Abstract
Background & objectives:
Estimation of haemoglobin is the most widely used method to assess anaemia. Although direct cyanmethaemoglobin method is the recommended method for estimation of haemoglobin, but it may not be feasible under field conditions. Hence, the present study was undertaken to compare indirect cyanmethaemoglobin method against the conventional direct method for haemoglobin estimation.
Methods:
Haemoglobin levels were estimated for 888 adolescent girls aged 11-18 yr residing in an urban slum in Delhi by both direct and indirect cyanmethaemoglobin methods, and the results were compared.
Results:
The mean haemoglobin levels for 888 whole blood samples estimated by direct and indirect cyanmethaemoglobin method were 116.1 ± 12.7 and 110.5 ± 12.5 g/l, respectively, with a mean difference of 5.67 g/l (95% confidence interval: 5.45 to 5.90, P<0.001); which is equivalent to 0.567 g%. The prevalence of anaemia was reported as 59.6 and 78.2 per cent by direct and indirect methods, respectively. Sensitivity and specificity of indirect cyanmethaemoglobin method were 99.2 and 56.4 per cent, respectively. Using regression analysis, prediction equation was developed for indirect haemoglobin values.
Interpretation & conclusions:
The present findings revealed that indirect cyanmethaemoglobin method overestimated the prevalence of anaemia as compared to the direct method. However, if a correction factor is applied, indirect method could be successfully used for estimating true haemoglobin level. More studies should be undertaken to establish agreement and correction factor between direct and indirect cyanmethaemoglobin methods.
Keywords: Adolescent girls, anaemia, direct cyanmethaemoglobin, indirect cyanmethaemoglobin
Anaemia is a major public health problem in developing countries. One of the reliable indicators for assessing anaemia in population is the determination of haemoglobin concentration1. Direct cyanmethaemoglobin method2 is the most widely used and recommended method by the International Committee for Standardization in Haematology for quantitative estimation of haemoglobin. It involves formation of a stable compound, cyanmethaemoglobin and is relatively a simple and cost-effective method3. This direct method involves estimation of haemoglobin in whole blood samples using spectrophotometer and hence requires laboratory facility which limits its applicability in large-scale surveys, as transportation of whole blood in vials from long distances to central laboratories for analysis may not be feasible. Thus, indirect cyanmethaemoglobin (filter paper) method which is based on the same principle but involves spotting of blood on filter paper is often used for the estimation of haemoglobin in population since it is simple and produces reliable results4. Due to the minimal invasiveness of sampling and ease of packaging and transportation from long distances, indirect cyanmethaemoglobin has been recommended, especially for those situations where laboratory is located at some distance from blood collection points5. Dr Robert Guthrie first used dried blood spot (DBS) specimens to measure phenylalanine in newborns for the identification of inborn errors for the detection of phenylketonuria6,7. Since that time, additional possibilities of using DBS cards for inborn errors of metabolism such as investigations of disorders of amino acid metabolism, fatty acid oxidation, organic acid metabolism, and congenital hypothyroidism have been explored8. With more advancements, DBS method was developed for the estimation of haemoglobin also. However, Sari et al9 indicated an overestimation of the prevalence of anaemia when analyzed by indirect method.
This study was carried out to compare indirect cyanmethaemoglobin method against the conventional direct method (gold standard) and to develop a prediction equation for haemoglobin values obtained by indirect cyanmethaemoglobin method.
Material & Methods
The study was carried out on adolescent girls (11-18 yr) residing in Kirti Nagar slums of West Delhi which is a notified colony as per the ‘Delhi Urban Shelter Improvement Board’ under the Government of National Capital Territory (NCT) of Delhi, India, consisting of approximately 11,500 small units with a total population of approximately 60,000. This study presents the secondary analysis of the haemoglobin values for the adolescent girls who formed part of a randomized controlled trial (RCT) to assess the impact of vitamin B12 supplementation along with iron and folic acid on mild and moderate anaemia10. The data were collected between January, 2012, and March, 2013.
The sample size was calculated for randomized double-blind trial with an assumption of reducing the prevalence of anaemia by 30 per cent with 95 per cent confidence interval and 90 per cent power of test. Hence, a total of 446 adolescent girls were enrolled for RCT. However, all the study volunteers (n = 888) whose blood samples were collected at baseline and post-intervention were tested for haemoglobin and the same data have been analysed in the present study.
