Abstract
The purpose of this study was to identify the various problems with surgical care in the developing world and enumerate identified strategies or propose solutions. We also sought to rank these strategies in order of potential impact. The MEDLINE database was sought. Studies published in English, reporting currently employed solutions to identified barriers or problems to surgical care in developing countries or potential solution(s) and published between 2000 and 2012 were eligible for inclusion. 2156 articles were identified for possible inclusion. MeSH terms include surgery, general surgery, developing countries, health services accessibility and quality improvement. Forty-nine full articles with a primary focus on the solutions to the challenges to surgical care in the developing world were included in the final review. Many articles identified problems with infrastructure, workforce shortage, inadequate or inappropriate policies, and poor financing as major problems with healthcare in the developing world. Solutions addressing these problems are multifactorial and would require active participation of local authorities and collaboration with providers from the developed world. The burden of surgical care is increasing. There is poor access to surgical services in the developing world. If and when surgical care is received, the quality could be less than the standard in developed nations. Solutions exist to tackle these problems but require a multidimensional approach to be successful.
Key words: surgical care, quality improvement, developing countries
Introduction
Surgical conditions affect all age groups in all populations, and cut across various aspects of the health system including maternal health, trauma and emergency services.1 The development of modern surgical equipment and techniques, as well as potent antibiotic therapy, has greatly improved outcomes of surgery. Yet, surgically treatable diseases remain a major component of global morbidity and mortality, with the greater proportion of deaths from surgical procedures, and surgically treatable diseases occurring in less-developed countries.1-3. Access to surgical care remains a significant contributor to the disease burden, particularly in developing countries which, though accounting for ~70% of the world’s population and 80% of deaths from surgicallytreated conditions,4 contribute only about 26% of the surgical procedures carried out worldwide.5 Paradoxically, developing countries account for greater proportion of the global burden of adverse surgical outcomes, despite contributing a lesser proportion of the total surgical procedures carried out worldwide.6 In addition, developing countries face a chronic health worker shortage, in spite of their greater proportion of the global burden of disease.7 The distribution of the available health workers within many developing countries closely mirrors the distribution of their health services and infrastructure, with higher concentrations of skilled health workers including surgeons in urban regions, though a greater need often exists in the rural regions.2 Also, many of the health facilities in rural areas have poor infrastructure and lack essential equipment needed for surgical care.8 Surgical procedures carried out by less-trained health workers, under sub-standard conditions are less likely to be successful and further contribute to adverse surgical outcomes.8 Surgical care available in rural regions thus tends to be of lower quality, often falling short of international standards of care, and frequently associated with complications.9
Increasing acknowledgement of the significance of poor surgical outcomes in developing countries has generated greater focus and discourse on this issue. Several interventions, which identify differing sections of health systems as the ideal intervention point for reducing the incidence of surgical complications in developing countries, have been proposed. However, to the best of the authors’ knowledge, no framework exists prioritizing these interventions in order of potential impact. This review was therefore carried out to identify and integrate strategies that have been proposed for the improvement of the quality of surgical care delivered in developing countries and to provide a framework to guide in the selection of the most effective strategies in the developing world.
Materials and Methods
Eligibility criteria
Studies published in English, reporting currently employed solutions to identified barriers or problems to surgical care in developing countries or potential solution(s) and published between 2000 and 2012 were eligible for inclusion. Quantitative studies as well as qualitative studies were eligible for review.
Data sources
An extensive search was conducted within the MEDLINE database. Articles were identified and retrieved using the following search terms: surgery, general surgery, developing countries, surgical care improvement, and health services accessibility. Relevant World Health Organization (WHO) Reports and Publications were also identified and included in the search results.
The authors reviewed the articles independently and then discussed and agreed on the eligibility of each study.
Data extraction
From each article reviewed, solutions to the existing challenges of surgical care in developing countries were noted. For completeness, the barriers which the solutions were targeted at were also identified, if enumerated. Barriers and solutions were then categorised into domains by the authors, based on degree of relatedness.
Results
From the MEDLINE search, 2156 articles were identified for possible inclusion. One hundred and thirty-one articles were excluded because they were not written in English. Other articles with solutions not specific to surgical care in developing countries or vague in their proposal for surgical improvement were also excluded (Figure 1). Forty-nine full articles with a primary focus on the solutions to the challenges to surgical care in the developing world were included in the final review (Table 1).
Figure 1.
