Abstract
The availability of mortality data for any society plays an essential role in health monitoring and evaluation, as well as in the design of health interventions. However, most resource-poor countries such as Ghana have no reliable vital registration system. In these instances, verbal autopsy (VA) may be used as an alternative method to gather mortality data.
In rural Ghana, the research team utilized a VA questionnaire to interview caretakers who were present with a child under the age of five prior to death. The data was given to two physicians who independently assigned the most probable cause of death for the child. A third, blinded physician analyzed the data in the cases where the first two physicians disagreed. When there was agreement between physicians, this was assigned as the cause of death for the individual child. During the study period, we recorded 118 deaths from 92 households. Twenty-nine (24.6%) were neonatal deaths with the leading causes of death being neonatal sepsis, birth asphyxia and pneumonia. The remaining 89 (75.4%) were post-neonatal deaths with the most common causes of death being pneumonia, malaria and malnutrition. While 63/118 (53.4%) deaths occurred in the home, there is no statistically significant relationship between the location of the home and the time of travel to the nearest health facility (P=0.132). VA is an important epidemiological tool for obtaining mortality data in communities that lack reliable vital registration systems. Improvement in health care is necessary to address the large number of deaths occurring in the home.
Key words: verbal autopsy, causes of death, neonates, post-neonates, Barekese, Ghana.
Introduction
Knowledge concerning the causes of childhood deaths in a given population is vital for effective allocation of health resources. In many areas, the ability to determine causes of mortality is nearly impossible. Over 57 million deaths occur worldwide each year1 and in the year 2008, 8.1 million deaths occurred among children under the age of five.2 Information concerning the cause of death is only available in one-third of all deaths.1 Many developing nations do not have a reliable and consistent approach to collecting information regarding causes of death, especially in rural areas. Regional coverage of death registration varies from close to 100% in Europe to around 50% in the Asia-Pacific region to less than 10% in Africa.3
Verbal autopsy (VA) is an indirect method of assigning a probable cause of death based on medical signs and symptoms that occurred during the period leading up to an individual's death.4 This information is obtained by interviewing someone who was present with the decedent around the time of death, and it is then interpreted by medical experts to ascertain a probable cause of death.4 VA is currently used in over 42 Demographic and Health Surveillance Sites in 19 countries, as well as by the Sample Registration System Sites in India and the Disease Surveillance Points System in China.5–7 It is estimated that VA was used to determine causes of death for approximately one-quarter of the global deaths in 2004.3
Based on guidelines issued by the World Health Organization (WHO), VA consists of a series of open-ended questions, in which the respondents recall information without prompting by the interviewer, and close-ended questions.8 The close-ended questions are structured in ways that allow the respondents to better recollect information that they may have forgotten to mention. Administration of a VA questionnaire should be performed by a trained interviewer educated in VA methods and the interview should be conducted in the native language of the primary respondent.9
While Ghana is one of the most rapidly developing countries in Western Africa, it faces challenges with regards to obtaining data about causes of death and disease burden. Of the 8.1 million children who died in 2008, 50,000 of these deaths occurred in Ghana.10
In Ghana, many of these deaths go unreported due to the complicated nature of officially reporting the event. The process includes reporting to the correct births and deaths registry, and obtaining a medical certificate from either a medical practitioner or coroner detailing the cause of death;11 thus, only 15.8% of all deaths in Ghana are reported.12
The objective of this study was to use VA methods to determine the common causes and setting of death for children under the age of five in selected rural communities in the Barekese sub-district of Ghana. Additionally, the study explores the association between location of death and the distance between the child's home and the nearest health center.
Materials and Methods
This study was conducted in the Barekese sub-district, which also serves as the Barekuma Community Collaborative Development Project (BCCDP) site in the Atwima Nwabiagya district in the Ashanti region of Ghana.13,14 The communities were purposely selected from within the BCCDP site to sample those with the greatest geographical barriers to accessing healthcare. Communities were categorized into two groups, taking into consideration the travel time by car from each community to the Barekese Community Health Center (BCHC), the nearest community health facility within the vicinity. The two groups were defined as communities less than or more than a 15-minute drive to the health facility. These times were chosen arbitrarily and could vary based on the prevailing weather conditions, access to public transport and the road terrain. The research team used the WHO's questionnaire designed for conducting VA.15 The questionnaire was reviewed by Ghanaian and US physicians and public health experts and deemed appropriate for use in the communities where the study took place.
