial mediation (MacKinnon, 2008). All mediation analyses were conducted using a SAS macro suite “PROCESS” (Hayes, 2013).
Finally, chi-square analyses were conducted to examine rates of clinically significant change by treatment group in PTSD symptoms, as determined by a 10 point decrease in score from baseline to 12 week and baseline to 3 month follow-up (10 points is recommended as a minimum threshold for determining whether improvement is clinically meaningful using the PCL; Weathers et al., 2013) and by a change from clinically elevated score (≥50) to a non-clinically elevated score (Weather et al., 2013).
Results
Participant characteristics
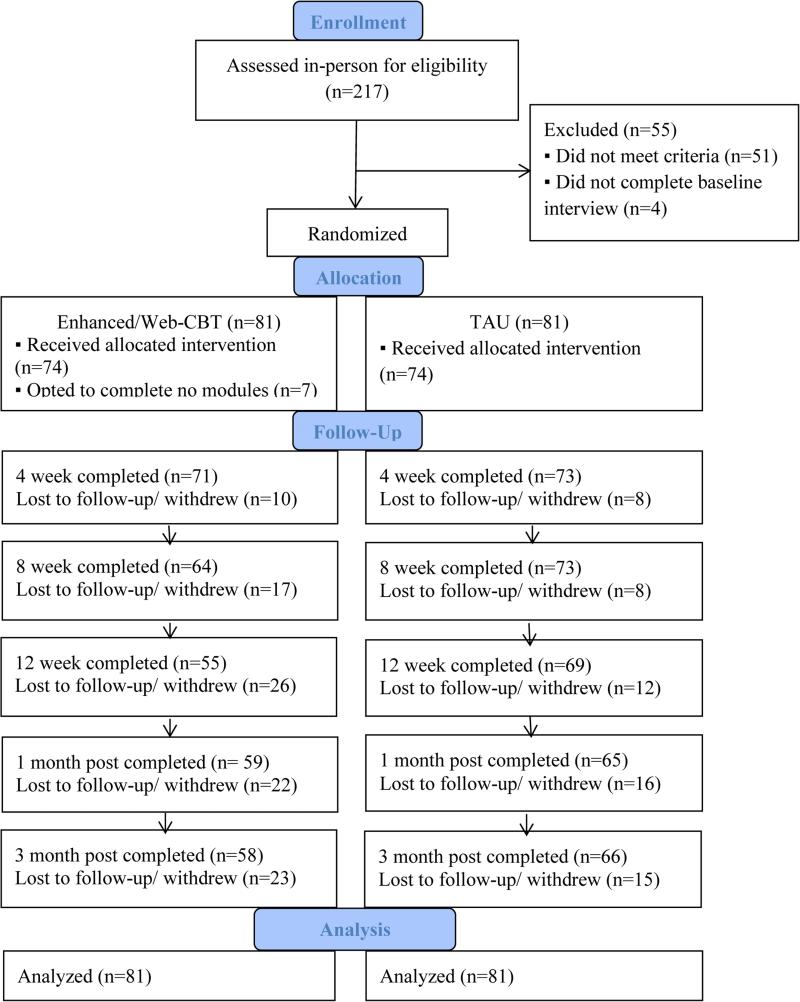
A total of 217 veterans were assessed in-person and, consistent with the proposed study protocol, 162 were randomized to either Web CBT (N=81) or TAU (N=81); see CONSORT Diagram for participant progress through the phases of the trial (Figure 2). The overwheming majority were male (93%) and identifed themselves as White (85%) and non-Hispanic (94%). Average age was 34 (SD 8.1, range=22-64). Slightly more than half (52%) had post-secondary education or a trade school certification; 55% reported they were receiving some type of disability and 62% were working full or part time. Almost half (n=78, 48%) met critiera for a current alcohol use disorder. Based on TLFB data the mean (SD) was 24% (SD = 25%) heavy drinking days, 2.79 (SD = 2.55) drinks/day, 47% (SD = 30%) drinking days, and 5.60 (SD = 3.46) drinks/drinking days, and 15% (SD = 31%) drug use days. Most participants (128, 79%) met criteria for diagnostic-level PTSD on the CAPS, with the remainder having subthrehsold PTSD symptoms. Means and SD for the major outcomes dervied from the TLFB, PCL, and WHO can be found in Table A2. There were no significant baseline differences between treatment conditions on any variable.
Figure 2.
CONSORT Flow Diagram
Thinking Forward intervention and feedback
Mean number of total modules completed was 8.8 (6.2). Participants provided intervention feedback on seven visual analog scales, ranging from 0 (poor) to 10 (excellent). Seventy-six percent of participants rated the intervention >5 for “interesting”, 82% for “useful”, 74% for “new information learned”, 67% for “clarified misconceptions about PTSD”, 62% for “clarified misconceptions about substance use”, 41% for “easy to understand” , and 89% for overall satisfication with the program. Over a third of participants (38.3%) completed all 11 core modules, which is consistent with other interventions of this type (e.g., Brief et al., 2013). A figure showing the percent of participants who accessed each module can be found in the online appendix (Figures A1 and A 2).
Collateral reports
Correlations between TLFB self-reports and collateral reports ranged from .57 (percent heavy drinking day) to .66 (percent drinking days) (all ps < .001). These correlations are consistent with other research in the field comparing TLFB to collateral reports (e.g., .42-.68 for DeMarce et al., 2007; .78-.89 for Fals-Stewart 2000). In addition, participants did not underestimate their drinking or drug use, compared to collateral reports. . Across all drinking outcomes, 36.9% of the patients reported more drinking, 23.0% reported the same amount of drinking, and 39.4% reported less drinking than their collateral contact. For percent of drug use days 5.1% reported more drug use, 83.1% reported the same amount of use, and 21.9% less drug use than their collaterals. Mean differences between participant and collateral reports were quite small, ranging from −1.87 (SD=26.45) for percent drinking days to .56 (SD=18.57) for heavy drinking, and the mean difference in estimated percentage of drug use days was 3.14 (SD=19.00).