Inclusion criteria: Apparently healthy, unmarried non-pregnant adolescent girls (11-18 yr) who volunteered for the study and whose parents gave written informed consent were enrolled in the study. The study volunteers assent was obtained prior to enrolment and they were given an information sheet indicating the details of the study. The Institutional Ethics committee clearance was obtained from the Ethics Committee of Lady Irwin College, University of Delhi, New Delhi.
Venous blood was drawn, and haemoglobin was estimated by direct and indirect cyanmethaemoglobin methods. A total of 888 paired (direct and indirect) values of haemoglobin were available.
Biochemical investigations: Venous blood sample (5 ml) was drawn and collected in ethylenediaminetetraacetic acid (EDTA). Blood in the EDTA vial was mixed thoroughly, and using a micropipette, 20 µl of blood was spotted on pre-labelled Whatman Filter paper-no. I. The filter paper was then allowed to dry and packed in zip pouch and transported to laboratory for analysis. Rest of the blood in EDTA vial was stored in thermocol boxes containing dry ice and transported to the laboratory situated at a distance of approximately 5 km from the field area. The blood samples in the laboratory were stored at -80°C till analysis.
The biochemical analysis was carried out in the laboratory of the Centre for Promotion of Nutrition Research and Training, with special focus on North-East, Tribal and Inaccessible Population, New Delhi [National Accreditation Board of Testing and Calibrating Laboratories (NABL) accredited under ISO 15189:2007]. Strict internal and external quality control measures were followed. Internal quality control was maintained using haemoglobin standard with every batch of samples, whereas for external quality control, the laboratory was enrolled in the External Quality Assurance Programmes offered by the Department of Haematology, All India Institute of Medical Sciences, New Delhi.
Estimation of haemoglobin by direct and indirect methods: The basic principle of both direct and indirect cyanmethaemoglobin methods is the same. In the direct method, the blood (20 µl) was directly pipetted in the Drabkin's solution; whereas in the indirect method, the blood was spotted on the filter paper which was then eluted in the Drabkin's solution.
Five millilitres of Drabkin's solution was taken in a test tube and 20 µl of whole blood was added to it from the EDTA vial. The tubes were vortexed for 60 sec and then kept for 15 min. The absorption was read at 540 nm wavelength against the reagent blank. The absorption of the pure stock haemoglobin standard was also recorded for each run11.
For the indirect method, the blood spotted on the filter paper was cut close to its periphery. Five millilitres of Drabkin's solution was pipetted into a test tube and the filter paper was dipped in the solution and kept for one hour at room temperature. The tubes were then vortexed for 60 sec and then again left for one hour. The absorption was read on spectrophotometer at 540 nm wavelength against the reagent blank. The absorption of the pure stock haemoglobin standard was also recorded for each run11,12.
Statistical analysis: Data were entered using Microsoft Office Excel 2007 and were then exported to SPSS Statistics software version 20 (IBM, New Delhi, India) for analysis. Analysis of variance was employed to compare the haemoglobin values using direct and indirect cyanmethaemoglobin methods and to compare the mean difference between the two methods on the basis of time gap between collection and analysis. Sensitivity and specificity were calculated for indirect cyanmethaemoglobin method using direct method as the gold standard. The classification of study volunteers by the direct and indirect methods as non-anaemic, mild, moderate and severe anaemic was done by Marginal Homogeneity test which is an extension of McNemar's test for multinomial responses. Regression analysis was done for direct and indirect haemoglobin values to develop a prediction equation. Validation of the regression model was done on haemoglobin values of the study volunteers collected by filter paper method for another study (unpublished data) carried out on pregnant women (n = 241) residing in Kirti Nagar slums.
Results
The mean haemoglobin levels for 888 whole blood samples estimated by direct and indirect cyanmethaemoglobin methods were 116.1 ± 12.7 and 110.5 ± 12.5 g/l, respectively, with a mean difference of 5.67 g/l [95% confidence interval (CI): 5.45 to 5.90, P<0.001]; that is equivalent to 0.567 g%. The scatter of values, however, was similar, being 12.7 g/l for the direct method and 12.5 g/l for the indirect method.