Respondents were located by going door-to-door within the community and from referrals from local community members and leaders, who had some prior knowledge of households where deaths had occurred during the defined study period. The response rate was 100%.
The selection criteria for participation in the study included the following: i) the child was no more than five years of age at the time of death; ii) the death occurred within the past five years (August 2005–August 2010); iii) the child's parents are permanent residents of the community and; iv) the deceased child was a permanent resident of the community, regardless of the ultimate location of death. As part of the interview process, the interviewer requested to see copies of the health records to validate the child's birth date, other demographic information and any notes recorded by medical professionals. However, in most cases, these records were destroyed or not taken from the hospital with the explanation that retaining any of the lost child's belongings causes grief for the bereaved family. Upon completion of the survey, the questionnaires were then given to two pediatric physicians who independently assigned a probable cause of death for each case. Each physician provided at most two likely causes of death for each child. The results from the two physicians were then collated, and in those cases where the two physicians agreed, a cause of death was assigned. In the situation where the two physicians did not agree on a cause of death for a particular case, a third physician, blinded to the other physician's diagnoses, assigned a cause of death. The results from the third physician were then compared with the diagnoses from the first two physicians. In each case, the results of the third physician agreed with one of the first two physicians, thus providing a majority diagnosis that was used (Figure 1).
Figure 1.
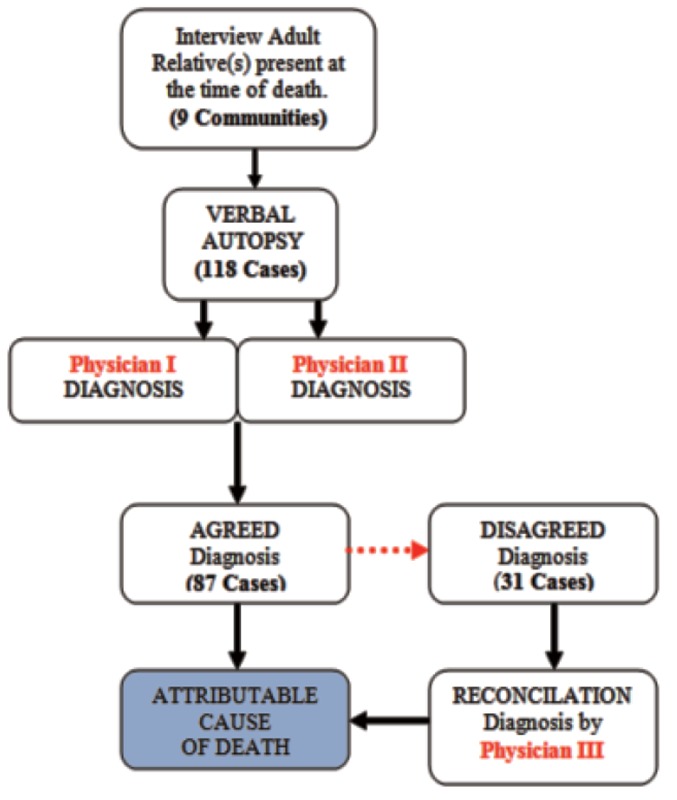
Methodology for assigning cause of death.
Data analysis
Data gathered from the VA questionnaire and causes of death were coded and entered into STATA statistical software package (StataCorp. 2007, Stata Statistical Software: Release 10. College Station, TX, USA: StataCorp LP) for analysis. Cross-tabulations were used to examine the distribution of causes of death and place of death by case type (i.e., neonates and post-neonates). Frequencies and percentages were also computed on the number of diagnoses on which the physicians agreed or disagreed, and other basic demographic information of the respondents such as age, number of years in school and number of individuals present at the time of the interview.