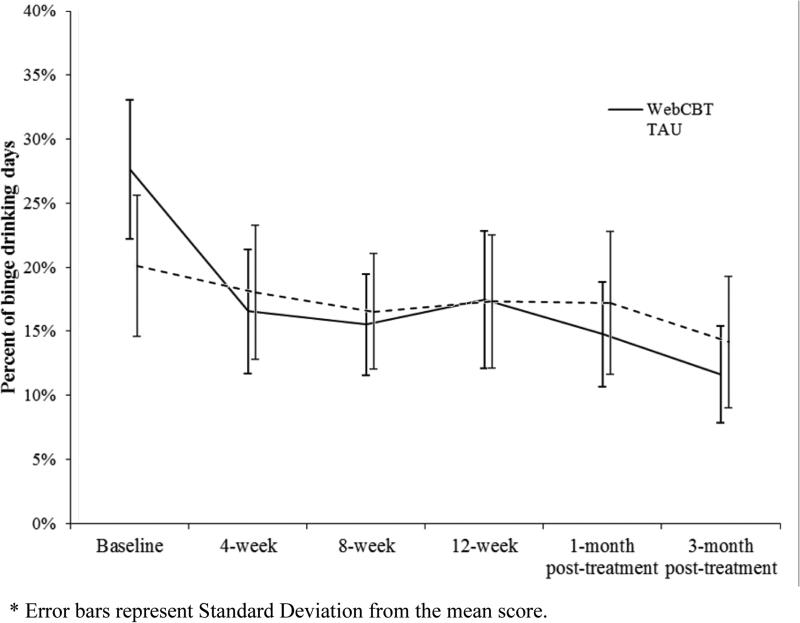
Substance use outcomes during intervention
Significant time effects were seen for both percent of drinking days and percent of heavy drinking days during the in-intervention period (Table 1). In addition, Thinking Forward participants reported significantly greater declines in percent of heavy drinking days compared to TAU participants (Figure 3). Effects were maintained in the post-intervention period, as evidenced by a lack of significant differences between the in- and post-intervention periods (Table 1). Thinking Forward participants showed a greater decline in percent drug use days compared to participants in TAU, but the difference did not reach statistical significance (as indicated by the treatment by time interactions) during the in- or post-treatment periods.
Table 1.
Results of the outcome analysis using generalized mixed-effects piecewise regression models
| In-treatment period | Contrast between in- and post-treatment periods | |||
|---|---|---|---|---|
| Treatment effect1 | Time Effect2 | Difference in treatment effect | Difference in time effect | |
| Estimate (s.e.) | Estimate (s.e.) | Estimate (s.e.) | Estimate (s.e.) | |
| Percent of drinking days | −0.93 (1.12) | −1.79 (0.56)** | 1.67 (1.84) | 0.11 (0.92) |
| Percent of heavy drinking days | −1.80 (0.79)* | −1.87 (0.40)** | 1.89 (1.33) | 1.22 (0.66) |
| Percent of drug use days | −0.27 (0.25) | −0.58 (0.12)** | −0.06 (0.49) | 0.27 (0.24) |
| PTSD severity – mean PCL score | −0.09 (0.50) | −1.57 (0.25)** | 0.40 (0.82) | 1.73 (0.41)** |
| QOL - Physical domain | 0.75 (0.52) | −0.16 (0.26) | −0.51 (0.91) | 0.45 (0.46) |
| QOL - Psychological domain | 0.77 (0.58) | 0.41 (0.29) | −0.88 (0.94) | −0.28 (0.47) |
| QOL - Social domain | 1.27 (1.02) | 2.47 (0.51)** | −2.00 (1.72) | −2.21 (0.86)* |
| QOL - Environment domain | 0.13 (0.61) | 0.94 (0.30)** | 0.15 (1.02) | −0.39 (0.51) |
Notes:
Treatment effect was indicated by treatment type by time interaction, that is, the difference between Thinking Forward and TAU in rate of improvement.
Time effect represents the outcome for all participants regardless of treatment condition.
s.e.= standard error
p<.05
p <.01.
Figure 3.
Percent heavy drinking days by treatment condtion
PTSD outcomes
There was no significant treatment by time effect for either of the two PTSD outcomes (change in PTSD severity and clinically significant change in PTSD symptoms). However, there were signifcant time effects, as all participants improved over time in PTSD severity during the in-treatment period but tended to reverse trend in the post-treatment period. compared to the in-treatment period. Regarding clinically significant change in PTSD symptoms, chi-square analyses did not reveal significant differences between treatment groups in the percent of participants who showed clinically meaningful improvement in PTSD symptoms on the PCL (i.e., ≥10-point decrease) at either 12 weeks (TAU 31.3% vs. intervention 41.0% improved) or 3 month follow-up (TAU 29.7% vs. intervention 37.5% improved). Chi-square analyses also did not show significant differences between treatment groups in the percentage of participants who moved from reporting clinically significant distress on the PCL (i.e., >50) to no longer reporting clinical levels of distress at 12 weeks (TAU 17.9% vs. intervention 22.2%) or 3 month follow up (TAU 23.4% vs. intervention 17.9%).
