Abstract
Objective
To describe the cause-specific morbidity and mortality, and referral patterns of all neonates admitted to a tertiary referral hospital in the northern provinces of Vietnam.
Design
A prospective hospital based observational study.
Setting
The Neonatal Department, National Hospital of Pediatrics, Hanoi, Vietnam.
Patients
All admissions to the Neonatal Department over a 12 month period.
Main outcome measures
Cause-specific morbidity and mortality; deaths.
Results
There were 5064 admissions with the commonest discharge diagnoses being infection (32%) and prematurity (29%). The case fatality ratio (CFR) was 13.9% (n = 703). Infection (38%), cardio/respiratory disorders (27%), congenital abnormalities (20%) and neurological conditions (10%) were the main causes of death. Of all the deaths, 38% had an admission weight ≥2500g. Higher CFR were associated with lower admission weights. Very few deaths (3%) occurred in the first 24 hours of life. Most referrals and deaths came from Hanoi and neighbouring provincial hospitals, with few from the most distant provinces. Two distant referral provinces had the highest CFR.
Conclusions
The CFR was high and few deaths occurred in neonates <24 hours old. The high rates of infection call for an improvement in infection control practices and peripartum antibiotic use at provincial and tertiary level. Understanding provincial hospital capacity and referral pathways is crucial to improving the outcomes at tertiary centres. A quality of care audit tool would enable more targeted interventions and monitoring of health outcomes.
Introduction
The slow decline in neonatal mortality impeded the attainment of Millennium Development Goal 4 for many countries. Globally, most neonatal deaths are due to prematurity (36%) infections (23%), asphyxia (23%), and congenital malformations (10%) [1, 2]. Data on cause-specific mortality is important for health planning as specific interventions are available, even in the most poorly resourced settings, to prevent and treat many of these conditions [3].
The postnatal period has been identified as a significant gap in service provision [4]. The recognition and management of common neonatal conditions requires clinical expertise and training, access to suitable equipment, and efficient referral pathways [5, 6]. To ensure health care is of sufficient quality, it is important to monitor outcomes of care provided [7], and then use this information to strategically determine which interventions should be prioritized.
Vietnam is a lower-middle income country (LMIC) and has shown substantial reductions in child mortality. The Neonatal Mortality Rate (NMR) is 11 per 1,000 live births in Vietnam, although population based studies show considerable regional variation [8, 9]. In Vietnam, over 90% of births occur in health facilities [10]. However most published data on neonatal health in Vietnam is community based [11–14]. Community based studies from rural northern Vietnam have linked neonatal mortality with ethnicity, place of birth and a poor referral system[15]. Provincial hospitals with newborn care units are often not equipped to treat or have training to care for many neonatal conditions (Khu, pers. comm.). Furthermore, families frequently bypass their local hospital and self-refer to major hospitals that are far away; this can result in a deterioration in the condition of neonates as safe transport systems are underdeveloped (Khu, pers. comm.). There are few published data on cause-specific neonatal morbidity and mortality, despite most deaths occurring in the hospital setting, particularly in northern Vietnam. The aim of this study is to describe the cause-specific morbidity and mortality, and referral patterns of all admissions to the largest neonatal unit in northern Vietnam.
Methods
Study site
The National Hospital of Pediatrics (NHP), Hanoi, is the leading pediatric department in Vietnam [16]. It is a tertiary referral centre for northern Vietnam and all neonates admitted to the Neonatal Department are born off-site. There are 25 provinces in northern Vietnam with a total population of approximately 37, 285,400 [17]. Each province has provincial and district hospitals. For convenience, hospital referring from Hanoi Province in this study are categorised as provincial hospitals. The Neonatal Department has 140 beds but can have a bed occupancy of up to 270 patients. The department has a nurse to patient ratio of 1:11. All doctors undergo neonatal training.
The Neonatal Department has access to advanced diagnostics including molecular microbiology, genetic testing and radiological imaging. Treatment options include: oxygen, artificial ventilation, intravenous and nasogastric therapy, exogenous surfactant, antibiotics, phototherapy, exchange transfusion, parenteral nutrition, and surgical procedures for congenital anomalies and cardiac defects.