Ethical clearance
The study had ethical approval from the University of Utah (U of U) Institutional Review Board and joint approval from the ethics committees of the Kwame Nkrumah University of Science of Technology (KNUST) and the Komfo Anokye Teaching Hospital (KATH) in Ghana. With the help of local interpreters, administration of the consent was conducted verbally to the adult respondent present with the child prior to death. Consideration was given to the sensitivity of the situation by allowing respondents to terminate or reschedule the interview at any time. If respondents became emotional or showed any hesitation, they were informed that the interview could be terminated if they did not want to continue. In all cases, those being interviewed elected to complete the survey. As part of a predetermined protocol, the interviewer had the responsibility to always show empathy to the family.
Results
At the end of the study period, 118 cases were reported from 92 households within the communities that participated. Out of these reported cases, 29 (24.6%) were classified as neonatal deaths (died within the first 28 days of life), while the remaining 89 (75.4%) were identified as post-neonatal deaths (died between 29 days and 5 years of life). Further classification of the deceased children by gender indicated that 63 (53.4%) of the recorded cases were males and the remaining 55 cases (46.6%) were females (Table 1). Analysis of the demographics of the interviewed respondents in the study showed 13 (11.0%) were males and 105 (89.0%) were females. The average amount of education for all respondents was about six years. On average, males had approximately two more years of education than females. Further distribution on the number of years of education of all respondents showed that 23 (19.5%) had no formal education. However, 20 (17.0%) had ten or more years of education. With regards to the child's health records, only 23 (19.5%) of the total respondents were able to show proof of available medical records on the deceased child. However, the available medical records contained limited information and could not be used to validate reviewer responses. However, of the 19 respondents who indicated that they had been issued a death certificate at the time of the child's death, none was able to show this record of death at the time of interview (Table 1). The distribution of the cases with reference to their proximity to the BCHC showed that 51 (43.2%) deaths occurred in locations with more than 15 min traveling time by car to the facility and the remaining 67 (56.8%) occurred in communities with less than 15 min driving time. Further study into the locations where these deaths occurred revealed that 38/67 (56.7%) cases that happened less than a 15-minute drive from the health facility occurred in the home, and 25/51 (49.0%) deaths in the greater than a 15-minute drive category occurred in the home. In all, there were 47 hospital-reported deaths (39.8%), and 63 (53.4%) home-reported deaths (Table 2).
Table 1. Subject and respondent characteristics.
| Characteristics of children (n=118) | |
|---|---|
| Sex | |
| Male | 63 (53.4%) |
| Female | 55 (46.6%) |
| Case type | |
| Neonate | 29 (24.6%) |
| Post-neonate | 89 (75.4%) |
| Place of death | |
| Hospital | 47 (39.8%) |
| Other health facility | 5 (4.2%) |
| Enroute to hospital | 3 (2.5%) |
| Home | 63 (53.4%) |
| Health records available | |
| Yes | 23 (19.5%) |
| No | 95 (80.5%) |
| Issued death certificates | |
| Yes | 19 (16.1%) |
| No | 99 (83.9%) |
| Characteristics of respondents (n=118) | |
|---|---|
| Sex | |
| Male | 13 (11.0%) |
| Female | 105 (89.0%) |
| Age group | |
| ≤ 30 yrs | 44 (37.3%) |
| 31–45 yrs | 38 (32.2%) |
| ≥ 46 yrs | 36 (30.5%) |
| Relationship to child | |
| Mother | 95 (80.5%) |
| Father | 12 (10.2%) |
| Grandmother | 6 (5.1%) |
| Grandfather | 1 (0.9%) |
| Aunt | 4 (3.4%) |
| Years of education | |
| 0 years | 23 (19.5%) |
| 1–6 years | 42 (35.6%) |
| 7–9 years | 33 (28.0%) |
| 10–15 years | 20 (17.0%) |
| Years of education | 5.9 yrs, 4.0 (mean, sd) |
| Travel time by car to health clinic | |
| Less than 15 min | 67 (56.8%) |
| More than 15 min | 51 (43.2%) |
Table 2. Distribution of place of death by category.
| Community | Hospital | Other health facilities | Enroute to hospital | Home | Total |
|---|---|---|---|---|---|
| Less than 15 min | 25 | 4 | 0 | 38 | 67 |
| More than 15 min | 22 | 1 | 3 | 25 | 51 |
| Total | 47 | 5 | 3 | 63 | 118 |
There is no statistically significant relationship between the location of death and the time of travel to the health facility (P=0.132). There is also no significant relationship between the respondent's years of education and the place where the death of the child occurred (P=0.283). However, there is a slightly negative correlation (r=−0.13) between the respondent's years of education and travel time to the BCHC, which could imply the higher the education level, the less likely individuals are to live in places further away from the facility.