Qualty of life outcomes
For QOL, all particpants reported significant improvements in the social and environmental domains during the treatment period, but improvement in social QOL significantly slowed down during the post-treatment period (Table 1). There was no significant effect of treatment on QOL over time.
Completers analyses
We conducted “completers” analysis, including only intervention participants that completed all 12 mandatory modules (n=31 / 81). That is, we fitted the same piecewise model to compare completers in web-CBT intervention and those who received TAU. The results of this analysis showed similar (though more robust and more pronounced) intervention effects for alcohol use (i.e., percent drinking days, percent heavy drinking days) during the 12 weeks’ treatment period, but, similar to the ITT analysis, there were no significant treatment by time differences for the other outcomes (i.e., drug use, PTSD, QOL). In addition, this enhanced effect was not sustained during the post-treatment period. A table summarizing the completers analyses can be found in the online appendix (Table A3).
Mediation analyses
We conducted mediation analyses for heavy drinking, as it was the only outcome showing significant treatment effects during the in-treatment period. Results of the univariate mediation analysis (Table 2) show that self-efficacy, social support, hope for the future, and coping were partial mediators of the treatment effect on percent of heavy drinking days1. To assess the collective mediation effect of all six proposed mediators, we also conducted multivariate mediation analyses. For percent of heavy drinking days, the combined mediators had a partial mediation effect: the total treatment effect −6.79 (p = 0.085) became −5.57 (p =0.125) after all mediators were included.
Table 2.
Results of mediation analysis for percent heavy drinking days using change scores (from Baseline to 12 weeks) for both outcome and mediators
| Mediators | Total effect | Direct effect | Indirect effect# | |||
|---|---|---|---|---|---|---|
| Coefficient (s.e.) | p-value | Coefficient (s.e.) | p-value | Coefficient | 95% Confidence Interval | |
| Univariate | ||||||
| Brief Situational Confidence Questionnaire (BSCQ)*p | −6.73 (3.78) | 0.078 | −5.62 (3.74) | 0.135 | −1.11 | (−3.23, 0.14) |
| Medical Outcomes Study Social Support Scale (MOS-SSS)*p | −6.67 (3.78) | 0.080 | −5.35 (3.43) | 0.122 | −1.32 | (−5.07, 1.55) |
| Readiness to Change Questionnaire (RTCQ) | −6.72 (3.74) | 0.075 | −7.10 (3.74) | 0.060 | 0.37 | (−0.40, 3.00) |
| The Future Scale*p | −6.72 (3.74) | 0.075 | −6.10 (3.73) | 0.105 | −0.62 | (−3.21, 0.25) |
| The Connor-Davidson Resilience Scale (CD-RISC) | −7.98 (3.57) | 0.027 | −8.25 (3.47) | 0.019 | 0.27 | (−1.50, 2.33) |
| The Coping Strategy Scale (CSS)*p | −7.06 (3.63) | 0.055 | −5.69 (3.60) | 0.117 | −1.37 | (−4.90, −0.10) |
| Mutivariate | −5.99 (4.21) | 0.156 | −5.47 (3.95) | 0.169 | −0.51 | (−6.16, 4.52) |
Notes: To facilitate interpretation, p-values are shown for total effect and direct effect, and confidence intervals are shown for mediated effect based on convention. s.e.= standard error
p<.05
** p <.01.
t= total mediation
partial mediation.
Discussion
The current study examined the efficacy of a web-based CBT intervention for OEF/OIF/OND veterans who presented in VA primary care with diagnostic or subthreshold PTSD and hazardous drinking or drug use. Our results show that the Thinking Forward intervention significantly reduced alcohol use (including heavy drinking) among recently returned combat veterans but did not change self-reported levels of PTSD or quality of life. Our positive findings for alcohol use are consistent with a growing literature supporting the efficacy of web-based interventions for substance misuse (e.g., Bickel et al., 2008; Brief et al., 2013; Kathleen M Carroll, 1998; Marsch, 2011). Also, reductions in heavy drinking correspond to our intervention's approach to target “problem drinking”, but not advocate for abstinence from alcohol as a treatment goal. This focus on reducing hazardous substance use, and not focusing on abstinence, may also explain why we did not see a significant treatment effect on percent of drinking days. It seems that participants in the treatment condition showed a “harm reduction” type of effect; they did not drink on fewer days, but they drank less on days when they did drink. As noted earlier, reducing the frequency of heavy drinking days, even when the total number of days in which alcohol is consumed does not change, tends to reduce the likelihood of experiencing alcohol-related problems. Interestingly, the same pattern was seen for percent of drug use days as for heavy drinking (Figure A3). However, this effect was not significant, likely due to the low rates of drug use in our sample.
The absence of a intervention effect on PTSD symptoms is counter to a recent meta-analysis finding that web-based CBT internvetions for PTSD were superior to passive control conditions (Kuester, Niemeyer, & Knaevelsrud, 2016). It is possible that the self-directed nature of the intervention allowed veterans to selectively attend to problems that were less impacted by avoidance symptoms, which is common in people with PTSD. Newman, Szkodny, Llera, and Przeworski (2011) conducted an extensive review and reported that technology-delivered interventions for substance use that were wholly or predominantly self-administered (as is Thinking Forward) showed efficacy, but that some amount of professional contact is important in maintaining and enhancing the gains made in treatment. The addition of therapuetic contact by mental health clinicians or peer support specialists may enhance the intervention's impact on PTSD symptoms. Another possible reason for non significant PTSD effects is that only four participants used the module, Overcoming Trauma Through Exposure module. Exposure has been identified as one of the most efficacious interventions for PTSD (Bradley, Greene, Russ, Dutra, & Westen, 2005). An intervention effect may have emerged if the exposure module had been a core rather than an optional module. It is also important to note that participants in our sample, though experiencing clinically significant distress associated with PTSD, were not enrolled in or seeking treatment for PTSD. Such individuals may have been reluctant to practice or apply the skills in the program targeting their PTSD, especially as many had high levels of avoidance around their PTSD symptoms.