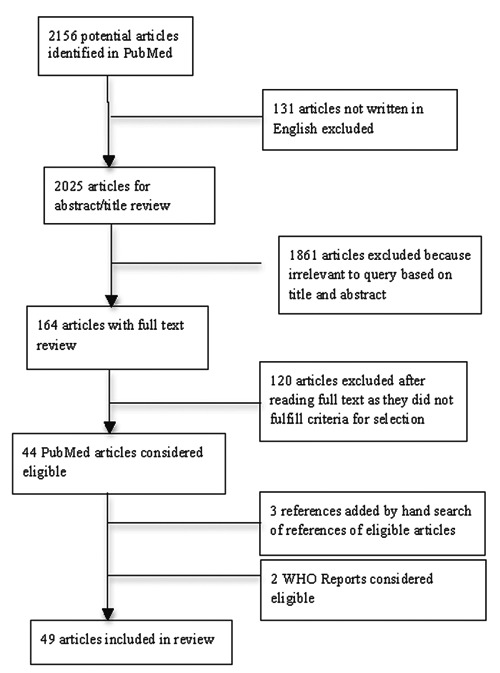
Flow-chart of search strategy.
Table 1.
Studies included in review (n=49).
| Author(s), year of publication | Country (if specified) | Author(s), year of publication | Country (if specified) |
|---|---|---|---|
| Archampong, 2006 | Leow et al., 2011 | Sierra Leone | |
| Arnold, 2012 | Linden et al., 2012 | Uganda | |
| Aswani et al., 2012 | Loefler, 2004 | ||
| Bickler et al., 2002 | Luboga et al., 2009 | ||
| Bickler et al., 2010 | (LMIC) | Luboga et al., 2010 | Uganda |
| Calisti et al., 2010 | Eritrea | Meo et al., 2006 | Sudan |
| Cameron et al., 2010 | Guyana | Mock et al., 2012 | |
| Chirdan et al., 2010 | (Africa) | Natuzzi et al., 2011 | Solomon Islands |
| Contini, 2007 | Ozgediz et al., 2008 | ||
| Daar et al., 2007 | Ozgediz et al., 2009 | (LMIC) | |
| Derbew et al., 2006 | (East Africa) | Perkins et al., 2010 | |
| Duda, 2007 | Petroze et al., 2012 | Rwanda | |
| Dunne et al., 2011 | Quansah et al., 2008 | Ghana | |
| Farner et al., 2008 | Riviello et al., 2010 | ||
| Figus et al., 2009 | Various developing countries | Rogers, 2006 | |
| Gosselin et al., 2011 | Shilpakar, 2011 | Nepal | |
| Haglund et al., 2011 | Uganda | Spiegel et al., 2007 | |
| Haynes et al., 2009 | Syed-Abdul et al., 2012 | ||
| Higginson et al., 2012 | Tollefson et al., 2012 | ||
| Jacobs, 2010 | Udwadia et al., 2008 | India | |
| Kingham, 2009 | Sierra Leone | Vos, 2009 | |
| Kruk et al., 2007 | Weiser et al., 2008 | ||
| Kushner et al., 2010 | Sierra Leone | Zafar et al., 2011 | Pakistan |
| Kwon et al., 2012 | Sierra Leone | [No authors listed], 2012 | |
| Leow et al., 2011 |
LMIC, Low- and middle-income countries.
The [barriers (Table 2) and] strategies (Table 3) proposed by these articles were classified under 5 broad and interrelated domains: personnel; equipment and infrastructure; methods/process; data systems and performance measurement; environment. These five domains are inter-related and together, constitute a pathway to the improvement of surgical care outcomes (Figures 2 and 3).
Table 2.
Relevant studies highlighting challenges to surgical care delivery.
| Domain | Challenges | References |
|---|---|---|
| Personnel | Shortage of manpower Regionalization of surgical services |
Zafar et al.,10 Leow et al.,11 Shilpakar,12 Natuzzi et al.,13 Cameron et al.,15 Meo,17 Archampong,18 Bickler et al.,19 Kingham,29 Arnold25 Zafar et al.,10 Petroze et al.,23 Loefler24 |
| Equipment and maintenance | Lack of basic equipment Poor maintenance |
Shilpakar,12 Natuzzi et al.,13 Calisti et al.,14 Bickler et al.,19 Aswani et al.,20 Petroze et al.,23 Linden et al.,35 Figus41 Archampong,18 Aswani et al.,20 Loefler24 |
| Data systems and performance measurement | Lack of data on performance and patient safety monitoring Poor research facilities |
Zafar et al.,10 Vos,50 Ozgediz et al.,51 Udwadia et al.,16 Derbew et al.53 Vos,50 Ozgediz et al.,51 Udwadia et al.,16 Derbew et al.53 |
| Environment | Mismanagement and corruption Lack of referral facilities | Shilpakar,12 Loefler24 Loefler,24 Duda31 |
Table 3.