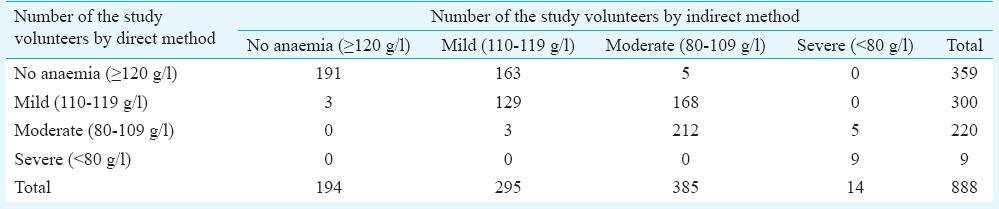
The prevalence of anaemia (<120 g/l)13 using indirect method was estimated as 78.2 per cent and was significantly higher (P<0.001) than by direct method i.e., 59.6 per cent. The prevalence of mild (110-119 g/l), moderate (80-109 g/l) and severe anaemia (<80 g/l)13 was found to be 33.8, 24.8 and 1.0 per cent, respectively, using the direct method and 33.2, 43.4 and 1.7 per cent, respectively, using indirect method. Table I shows the distribution of patients as mild, moderate and severe anaemic and nonanaemic by the two methods. The proportion of study volunteers with identical classification by the two methods (as no anaemia; mild; moderate or severe anaemia) was 541/888 i.e., 61 per cent. Of the remaining 347 volunteers, 341 were classified by the indirect method as belonging to a higher anaemic class than the direct method, compared to only six in the opposite direction (P<0.001). Further analysis showed that 168 (46.7%) of 359 nonanaemic girls were misclassified as anaemic by the indirect method, while 168 (56%) of 300 patients with mild anaemia were labelled as having moderate anaemia.
Table I.
Comparison of outcomes with direct and indirect methods of haemoglobin estimation
The sensitivity of the indirect cyanmethaemoglobin method was 99.2 per cent (95% CI: 98.0-99.7) whereas the specificity was found to be 56.4 per cent (95% CI: 51.3-61.4), which implied that a higher prevalence of anaemia would be reported using indirect method.
On comparing the classification of study volunteers by the direct and indirect methods as nonanaemic, mild, moderate and severe anaemic a significant difference was observed in the number of patients in each category by the two methods (P<0.001).
Stability of haemoglobin estimation by filter paper method: In the present study, samples were analyzed by indirect method within 2-12 days of collection, whereas direct analysis was undertaken within 0-5 days of sample collection. There was no significant difference in the mean difference between direct and indirect methods on the basis of the time gap between collection and analysis except in 8-9 days gap group. Regression analysis of the individual differences on the time gap indicated no significant association between the two.
Regression analysis and prediction equation: The regression of indirect method to direct method was done, and slope and intercept were calculated as 0.97 (95% CI: 0.95-0.98) and 9.4 (95% CI: 7.4-11.4), respectively. Based on the prediction of direct values, the following regression equation was developed:
Hb value (direct Cyanmet method) = 9.4 + (0.97 × indirect Cyanmet method) (r2 = 0.906)
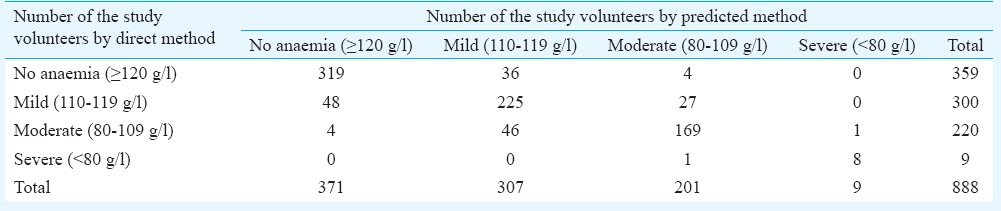
The prediction equation developed was applied to 888 study volunteers to observe its impact on the prevalence of anaemia by the indirect method. After applying the prediction equation, the prevalence rates were 34.6, 22.6, 1.0 and 41.8 per cent for mild, moderate, severe anaemia and non-anaemia, respectively, and matched well with the prevalence as indicated by the direct method. Further, on comparing the data in Tables I and II, it was found that the proportion of study volunteers with identical classification by the two methods (as no anaemia; mild, moderate or severe anaemia) increased from 61 per cent (541/888) to 81.2 per cent (721/888). The specificity of the indirect method was found to increase from 56.4 to 85.2 per cent whereas sensitivity of the method decreased from 99.2 to 91.2 per cent.
Table II.
