Abstract
Hepatitis B virus (HBV) infection remains a global challenge, although there is currently a safe and effective vaccine available. HBV prevalence in Ghana is not well documented, but vary regionally from 4.8% to 12.3% in the general population, 10.8% to 12.7% in blood donors and about 10.6% in pregnant women. This puts Ghana among the high endemic countries in Africa. The study objective was to determine the sero-prevalence of HBs antigen (Ag) and HBeAg among pregnant women in the Ho municipality. Two hundred and eigh participants (pregnant women), attending Ho Municipal antenatal clinic were enrolled into the study. This study recorded a HBsAg sero-prevalence rate of 2.4% among the pregnant women, with primigravida pregnant women recording (0.98%) and multigravida (1.42%). The prevalence of HBsAg among the pregnant women can be classified as Low Intermediate; therefore there is still the need for routine screening of pregnant women during antenatal visits. Amongst HBsAg positives, HBeAg positivity was significantly high (40% of all HBsAg positive women), which suggests high chances of carrier and vertical transmission (mother to child) state.
Key words: Sero-prevalence, Surface antigen, Pregnant women, Antenatal
Introduction
Hepatitis B Virus (HBV) infection is a major global public health problem with varied prevalence worldwide, it is responsible for about 500, 000 to 1.2 million deaths globally.1 The infection is associated with different clinical outcomes and leads to chronic carrier state in 5 to 10% of patients infected in adult life and 85 to 90% of those infected in infancy.2 Also, about one-third of all these carriers may develop chronic liver diseases, including chronic hepatitis, cirrhosis and hepatocellular carcinoma.2 The major route of transmitting the virus is by percutaneous or mucosal exposure to infected blood and other body fluids such as saliva, semen, sweat, breast milk, tears, urine, and vaginal secretion.3 The virus can also be transmitted among family members within households from carriers, possibly by contact of non-intact skin or mucous membrane with secretions or saliva containing HBV by the oral route or by sexual or intimate exposure.3 However, at least 30% of reported hepatitis B among adults cannot be associated with an identifiable risk factor.3 Factors affecting the prevalence of chronic HBV include age at the time of infection and mode of acquisition, which vary geographically.4,5 In the United States and Western Europe, HBV is often acquired in adolescence or adulthood via sexual contact or injection drug use; while in Ghana and Africa, the major means of HBV is through Vertical exposure from mother to child and horizontal transmission from child to child usually in pre-schools.6 The first detectable serological marker in acute HBV infection is Hepatitis B surface antigen (HBsAg), which is most frequently used to screen for the presence of HBV infection and its persistence for more than 6 months suggests chronic infection.6
The virus is endemic in most parts of the world, with higher endemicity in Asia and subSahara Africa, where sero-prevalence rate is above 6%.7 But the endemicity of HBV is low in most developed countries, such as North America, Northern and Western Europe and Australia.5,8 In sub-Saharan Africa, the prevalence rate varies from one region to the other; East Sub- Saharan Africa have 4.8% prevalence rate, Southern Sub-Saharan Africa 4.1%, Central Sub-Saharan Africa 3% and 6.2% West Sub- Saharan Africa.5 Hepatitis B infection during pregnancy may adversely affect pregnancy outcome, leading to spontaneous abortion, premature delivery, intrauterine growth restrictions, and low birth weight of infants.6 And without intervention such as immunoprophylaxis, a mother who is positive for HBsAg confers a 20% risk of passing the infection to her offspring at the time of birth. This risk is as high as 90% if the mother is also positive for HBeAg.6,9,10 A HBeAg positive test is an indication of the risk of transmission at a rate as high as 70-90% to a neonate, whereas a negative test indicates a <10% rate of transmission.10 In these mothers with HBeAg, the risk of HBV perinatal transmission is reduced from 70% to 90% to approximately 5-15% when the infant receives postnatal immunoprophylaxis with both hepatitis B immune globulin and hepatitis B vaccine series. 6,9,10 To the best of our knowledge there is no available data on the prevalence of Hepatitis B in the Volta region.
Materials and Methods
This was a cross-sectional study involving pregnant women who attended Ho Municipal Hospital Antenatal Clinic in the Volta region of Ghana, between March, 2016 and May, 2016. The purpose of the study was explained to the participants in their preferred language prior to the study and an informed consent was obtained from them. Their socio-demographic characteristics were documented in a structured questionnaire for each participant. Pregnant women who could not give consent and/or have history of hepatitis B immunization where excluded from the study.
