Abstract
Dermatophyte infection is a common skin disorder. Tinea capitis, infection of the scalp and hair shaft, is the most common dermatophytosis in children aged between six months and pre-pubertal age. The aim of the study was to determine the prevalence, causative agents and to identify predisposing factors among primary school children in a rural community in Sagamu, Ogun state, Nigeria. This was a descriptive cross sectional study. Interviewer administered questionnaire was used. Following a physical examination, children with a clinical diagnosis of tinea capitis had scalp and hair scrapings for microscopy and culture. Tinea capitis was confirmed in 15.4%. Trichophyton mentagrophyte (51.7%) and Microsporum aoudouinii (20.7%) were the most prevalent organisms in this study. The most common predisposing factors were carrying of objects on the scalp; sharing of hair clippers, scissors, combs, towels and fomites. Low socioeconomic status coupled with overcrowding and poor hygiene was the major determinant of tinea capitis among the children. Tinea capitis remains a common infection among Nigerian school children. Health promotion and health education interventions are recommended to promote good hygiene, better living conditions, early identification and treatment.
Key words: tinea capitis, school children, public health, Nigeria
Introduction
Dermatophyte infection is a common skin disorder ranked amongst the top five diseases seen at dermatology clinics across Nigeria.1-3 Tinea capitis, the most common dermatophytoses in children is an infection of the scalp and hair shaft.4 Transmission can be anthropophilic, zoophilic and geophilic.4
Transmission of tinea capitis is enhanced by poor hygiene, overcrowding, contaminated hats, brushes, pillows and other inanimate objects.5 A local barber who used the same barbing equipment has been identified as the source of infection among students.6 Clinical presentation depends on the geographical location, immunity of the host, prevailing organisms in the environment and mode of transmission. In the last decade, there has been a shift in the pattern of prevalent organisms in from T. Schoenleinii in Northern Nigeria to T. rubrum and T. Canis in southern Nigeria. More recently, T. Mentagrophyte was the most common organism implicated in south western Nigeria; compared with Microsporum audouini which was the most common organism causing T. capitis in rural community in south west Nigeria several decades earlier.6 Trichophyton violaceum was found most commonly in Iran7 and Nairobi,8 whilst Microsporum canis is the commonest organism causing T. capitis in Europe.9
Clinical features of tinea capitis include scalp scaling, pruritus, cervical and occipital lymphadenopathy, alopecia (diffuse, discrete or patchy) and a boggy mass.5 A recent survey of dermatophyte infections at the skin clinic of Lagos University Teaching Hospital (LUTH) revealed that tinea capitis was found in all age groups and accounted for 72.2% of fungal infections between ages 0 and 9; while the frequency of presentation reduces with increasing age.10
The aim of the study was to determine the prevalence and causative agents of tinea capitis; and the predisposing factors among primary school students in a rural community in Sagamu, Ogun state, Nigeria.
Materials and Methods
This was a descriptive, cross sectional study involving nursery and primary school children in two primary schools in Soyindo, a rural community in Sagamu, Ogun state. Ethical approval was obtained from the Health Research and Ethics committee of Lagos University Teaching Hospital and consent was obtained from the local education authority. Written informed consent was obtained from the parents.
Interviewer administered questionnaire was used to obtain socio-demographic and clinical data from all children who had written parental consent. Exclusion criteria were non-consenting parents and non-assenting pupils. The socioeconomic status of the children was determined by parents’ occupation, level of education and living conditions.
Physical examination of each student was carried out in a well-lit room with adequate ventilation. The scalp and skin were examined for dermatophyte infections, complications of the infection and any other dermatoses. The clinical diagnosis of tinea capitis was made using the following criteria: scaly patches on the scalp, with or without hair loss; partial hair loss with broken-off hairs, brittle and lustreless hair strands, annular lesions with fairly sharp margins, massive scaling, folliculitis, kerion and favus.