Figures 2 and 3 show the distribution of the causes of deaths by case type. Of the 29 neonatal deaths, the most commonly assigned causes of death were neonatal sepsis, birth asphyxia and pneumonia. There were 12 (41.4%) reported cases of neonatal sepsis, 10 (34.5%) cases of birth asphyxia and 4 (13.8%) cases of pneumonia. Among the post-neonates, the top three most commonly-assigned causes of death were pneumonia, malaria and malnutrition. Among the 89 reported post-neonatal deaths, there were 29 (32.6%) deaths due to pneumonia, 18 (20.2%) deaths due to malaria, 14 (15.7%) malnutrition-attributable deaths, 11 (12.4%) meningitis cases, 6 (6.7%) deaths due to diarrhea, and 4 (4.5%) measles reported deaths.
Figure 2.
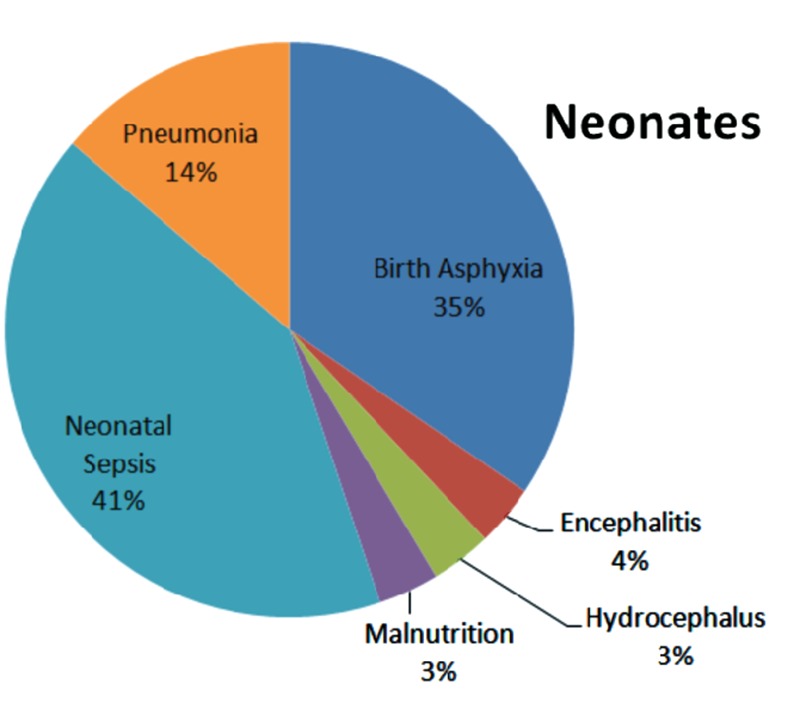
Causes of death among neonates.
Figure 3.
