Abstract
Shortage of healthcare workers in rural and remote areas remains a growing concern both in developed and developing countries. This review aims to synthesize the significant factors impacting healthcare professionals’ recruitment and retention in rural and remote areas, and to identify those relevant for developing countries. This paper included the following steps: exploring scientific literature through predetermined criteria and extracting relevant information by two independents reviewers. The AMSTAR tool was used to assess the methodological quality. Of the 224 screened publications, 15 reviews were included. Four reviews focused on recruitment factors, and another four reviews focused on retention factors. The remaining focused both on recruitment and retention factors. The most important factors influencing recruitment were rural background and rural origin, followed by career development. Opportunities for professional advancement, professional support networks and financial incentives were factors impacting retention. While the main factors influencing recruitment and retention have been largely explored in the literature, the evidence on strategies to reduce the shortage of healthcare workers in rural area, particularly in developing countries, is low. Further research in this field is needed.
Key words: health personnel, recruitment and retention, rural and remote areas, systematic review
Introduction
The shortage of healthcare workers in rural and remote areas remains a growing concern in developing and developed countries.1 Developing countries, and particularly Sub-Saharan Africa countries, are facing a serious human resource crisis in the health sector. In these countries, the number of healthcare workers is insufficient to achieve population health goals.2
In 2004, the Joint Learning Initiative (JLI) report Human Resources for Health,3 stated that Sub-Saharan countries must nearly triple their current numbers of workers by adding the equivalent of one million workers through retention, recruitment and training if they are to come close to approaching the Millennium Development Goals for health (MDGs). The severity of the health workforce crisis in some of the world’s poorest countries is illustrated by the World Health Organization (WHO),4 which estimates that 57 countries, of which 36 in Africa, have a deficit of 2.4 million doctors, nurses and midwives. Also, the uneven distribution of the health workforce between urban and rural areas and the absence of a well-trained and supported staff constitute major problems in delivering services to meet the needs of communities in developing countries.5
According to the WHO4 health system performance depends hardly on the quality, composition, distribution and retention of qualified healthcare workers. Globally, it is recognized that nearly half of the global population living in rural and remote areas is facing enormous difficulties in access to quality healthcare. To solve this problem, the WHO has developed recommendations for health policy of its member countries. These recommendations are intended to improve access to healthcare professionals in rural and remote areas through improving their retention.6
However, attracting and retaining healthcare professionals in rural and remote areas is an acknowledged problem in many countries.3 It is crucial to identify and recognize important factors for recruiting and retaining trained personnel in rural and remote areas. A number of significant factors that can improve retention of physicians in rural practice has been studied in developed countries, notably the USA, Canada, New Zealand and Australia.7 These include an adequate income, appropriate workload, locum provision, access to specialists’ advice and continuing education, spouse career opportunities and children education.8 However, little is known about the transferability of these results to other healthcare professionals and to other settings, particularly developing countries.
This overview aims to synthesize the significant factors impacting healthcare professionals’ recruitment and retention in rural and remote areas, and to identify those relevant for developing countries in order to propose effective interventions to address the healthcare workforce shortage.
Materials and Methods
An umbrella review was performed, which provides an overview of existing systematic reviews9 to synthesize the significant factors impacting healthcare professionals’ recruitment and retention in rural and remote areas. The following keywords, and their variations, were used in combination with each other: recruitment and retention, health personnel or health manpower, rural and remote areas, systematic review or literature review. The following databases were consulted: MEDLINE (PubMed interface), CINAHL, EMBASE, PsycINFO, EPISTEMONIKOS and Web of Science. The search strategy is illustrated in Table 1. The reference lists of all included reviews were also searched and hand searches in journals identified as relevant to this area in Google Scholar were conducted. While the search was international, inclusion of publications were limited from a 14-year period (January 1 2000 to August 31 2014). Studies were eligible for the review if they met the following inclusion criteria: i) derived from a systematic review; ii) involved healthcare professionals; iii) reported on factors related to recruitment and retention in rural and/or remote areas; and iv) were published in English or French.
Table 1.