Those with a clinical diagnosis of tinea capitis had scalp and hair scrapings for microscopy and culture to confirm the diagnosis. The lesions were cleaned with 70% ethyl alcohol; this is aimed at clearing out the bacterial flora and etiological bacteria of possible super infection. Skin scrapings were collected into white envelopes using the blunt edge of a sterile surgical scalpel blade (one for each child) from the erythematous, peripheral actively growing margins of the lesion. Hair samples were the dull, lustreless hair strands and the stubs were chosen and plucked using sterile forceps. The envelopes were sealed with office clips and transported to the mycology laboratory for direct microscopy and culture. All patients with tinea capitis were treated with oral griseofulvin tablets and topical antifungal agent (Whitfield’s ointment, which contains 6% w/w benzoic and 3% w/w salicylic acid).
Identification and characterization
The specimens were prepared using 20% KOH and examined with direct microscopy for presence of fungal elements. They were subsequently cultured in two Sabouraud’s dextrose agar plates (2% glucose) with chloramphenicol (50 μg/mL) media as the main isolation media and incubated at appropriate temperature. Inoculated plates were incubated at room temperature (for moulds) and 37°C (for yeast) and inspected every other day for the presence of fungal growth. The test was considered as negative for dermatophytes when no growth was seen after 4 weeks of incubation. Dermatophyte molds were identified by microscopy and their colonial morphology. No antifungal susceptibility testing was done. Isolates were stored in sabouraud slopes.
Data analysis
All data collected from the participants were entered using SPSS 15 package and analyzed using Epi-info windows version 3.5.1. Data were kept confidential at all stages of the study. Level of significance was set at 0.05.
Results
A total of 604 school children were recruited. There was an almost equal proportion of male 299 (49.5%) to female 305 (50.5%) children and the mean age was 8.1±3.1 years, with a range of 2 to 17 years. Three hundred and twenty children (53%) had a scalp lesion and of these, only 46 (14.4%) were aware of the condition, and only a small proportion had associated symptoms as shown in Table 1. Samples for KOH microscopy were taken from 201 (62.8%) of the clinically suspected tinea capitis subjects, and of these, 29 (15.4%) were mycologically proven.
Table 1.
Prevalence of scalp lesion and associated symptoms among respondents.
| Variables | Frequency | Percentage |
|---|---|---|
| Presence of scalp lesion (n=604) | ||
| Yes | 320 | 53.0 |
| No | 284 | 47.0 |
| Awareness of presence of scalp lesion (n=320) | ||
| Aware | 46 | 14.4 |
| Unaware | 274 | 85.6 |
| Presence of associated symptoms (n=320) | ||
| Itching | 18 | 5.6 |
| welling | 7 | 2.2 |
| Pain | 7 | 2.2 |
| Biting | 5 | 1.6 |
| Constitutional symptoms (fever, malaise, arthralgia) | 6 | 1.9 |
| Features of atopy | 7 | 2.2 |
| Presence of other scalp disorders (n=604) | ||
| Seborrhoeic dermatitis | 8 | 1.3 |
| Scarring alopecia | 3 | 0.5 |
| Superficial bacterial infection | 1 | 0.2 |
| Alopecia | 1 | 0.2 |
Figure 1 shows the predisposing factors to tinea capitis that were identified among the subjects. They were mostly sharing of hair clippers/scissors (52.6%) and carrying objects on the scalp (56.5%). A higher proportion of children with parents of secondary school education and under, were noted to have tinea capitis, as compared with children of parents with post secondary education. Similarly, a higher proportion of children whose mothers were senior or intermediate professionals did not have tinea capitis and higher proportions whose mothers were skilled, semi-skilled, and unskilled or unemployed had tinea capitis. These are shown in Table 2.
Figure 1.
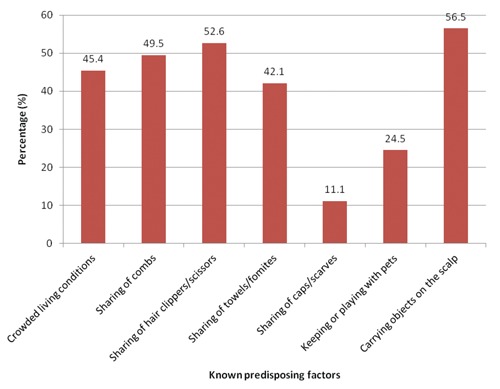
Predisposing factors to tinea infection (n=604).
Table 2.