Ethical approval (ID: GHS-ERC:03/01/15) was obtained from the Ghana Health Service Ethics Review committee and approval was also given by the hospital authorities. Women who came to antenatal clinic and consented to screening were directed to the hospital’s laboratory. Their blood samples were collected and processed. Plasma samples were tested for HBsAg using Quick TestTM HBsAg Serum/Plasma/Whole Blood Rapid Test Strip (Acon Biotech Diagnostic Systems, San Diego, CA, USA) in the Ho Municipal Hospital laboratory. Positive (Reactive) samples and 10 randomly selected samples were further tested for HBsAg, and HBeAg using Enzyme-Linked Immuno Sorbent Assay (ELISA) in Navrongo Health Research Centre Clinical Laboratory.
Results
Two hundred and eight women were enrolled into the study during the three month period from 3rd March to 11th May, 2016. Of these, 5 tested positive to HBsAg, giving a sero-prevalence rate of 2.4% in the study population. The average age was 27.7 years, 74.5 % of them had Basic education and 72.6% of them are married.
The prevalence of HBsAg in pregnant women according to the age groups; there was some significant statistical association between age group and HBsAg positivity (2=50.2, P<0.001). The highest prevalence of 5.3% (2/38) was found in age group 15-20 and the lower of 0.0% was found in age groups 21-25, 26-30 and 36-40 (Table 1).
Table 1.
Prevalence of hepatitis B surface antigen (HBsAg) in pregnant women, according to the age groups in years.
| Age | Tested | HBsAg positive (%) | HBsAg negative (%) |
|---|---|---|---|
| 15-20 | 38 | 2 (5.3) | 36 (94.7) |
| 21-25 | 48 | 0 (0) | 48(100) |
| 26-30 | 56 | 0 (0) | 56(100) |
| 31-35 | 37 | 1 (2.7) | 36 (97.3) |
| 36-40 | 22 | 0 (0) | 22(100) |
| 41-45 | 6 | 1 (16.6) | 5 (83.4) |
| 46-50 | 1 | 1(100) | 0 (0) |
| Total | 208 | 5 (2.4) | 203 (97.6) |
Pearson chi square (χ2)=50.24, P=0.000.
Study of HBsAg sero-positivity in different gravidae among the women revealed that, there was no significant statistical differences between samples screened and gravida with HBsAg positivity (2=3.0, P>0.05). However, the highest prevalence of 3.7% (2/54) was found amongst HBsAg positive mothers in their first time pregnancy (Table 2).
Table 2.
Hepatitis B surface antigen (HBsAg) seropositivity by gravidae.
| Gravidae | No. | HBsAg positive (%) | HBsAg negative (%) |
|---|---|---|---|
| Primigravida | 54 | 2 (3.7) | 52 (96.3) |
| Multigravida | 154 | 3 (1.9) | 151 (98.1) |
| Total | 208 | 5 (2.4) | 203 (97.6) |
Pearson chi square (χ2)=3.03, P=0.075.
Study of HBs Ag sero-positivity according to marital status revealed that, there was no significant statistical association between HBsAg positivity and marital status (2=0.4, P>0.05). However, the highest prevalence of 3.5% (2/57) was found amongst the unmarried women (Table 3).
Table 3.
Hepatitis B surface antigen (HBsAg) seropositivity by marital status.
| Status | No. | HBsAg positive (%) | HBsAg negative (%) |
|---|---|---|---|
| Married | 151 | 3 (1.9) | 148 (98.1) |
| Unmarried | 57 | 2 (3.5) | 55 (96.5) |
| Total | 208 | 5 (2.4) | 203 (97.6) |
Pearson chi square (2)=0.40, P=0.523
A test for Hepatitis B markers (HBeAg) in pregnant women positive to HBsAg revealed that 40% of all HBsAg positive mothers were also positive to HBeAg (Figure 1).
Figure 1.
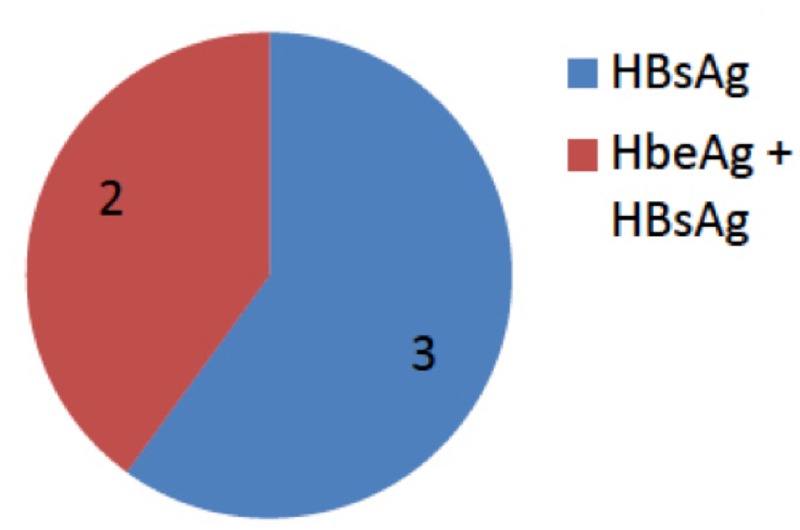
Hepatitis B e antigen (HBeAg) in pregnant women positive to Hepatitis B surface antigen (HBsAg).