Search strategy.
| Pubmed | CINHAL |
|---|---|
| (“Personnel Management” [Mesh] OR “personnel selection” MeSH Terms] OR “manpower” [TIAB] | MH “Personnel Recruitment” OR MH |
| OR “personnel turnover”[MeSH Terms] OR “human resource”[Title/Abstract] OR “human resourced” | (“Personnel Retention”) AND (MH “practical nurse” |
| [Title/Abstract] OR “human resources”[Title/Abstract] OR “recruitment”[Title/Abstract] | OR MH “Health Manpower” OR MH “Medical Staff”) |
| OR “retention”[Title/Abstract]OR “Job Satisfaction”[Mesh] OR “Personal Satisfaction”[Mesh]) | AND MH “Rural areas” AND MH” |
| AND (“Health Personnel”[Mesh] OR “Nurses”[Mesh] OR “Pharmacists”[Mesh] OR | Developing countries” |
| “Dentists”[Mesh] OR “Health worker”[TIAB] OR “Healthcare worker”[TIAB] | |
| OR “Health care worker”[TIAB] OR “Health care personnel”[TIAB] | |
| OR “Health professional”[TIAB] OR “Healthcare professional”[TIAB] | |
| OR “Health care professional”[TIAB] OR “Dietetician” [TIAB] OR “Psychiatrist”[TIAB] | |
| OR “Psychologist”[TIAB] OR “Physical therapist”[TIAB] OR “Specialist”[TIAB] | |
| OR “Health Manpower”[Mesh]) | |
| AND (“Rural Population”[Mesh] OR “Hospitals, Rural”[Mesh] | |
| OR “Rural Health Services”[Mesh]OR “Medically Underserved Area”[Mesh] | |
| OR “Professional Practice Location”[Mesh])AND “Developing countries” | |
| [Title/Abstract] AND [2000-2014] |
Studies that were not reviews, did not relate to recruitment and retention of healthcare workers, did not specifically concern rural and remote areas, and were published in other languages were excluded.
The systematic review process is shown in Figure 1. First, two members of the research team independently read the title and abstract of each retrieved article to identify potentially relevant reviews. Then, the same two reviewers independently reviewed the full text of each potentially relevant article, compared their results and agreed about the final codification. Finally, the AMSTAR, a quality appraisal tool created to assess the methodological quality of systematic reviews10 that consists of 11 items was used.
Figure 1.
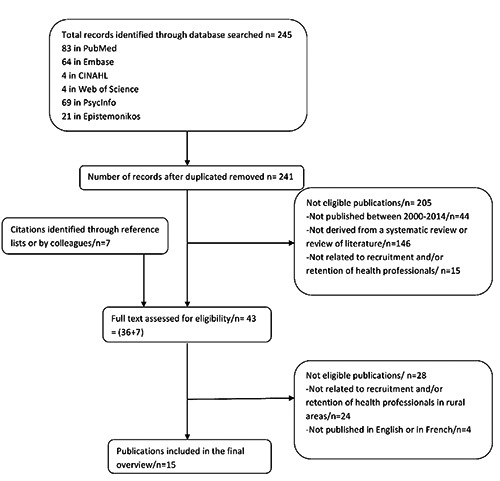
Study selection flow.
This evaluation of the methodological quality of reporting did not aim to decide study inclusion or exclusion, but rather to consider this score in the interpretation of results.
Ethical approval was received from the research ethics committee of Université Laval, on September, 30 2014 (approval number: 2014-191/30-09-2014).
Results
The search strategy identified 245 citations. Duplicates were then removed, leaving 241 citations. Two reviewers independently screened titles and abstracts, and selected 36 publications for full text review. Seven additional references were located by searching the table of contents of relevant journals and from citations within the articles obtained through the literature search. Thus, a total of 43 full text publications were screened independently by two reviewers based on inclusion criteria, of which 15 were ultimately included in the overview (Figure 1). These publications met the final criteria which are: derived from a systematic review; involve healthcare professionals in rural and/or remote areas; report on factors related to recruitment and retention in rural and/or remote areas; and be published in English or in French.
The characteristics of the included reviews and the quality appraisal score of studies were reported in Table 2. A summary of the various topics covered in the studies and their classification by AMSTAR tool is shown in Table 3.
Table 2.