Relevant studies highlighting proposed solutions to the challenge of surgical care delivery in developing countries.
| Domain | Solutions | References |
|---|---|---|
| Personnel | Training of workforce | Zafar et al.,10 Leow et al.,11 Archampong,18 Petroze et al.,23 Contini,27 No author listed,28 Spiegel et al.44 |
| Incentives to prevent brain drain Diversification/retraining of health workers; task-shifting Volunteer surgical professionals Skill preservation through CMEs Intra- and international academic partnerships - twinning |
Zafar et al.,10 Natuzzi et al.,13 No author listed,28 Kushner et al.30 Zafar et al.,10 Leow et al.,11 Meo,17 Luboga et al.,26 Gosselin et al.,32 Bickler et al.,19 Quansah et al.,34 Linden et al.35 Farmer et al.,2 Tollefson et al.,38 Leow et al.,11 Dunne et al.,39 Figus et al.40 Leow et al.,42 Udwadia et al.,16 Duda,31 Quansah et al.34 Farmer et al.,2 Chirdan et al.,8 Tollefson et al.,38 Zafar et al.,10 Shilpakar,12 Natuzzi et al.,13 Calisti et al.,14 Cameron et al.,15 Udwadia et al.,16 Petroze et al.,23 Luboga et al.,26 Contini,27 No author listed,28 Kingham et al.,29 Gosselin et al.,32 Quansah et al.,34 Perkins et al.,41 Leow et al.,11 Haglund et al.,43 Spiegel et al.44 |
|
| Equipment and infrastructure | Provision of basic supplies and equipment Infrastructure building, including electricity Training staff on care and maintenance of the equipment |
Farmer et al.,2 Natuzzi et al.,13 Meo,17 Kwon et al.,22 Duda,31 Spiegel et al.44 Farmer et al.,2 Natuzzi et al.,13 Petroze et al.,23 Spiegel et al.44 Farmer et al.,2 Luboga et al.37 |
| Methods and processes | Good referral systems and emergency services Innovative practice: Use of care protocols, checklists, telemedicine Appraisal reviews at hospitals |
Tollefson et al.38 Mock et al.,46 Haynes et al.,47 Syed-Abdul et al.21 Linden et al.,35 Higginson et al.49 |
| Data systems and performance measurement | Robust health data systems Targets and benchmarks for identifying best practices Research fellowships, academic collaborations Develop health information systems Clinical research modules |
Ozgediz et al.,51 Contini,27 No authors listed,28 Duda,31 Vos50 Ozgediz et al.,51 Bickler et al.,33 Duda,31 Rogers52 Perkins et al.,41 Riviello et al.45 Daar et al.,4 Weiser et al.,5 Vos50, Ozgediz et al.1 Nadler et al.54 |
| Environment | Well aligned government policies Support of, and engagement for political and local leaders |
Zafar et al.,10 Linden et al.35 Aswani et al.,20 Kushner et al.,30 Gosselin et al.,32 Jacobs55 |
Figure 2.

Factors identified as crucial to sustained and improved surgical care in developing countries.
Figure 3.
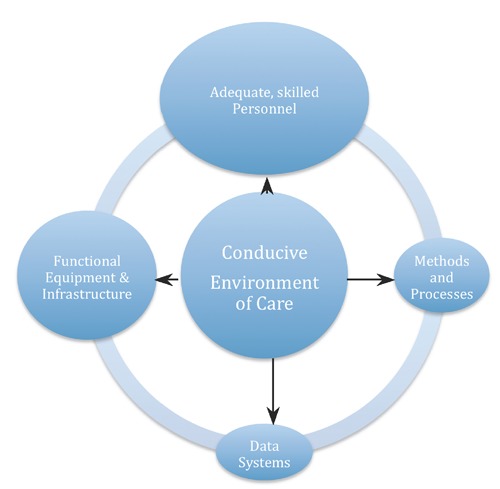
Framework showing relative contribution of major intervention domains to quality of surgical care in developing countries.