Discussion
In west sub-Sahara Africa, the prevalence in the general population varies from country to country. Where Nigeria have 3.7% to 7.7% prevalence rate,9,10 the prevalence rate is between 4.8% and 16% in Ghana.11 The same variation can be seen in pregnant women in the sub-region.
In Nigeria, Kolawole et al.12 had a Prevalence rate of 16.5% among pregnant women in Osogbo, 3.9.0% was reported among pregnant women in Kaduna by Aba,13 and Akani et al.14 reported a prevalence of 4.3% in pregnant women in Port Harcourt. In Yaounde, Cameroon Kfutwah and colleagues reported a prevalence of 16% among pregnant women and in Ghana,15 Damale et al. reported a prevalence of 10.5 % in Accra,16,17 and Cho and others also reported a prevalence of 10.6% in pregnant women in eastern region.17,18
But this study observed a 2.4% prevalence rate of HBsAg among the study participants. This rate is relatively low, compared to previous studies in Ghana that had prevalence of 10.5 and 10.6 percent in pregnant women.11
The differences in the prevalence rate may be due to the geographic variation among regions or due to a difference in the detection method used. It is also worth noting that, globally there is an age related decrease in Hepatitis B prevalence,5 which may be attributed to the introduction of HBV testing in pregnant women combined with immunoglobulin prophylaxis and/or hepatitis B vaccination immediately after delivery in children born to HBsAg positive mothers.11 The decrease may also be attributed to the introduction of universal infant immunization in most countries worldwide.11 This decrease in prevalence was observed in 1990 among age group (25-29) upwards, except in Asia Pacific and Western Europe where there was a relative increase.5 The same trend was seen in 2005, but this time it is Australasia that record an increase in age related prevalence from younger to older populations, with Western Europe and East Asia recording a marginal increase in prevalence from age 60 and above.5 This age related decrease was mostly seen in countries that have adopted the use of hepatitis B vaccine (pentavalent vaccine) in their routine childhood immunization.8,12 In Ghana the Hepatitis B vaccine was introduced in the EPI in Ghana in 2002, therefore those 15 years and above may not benefit directly by having the vaccine, but these people would have benefitted from the herd immunity provided by those who have been immunized with the vaccine, because majority of those vaccinated cohort may seized to be carriers, therefore breaking the chain of transmission.
With regards to age, the present study have shown that the age of a pregnant woman do influence her chances of becoming a HBs Ag carrier (2=50.2, P< 0.001) with women between 46 to 50 years been more at risk . The prevalence of HBsAg within this age group (46-50) was 100% (1/1). This represents 20% off all positive cases. In similar studies conducted in Nigeria and India,13,14 a high seropositivity was found in 18-24 and 21-25 years group respectively. Number of weeks of pregnancy (Trimester) in our study also had no statistical significant effect on the chances of been HBs Ag positive in this study, though the highest prevalence was observed in pregnant women in their third trimester (4/126), 3.17%. This is followed by those in their second (1/62) and first trimester (0/21).
The chance of an infant getting the infection from the mother when she is only HBsAg positive is about 10 to 30%, but when mother is both HbsAg and HBeAg positive the risk is increased to 70-90%.1,15 In this study 0.96% (2/208) of the pregnant women have an increased risk of transmitting the virus prenatally, though a relative little risk of prenatal transmission can be seen in mothers who are HBs Ag-positive, but HBeAg-negative. This suggests the importance of screening for HBV markers (HBeAg) amongst the HBsAg positive women before delivery.
Conclusions
It is clear from this study that Volta region in Ghana is among the areas of lower Hepatitis B prevalence. To sustain and improve on the current rate we recommend routine screening of pregnant women in all health facilities in the country, to identify HBsAg positive mothers for the administration of the birth dose to children born to these women immediately after birth.