Regarding intervention acceptability, with the exception of “easy to understand,” the majority of veterans provided positive feedback across several evaluative domains such as useful, interesting, and clarification of PTSD and subtance misuse. It's possible that while the overall intervention was engaging, veterans may have had difficulty fully understanding the cognitive therapy sections of the programs despite the use of the concrete examples and exercises. A more fine-grained examination of response to each program section is needed to improve ease of understanding. Even with a slightly lower rating of ease of understanding, adherence to the intervention was consistent with other technology-based interventions (e.g., Bickel et al., 2008; Brief et al., 2013; Kathleen M Carroll, 1998; Marsch, 2011). Most veterans completed the core intervention content, but there was a drop in engagement with the additional (optional) program sections. Differentiating between core content and additional content may somehow imply to users that the additional content is less important, potent, or easier to ignore.
We also failed to find a treatment effect for change in quality of life. This may have been due to a ceiling effect; veterans in our sample reported high levels of quality of life at baseline, so there was not much opportunity to show improvement on this measure. It is possible the measure we chose was not sensitive enough to capture real changes in our generally well sample, as the WHO-QOLBREF was designed to assess quality of life in chronically ill and other medical populations with much greater life interference as our current sample.
Regarding mechanisms of change for the intervention, our results indicate that self-efficacy, social support, coping, and hope for the future served as partial intervening mediators for redcutions in heavy drinking. Self-efficacy has been found to mediate the effects of other web-based CBT interventions for substance misuse (eg. Danaher, Smolkowski, Seeley, & Severson, 2008) while social support is a common mediator in a variety of treatments (Magura et al., 2003). The skills building, strengths-based approach of our web-based CBT may have helped to increase self-efficacy in our veteran sample, and our focus on communication and improving relationships may have fostered improved social support. While we anticipated that Thinking Forward would also foster resilience, we did not find support for this.
One limitation of the current study is the use of self-report data to assess our primary outcome of alcohol and drug use (via TLFB). However, significant, positive correlations between veteran self-reports and collaterals, lack of trend for underreporting compared to collaterals, and very small differences in the amount of use reported strengthen the confidence in the validity of self-reported alcohol use. In addition, the TLFB is a widely used and validated method for assesisng alcohol use. Another potential limitation to the current study was the inclusion of veterans reporting subthreshold (and not just diagnostic) PTSD. We chose to include veterans with subthreshold PTSD as they have been shown to exhibit significant functional difficuties, similar to those with diagnostic PTSD, but may be less likely to receive treatment due to lack of a formal diagnosis (Jakupcak et al., 2007; Pietrzak et al., 2009b). A third limitation of the current study was that, given the limits of our data collection, we were unable to clearly establish temporal precedence in our mediational analyses. Finally, our study drop out may be seen as a limitation despite retaining the majority of our sample through the 3-month follow up (76.5%). Our retention rates are consistent with other treatment studies (e.g., Bickel et al., 2008; Brief et al., 2013; Kathleen M Carroll, 1998; Marsch, 2011), and better than other web-based CBT studies of OEF/OIF veterans (~40% retained at 3-month follow up in Brief et al., 2013). We attempted to mitigate the drop out by employing an ITT approach in our analyses but recognize this is still a limitation of the current study.
Conclusions
The current study demonstrated that a web-based CBT intervention was effective in reducing heavy drinking among OEF/OIF/OND veterans with symptomatic PTSD and hazardous substance use. The impact of the intervention on heavy drinking was mediated by intervening increases in social support, self-efficacy, coping, and hope for the future during the 12-week intervention period. These findings indicate that a web-based, self-management intervention may be useful for engaging and providing treatment to difficult to reach veterans with behavioral health and substance use needs. This type of web-based intervention could be made easily accessible to the many thousands of veterans who need treatment, but are reluctant or unable to receive traditional mental health or substance use treatment. Future research is needed to investigate if adding professional support to web-based treatments may boost their effectiveness in treating PTSD and to determine which aspects of the current treatment are essential to generate the desired improvements in PTSD and substance use outcomes.
Supplementary Material
Highlights.
A web-based CBT intervention significantly decreased binge drinking in a sample of OEF/OIF veterans with symptomatic PTSD and substance use recruited through VA primary care clinics
Treatment-related decreases in binge drinking were mediated by intervening increases in coping, social support, self-efficacy, and hope for the future
Technology-delivered interventions hold promise for providing treatment to difficult-to-reach populations
Acknowledgements
The authors would like to acknowledge the contributions of our veteran participants and the following research staff members for their help collecting data: Juanita Fuentes, Dezarie Hutchison, Todd Bishop, Suzanne Spinola, and Bronte Emery.