Personnel
Human resources are the most critical of the components of surgical care provision. Many developing countries struggle with a shortage of surgical personnel,10-22 and regionalization of available surgical services.23,24 Therefore factors to be considered include excellent and appropriate training of the workforce; proper payment structure and incentives for providers with the ultimate aim of improving the retention of workers through the avoidance of internal or external brain drain.
Staff must be appropriately trained to provide safe effective care and yet motivated enough to remain in the region after receiving this training. To retain surgical providers in the country, incentives must be well aligned to prevent concentration of services in urban areas or external brain drain whereby these trained surgical personnel could relocate to developed countries in search of greener pastures or other fulfilment.25,26 These incentives should be both professional - giving the surgeons opportunities to compete with and be recognized by peers worldwide,27-29 and financial,10,13,27-31 particularly as financial incentives alone cannot adequately control the emigration of providers from developing countries. A combined approach of incentives along with mentoring of young physicians to embrace the field of surgery can help ensure the much needed providers remain in these regions to deliver the most needed care.8
Surgical care is highly specialized. However to quell this workforce shortage of over 2 million,7 other generalists and/or mid-level staff should be trained to provide surgical services such as anaesthesia.10,17,26,32-35 Already in many developing countries, non-surgeons provide most of the anaesthesia and other surgical roles with the quality of care given being similar to that provided by trained anaesthesiologists or surgeons.36,37 Volunteer surgeons and surgical residents from developed countries may periodically help to alleviate the surgical health worker shortage on a short-term basis.2,11,38-40 However, this would not eliminate the longstanding problem of shortage of surgeons.27
Surgeons and other supporting staff in these countries must be trained to constantly deliver standard and safe practices. Surgical skills should be improved through continuous medical education and workshops, visiting lectureships by surgeons from developing countries, collaboration between providers in rural regions and specialists in the urban area, and/or academic partnerships (otherwise called Twinning) with hospitals from developed countries.2,8,10,12-16,18,23,26-29,32,34,38,41-45
Equipment and infrastructure
Many surgical units in developing countries lack the basic equipment- such as anaesthetic machines, diagnostic equipment; proper maintenance of available equipment; availability of basic amenities: portable water, electricity; building of basic infrastructure: operating rooms, ancillary structures: blood banks etc. needed to provide quality care.13,14,19,20,23,35 These also contribute to the poor diagnostic ability in many hospitals in developing countries.19 When equipment are available, some of them are also poorly maintained leading to breakdown.18,20,24
The availability of basic supplies and equipment is crucial to the functioning of a surgical unit.38 Infrastructure to support surgical services such as operating rooms, blood banks and laboratories should also be built to support the smooth operation of the unit.2,13,17,22 Regular supply of electricity or alternative power source should also be prioritized.2,23
To ensure equipment are useful for their expected lifetime and to save costs, local staff should be trained in the care and maintenance of available equipment.2,26
Methods/processes
Factors critical to quality are: standardization of care processes; accountability: existing quality assessment program; good emergency and referral systems; use of innovative tools including checklists and simulation programs.
The methods and processes applied in the healthcare system affect the quality of care. Home-hospital, as well as hospital-hospital communication and transfers should be as smooth as possible. Thus good referral systems and emergency services are a necessary constituent of surgical care improvement in these countries.38
Use of guidelines or care protocols would also offer a way of standardizing processes across settings and comparing outcomes.46 Other tools such as checklists,47 simulation and telemedicine21,48 have also been successfully used to improve surgical care. Morbidity and mortality meetings also offer a means of appraisal of care delivered and outcomes and can help improve surgical care across different settings.35,49
Just like the National Surgical Quality Improvement Program (NSQIP) established by the American College of Surgeons, regulatory bodies in the medical field of these countries have to play a more prominent role in quality improvement (QI). The basic methods of QI should be taught to providers and even medical students.38
Data systems and performance measurement
Factors critical to quality are: development and/or adaptation of performance metrics for surgical care; building of data registries and feedback on performance.