Comparison of outcomes between predicted values of haemoglobin using regression equation and direct method
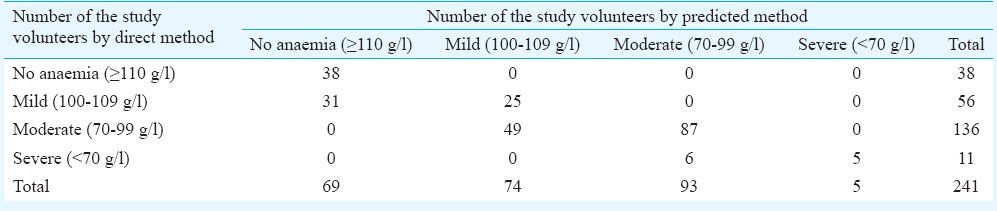
For further validation of regression model, haemoglobin values of the study volunteers collected by filter paper method for another study (unpublished data) carried out on pregnant women (n = 241) were pooled and direct haemoglobin values were predicted using regression equation developed in the present study. It was observed that the prevalence of anaemia reduced from 84.2 to 71.4 per cent. Table III depicts the number of anaemic and nonanaemic pregnant women using the direct and predicted haemoglobin values.
Table III.
Impact of applying regression equation on the prevalence of anaemia among pregnant women
Discussion
The prevalence of anaemia was significantly higher when estimated by indirect cyanmethaemoglobin method as compared to direct cyanmethaemoglobin method (59.6 vs. 78.2%) and had low specificity (53.2%), which might be due to incomplete dissolution of blood from the filter paper to the Drabkin's solution. Sari et al9 also reported significantly higher prevalence of anaemia when haemoglobin concentrations were estimated by the indirect cyanmethaemoglobin (31-38%) method compared to those by the direct cyanmethaemoglobin and HemoCue (14-18%) methods. In the present study, sensitivity of the indirect method was high (99.2%) exhibiting good agreement between the two methods.
Indirect method has the advantage of being relatively simple, cheap and offers ease of transportation of samples even from far-flung places. The indirect method was found to be stable and the results obtained till 15 days of collection of blood spots were comparable, which further increases the applicability of this method in large-scale surveys. However, training required for accurate spotting of blood spot on filter paper and elution of blood from the filter paper are limiting factors for this method. The mean difference in haemoglobin levels observed between direct and indirect cyanmethaemoglobin methods was 5.67 g/l. Hence, if a correction factor/prediction equation was applied to the values obtained by indirect estimation of haemoglobin, a reasonable agreement was established with direct cyanmethaemoglobin method.
From the regression equation, it can be inferred that the predicted haemoglobin value would be 9.4 g/l if the indirect method yields a value of zero, indicating that the indirect method would be meaningful only in situations where the true haemoglobin value is >10 g/l. In other words, the sensitivity level of the indirect method may be deemed to be about 10.
Attempts have been made to develop HemoCue method as an alternative method for the analysis of haemoglobin under field conditions14,15,16,17,18. The main advantages of the method are little staff training required, portable equipment and immediate results. However, the cost of the cuvettes involved in HemoCue method makes it an expensive method and limits its applicability for large-scale surveys in resource-constraint situations. Further, there is conflicting literature with respect to agreement of HemoCue method as compared to direct method. A few studies have indicated a good correlation between direct cyanmethaemoglobin and HemoCue method14,15,16, whereas others have not supported the use of HemoCue method17,18.
In conclusion, indirect cyanmethaemoglobin method can be useful in field conditions to estimate haemoglobin levels; however, a correction factor needs to be applied. More studies should be undertaken to establish agreement and correction factor between direct and indirect cyanmethaemoglobin methods.
Acknowledgment
The first author (PGB) acknowledges the Indian Council of Medical Research, for granting Senior Research Fellowship to carry out the work as part of Ph.D. and for providing facility for biochemical analysis at ICMR.
Footnotes
Conflicts of Interest: None.