Association between socioeconomic variables and prevalence of tinea capitis.
| Variables | Has tinea capitis Frequency (%) |
Does not have tinea capitis Frequency (%) |
Total Frequency (%) |
P-value |
|---|---|---|---|---|
| Mother’s occupation | 0.0003 | |||
| Senior professional | 3 (37.5) | 5 (62.5) | 8 (100) | |
| Intermediate professional | 14 (25.0) | 42 (75.0) | 56 (100) | |
| Junior professional/skilled | 96 (60.4) | 63 (39.6) | 159 (100) | |
| Semi-skilled | 140 (50.9) | 135 (49.1) | 140 (100) | |
| Unskilled | 8 (61.5) | 5 (38.5) | 13 (100) | |
| Housewife/student | 19 (63.3) | 11 (36.7) | 30 (100) | |
| Father’s occupation | 0.053 | |||
| Senior professional | 2 (18.2) | 9 (81.8) | 11 (100) | |
| Intermediate professional | 6 (35.3) | 11 (64.7) | 17 (100) | |
| Junior professional/skilled | 111 (53.9) | 95 (46.1) | 206 (100) | |
| Semi-skilled | 149 (53.8) | 128 (46.2) | 277 (100) | |
| Unskilled | 24 (54.5) | 20 (45.5) | 44 (100) | |
| Unemployed/student | 19 (70.4) | 8 (29.6) | 27 (100) | |
| Parents’ educational status | 0.002 | |||
| No formal | 115 (57.8) | 84 (42.2) | 199 | |
| Primary | 71 (48.0) | 77 (52.0) | 148 | |
| Secondary | 113 (58.5) | 80 (41.5) | 193 | |
| Post secondary | 21 (33.9) | 41 (66.1) | 62 | |
| Type of house | 0.102 | |||
| One room apartment | 171 (57.6) | 126 (42.4) | 297 | |
| Two room apartment | 102 (52.0) | 94 (48.0) | 196 | |
| Three room apartment | 25 (44.6) | 31 (55.4) | 56 | |
| Flat | 12 (36.4) | 21 (63.6) | 33 | |
| Bungalow | 10 (47.6) | 11 (52.4) | 21 | |
| Source of water | 0.539 | |||
| Public tap | 104 (56.5) | 80 (43.5) | 184 | |
| Borehole | 191 (52.6) | 172 (47.4) | 363 | |
| Well | 8 (66.7) | 4 (33.3) | 12 | |
| Stream | 6 (75.0) | 2 (25.0) | 8 | |
| Stored water | 131 (53.3) | 115 (46.7) | 246 | |
| Water corporation | 8 (42.1) | 11 (57.9) | 19 | |
Table 1 shows the clinical features identified among children with tinea capitis. Most (76.6%) had scaling, 38.8% had lymphadenopathy and 35.6% had patchy alopecia. Over a third, 121 (37.8%) had a wide variety of other skin conditions, the commonest being ecthyma 24 (19.8%), naevus 20 (16.5%), papular urticaria 19 (15.7%) and seborrhoeic dermatitis 15 (12.4%). Other scalp disorders noted include: scalp seborrhoiec dermatitis in 8 patients (1.3%); scarring alopecia in 3 patients (0.5%); bacterial infection in 1 patient (0.2%) and alopecia areata in 1 patient (0.2%). Among the 29 children with mycologically proven T. capitis; 18 also had clinical evidence of dermatophyte infection in other parts of the body. These include the arm 1 (5.6%); body 1 (5.6%); ear 1 (5.6%); face 6 (33.3%); feet 5 (27.8%); hands 1 (5.6%); trunk 2 (11.1%) and upper knee 1 (5.6%). This is appropriately classified as T. pedis 5 (27.8%) representing the feet; T. fascei 7 (%) representing face and ear; T. corporis 5 (%) representing body (1), arm (1), trunk (2) and upper knee (1) and T. manum 1 (5.6 %) representing the hand.
Samples were taken from 201 (62.8%) of the children with scalp lesions for KOH microscopy which showed the presence of hyphae in 15.4% (29) of the samples (Figure 2). Trichophyton mentagrophytes was the commonest organisms found in 15 samples (51.7%), followed by Microsporum audouini in 6 samples (20.7%), Trychophyton tonsurans in 5 samples (17.2%), Microsporum canis in 2 samples (6.9%), and Trichophyton rubrum in 1 sample (3.4%).
Figure 2.