The lack of data on performance and patient safety monitoring contributes to the poor quality of surgical services.10,50 The knowledge of the burden of disease in these countries is crucial to proper planning and advocacy, efficient resource allocation and intervention strategies.3,51 But this knowledge will not be obtained without the establishment of robust data systems that can adequately assess the burden of disease, and the outcomes of care provided.1,27,28,31,50 Also, continual monitoring of impact and cost-effectiveness of programs implemented is needed.44
Feedback to surgical care providers on their performance will be essential for the involvement and active participation of providers in these countries in the quest for better surgical care. Targets should be set, and practices should be compared with both internal and external benchmarks, with the aim of identifying and emulating best practices.52 The awareness of performance evaluation may also, through a Hawthorne effect, further motivate providers to seek for strategies to improve the quality of care provided.3
Research in these countries also has to be improved.2,10,16,20,53 A previous survey among surgeons in sub-Saharan Africa had shown that many surgeons in these areas desire a better understanding of clinical research.54 This knowledge is critical to improving interest and quality of surgical research. Research fellowships and academic collaborations with teaching hospitals in developed countries could help improve this knowledge.41 The medical school curricula in these countries should also include modules in clinical research whereby students can learn and be mentored into taking up research roles in addition to their clinical responsibilities upon graduation. Financial as well as academic support should also be given to researchers to encourage research on surgical conditions. Improved data through health information systems and networks should ultimately improve the quality of care.39,50,51
Environment
A stable socio-political environment is critical to health care quality.12,24 There should be appropriate health policies, government funding and a general upgrade in the standard of living for citizens.8 Mismanagement and corruption at hospital and government levels must also be curtailed for surgical care to be optimal.12,24
To begin new efforts or sustain existing ones to improve surgical care in these countries, the healthcare environment must be conducive. Government policies should be well aligned with the goals of the WHO, donors, providers or volunteers seeking to improve surgical care.10,35 This therefore makes the support and engagement of political and local leaders indispensable.20,30,32,55 Leaders must be committed to improving the health and livelihood of citizens-especially the poor.2 Good transport and communication are also key to an effective referral system.24,31
Poverty may deter citizens from seeking appropriate surgical care.20,24 A fee-for-service payment system could further prevent citizens from seeking the much needed care in a timely fashion. Medical insurance should therefore be provided for the poor. This improvement could in itself improve the health of citizens. Due to the resource limitations in these settings,34 funding and support from international organizations to help fund projects for surgical care improvement will be important.10,11,15,34,35 To strengthen these healthcare systems, continual sufficient government funding of the health sector and on-going support from government bodies is also important28 as well as Public-Private partnerships.16
Discussion
The burden of surgical diseases in developing countries is increasing. Various strategies to improve surgical care in these countries have been geared towards improving access and/or improving the quality of care when care is received. Unfortunately, the identified strategies, either at the micro level or macro level, are not individually capable of creating a permanent and sustainable improvement in surgical care in developing countries. The potential impact of, and inter-relationship between these factors makes it essential that these different factors are addressed simultaneously.
The shortage of well-qualified surgical personnel remains one of the major challenges of surgical care in the developing world. This is further worsened by the regionalization of services with many of the available workers congregating in urban regions of these countries.2 The problem posed by brain drain which has been estimated to cost some developing countries as much as $2.78 billion in loss of returns from investment also needs to be addressed.56 Developing countries must devise a means of reducing brain drain along financial gradients, while maximizing the amount of care that can be obtained from available health care workers within the countries. Local providers must be afforded opportunities to grow professionally and compete with peers from within and outside the countries and also be able to earn a decent pay such that leaving the country in search of greener pastures will look less enticing. In the interim, surgical mission trips can help fill the gap. These stopgap measures must be well aligned with local needs and with collaboration with local providers. Reducing this shortage in the short-term, or improving the skills of providers in these countries will however not produce lasting effects without the support of the governments in these countries.
To ensure equipment that are well maintained, local staff should be trained in the care and maintenance of these equipment. Given resource limitations, equipment purchased by and donated to these health facilities should also be well adapted to the local environment, i.e. cost-effective.
As improvements are made, performance and outcome measurement will be key to identifying areas for improvement. These data should be used for policy development and planning effective strategies. Over the years, the WHO Reports for many healthcare indicators in these developing countries have shown abysmal numbers. Local governments and healthcare agencies should find ways to personalize these data and give feedback to the smallest unit of the healthcare system. This will make these data actionable, allowing for the development of targeted local improvement strategies. The awareness of their performance being measured might in itself through a Hawthorne effect improve care in areas where providers are already empowered to effect change. Just like the NSQIP established by the American College of Surgeons, regulatory bodies in the medical field of developing countries have to play a more prominent role in QI. The basic methods of QI should be taught to providers and even medical students.38
Research must also be encouraged and sustained. This is particularly essential, as the presentation and burden of diseases often differs between regions. To address the common conditions plaguing the citizens of developing countries, the onus rests on researchers in these countries to contribute to the body of knowledge through research.