Funding: This work was supported by the National Institutes of Health (grant numbers R01AA020181 and P30DA029926).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Complete mediation is not commonly seen in social behavioral studies
References
- Aickin M. A program for balancing the allocation of subjects to treatment in a clinical trial. Computers and Biomedical Research. 1982;15(6):519–524. doi: 10.1016/0010-4809(82)90014-3. [DOI] [PubMed] [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. Audit. The Alcohol Use Disorders Identification Test (AUDIT): Guidelines for use in primary care. 2001 [Google Scholar]
- Back SE, Brady KT, Jaanimagi U, Jackson JL. Cocaine dependence and PTSD: a pilot study of symptom interplay and treatment preferences. Addictive Behaviors. 2006;31(2):351–354. doi: 10.1016/j.addbeh.2005.05.008. doi: 10.1016/j.addbeh.2005.05.008. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Marsch LA, Buchhalter AR, Badger GJ. Computerized behavior therapy for opioid-dependent outpatients: a randomized controlled trial. Experimental and Clinical Psychopharmacology. 2008;16(2):132–143. doi: 10.1037/1064-1297.16.2.132. doi: 10.1037/1064-1297.16.2.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress. 1995;8(1):75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Bradley R, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. American Journal of Psychiatry. 2005;162(2):214–227. doi: 10.1176/appi.ajp.162.2.214. doi: 10.1176/appi.ajp.162.2.214. [DOI] [PubMed] [Google Scholar]
- Breslin FC, Sobell LC, Sobell MB, Agrawal S. A comparison of a brief and long version of the Situational Confidence Questionnaire. Behaviour Research and Therapy. 2000;38(12):1211–1220. doi: 10.1016/s0005-7967(99)00152-7. [DOI] [PubMed] [Google Scholar]
- Brief DJ, Rubin A, Keane TM, Enggasser JL, Roy M, Helmuth E, Rosenbloom D. Web intervention for OEF/OIF veterans with problem drinking and PTSD symptoms: a randomized clinical trial. Journal of Consulting and Clinical Psychology. 2013;81(5):890–900. doi: 10.1037/a0033697. doi: 10.1037/a0033697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burleson JA, Kaminer Y. Self-efficacy as a predictor of treatment outcome in adolescent substance use disorders. Addictive Behaviors. 2005;30(9):1751–1764. doi: 10.1016/j.addbeh.2005.07.006. doi: 10.1016/j.addbeh.2005.07.006. [DOI] [PubMed] [Google Scholar]
- Carroll KM. Therapy Manuals for Drug Addiction, Manual 1: A Cognitive-Behavioral Approach: Treating Cocaine Addiction. National Institute on Drug Abuse; 1998. [Google Scholar]
- Carroll KM, Ball SA, Martino S, Nich C, Babuscio TA, Rounsaville BJ. Enduring effects of a computer-assisted training program for cognitive behavioral therapy: a 6-month follow-up of CBT4CBT. Drug and Alcohol Dependence. 2009;100(1-2):178–181. doi: 10.1016/j.drugalcdep.2008.09.015. doi: 10.1016/j.drugalcdep.2008.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Condiotte MM, Lichtenstein E. Self-efficacy and relapse in smoking cessation programs. Journal of Consulting and Clinical Psychology. 1981;49(5):648–658. doi: 10.1037//0022-006x.49.5.648. [DOI] [PubMed] [Google Scholar]
- Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depression and Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- Danaher BG, Smolkowski K, Seeley JR, Severson HH. Mediators of a successful web-based smokeless tobacco cessation program. Addiction. 2008;103(10):1706–1712. doi: 10.1111/j.1360-0443.2008.02295.x. doi: 10.1111/j.1360-0443.2008.02295.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeMarce JM, Burden JL, Lash SJ, Stephens RS, Grambow SC. Convergent validity of the Timeline Followback for persons with comorbid psychiatric disorders engaged in residential substance use treatment. Addictive Behaviors. 2007;32:1582–1592. doi: 10.1016/j.addbeh.2006.11.015. [DOI] [PubMed] [Google Scholar]
- Dunn C, Deroo L, Rivara FP. The use of brief interventions adapted from motivational interviewing across behavioral domains: a systematic review. Addiction. 2001;96(12):1725–1742. doi: 10.1046/j.1360-0443.2001.961217253.x. doi: 10.1080/09652140120089481. [DOI] [PubMed] [Google Scholar]
- Erbes C, Westermeyer J, Engdahl B, Johnsen E. Post-traumatic stress disorder and service utilization in a sample of service members from Iraq and Afghanistan. Military Medicine. 2007;172(4):359–363. doi: 10.7205/milmed.172.4.359. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W, O'Farrell TJ, Freitas TT, McFarlin SK, Rutigliano P. The Timeline Followback reports of psychoactive substance use by drug-abusing patients: Psychometric properties. Journal of Consulting and Clinical Psychology. 2000;68(1):134–144. doi: 10.1037//0022-006x.68.1.134. doi: 10.1037//0022-006X.68.1.134. [DOI] [PubMed] [Google Scholar]
- Fitzmaurice GM, Laird NM, Ware JH. Applied longitudinal analysis. 2nd ed. John Wiley & Sons, Inc.; New Jersey: 2011. [Google Scholar]
- Garcia HA, Kelley LP, Rentz TO, Lee S. Pretreatment predictors of dropout from cognitive behavioral therapy for PTSD in Iraq and Afghanistan war veterans. Psychological Services. 2011;8(1):1. [Google Scholar]
- Gros DF, Yoder M, Tuerk PW, Lozano BE, Acierno R. Exposure therapy for PTSD delivered to veterans via telehealth: Predictors of treatment completion and outcome and comparison to treatment delivered in person. Behavior Therapy. 2011;42(2):276–283. doi: 10.1016/j.beth.2010.07.005. [DOI] [PubMed] [Google Scholar]