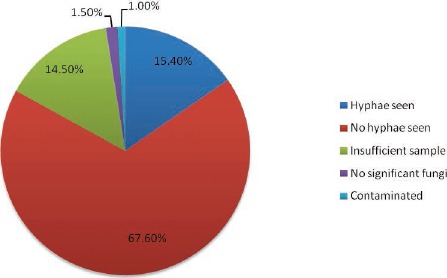
Results of microscopy of children with scalp lesions (n=201).
Discussion
Tinea capitis has been documented as a major health challenge in primary school children in Africa and all over the world, and this should be taken into consideration by health authorities concerned when planning for school health. Studies done in the US and Europe revealed that tinea capitis affects mainly African American children and migrant African children.9,11,12 The prevalence of tinea capitis varies widely in Nigeria: between 9.4% and 51.8% in the eastern part of Nigeria.13-15 In Ivory Coast, the prevalence was 11.34% and in Ethiopia a high prevalence similar to that of Ebonyi state in Nigeria was noted.16,17
Following a clinical examination, 53% of the children had features suggestive of tinea capitis. A very large percentage of samples taken from these children were noted to have microscopic negative and culture negative results (15.4% of 201 samples taken were culture positive). This is low compared to other studies both in Nigeria and other parts of the world (Forteca, Brazil, Bengal India, Saudi, and Anambra state in Nigeria).13,18,19 Factors that may be responsible for the low culture yield include: insufficient samples, non dermatophyte infections (malassezia sp. and candida sp.), contaminations (Figure 2) and prior treatment with antifungals. A study from Kwara state, Nigeria revealed that a large proportion of scalp lesions were caused by the non dermatophyte moulds.20 Herbal remedies and topical hair products with antifungal properties are available and frequently used, self prescribed by parents, families and friends for treatment of dermatophyte infections. In the negative cultures and microscopy, differentials of tinea capitis to be considered in individuals with scaly, crusted scalp with loss of hair include alopecia areata, impetigo, pediculosis, psoriasis, seborrhoeic dermatitis, traction alopecia and trichotillomania.4,5
A major determinant of the presence of tinea capitis amongst the children examined was low socioeconomic conditions, evidenced by statistically significant associations between mother’s occupation, parents’ educational status and presence of tinea capitis in the children (Table 2).
Lower occupational strata of mothers and lower educational status of parents were found to be associated with tinea capitis in children (P<0.05). A higher proportion of children whose fathers were in higher occupational strata had tinea capitis compared to those of a lower strata; this was close to being statistically significant (P=0.053).
These findings corroborate the reports of other studies in Nigeria and other African countries.16,17,21 In countries with a low prevalence of tinea capitis such as Iraq (2.7%), it was found predominantly amongst children from low socioeconomic background evidenced by low standard of living, poor hygiene, low level of parental education and overcrowded living conditions.22 A study done in Saudi Arabia revealed higher prevalence of transmissible diseases including tinea capitis in the rural areas compared to urban areas.23
The attitude of the general populace, especially the lower socioeconomic groups who are rural dwellers in Nigeria, is to ignore these lesions in their children since they are not life threatening and only attempt herbal treatment when prompted to. Despite presence of florid infections, large percentage (85.6%) of the children claimed they are not aware of the presence of tinea infection on their scalp. There appears to be some form of tolerance to the infections because of the low percentage of children with symptomatic infections (Table 1). The most common predisposing factors to tinea capitis in this study include carrying objects on the scalp and sharing of hair clippers, scissors, combs, towels and fomites. Other factors noted were overcrowding and poor hygiene (Figure 1). A report confirmed combs and hair trimming tools (which are often shared) as reservoirs for dermatophyte infection in families of previously infected individuals treated in a hospital.24 It is not uncommon in the rural setting of Nigeria and Africa, to find children carrying goods on their heads to hawk, and carry buckets which are placed in fairly unclean surroundings on their heads.