The environment of care, including government policies and funding, general standard of living of citizens and socio-political climate will play a pivotal role in improving surgical care in these countries. A strong political will is vital for improving surgical care. A government committed to improving the health of its citizens is more likely to embrace the various interventions geared towards surgical care improvement. With this commitment, local and international efforts are more likely to produce lasting and far-reaching effects. Even when services are available, poverty and ignorance may deter citizens from presenting on time when they have a surgically amenable condition. This is further compounded by the out-of-pocket fee payment structure for care that exists in many of these countries, making it difficult for poor citizens- who usually needs surgical care the most- to look for and afford surgery. For sustainability of surgical care improvement in these countries, it is vital that the general socioeconomic status of citizens of these countries improves and appropriate payment structures put in place.8 The plague of infectious diseases, civil wars etc. also impoverish citizens and have to be simultaneously addressed for any efforts implemented to have a lasting impact. The different strategies to improve care in these countries will come at different costs, different magnitude of impact and different durations of effect. Unfortunately, no silver bullet exists to improve healthcare in these countries. Only when each of these factors is addressed will the improvement of surgical care in these countries be permanent and sustainable. Each factor should therefore be considered against the background of its effectiveness, financial commitment and most importantly, its potential to impact the quality of care. Ultimately, improving surgical care in the developing world will require a multi-dimensional approach, and integration with local efforts along with a proven commitment by the entire health system is crucial to attaining the desired gains, and for the sustainability of any improvements made.2,57
This study is not without limitations; in conducting this review, the effect of the characteristics of the regional setting on the effectiveness of the various proposed interventions was not investigated. In particular, the emphasis laid on each of these identified factors by countries seeking to improve surgical outcomes may vary with differing combinations of the challenges to surgical care and this may limit the extent to which the findings in this paper can be generalized. However, the framework for the improvement of surgical care put forth in this paper can serve as a guide to policy makers in developing countries seeking to improve the quality of care that is provided within them. In particular, the framework provides a holistic view of how various interventions along the outcome improvement pathway fit together to yield improved surgical care. Future research will be helpful in identifying the factors that may accelerate the rate of improvement of surgical care in different settings.
Conclusions
Many solutions exist to improve the quality of surgical care in developing countries. However a multidimensional approach with the use of the cost-effective strategies could help achieve the lasting effect desired.
References
- 1.Ozgediz D, Jamison D, Cherian M, McQueen K. The burden of surgical conditions and access to surgical care in low- and middle-income countries. Bull World Health Organ 2008;86:646-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Farmer PE, Kim JY. Surgery and global health: a view from beyond the OR. World J Surg 2008;32:533-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taira BR, Kelly McQueen KA, Burkle FM., Jr. Burden of surgical disease: does the literature reflect the scope of the international crisis? World J Surg 2009;33:893-8. [DOI] [PubMed] [Google Scholar]
- 4.Daar AS, Singer PA, Persad DL, et al. Grand challenges in chronic non-communicable diseases. Nature 2007;450:494-6. [DOI] [PubMed] [Google Scholar]
- 5.Weiser TG, Regenbogen SE, Thompson KD, et al. An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet 2008;372:139-44. [DOI] [PubMed] [Google Scholar]
- 6.Myles PS, Haller G. Global distribution of access to surgical services. Lancet 2010; 376:1027-8. [DOI] [PubMed] [Google Scholar]
- 7.World health Organization. The World Health Report 2006 - working together for health. Geneva: World health Organization; 2006. Available from: http://www.who.int/whr/2006/en/index.html