- Grubaugh AL, Cain GD, Elhai JD, Patrick SL, Frueh BC. Attitudes toward medical and mental health care delivered via telehealth applications among rural and urban primary care patients. Journal of Nervous and Mental Disease. 2008;196(2):166–170. doi: 10.1097/NMD.0b013e318162aa2d. doi: 10.1097/NMD.0b013e318162aa2d. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press; 2013. [Google Scholar]
- Hellstrom C, Jansson B, Carlsson SG. Subjective future as a mediating factor in the relation between pain, pain-related distress and depression. European Journal of Pain (London, England) 1999;3(3):221–233. doi: 10.1053/eujp.1999.0122. doi: 10.1053/eujp.1999.0122. [DOI] [PubMed] [Google Scholar]
- Hellstrom C, Jansson B, Carlsson SG. Perceived future in chronic pain: the relationship between outlook on future and empirically derived psychological patient profiles. European Journal of Pain. 2000;4:283–290. doi: 10.1053/eujp.2000.0184. doi:10.1053/eujp.2000.0184. [DOI] [PubMed] [Google Scholar]
- Helmer DA, Chandler HK, Quigley KS, Blatt M, Teichman R, Lange G. Chronic widespread pain, mental health, and physical role function in OEF/OIF veterans. Pain Medicine. 2009;10(7):1174–1182. doi: 10.1111/j.1526-4637.2009.00723.x. doi: 10.1111/j.1526-4637.2009.00723.x. [DOI] [PubMed] [Google Scholar]
- Hendricks PS, Delucchi KL, Hall SM. Mechanisms of change in extended cognitive behavioral treatment for tobacco dependence. Drug and Alcohol Dependence. 2010;109(1-3):114–119. doi: 10.1016/j.drugalcdep.2009.12.021. doi: 10.1016/j.drugalcdep.2009.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine. 2004;351(1):13–22. doi: 10.1056/NEJMoa040603. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Terhakopian A, Castro CA, Messer SC, Engel CC. Association of posttraumatic stress disorder with somatic symptoms, health care visits, and absenteeism among Iraq war veterans. American Journal of Psychiatry. 2007;164(1):150–153. doi: 10.1176/ajp.2007.164.1.150. doi: 10.1176/ajp.2007.164.1.150. [DOI] [PubMed] [Google Scholar]
- Jacobsen LK, Southwick SM, Kosten TR. Substance use disorders in patients with posttraumatic stress disorder: a review of the literature. American Journal of Psychiatry. 2001;158(8):1184–1190. doi: 10.1176/appi.ajp.158.8.1184. doi: 10.1176/appi.ajp.158.8.1184. [DOI] [PubMed] [Google Scholar]
- Jakupcak M, Conybeare D, Phelps L, Hunt S, Holmes HA, Felker B, McFall ME. Anger, hostility, and aggression among Iraq and Afghanistan War veterans reporting PTSD and subthreshold PTSD. Journal of Traumatic Stress. 2007;20(6):945–954. doi: 10.1002/jts.20258. doi: 10.1002/jts.20258. [DOI] [PubMed] [Google Scholar]
- Jakupcak M, Luterek J, Hunt S, Conybeare D, McFall M. posttraumatic stress and its relationship to physical health functioning in a sample of Iraq and Afghanistan War veterans seeking postdeployment VA health care. Journal of Nervous and Mental Disease. 2008;196(5):425–428. doi: 10.1097/NMD.0b013e31817108ed. doi: 10.1097/NMD.0b013e31817108ed. [DOI] [PubMed] [Google Scholar]
- Jarrett TA. Warrior Resilience and Thriving (WRT): Rational Emotive Behavior Therapy (REBT) as a Resiliency and Thriving Foundation to Prepare Warriors and Their Families for Combat Deployment and Posttraumatic Growth in Operation Iraqi Freedom, 2005–2009. Journal of Rational-Emotive and Cognitive-Behavior Therapy. 2013;31(2):93–107. [Google Scholar]
- Kaskutas LA, Bond J, Humphreys K. Social networks as mediators of the effect of Alcoholics Anonymous. Addiction. 2002;97(7):891–900. doi: 10.1046/j.1360-0443.2002.00118.x. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology. 2007;3:1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432. doi: 10.1146/annurev.clinpsy.3.022806.091432. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ. The self-medication hypothesis of substance use disorders: a reconsideration and recent applications. Harvard Review of Psychiatry. 1997;4(5):231–244. doi: 10.3109/10673229709030550. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- Kiluk BD, Nich C, Babuscio T, Carroll KM. Quality versus quantity: acquisition of coping skills following computerized cognitive-behavioral therapy for substance use disorders. Addiction. 2010;105(12):2120–2127. doi: 10.1111/j.1360-0443.2010.03076.x. doi: 10.1111/j.1360-0443.2010.03076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleim B, Grey N, Wild J, Nussbeck FW, Stott R, Hackmann A, Ehlers A. Cognitive change predicts symptom reduction with cognitive therapy for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2013;81(3):383. doi: 10.1037/a0031290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein B, Mitchell J, Abbott J, Shandley K, Austin D, Gilson K, Redman T. A therapist-assisted cognitive behavior therapy internet intervention for posttraumatic stress disorder: pre-, post- and 3-month follow-up results from an open trial. Journal of Anxiety Disorders. 2010;24(6):635–644. doi: 10.1016/j.janxdis.2010.04.005. doi: 10.1016/j.janxdis.2010.04.005. [DOI] [PubMed] [Google Scholar]