Characteristics of included reviews.
| Authors | Year | Country | Included studies | Type of professionals | Dimension | Factors having an impact on recruitment and/or retention | AMSTAR score |
|---|---|---|---|---|---|---|---|
| Campbell et al. | 2012 | Australia | 35 | Allied health professionals | Recruitment and retention | Professional development; Professional isolation; Insufficient supervision; Rural lifestyle; Autonomy and community connectedness |
7/11 |
| Ballance et al. | 2009 | United States | 21 | Physicians | Recruitment and retention | Rural experiences during medical school and residency; Rural origin |
5/11 |
| Lehmann et al. | 2008 | Middle and low-inco countries | me 55 | Health personnel | Recruitment and retention | Career opportunities; Higher income; General living conditions; Rural upbringing; Work environment |
6/11 |
| Brooks et al. | 2002 | United States | 21 | Primary care physicians | Recruitment and retention | Rural upbringing; Rural experiences during medical school and residency |
10/11 |
| Roots & Li | 2013 | Canada | 12 | Rehabilitation professionals | Recruitment and retention | Rural background; Professional support; Professional development |
9/11 |
| Bilodeau & Leduc | 2003 | Australia, Canada, USA | 37 | Physicians | Recruitment and retention | Rural background; Rural experiences; Career opportunities; Professional support; Autonomy |
6/11 |
| Viscomi et al. | 2013 | Canada and Australia | 86 | Family practitioners | Recruitment and retention | Rural background; Rural experiences during medical school and residency; Rural lifestyle; Career development |
7/11 |
| Trépanier et al. | 2013 | Canada | 15 | Newly graduated nurses | Recruitment | Rural background; Rural clinical experience; Opportunities for family practice; Professional and peer support; Income potential |
10/11 |
| Henry et al. | 2009 | Australia | Not specified | Medical graduates | Recruitment | Rural background; Rural clinical experience; Rural lifestyle; Professional support |
5/11 |
| McAuliffe & Barnett | 2009 | Australia | 10 | Occupational therapy students | Recruitment | Rural background; Rural placement; Professional support; Career opportunities |
7/11 |
| Philipp & Wright | 2005 | United States | Not specified | Health personnel | Recruitment | Rural background; Rural clinical experience; Financial incentives; Professional support |
4/11 |
| Humphreys et al. | 2001 | Australia | 28 | General practitioners | Retention | Professional support; Autonomy; Continuing medical education; Opportunities for family practice; Rural lifestyle |
6/11 |
| Glazebrook & Harrison | 2006 | Australia | 66 | Medical practitioners | Retention | Career development; Continuing education; Family support; Working and living conditions; Financial incentives |
6/11 |
| Roberge | 2009 | Canada | Not specified | Nurses | Retention | Rural lifestyle; Professional support; Autonomy; Peer recognition; Community satisfaction |
6/11 |
| Willis-Shattuck et al. | 2008 | Developing countries | 20 | Health workers | Retention | Financial incentives; Career development; Professional support; Working conditions; Peer recognition |
9/11 |
Table 3.
Summary of the various topics and classification by AMSTAR tool.
| Topics addressed | References of studies |
|---|---|
| Recruitment | 26,29-31 |
| Retention | 7, 16,27,32 |
| Both Recruitment and retention | 22-25,28, 33, 34 |
| Physicians or medical students | 16, 22-27 |
| Nurses | 31,32 |
| Rehabilitation professionals | 29, 33 |
| Other healthcare professionals | 7, 28, 30, 34 |
| Studies conducted in developed countries | 16, 22-27, 29-34 |
| Studies conducted in developing countries | 7, 28 |
| Studies published between 2008 and 2013 | 7, 22, 25, 26, 28, 29, 31,32, 33, 34 |
| Studies published between 2001 and 2006 | 16, 23, 24, 27, 30 |
| Classification by AMSTAR tool | |
| Studies with more than 80% of the AMSTAR appraisal criteria | 7, 23, 31, 33 |
| Studies with more than 55% of the AMSTAR appraisal criteria | 16,24,25,27-29, 32,34 |
| Studies with more than 36% of the AMSTAR appraisal criteria | 22,26,30 |
Given the methodological heterogeneity of included reviews, a narrative synthesis approach was adopted to summarise and synthesis findings.