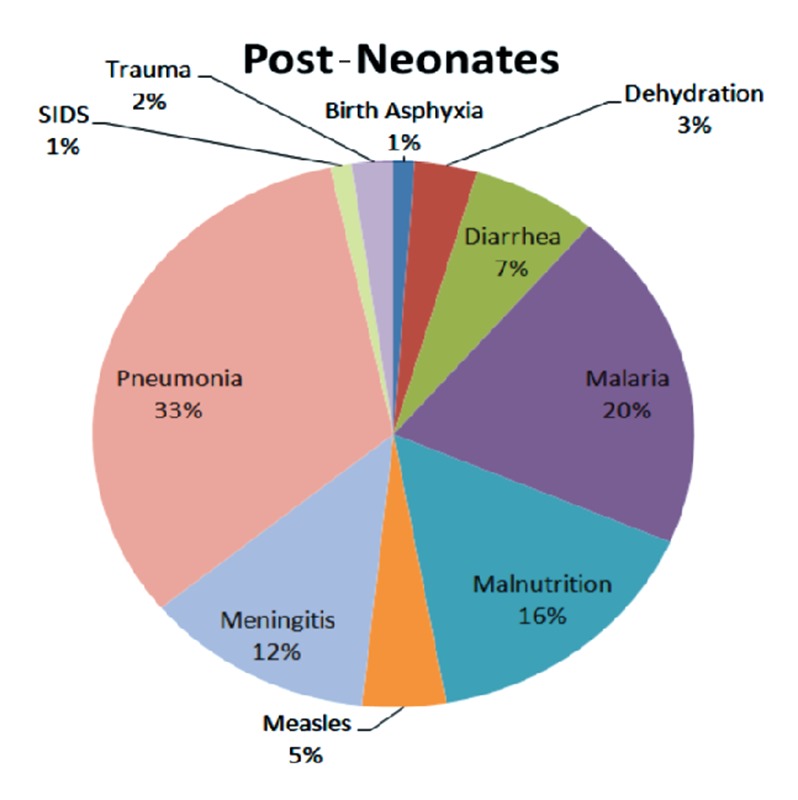
Causes of death among post-neonates.
Further data analysis, to determine how the physicians compare on their initial assigned probable causes of death, revealed a correlation coefficient of 0.7 between physician I and physician II, signifying a high positive correlation between the assigned diagnoses. Physician I and II agreed on 87/118 (73.7%) cases by first attempt. Of the remaining 31 cases, physician III agreed with physician I on 14/31 (45.2%) cases and physician II on 17/31 (54.8%) cases; there were no new causes of death introduced by physician III. Figure 4 shows the distribution of the overall causes of death as assigned by the first two physicians.
Figure 4.

Distribution of diagnoses by physicians I and II.
Discussion
In most developing countries such as Ghana, childhood deaths are too often attributable to preventable causes.16 However, most of these deaths are unreported, leading to difficulties in designing effective intervention programs and allocating resources. The challenges stem from the fact that these regions often do not have a reliable vital statistics system that collects and maintains basic demographic information and health records on individual inhabitants. Contributing factors to these problems include the low population literacy rates, a cumbersome system of vital registration and the poor infrastructure in these resource-limited settings. This fact was solidified over the course of our project where the respondent's average number of years completed in the education system was approximately six years. The consequential effect of a limited education is seen in the quality of information provided during the VA interview, as most of the respondents could not give the exact death date of their child.
From our study, it was determined that there were three-times as many post-neonatal deaths as neonatal deaths. For the purposes of this study, a neonatal death is defined as a death occurring on or before 28 days of life, and a post-neonatal death is defined as a death occurring between the 29th day of life and the 5th year of life. This age distribution of deaths is consistent with similar studies conducted in both the West African sub-region17 and among other similar socioeconomic countries in Southern Asia.18
It was determined that more than half of the total deaths occurred at home. This could be attributed to many factors including: i) families are not recognizing severely ill children and are not seeking timely medical attention; ii) families are recognizing severely ill children and are not or cannot access advanced health care; iii) families are recognizing severely ill children and are seeking care too late or from inappropriate providers and iv) families are recognizing severely ill children and are seeking appropriate care, but care is inadequate. These issues require further research, but could lead to valuable community education efforts.
Another interesting observation came from analyzing the cases in respect to their proximity to the BCHC. Cases in the closest (less than 15 min driving time) and farthest (more than 15 min driving time) proximity recorded 38 (60.3%) and 25 (39.7%), respectively, out of the 63 deaths that occurred at home. By word of caution, the travel times used for the analysis were chosen based on the researchers' traveling times between the communities and the health facility. The actual estimate for the inhabitants who have no private vehicular traveling means depends on finances, social network, availability of local transport, the prevailing weather conditions and time of day or night. Although proximity to the BCHC would theoretically enable families easier access to the facility, our study revealed anecdotal information regarding affordability of care and failure to recognize life-threatening conditions as barriers to care seeking. Therefore, there may be the need to intensify public education to help parents identify alarm symptoms of illnesses in children and to seek medical attention as early as possible.