- Knaevelsrud C, Maercker A. Internet-based treatment for PTSD reduces distress and facilitates the development of a strong therapeutic alliance: a randomized controlled clinical trial. BMC psychiatry. 2007;7(1):1. doi: 10.1186/1471-244X-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuester A, Niemeyer H, Knaevelsrud C. Internet-based interventions for posttraumatic stress: A meta-analysis of randomized controlled trials. Clinical Psychology Review. 2016;43:1–16. doi: 10.1016/j.cpr.2015.11.004. doi: 10.1016/j.cpr.2015.11.004. [DOI] [PubMed] [Google Scholar]
- Lee JE, Sudom KA, Zamorski MA. Longitudinal analysis of psychological resilience and mental health in Canadian military personnel returning from overseas deployment. Journal of Occupational Health Psychology. 2013;18(3):327–337. doi: 10.1037/a0033059. doi: 10.1037/a0033059. [DOI] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, Cooney NL, Kabela E. Coping skills and treatment outcomes in cognitive-behavioral and interactional group therapy for alcoholism. Journal of Consulting and Clinical Psychology. 2003;71(1):118–128. doi: 10.1037//0022-006x.71.1.118. [DOI] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, Kabela-Cormier E, Petry NM. Coping skills training and contingency management treatments for marijuana dependence: exploring mechanisms of behavior change. Addiction. 2008;103(4):638–648. doi: 10.1111/j.1360-0443.2008.02137.x. doi: 10.1111/j.1360-0443.2008.02137.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litz BT, Engel CC, Bryant RA, Papa A. A randomized, controlled proof-of-concept trial of an Internet-based, therapist-assisted self-management treatment for posttraumatic stress disorder. The American Journal of Psychiatry. 2007;164:1676–1684. doi: 10.1176/appi.ajp.2007.06122057. doi:10.1176/appi.ajp.2007 .06122057. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP. Introduction to statistical mediation analysis. Routledge; 2008. [Google Scholar]
- Maisto SA, Roos CR, O'Sickey AJ, Kirouac M, Connors GJ, Tonigan JS, Witkiewitz K. The indirect effect of the therapeutic alliance and alcohol abstinence self-efficacy on alcohol use and alcohol-related problems in Project MATCH. Alcoholism: Clinical and Experimental Research. 2015;39(3):504–513. doi: 10.1111/acer.12649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magura S, Knight EL, Vogel HS, Mahmood D, Laudet AB, Rosenblum A. Mediators of effectiveness in dual-focus self-help groups. American Journal of Drug and Alcohol Abuse. 2003;29(2):301–322. doi: 10.1081/ADA-120020514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsch L. Computer-delivered psychosocial treatment for substance use disorders.. Presentation in symposium on Neurobehavioral and Technological Mechanisms to Improve the Efficacy and Effectiveness of Substance Abuse Treatment; Paper presented at the American Psychological Association Annual Meeting.2011. [Google Scholar]
- McCauley JL, Killeen T, Gros DF, Brady KT, Back SE. Posttraumatic Stress Disorder and Co-Occurring Substance Use Disorders: Advances in Assessment and Treatment. Clinical Psychology. 2012;19(3) doi: 10.1111/cpsp.12006. doi: 10.1111/cpsp.12006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDevitt-Murphy ME, Williams JL, Bracken KL, Fields JA, Monahan CJ, Murphy JG. PTSD symptoms, hazardous drinking, and health functioning among U.S.OEF and OIF veterans presenting to primary care. Journal of Traumatic Stress. 2010;23(1):108–111. doi: 10.1002/jts.20482. doi: 10.1002/jts.20482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGovern MP, Lambert-Harris C, Alterman AI, Xie H, Meier A. A Randomized Controlled Trial Comparing Integrated Cognitive Behavioral Therapy Versus Individual Addiction Counseling for Co-occurring Substance Use and Posttraumatic Stress Disorders. Journal of Dual Diagnosis. 2011;7(4):207–227. doi: 10.1080/15504263.2011.620425. doi: 10.1080/15504263.2011.620425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgenstern J, Labouvie E, McCrady BS, Kahler CW, Frey RM. Affiliation with Alcoholics Anonymous after treatment: a study of its therapeutic effects and mechanisms of action. Journal of Consulting and Clinical Psychology. 1997;65(5):768–777. doi: 10.1037//0022-006x.65.5.768. [DOI] [PubMed] [Google Scholar]
- Morgenstern J, Longabaugh R. Cognitive-behavioral treatment for alcohol dependence: a review of evidence for its hypothesized mechanisms of action. Addiction. 2000;95(10):1475–1490. doi: 10.1046/j.1360-0443.2000.951014753.x. [DOI] [PubMed] [Google Scholar]
- Morland L, Frueh B, Pierce K, Miyahira S. PTSD and telemental health: Updates and future directions. National Center for PTSD Clinical Quarterly. 2003;12(1):1–5. [Google Scholar]
- Mureşan V, Montgomery GH, David D. Emotional outcomes and mechanisms of change in online cognitive-behavioral interventions: A quantitative meta-analysis of clinical controlled studies. Journal of Technology in Human Services. 2012;30(1):1–13. [Google Scholar]
- Murphy B, Herrman H, Hawthorne G, Pinzone T, Evert H. Australian WHOQoL instruments: User's manual and interpretation guide. Australian WHOQOL Field Study Centre; Melbourne, Australia: 2000. [Google Scholar]
- Newman MG, Szkodny LE, Llera SJ, Przeworski A. A review of technology-assisted self-help and minimal contact therapies for drug and alcohol abuse and smoking addiction: is human contact necessary for therapeutic efficacy? Clinical Psychology Review. 2011;31(1):178–186. doi: 10.1016/j.cpr.2010.10.002. doi: 10.1016/j.cpr.2010.10.002. [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein MB, Malley JC, Johnson DC, Southwick SM. Subsyndromal posttraumatic stress disorder is associated with health and psychosocial difficulties in veterans of Operations Enduring Freedom and Iraqi Freedom. Depression and Anxiety. 2009b;26(8):739–744. doi: 10.1002/da.20574. doi: 10.1002/da.20574. [DOI] [PubMed] [Google Scholar]