References
- 1.Morris SS, Ruel MT, Cohen RJ, Dewey KG, de la Brière B, Hassan MN. Precision, accuracy, and reliability of hemoglobin assessment with use of capillary blood. Am J Clin Nutr. 1999;69:1243–8. doi: 10.1093/ajcn/69.6.1243. [DOI] [PubMed] [Google Scholar]
- 2.Zwart A, van Assendelft OW, Bull BS, England JM, Lewis SM, Zijlstra WG. Recommendations for reference method for haemoglobinometry in human blood (ICSH standard 1995) and specifications for international haemiglobinocyanide standard. J Clin Pathol. (4th ed) 1996;49:271–4. doi: 10.1136/jcp.49.4.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Srivastava T, Negandhi H, Neogi SB, Sharma J, Saxena R. Methods for haemoglobin estimation: a review of “what works”. J Hematol Transfus. 2014;2:1028. [Google Scholar]
- 4.Pathak P, Kapoor SK, Dwivedi SN, Singh P, Kapil U. Comparison of hemoglobin estimates from filter paper cyanmethemoglobin and HemoCue methods. Indian J Community Med. 2004;29:149–50. [Google Scholar]
- 5.DeMaeyer EM, Dallman P, Gurney JM, Hallberg L, Sood SK, Srikantia SG. The prevalence of anaemia in the world. Preventing and controlling iron deficiency anaemia through primary health care: a guide for health administrators and programme managers. Geneva, Switzerland: WHO; 1989. [Google Scholar]
- 6.Guthrie R, Susi A. A simple method for detecting phenyl ketonuria in large population of newborn infants. Pediatrics. 1963;32:338–43. [PubMed] [Google Scholar]
- 7.Mei JV, Alexander JR, Adam BW, Hannon WH. Use of filter paper for the collection and analysis of human whole blood specimens. J Nutr. 2001;131:1631S–6S. doi: 10.1093/jn/131.5.1631S. [DOI] [PubMed] [Google Scholar]
- 8.Lacher DA, Berman LE, Chen TC, Porter KS. Comparison of dried blood spot to venous methods for hemoglobin A1c, glucose, total cholesterol, high-density lipoprotein cholesterol, and C-reactive protein. Clin Chim Acta. 2013;422:54–8. doi: 10.1016/j.cca.2013.03.032. [DOI] [PubMed] [Google Scholar]
- 9.Sari M, de Pee S, Martini E, Herman S, Sugiatmi, Bloem MW, et al. Estimating the prevalence of anaemia: a comparison of three methods. Bull World Health Organ. 2001;79:506–11. [PMC free article] [PubMed] [Google Scholar]
- 10.Bansal PG, Toteja GS, Bhatia N, Vikram NK, Siddhu A. Impact of weekly iron folic acid supplementation with and without Vitamin B12 on anaemic adolescent girls: a randomised clinical trial. Eur J Clin Nutr. 2016;70:730–7. doi: 10.1038/ejcn.2015.215. [DOI] [PubMed] [Google Scholar]
- 11.International Nutritional Anemia Consultative Group. Measurement of iron status. Washington, DC: INACG; 1985. [Google Scholar]
- 12.Mohanram M, Ramana Rao GV, Sastry JG. A comparative study on prevalence of anaemia in women by cyanmethaemoglobin and Haemo-Cue methods. Indian J Community Med. 2002;27:58–61. [Google Scholar]
- 13.WHO. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and Mineral Nutrition Information System (WHO/NMH/NHD/MNM/111) Geneva: World Health Organization; 2011. [accessed on January 24, 2015]. Available from: http://www.who.int/vmnis/indicators/haemoglobin.pdf . [Google Scholar]
- 14.Nkrumah B, Nguah SB, Sarpong N, Dekker D, Idriss A, May J, et al. Hemoglobin estimation by the HemoCue ® portable hemoglobin photometer in a resource poor setting. BMC Clin Pathol. 2011;11:5. doi: 10.1186/1472-6890-11-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Van de Louw A, Lasserre N, Drouhin F, Thierry S, Lecuyer L, Caen D, et al. Reliability of HemoCue in patients with gastrointestinal bleeding. Intensive Care Med. 2007;33:355–8. doi: 10.1007/s00134-006-0461-6. [DOI] [PubMed] [Google Scholar]
- 16.Rippmann CE, Nett PC, Popovic D, Seifert B, Pasch T, Spahn DR. HemoCue, an accurate bedside method of hemoglobin measurement? J Clin Monit Comput. 1997;13:373–7. doi: 10.1023/a:1007451611748. [DOI] [PubMed] [Google Scholar]
- 17.Bhaskaram P, Balakrishna N, Radhakrishna KV, Krishnaswamy K. Validation of hemoglobin estimation using HemoCue. Indian J Pediatr. 2003;70:25–8. doi: 10.1007/BF02722739. [DOI] [PubMed] [Google Scholar]
- 18.Zhou X, Yan H, Xing Y, Dang S, Zhuoma B, Wang D. Evaluation of a portable hemoglobin photometer in pregnant women in a high altitude area: a pilot study. BMC Public Health. 2009;9:228. doi: 10.1186/1471-2458-9-228. [DOI] [PMC free article] [PubMed] [Google Scholar]