With the help of local interpreters, most of the interviews were conducted without problems. However, there were instances where some of the scientific terms used in the questionnaire had no direct local correlate and thus, were difficult for interpreters to explain. We recommend that future researchers in related studies in these communities take the initiative of researching more local names for medical and scientific terminologies and also have more interpreter training time before executing any study.9
Our findings indicate the majority of deaths in the study region were due to causes that are treatable or preventable when interventions such as basic newborn resuscitation by skilled attendants for birth asphyxia, immunizations and antibiotic treatment for infections are administered.19 By sharing these results with the community leaders and the local health authorities, we hope our study will influence priority settings and interventions that will help reduce the number of deaths among children in the sub-district and beyond.
The study identified four deaths due to measles in the study area. It is worth noting that the Ministry of Health in Ghana has reported zero measles-related deaths in the past eight years.20 Verbal autopsy cannot confirm the diagnosis of disease, and therefore these findings must be interpreted with caution. An active case reporting system is recommended as it would facilitate the ascertainment of causes of death due to measles and other communicable disease which are on the verge of eradication in the country.
Limitations
Our study had several limitations. First, our sample size was limited to 118 cases from 92 households within the Barekese sub-district. The small sample size lends to greater variability and less precision amongst the common causes of death within the area and impacts the external validity of the study results. Second, the information gathered from family members was subject to recall bias. The study attempted to reduce the recall bias by restricting the time frame of deaths to the five years preceding the interview date. Third, while we used trained medical professionals from the region to serve as interpreters, there was no standardized training on utilization of the verbal autopsy questionnaire. This may have led to differences among interpreters and their explanations of certain symptoms to respondents, as well as the terminology used to describe various situations. Fourth, while assigning a single cause of death may facilitate an understanding of local child survival epidemiology, in reality many deaths are multi-factorial and synergistic, especially deaths due to infection among undernourished children.21 Finally, it is possible that the training backgrounds of the physicians who diagnosed the cases could have had some effect on their findings. Physician I and III are US-trained pediatricians while physician II is a Ghanaian-trained pediatrician. However, physicians I and II independently assigned the same diagnosis approximately 75% of the time. The fact that the third physician did not add a third diagnosis on the contested cases does imply an intra-physician precision, despite the differences in their experience and education.
Conclusions
The need for cause of death information to facilitate health planning, priority setting, monitoring and evaluation in trends of disease outbreaks and to support policy and program development is essential. However, most developing countries such as Ghana lack a reliable vital registration system for this cause. This can be attributed to high cost for establishing and maintaining such systems for public health purposes, as well as the poor infrastructure of the country.22 VA is now widely used as an effective epidemiological tool in research in most resource-poor settings to collect such vital data.
From this study, pneumonia, malaria, malnutrition, neonatal sepsis and birth asphyxia were determined to be the major causes of death among children under the age of five years who died between August 2005 and August 2010 in the Barekese sub-district in Ghana. Although more studies need to be completed to understand the cultural practices and health beliefs of the members of these communities, we believe the findings from this study are important and informative. We hypothesize that improvement in health care at multiple levels is necessary to address the large number of deaths occurring in the home through: i) improved recognition and care seeking for childhood illnesses by care-giving families; ii) improved quality of care at all referral levels and iii) improvements in referral systems including transportation and communication.
Acknowledgements:
the authors would like to acknowledge the residents of the Barekese sub-district in the Ashanti region of Ghana for their commitment and support during the study. They also want to express their appreciation to Amalia Brown, Erik Hasenoehrl, Michael Stevens, Abigail Antwi and Smart Nkansah for their assistance in the data collection. Many thanks to Isaac Boakye and Bernard Arhin for coordinating the study and facilitating the local IRB process.
References
- 1.World Health Organization. The world health report 2004 - changing history. Available from: http://www.who.int/whr/2004/en/
- 2.UNICEF. Global child mortality continues to drop. 2009 Available from: http://www.unicef.org/media/media_51087.html.