- Possemato K, Maisto SA, Wade M, Barrie K, McKenzie S, Lantinga LJ, Ouimette P. Ecological momentary assessment of PTSD symptoms and alcohol use in combat veterans. Psychology of Addictive Behaviors. 2015;29(4):894–905. doi: 10.1037/adb0000129. doi: 10.1037/adb0000129. [DOI] [PubMed] [Google Scholar]
- Prins A, Cimpean D, Schnurr PP. Treatment in primary care settings. In: Mueser KT, Rosenberg SD, Rosenberg HJ, editors. Treatment of posttraumatic stress disorder in special populations: A cognitive restructuring program. American Psychological Association; Washington, DC: 2009. pp. 301–314. [Google Scholar]
- Riper H, Spek V, Boon B, Conijn B, Kramer K, Martin-Abello K, Smit F. Effectiveness of e-self-help interventions for curbing adult problem drinking: A meta-analysis. Journal of Medical Internet Research. 2011;13(2):e42. doi: 10.2196/jmir.1691. doi:10.2196/jmir.1691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rollnick S, Heather N, Gold R, Hall W. Development of a short 'readiness to change' questionnaire for use in brief, opportunistic interventions among excessive drinkers. British Journal of Addiction. 1992;87(5):743–754. doi: 10.1111/j.1360-0443.1992.tb02720.x. [DOI] [PubMed] [Google Scholar]
- Roy-Byrne P, Craske MG, Sullivan G, Rose RD, Edlund MJ, Lang AJ, Stein MB. Delivery of evidence-based treatment for multiple anxiety disorders in primary care: a randomized controlled trial. JAMA. 2010;303(19):1921–1928. doi: 10.1001/jama.2010.608. doi: 10.1001/jama.2010.608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnurr PP, Lunney CA, Sengupta A, Spiro A., 3rd A longitudinal study of retirement in older male veterans. Journal of Consulting and Clinical Psychology. 2005;73(3):561–566. doi: 10.1037/0022-006X.73.3.561. doi: 10.1037/0022-006X.73.3.561. [DOI] [PubMed] [Google Scholar]
- Seal KH, Maguen S, Cohen B, Gima KS, Metzler TJ, Ren L, Marmar CR. VA mental health services utilization in Iraq and Afghanistan veterans in the first year of receiving new mental health diagnoses. Journal of Traumatic Stress. 2010;23(1):5–16. doi: 10.1002/jts.20493. doi: 10.1002/jts.20493. [DOI] [PubMed] [Google Scholar]
- Seal KH, Metzler TJ, Gima KS, Bertenthal D, Maguen S, Marmar CR. Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans using Department of Veterans Affairs health care, 2002-2008. American Journal of Public Health. 2009;99(9):1651–1658. doi: 10.2105/AJPH.2008.150284. doi: 10.2105/AJPH.2008.150284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan D, Janavs J, Baker R, Harnett-Sheehan K, Knapp E, Sheehan M. The MINI International Neuropsychiatric Interview. 2004 [Google Scholar]
- Sherbourne CD, Stewart AL. The MOS social support survey. Social Science and Medicine. 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- Skinner HA. The drug abuse screening test. Addictive Behaviors. 1982;7(4):363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Alcohol Timeline Followback (TLFB). In: I. A. P. A., editor. Handbook of Psychiatric Measures. American Psychiatric Association; Washington, DC: 2000. pp. 477–479. [Google Scholar]
- Stecker T, McGovern MP, Herr B. An intervention to increase alcohol treatment engagement: a pilot trial. Journal of Substance Abuse Treatment. 2012;43(2):161–167. doi: 10.1016/j.jsat.2011.10.028. doi: 10.1016/j.jsat.2011.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein LA, Minugh PA, Longabaugh R, Wirtz P, Baird J, Nirenberg TD, Gogineni A. Readiness to change as a mediator of the effect of a brief motivational intervention on posttreatment alcohol-related consequences of injured emergency department hazardous drinkers. Psychology of Addictive Behaviors. 2009;23(2):185–195. doi: 10.1037/a0015648. doi: 10.1037/a0015648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Ford J. Psychometric review of the PTSD Checklist. In: Stamm BH, editor. Measurement of stress, trauma, and adaptation. Sidran Press; Lutherville, MD: 1996. [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL-5) 2013 Scale available from the National Center for PTSD at www.ptsd.va.gov.
- Wilson JA, Onorati K, Mishkind M, Reger MA, Gahm GA. Soldier attitudes about technology-based approaches to mental health care. Cyberpsychology & Behavior. 2008;11(6):767–769. doi: 10.1089/cpb.2008.0071. doi: 10.1089/cpb.2008.0071. [DOI] [PubMed] [Google Scholar]
- Wooten NR. Deployment cycle stressors and post-traumatic stress symptoms in Army National Guard women: the mediating effect of resilience. Social Work in Health Care. 2012;51(9):828–849. doi: 10.1080/00981389.2012.692353. doi: 10.1080/00981389.2012.692353. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Rodriguez BF, Weisberg RB, Bruce SE, Spencer MA, Culpepper L, Keller MB. Chronicity in posttraumatic stress disorder and predictors of the course of posttraumatic stress disorder among primary care patients. Journal of Nervous and Mental Disease. 2004;192(2):153–159. doi: 10.1097/01.nmd.0000110287.16635.8e. doi: 10.1097/01.nmd.0000110287.16635.8e. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.