Etiological agents of Tinea capitis varies geographically and changes over time. The finding of Trichophyton mentagrophyte (51.7%) followed by Microsporum aoudouinii (20.7%) as the most prevalent organism causing tinea capitis corroborates findings from recent studies in the south western and south eastern Nigeria, while studies from the north revealed different organisms (M. ferrugineum and Trichophyton schoenleinii).13,14,20,25,26 Studies done prior to the year 2000 in Nigeria revealed that Trichophyton soudanense and Microsporum aoudouinii are the prevailing organisms causing tinea capitis and dermatophyte infections.27,28 In Ivory Coast, another West African country, Trichophyton soudanense was the most prevalent organism;16 while in Ethiopia and Libya, Trichophyton violaceum was the most common organism.17,29 Microsporum canis was noted commonly in Saudi Arabia, Asia (China) and Europe,9,23,30 and Trichophyton tonsurans in the US and Brazil.11,18
One major limitation of this study was the difficulty obtaining information from children, and thus, some of this information was collected from their teachers and older siblings. A major factor in addressing the epidemic of tinea capitis is improving the socio economic status, hygiene, and living conditions in the community studied, apart from using topical and systemic antifungal therapy. Parents and primary school children will benefit from periodic mass treatment and eventual isolation and prompt treatment of subsequent new infections.
Conclusions
Tinea capitis remains a common infection among Nigerian school children. Health promotion and health education interventions are recommended to promote good hygiene, better living conditions, early identification and treatment.
Acknowledgements
We would like to thank the pupils, parents and teachers who participated in the study and to acknowledge Dr Shiyanbola and the rest of the doctors in the dermatology unit who accompanied us to Sagamu for the study.
This study was supported financially by the authors, and we acknowledge Unique Pharmaceuticals who donated topical antifungal creams as an adjunct to treatment. This work has not been presented at any conference.
References
- 1.Nnoruka EN. Skin diseases in South-East Nigeria: a current perspective. Int J Dermatol 2005;44;29-33. [DOI] [PubMed] [Google Scholar]
- 2.Ogunbiyi AO, Daramola OOM, Alese OO. The prevalence of skin diseases in Ibadan, Nigeria. Int J Dermatol. 2004;43:31-6. [DOI] [PubMed] [Google Scholar]
- 3.Onayemi O, Isezuo SA, Njoku CH, Prevalence of different skin conditions in an outpatients setting in North- Western Nigeria. Int J Dermatol. 2005;44:7-11. [DOI] [PubMed] [Google Scholar]
- 4.Nelson MM, Martin AG, Heffernan MP. Superficial fungal infection: dermatophytosis, Tinea nigra, Piedra. : Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, Fitzpatrick’s dermatology in general medicine, 6th ed. New York: McGraw-Hill; 2003. 1989-2005. [Google Scholar]
- 5.Hainer BL. Dermatophyte infections. Am Fam Physicians. 2003;67:101-8. [PubMed] [Google Scholar]
- 6.Soyinka F. Epidemiologic study of dermatophyte infections in Nigeria (Clinical survey and laboratory investigations). Mycopathologica. 1978;63:99-103. [DOI] [PubMed] [Google Scholar]
- 7.Bassiri-Jahromi S, Khaksari AA. Epidemiolocal survey of dermatophytosis in Tehran, Iran from 2000 to 2005. Indian J Venereol Leprol. 2009;75:142-7. [DOI] [PubMed] [Google Scholar]
- 8.Chepchirchir A, BII C, Ndinya-Achola JO. Dermatophyte infections in primary school children in Kibera Slums of Nairobi. East African Med J. 2009;86:59-68. [DOI] [PubMed] [Google Scholar]
- 9.Ginter-Hanselmayer G, Weger W, Smolle J. Epidemiology of tinea capitis in Europe: Current state and changing pattern. Mycoses. 2007;50:6-13. [DOI] [PubMed] [Google Scholar]
- 10.Ayanlowo O., Akinkugbe AO. Dermatophyte infections at the Dermatology Outpatients’ Clinic of the Lagos University Teaching Hospital. Nig Qt J Hosp Med. 2013;23:1-6. [PubMed] [Google Scholar]