- 3.Mathers CD, Boerma T, Ma Fat D. Global and regional causes of death. Br Med Bull. 2009;92:7–32. doi: 10.1093/bmb/ldp028. [DOI] [PubMed] [Google Scholar]
- 4.Baiden F, Bawah A, Biai S, et al. Setting international standards for verbal autopsy. Bull World Health Organ. 2007;85:570–1. doi: 10.2471/BLT.07.043745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang G, Hu J, Rao KQ, et al. Mortality registration and surveillance in China: History, current situation and challenges. Popul Health Metr. 2005;3:3–3. doi: 10.1186/1478-7954-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jha P, Gajalakshmi V, Gupta PC, et al. Prospective study of one million deaths in India: rationale, design and validation results. PLoS Med. 2006;3:e18–e18. doi: 10.1371/journal.pmed.0030018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Indepth Network. An international network of field sites with continuous demographic evaluation of populations and their health in developing countries. Available from: http://www.indepth-network.org/
- 8.Joshi R, Kengne AP, Neal B. Methodological trends in studies based on verbal autopsies before and after published guidelines. Bull World Health Organ. 2009;87:678–82. doi: 10.2471/BLT.07.049288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Soleman N, Chandramohan D, Shibuya K. Verbal autopsy: current practices and challenges. Bull World Health Organ. 2006;84:239–45. doi: 10.2471/blt.05.027003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.UNICEF. At a glance: Ghana - Statistics, 2010. Available from: http://www.unicef.org/infobycountry/ghana_statistics.html.
- 11.Service OotHC. Births and Deaths Registry, 2007. Available from: http://www.bdrghana.gov.gh/
- 12.Tradig Economics. Completeness of total death reporting (Percentage of reported total deaths to estimated total deaths) in Ghana. 2002 Available from: http://www.tradingeconomics.com/ghana/completeness-of-total-death-reporting-percent-of-reported-total-deaths-to-estimated-total-deaths-wb-data.html.
- 13.Crookston BT, Alder SC, Boakye I, et al. Exploring the relationship between chronic undernutrition and asymptomatic malaria in Ghanaian children. Malar J. 2010;9:39–39. doi: 10.1186/1475-2875-9-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Schweinitz P, Ansong D, Manortey S, et al. Evaluating international collaboration: differential perceptions of partnership in a CBPR project in Ghana. J Empir Res Hum Res Ethics. 2009;4:53–67. doi: 10.1525/jer.2009.4.4.53. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. A standard verbal autopsy method for investigating causes of death in infants and children. Available from: http://www.who.int/csr/resources/publications/surveillance/WHO_CDS_CSR_ISR_99_4/en/index.html.
- 16.Adams I, Darko D, Accorsi S. Assessing efficiency in service delivery. Ghana Health Service Publication. 2004 [Google Scholar]
- 17.Black RE, Cousens S, Johnson HL, et al. Global, regional, and national causes of child mortality in 2008: A systematic analysis. Lancet. 2010;375:1969–87. doi: 10.1016/S0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]
- 18.Rajaratnam JK, Marcus JR, Flaxman AD, et al. Neonatal, postneonatal, childhood, and under-5 mortality for 187 countries, 1970–2010: a systematic analysis of progress towards Millennium Development Goal 4. Lancet. 2010;375:1988–2008. doi: 10.1016/S0140-6736(10)60703-9. [DOI] [PubMed] [Google Scholar]
- 19.Jones G, Steketee RW, Black RE, et al. How many child deaths can we prevent this year? Lancet. 2003;362:65–71. doi: 10.1016/S0140-6736(03)13811-1. [DOI] [PubMed] [Google Scholar]
- 20.Ghana Ministry of Health. Annual Report 2008. Available from: http://www.mohghana.org/UploadFiles/Publications/ANNUALREVIEWREPORT2008090825071054.pdf.
- 21.Black RE, Morris SS, Bryce J. Where and why are 10 million children dying every year? Lancet. 2003;361:2226–34. doi: 10.1016/S0140-6736(03)13779-8. [DOI] [PubMed] [Google Scholar]
- 22.Yang G, Rao C, Ma J, et al. Validation of verbal autopsy procedures for adult deaths in China. Int J Epidemiol. 2006;35:741–8. doi: 10.1093/ije/dyi181. [DOI] [PubMed] [Google Scholar]