Factors associated to recruitment of healthcare workers in remote and rural areas
The four reviews that focus on recruitment and the seven others focusing on both recruitment and retention present a set of personal, professional, social and financial factors that influence attraction to rural or remote areas. Personal factors highlighted in these studies are mostly related to the health worker’s background in rural area and rural origins.11-16
Career opportunities for either the spouse or partner are also an influent factor, along with family ties to the rural area.17,18 The slower, more relaxed lifestyle that rural community offers is also a powerful incentive that could attract healthcare professionals.15
With respect to professional factors, the importance of working conditions in rural areas is highlighted. These working conditions encompass the mode of practice, the high workload, a lack of staff backfill and the availability of equipment.14,16,18,19 Also, career opportunity or appropriate professional development is identified among the first factors of importance in attracting health professionals in rural areas.12-15,18-20 Other factors identified include professional and peer support,12,15,16, 18-20 and greater responsibility and personal autonomy in rural practice.18,20 With respect to social or environmental factors, a rural lifestyle that encompasses relaxed and friendly working environment, social entertainment facilities in rural and remote areas, geographical location of positions, and a perception of closer relationships between health professionals and their rural community are identified in previous reviews.11,12,14-16,18,19 Finally, some financial factors are highlighted as having an impact on recruitment of health professionals in rural areas such as loan repayment, need of health insurance and income potential.15,16,19
Factors associated to retention of healthcare workers in rural and remote areas
The four articles focusing on retention and the seven others focusing both on recruitment and retention also provide personal, professional, social and financial factors related to healthcare worker retention in remote and rural areas. With respect to personal factors, opportunities of employment or activities for the spouse as well as educational opportunities for the children favour retention of healthcare workers.8,11,18,21 The proximity of family and friends and conditions facilitating conciliation between work and family also support retention.8,18 Professional factors influencing retention of healthcare workers are quite similar to those influencing their recruitment. Opportunities for professional advancement, professional support networks, managerial support, professional autonomy, maintenance of clinical skills and peer recognition were highlighted as having an influence on retention of health professionals in rural and remote areas.5,8,11,20-22 Other professional factors were identified such as resource availability, hospital management and hospital infrastructure.5,11,21 Social or environmental factors listed in these reviews include: feeling a sense of belonging in the community, working in a family friendly environment, and having access to social networks.22,23 The importance of general living conditions, better quality of children schools, social/recreational opportunities, safety and access to rapid transport to other cities were also highlighted as having an influence on retention.13,18,21,22 Finally, financial incentives related to healthcare worker motivation were only mentioned in two reviews.5,11
Factors associated to recruitment and retention of healthcare workers in developing countries
Only two reviews focused specifically on developing countries.5,13 The main factors influencing recruitment and retention of healthcare workers in rural areas were the living environments such as: staff accommodation, schools and qualified teachers, good drinking water, electricity, roads and transport; the working conditions and environments such as: organisational arrangement, management support, high-risk work environment, availability of equipment, appreciation by managers and colleagues, appreciation by community and a stable job; the development of opportunities and financial incentives.5,13
Effective strategies to recruit and retain healthcare professionals in developing countries
Successful recruitment in developing countries is supported by improved employment opportunities and/or career prospects, higher income, better living conditions or a more stimulating environment.13 With respect to retention, working and living conditions, opportunities of career advancement and financial incentives have a strong influence on retention in low-income countries.5, 13
Furthermore, there is now considerable agreement in research conducted in high and low-income countries that rural upbringing increases chances of healthcare professionals returning to practice in rural communities.24
Some effective strategies regarding the main factors influencing recruitment and retention of healthcare workers in developing countries are mentioned in the literature. Training for rural practice has become critically important in the context of alleviating serious shortages of health professionals in rural areas.25 This strategy supports rural background and the desire of adventure. For instance, the results of a medical programme at Zamboanga School of Medicine in the South Mindanao region of the Philippines, for which students come predominantly from the local region, showed that more than 90% of its graduates take practice within the region.25
In Mali, appropriate training of young rural doctors showed that retention of trained rural doctors is relatively high for the Malian context. Precisely, the three first cohorts of trainees showed 50% retention after 4 years, 77% after 3 years, and 86% after 2 years.26,27 Another study in Uganda showed that the community based training experience of graduates significantly influenced their choice to work in a rural and underserved area of Uganda, compared with their counterparts from the traditional curriculum.27 The authors of this study concluded that while personal values may impact on a decision to work in a rural area, training experience also shapes personal values and choices.27 However, some authors argue that training alone cannot be the main determinant of retention.13
Financial mechanisms include scholarships, loan repayment schemes and higher salaries for individuals working in the public health sector as well as rural allowances. Further retention grants have been introduced in some countries.8 However, little evidence exists regarding financial interventions in developing countries.1 For instance, a locally based scholarship scheme in northern KwaZulu-Natal offers the local community the opportunity to develop its own human resources for healthcare.28 The success of this scheme provides a model for human resource development at a district level that could be usefully adopted by any tier of government.28 On the other hand, a review conducted in South Africa by Kotzee and Couper29 reveals that improving the salaries of rural doctors is often mentioned as one of the most important intervention to attract and retain them in rural practice.