- 11.Magill SS, Manfredi L, Swiderski A, et al. Isolation of Trichophyton violaceum and Trichophyton soudanense in Baltimore, Maryland. J Clin Microbiol. 2007;45:461-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hallgren J, Petrini B, Wahlgren CF. Increasing tinea capitis prevalence in Stockholm reflects immigration. Med Mycol. 2004;42:505-9. [DOI] [PubMed] [Google Scholar]
- 13.Emele FE, Oyeka CA. Tinea capitis among primary school children in Anambra state of Nigeria. Mycoses. 2008;51:536-41. [DOI] [PubMed] [Google Scholar]
- 14.Achufus IJ, Nwobu RA, Okonkwo JC. Tinea capitis among primary school children in Onitsha North and Ogbaru local government areas of Anambra state, Nigeria. J Biomed Invest. 2006;4:28-31. [Google Scholar]
- 15.Uneke CJ, Ngwu BA, Egemba O. Tinea capitis and Pityriasis versicolor infections among school children in the South-Eastern Nigeria: the Public Health implications. Internet J Dermatol. 2006;4:2. [Google Scholar]
- 16.Ménan EI, Zongo-Bonou O, Rouet F, et al. Tinea capitis in schoolchildren from Ivory Coast (Western Africa). A 1998-1999 cross-sectional study. Int J Dermatol. 2002;41: 204-7. [DOI] [PubMed] [Google Scholar]
- 17.Ali J, Yifru S, Woldeamanuel Y. Prevalence of tinea capitis and the causative agent among school children in Gondar, North West Ethiopia. Ethiop Med J. 2009;47:261-9. [PubMed] [Google Scholar]
- 18.Brilhante RSN, Cordeiro RA, Rocha MFG, et al. Tinea capitis in a dermatology center in the city of Fortaleza, Brazil: the role of Trichophyton tonsurans. Int J Dermatol. 2004;43: 575-9. [DOI] [PubMed] [Google Scholar]
- 19.Kundu D, Mandal L, Sen G. Prevalence of Tinea capitis in school going children in Kolkata, West Bengal. J Nat Sc Biol Med. 2012;3:152-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Adefemi SA, Odeigah LO, Alabi KM. Prevalence of dermatophytosis among primary school children in Oke-oyi community of Kwara state. Niger J Clin Pract. 2011;14:23-8. [DOI] [PubMed] [Google Scholar]
- 21.Amoran OE, Runsewe-Abiodun OO, Mautin AO, Amoran IO. Determinants of dermatological disorders among school children in Sagamu, Nigeria. Educ Res. 2011;2:1743-8. [Google Scholar]
- 22.Fathi HI, al-Samarai AG. Prevalence of tinea capitis among schoolchildren in Iraq. East Mediterr Health J. 2000;6:128-37. [PubMed] [Google Scholar]
- 23.Amin TT, Ali A, Kaliyadan F. Skin disorders among male primary school children in Al Hassa, Saudi Arabia: prevalence and sociodemographic correlates - a comparison of urban and rural populations. Rural Remote Health. 2011;11:1517. [PubMed] [Google Scholar]
- 24.Winge MCG, Chryssanthou E, Wahlgren C. Combs and hair-trimming tools as reservoirs for dermatophytes in juvenile Tinea capitis. Acta Derm Venereol. 2009;89:536-7. [DOI] [PubMed] [Google Scholar]
- 25.Anosike JC, Keke IR, Uwaezuoke JC, et al. Prevalence and distribution of ringworm infections in Primary school children in parts of Eastern, Nigeria. J Appl Sci Environ Manag. 2005;9:21-5. [Google Scholar]
- 26.Nweze EI. Etiology of dermatophytoses amongst children in north eastern Nigeria. Med Mycol. 2001;39:181-4. [DOI] [PubMed] [Google Scholar]
- 27.Obasi OE, Clayton YM. Dermatophyte fungi in the Guinea Savannah region of Nigeria and the changing phase of dermatophytosis in Nigeria. Mycoses. 1989;32: 381-5. [PubMed] [Google Scholar]
- 28.Ayanbimpe GH, Bello CSS, Gugnani HC. The aetiological agents of superficial cutaneous mycoses in Jos, Plateau State of Nigeria. Mycoses. 1995;38:235-7. [DOI] [PubMed] [Google Scholar]
- 29.Gargoom AM, Elyazachi MB, Al-Ani SM, Duweb GA. Tinea capitis in Benghazi, Libya. Int J Dermatol. 2000;39:263-5. [DOI] [PubMed] [Google Scholar]
- 30.Zhu M, Li L, Wang J, et al. Tinea capitis in South eastern China: a 16-year survey. Mycopathologia. 2010;169:235-9. [DOI] [PubMed] [Google Scholar]