Acknowledgments
We are grateful to all the study participants as well as the staff of Ho Municipal Hospital Laboratory. We are also indebted to Dr. Gameli Kwame Norgbe, Dr. Lawrence Y. Kumi, Mr Perfect Ackumey, Mr MA. K. Buadi, Mr. Patrick Owiafi for their support in conducting this study. Arnold Togiwe Luuse was supported by a WACCBIP-World Bank ACE Masters/PhD fellowship (ACE02-WACCBIP: Awandare).
References
- 1.Dyson JK, Waller J, Turley A, et al. Hepatitis B in pregnancy. Frontline Gastroenterol 2014;5:111-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zekri AN, Hafez MM, Mohamed NI, et al. Hepatitis B virus (HBV) genotypes in Egyptian pediatric cancer patients with acute and chronic active HBV infection. Virol J 2007;7:1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aminu M, Okachi EE, Abubakar SM, Yahaya A. Prevalence of hepatitis B virus surface antigen among healthy asymptomatic students in a Nigerian. Ann Afr Med 2013;12:55-6. [DOI] [PubMed] [Google Scholar]
- 4.Shepard CW, Simard EP, Finelli L, et al. Hepatitis B virus infection: epidemiology and vaccination. Epidemiol Rev 2006;28:112-25. [DOI] [PubMed] [Google Scholar]
- 5.Ott JJ, Stevens GA, Groeger J, Wiersma ST. Global epidemiology of hepatitis B virus infection : New estimates of age-specific HBsAg seroprevalence and endemicity. Vaccine 2012;30:2212-9. [DOI] [PubMed] [Google Scholar]
- 6.Ghosh M, Nandi S, Dutta S, Saha MK. Detection of hepatitis B virus infection: a systematic review. World J Hepatol 2015;7:2482-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Locarnini S, Hatzakis A, Chen D, Lok A. Review strategies to control hepatitis B: public policy, epidemiology, vaccine and drugs. J Hepatol 2015;62:S76-86. [DOI] [PubMed] [Google Scholar]
- 8.Custer B, Sullivan SD, Hazlet TK, et al. Global epidemiology of Hepatitis B virus. J Clin Gastroenterol 2004;38: 158-68. [DOI] [PubMed] [Google Scholar]
- 9.American Academy of Pediatrics. A comprehensive immunization strategy to eliminate transmission of Hepatitis B virus infection in the United States. 2006. Available from: https://pediatrics.aappublications.org/content/pediatrics/118/1/404.full.pdf
- 10.Xu ZY, Liu CB, Francis DP, et al. Prevention of perinatal acquisition of hepatitis B virus carriage using vaccine: preliminary report of a randomized, double-blind placebo-controlled and comparative trial. Pediatrics 1985;76:713-8. [PubMed] [Google Scholar]
- 11.Kfutwah AKW, Tejiokem MC, Njouom R. A low proportion of HBeAg among HBsAg-positive pregnant women with known HIV status could suggest low perinatal transmission of HBV in Cameroon. Virol J 2012;9:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Franco E, Bagnato B, Marino MG, et al. Hepatitis B: epidemiology and prevention in developing countries. World J Hepatol 2012;4:74-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yakasai IA, Ayyuba R, Abubakar IS, Ibrahim SA. Sero-prevalence of Hepatitis B Virus infection and its risk factors among pregnant women attending antenatal clinic at Aminu Kano Teaching Teaching Hospital, Kano, Nigeria. J Basic Clin Reprod Sci 2012;1:49-56. [Google Scholar]
- 14.Khakhkhar VM, Bhuva PJ, Bhuva SP, et al. Sero-prevalence of hepatitis B amongst pregnant women attending the antenatal clinic of a tertiary care hospital, Jamnagar (Gujarat). Natl J Med Res 2012;2:362-5. [Google Scholar]
- 15.Umar M1, Hamama-Tul-Bushra Umar S, Khan HA. HBV perinatal transmission. Int J Hepatol 2013;2013:875791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Damale NK, Lassey AT, Bekoe V. Hepatitis B virus seroprevalence among parturients in Accra, Ghana. Int J Gynaecol Obstet 2005;90:240-1. [DOI] [PubMed] [Google Scholar]
- 17.Ofori-asenso R, Agyeman AA. Hepatitis B in Ghana: a systematic review and meta-analysis of prevalence studies (1995-2015). BMC Infect Dis 2016;16:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cho Y, Bonsu G, Akoto-Ampaw A, et al. The prevalence and risk factors for hepatitis B surface Ag positivity in pregnant women in eastern region of Ghana. Gut Liver 2012;6:235-40. [DOI] [PMC free article] [PubMed] [Google Scholar]