Discussion
The aim of this overview was to synthesize the significant factors impacting healthcare professionals’ recruitment and retention in rural and remote areas, and to list those relevant for developing countries for which interventions could be effective.
Findings from this overview confirm that a rural background, rural origins and rural lifestyle are personal factors associated with recruitment and retention of health professionals to rural areas. Working conditions and environment, and opportunities for professional advancement represent the main professional and social factors influencing recruitment and retention in rural areas. Financial incentives also play an important role in the recruitment and retention of healthcare workers in rural areas. However, it is difficult to explore the differences between developed countries and developing countries because of the limited number of systematic reviews focusing on recruitment and retention of healthcare workers in developing countries.
On the other hand, few studies have emphasized the efficiency of training for rural practice.27 Although the importance of the immediate working environment on attraction and retention has been identified in numerous studies, little evidence of strategies that address management and working conditions at the work place has been reported.13 Generally, literature mentions that the evidence on strategies to reduce the shortage of health professionals in rural areas in developing countries is low.13
However, in many developing countries, it is reported that improved salaries and benefits are major financial incentives for workers to remain in the health sector,30 but it is often difficult to increase salaries in resource-constrained settings.5 The coercive measures address short-term recruitment problems and are not well accepted by healthcare professionals.1 In summary, it is important to use multiple strategies to address the shortage of health workers in developing countries.
Few studies documented the effectiveness of these interventions, and the reported outcomes are highly variable.1 Also, literature is poor on the various recruitment and retention strategies implemented in low- and middle-income countries, and their impact on healthcare workers.13 Further studies are highly needed on the topic.
Limitations
One important limitation of this overview is most likely the heterogeneity and limited methodological quality of the included studies. In particular, the limited number of reviews dealing with recruitment and retention factors in developing countries impeded us to contrast these factors with those from developed countries. For these reasons and because of the lack of evidence on all factors identified and strategies highlighted in this overview, caution should be exercised before generalizing the findings.
Conclusions
This overview allowed us to identify the main factors influencing recruitment and retention in developed and developing countries and to highlight some effective strategies implemented in developing countries. However, literature is poor on the various targeted strategies and few studies have documented the effectiveness of interventions to alleviate healthcare workforce shortage. Further studies are needed to address the pressing issue of equitable healthcare delivery and identify winning strategies to guide future practice and policy.
Acknowledgements
The authors would like to thank Patrice Ngangue and Durosaire Bakoua for the immense support received in the preparation of this overview.
References
- 1.Wilson NW, Couper ID, De Vries E, et al. A critical review of interventions to redress the inequitable distribution of healthcare professionals to rural and remote areas. Rural Remote Health 2009;9:1060. [PubMed] [Google Scholar]
- 2.Mathauer I, Imhoff I. Health worker motivation in Africa: the role of non-financial incentives and human resource management tools. Hum Resour Health 2006;4:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen L, Evans T, Anand S, et al. Human resources for health: overcoming the crisis. The Lancet 2004;364:1984-90. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. World health report. Geneva, 2006. [Google Scholar]
- 5.Willis-Shattuck M, Bidwell P, Thomas S, et al. Motivation and retention of health workers in developing countries: a systematic review. BMC Health Serv Res 2008;8:247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rourke J. WHO recommendations to improve retention of rural and remote health workers-important for all countries. Rural Remote Health 2010;10. [PubMed] [Google Scholar]