- 8.Chirdan LB, Ameh EA, Abantanga FA, et al. Challenges of training and delivery of pedi atric surgical services in Africa. J Pediatr Surg 2010;45:610-8. [DOI] [PubMed] [Google Scholar]
- 9.Mayer ML, Beil HA, von Allmen D. Distance to care and relative supply among pediatric surgical subspecialties. J Pediatr Surg 2009;44:483-95. [DOI] [PubMed] [Google Scholar]
- 10.Zafar SN, McQueen KA. Surgery, Public health, and Pakistan. World J Surg 2011;35:2625-34. [DOI] [PubMed] [Google Scholar]
- 11.Leow JJ, Kushner AL. A President’s Emergency Plan for AIDS Relief for surgery: a call to action for surgical care in low- and middle-income countries. Arch Surg 2011;146:1003-4. [DOI] [PubMed] [Google Scholar]
- 12.Shilpakar SK. Subspecialties in neurosurgery and its challenges in a developing country. World Neurosurg 2011;75:335-7. [DOI] [PubMed] [Google Scholar]
- 13.Natuzzi ES, Kushner A, Jagilly R, et al. Surgical care in the Solomon Islands: a road map for universal surgical care delivery. World J Surg 2011;35:1183-93. [DOI] [PubMed] [Google Scholar]
- 14.Calisti A, Belay K, Mazzoni G, et al. Promoting major pediatric surgical care in a low-income country: a 4-year experience in Eritrea. World J Surg 2011;35:760-6. [DOI] [PubMed] [Google Scholar]
- 15.Cameron BH, Rambaran M, Sharma DP, Taylor RH. International surgery: the development of postgraduate surgical training in Guyana. Can J Surg 2010;53:11-6. [PMC free article] [PubMed] [Google Scholar]
- 16.Udwadia TE, Sen G. Surgical training in India. World J Surg 2008;32:2150-5. [DOI] [PubMed] [Google Scholar]
- 17.Meo G, Andreone D, De Bonis U, et al. Rural surgery in southern Sudan. World J Surg 2006;30:495-504. [DOI] [PubMed] [Google Scholar]
- 18.Archampong EQ. Surgery in developing nations. Br J Surg 2006;93:516-7. [DOI] [PubMed] [Google Scholar]
- 19.Bickler SW, Rode H. Surgical services for children in developing countries. Bull World Health Organ 2002;80:829-35. [PMC free article] [PubMed] [Google Scholar]
- 20.Aswani J, Baidoo K, Otiti J. Establishing a head and neck unit in a developing country. J Laryngol Otol 2012;126:552-5. [DOI] [PubMed] [Google Scholar]
- 21.Syed-Abdul S, Scholl J, Chen CC, et al. Telemedicine utilization to support the management of the burns treatment involving patient pathways in both developed and developing countries: a case study. J Burn Care Res 2012;33:e207-12. [DOI] [PubMed] [Google Scholar]
- 22.Kwon S, Kingham TP, Kamara TB, et al. Development of a surgical capacity index: opportunities for assessment and improvement. World J Surg 2012;36:232-9. [DOI] [PubMed] [Google Scholar]
- 23.Petroze RT, Nzayisenga A, Rusanganwa V, et al. Comprehensive national analysis of emergency and essential surgical capacity in Rwanda. Br J Surg 2012;99:436-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Loefler I. Africa--surgery in an unstable environment. ANZ J Surg 2004;74:1120-2. [DOI] [PubMed] [Google Scholar]
- 25.Arnold PC. Root causes of doctors’ dissatisfaction must be tackled to stop brain drain. BMJ. 2012;344:e190. [DOI] [PubMed] [Google Scholar]
- 26.Luboga S, Galukande M, Mabweijano J, et al. Key aspects of health policy development to improve surgical services in Uganda. World J Surg 2010;34:2511-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Contini S. Surgery in developing countries: why and how to meet surgical needs worldwide. Acta Biomed 2007;78:4-5. [PubMed] [Google Scholar]
- 28.[No authors listed] Global surgery--the final frontier? Lancet 2012;379:194. [DOI] [PubMed] [Google Scholar]
- 29.Kingham TP, Kamara TB, Cherian MN, et al. Quantifying surgical capacity in Sierra Leone: a guide for improving surgical care. Arch Surg 2009;144:122-7; discussion 128. [DOI] [PubMed] [Google Scholar]
- 30.Kushner AL, Kamara TB, Groen RS, et al. Improving access to surgery in a developing country: experience from a surgical collaboration in Sierra Leone. J Surg Educ 2010;67:270-3. [DOI] [PubMed] [Google Scholar]
- 31.Duda RBHA. Surgery in developing countries: should surgery have a role in population-based health care? Bull Am Coll Surg 2007;92:12-8. [PubMed] [Google Scholar]
- 32.Gosselin RA, Gyamfi YA, Contini S. Challenges of meeting surgical needs in the developing world. World J Surg 2011;35:258-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bickler SW, Spiegel D. Improving surgical care in low- and middle-income countries: a pivotal role for the World Health Organization. World J Surg 2010;34:386-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Quansah R, Abantanga F, Donkor P. Trauma training for nonorthopaedic doctors in low-and middle-income countries. Clin Orthop Relat Res 2008;466:2403-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Linden AF, Sekidde FS, Galukande M, et al. Challenges of surgery in developing countries: a survey of surgical and anesthesia capacity in Uganda’s public hospitals. World J Surg 2012;36:1056-65. [DOI] [PubMed] [Google Scholar]