- 7.Butterworth K, Hayes B, Neupane B. Retention of general practitioners in rural Nepal: a qualitative study. Aust J Rural Health 2008;16:201-6. [DOI] [PubMed] [Google Scholar]
- 8.Humphreys J, Jones J, Jones M, et al. A critical review of rural medical workforce retention in Australia. Aust Health Rev 2001;24:91-102. [DOI] [PubMed] [Google Scholar]
- 9.Bialy L, Smith M, Bourke T, Becker L. The Cochrane library and bronchiolitis: an umbrella review. Evidence-Based Child Health Cochrane Rev J 2006;1:939-47. [Google Scholar]
- 10.Shea B, Grimsham L, Wells G, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol 2007;7:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Viscomi M, Larkins S, Gupta TS. Recruitment and retention of general practitioners in rural Canada and Australia: a review of the literature. Can J Rural Med 2013;18:13-23. [PubMed] [Google Scholar]
- 12.Henry JA, Edwards BJ, Crotty B. Why do medical graduates choose rural careers? Rural Remote Health 2009;9:1083. [PubMed] [Google Scholar]
- 13.Lehmann U, Dieleman M, Martineau T. Staffing remote rural areas in middle- and low-income countries: a literature review of attraction and retention. BMC Health Serv Res 2008;8:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McAuliffe T, Barnett F. Factors influencing occupational therapy students’ perceptions of rural and remote practice. Rural Remote Health 2009;9:1078. [PubMed] [Google Scholar]
- 15.Philipp D, Wright D. Recruiting Healthcare Professionals to Rural Areas. Radiol Manag 2005:44-50. [PubMed] [Google Scholar]
- 16.Trepanier A, Gagnon MP, Mbemba GI, et al. Factors associated with intended and effective settlement of nursing students and newly graduated nurses in a rural setting after graduation: a mixed-methods review. Int J Nurs Stud 2013;50:314-25. [DOI] [PubMed] [Google Scholar]
- 17.Ballance D, Kornegay D, Evans P. Factors that influence physicians to practice in rural locations: a review and commentary. J Rural Health 2009;25:276-81. [DOI] [PubMed] [Google Scholar]
- 18.Bilodeau H, Leduc N. [Inventory of the main factors determining the attraction, installation and retention of physicians in remote areas]. Cah Sociol Demogr Med 2003;43:485-504. [PubMed] [Google Scholar]
- 19.Campbell N, McAllister L, Eley D. The influence of motivation in recruitment and retention of rural and remote allied health professionals: a literature review. Rural Remote Health 2012;12:1900. [PubMed] [Google Scholar]
- 20.Roots R, Li L. Recruitment and retention of occupational therapists and physiotherapists in rural regions: A meta-synthesis. BMC Health Serv Res 2013;13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Glazebrook RM, Harrison SL. Obstacles and solutions to maintenance of advanced procedural skills for rural and remote medical practitioners in Australia. Rural Remote Health 2006;6:502. [PubMed] [Google Scholar]
- 22.Roberge C. Who stays in rural nursing practice? An international review of the literature on factors influencing rural nurse retention. Online J Rural Nurs Healthc 2009;9. [Google Scholar]
- 23.Brooks RG, Walsh M, Mardon RE, et al. The roles of nature and nurture in the recruitment and retention of primary care physicians in rural areas: a review of the literature. Acad Med 2002;77:790-8. [DOI] [PubMed] [Google Scholar]
- 24.Mullan F, Frehywot S. Non-physician clinicians in 47 sub-Saharan African countries. Lancet 2007;370:2158-63. [DOI] [PubMed] [Google Scholar]
- 25.Strasser R, Neusy AJ. Context counts: training health workers in and for rural and remote areas. Bull World Health Organ 2010;88:777-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Van Dormael M, Dugas S, Kone Y, et al. Appropriate training and retention of community doctors in rural areas: a case study from Mali. Hum Resour Health 2008;6:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kaye DK, Mwanika A, Sewankambo N. Influence of the training experience of Makerere University medical and nursing graduates on willingness and competence to work in rural health facilities. Rural Remote Health 2010;10:1372. [PubMed] [Google Scholar]
- 28.Ross A, Couper I. Rural scholarship schemes: a solution to the human resource crisis in rural district hospitals. South Afr Fam Pract 2004;46:5-6. [Google Scholar]
- 29.Kotzee TJ, Couper ID. What interventions do South African qualified doctors think will retain them in rural hospitals of the Limpopo province of South Africa? Rural Remote Health 2006;6:581. [PubMed] [Google Scholar]
- 30.Wibulpolprasert S, Pengpaibon P. Integrated strategies to tackle the inequitable distribution of doctors in Thailand: four decades of experience. Hum Resour Health 2003;1:12. [DOI] [PMC free article] [PubMed] [Google Scholar]