- 36.Kruk ME, Pereira C, Vaz F, et al. Economic evaluation of surgically trained assistant medical officers in performing major obstetric surgery in Mozambique. BJOG 2007;114:1253-60. [DOI] [PubMed] [Google Scholar]
- 37.Luboga S, Macfarlane SB, von Schreeb J, et al. Increasing access to surgical services in sub-saharan Africa: priorities for national and international agencies recommended by the Bellagio Essential Surgery Group. PLoS Med 2009;6:e1000200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tollefson TT, Larrabee WF., Jr. Global surgical initiatives to reduce the surgical burden of disease. JAMA 2012;307:667-8. [DOI] [PubMed] [Google Scholar]
- 39.Dunne JA, Blackstock SJ., Re: Huijing MA, et al. Facial reconstruction in the developing world: a complicated matter [Br. J. Oral Maxillofac. Surg. 49 (2011) 292-296]. Br J Oral Maxillofac Surg 2011;49:675. [DOI] [PubMed] [Google Scholar]
- 40.Figus A, Fioramonti P, Morselli P, Scuderi N. Interplast Italy: a 20-year plastic and reconstructive surgery humanitarian experience in developing countries. Plast Reconstr Surg 2009;124:1340-8. [DOI] [PubMed] [Google Scholar]
- 41.Perkins RS, Casey KM, McQueen KA. Addressing the global burden of surgical disease: proceedings from the 2nd annual symposium at the American College of Surgeons. World J Surg 2010;34:371-3. [DOI] [PubMed] [Google Scholar]
- 42.Leow JJ, Groen RS, Kamara TB, et al. Teaching emergency and essential surgical care in Sierra Leone: a model for low income countries. J Surg Educ 2011;68: 393-6. [DOI] [PubMed] [Google Scholar]
- 43.Haglund MM, Kiryabwire J, Parker S, et al. Surgical capacity building in Uganda through twinning, technology, and training camps. World J Surg 2011;35:1175-82. [DOI] [PubMed] [Google Scholar]
- 44.Spiegel DA, Gosselin RA. Surgical services in low-income and middle-income countries. Lancet 2007;370:1013-5. [DOI] [PubMed] [Google Scholar]
- 45.Riviello R, Ozgediz D, Hsia RY, et al. Role of collaborative academic partnerships in surgical training, education, and provision. World J Surg 2010;34:459-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mock CLJ, Goosen J, Joshipura M, Peden M. Guidelines for essential trauma care. Geneva: World Health Organization; 2004. Accessed: 7 July 2012. [Google Scholar]
- 47.Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med 2009;360:491-9. [DOI] [PubMed] [Google Scholar]
- 48.Agrawal S, Maurya AK, Shrivastava K, et al. Training the trainees in radiation oncology with telemedicine as a tool in a developing country: a two-year audit. Int J Telemed Appl 2011;2011:230670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Higginson J, Walters R, Fulop N. Mortality and morbidity meetings: an untapped resource for improving the governance of patient safety? BMJ Qual Saf 2012;21:576-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vos T. Improving the quantitative basis of the surgical burden in low-income countries. PLoS Med 2009;6:e1000149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ozgediz D, Hsia R, Weiser T, et al. Population health metrics for surgery: effective coverage of surgical services in low-income and middle-income countries. World J Surg 2009;33:1-5. [DOI] [PubMed] [Google Scholar]
- 52.Rogers SO., Jr. The holy Grail of surgical quality Improvement: process measures or risk-adjusted outcomes? Am Surg 2006;72: 1046-50; discussion 1061-49, 1133-48. [PubMed] [Google Scholar]
- 53.Derbew M, Beveridge M, Howard A, Byrne N. Building surgical research capacity in Africa: the Ptolemy Project. PLoS Med 2006;3:e305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nadler EP, Nwomeh BC, Frederick WA, et al. Academic needs in developing countries: a survey of the West African College of Surgeons. J Surg Res 2010;160:14-7. [DOI] [PubMed] [Google Scholar]
- 55.Jacobs DO. Improving surgical services in developing nations: getting to go. World J Surg 2010;34:2509-10. [DOI] [PubMed] [Google Scholar]
- 56.Mills EJ, Kanters S, Hagopian A, et al. The financial cost of doctors emigrating from sub-Saharan Africa: human capital analysis. BMJ 2011;343:d7031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Clarke JR. Making surgery safer. J Am Coll Surg 2005;200:229-35. [DOI] [PubMed] [Google Scholar]