Study design
This was a 12-month prospective hospital based observational study of all neonates admitted to the Neonatal Department, NHP, between the 1st of July, 2011 and 30th of June, 2012. Outcomes were monitored until the 17th of August, 2012. In this study all participants are termed “neonates”, for convenience, even though some may have been older than 28 days.
Data collection
Demographic and clinical details were extracted from each neonate’s medical record. Admission weight was collected as reliable birth weight information was not available for all neonates as all were outborn and birthweight was either not recorded or not always available. Gestational age is not routinely recorded.
Discharge diagnoses were categorised using the Perinatal Society of Australia and New Zealand Mortality classification system (PSANZ-NDC), 2009 [18] by co-author (MM) using the primary discharge diagnosis. These classifications included congenital abnormality, extreme prematurity, prematurity, cardio/respiratory disorders, infections, neurological, gastrointestinal, other, and unknown.Neonates who had a discharge diagnosis of “prematurity” were classified as “extreme prematurity” if the admission weight was ≤600g as per PSANZ-NDC, or “premature” if no other discharge diagnosis was recorded. Neonates who had a discharge diagnosis of “jaundice” were classified as “other” if no other diagnostic information was available.
An outcome of death was recorded for any neonate who died, or was discharged home to die. All deaths were identified by a Vietnamese neonatal doctor (LTH), who attended the ward’s handover each week-day and reviewed all medical records. Deaths were classified using the PSANZ-NDC system. Pneumonia was classified as “”Infection: Other” unless the aetiology (acquired or congenital) was known. For “extreme prematurity” classifications, the admission weight was checked to ensure it was <600g. In cases where the admission weight was >600g, cause of death was reclassified as “unknown” if no other discharge diagnosis was recorded.
Data management
Data for all admissions and deaths were entered in Excel and EpiData version 3.1, respectively, then transferred to STATA Version 12.1 for cleaning and analysis. Any discrepancies were re-checked against the medical record.
Statistical analysis
Continuous data were summarised as medians and inter-quartile ranges. Categorical data were summarised by number and proportion of cases for each variable. Categorical data were compared using a Chi Square Test, or Fisher’s exact test, where appropriate. STATA Version 12.1 was used to map home province.
Ethical approval
Ethics approvals were gained from the NHP Ethics Committee, Hanoi, and the Monash University Health Research Ethics Committee, Melbourne, Australia. No individual consent was obtained as this study was deemed by the local ethics committee as an audit, with individual consent not being required.
Results
There were 5064 neonates admitted to NHP, and 703 died (CFR 13.9%). Table 1 shows the features of all admissions and deaths. More than half of all admissions (56.7%) were referred from provincial hospitals and 24% were self-referred. Most deaths (87.1%) were referred from provincial hospitals, with CFR of 21.3%, (n = 612). The CFR for admissions that had been self-referred (n = 1214) was lower (3.4%). Nearly half of admissions (49.9%) and 88.5% of neonates who subsequently died, were transferred by ambulance.
Table 1. Demographic, referral, and clinical features of all admissions and deaths to the Neonatal Department, National Hospital of Pediatrics, between 1st July 2011 and 30th June 2012.
| Demographic features | Admissions (n = 5064) | Deaths (n = 703) | CFR | |
|---|---|---|---|---|
| n (%)1 | n (%)1 | |||
| Gender | Male | 3388 (66.9%) | 446 (63.4%) | 13.2% |
| Female | 1673 (33.0%) | 256 (36.4%) | 15.3% | |
| Unstated | 3 (0.1%) | 1 (0.1%) | 33.3% | |
| Referral centre | Provincial hospital | 2871 (56.7%) | 612 (87.1%) | 21.3% |
| District hospital | 110 (2.2%) | 36 (5.1%) | 32.7% | |
| Self-referral | 1214 (24%) | 41 (5.8%) | 3.4% | |
| Other | 2 (0.03%) | 1 (0.1%) | 50% | |
| Unknown | 867 (17.1%) | 13 (1.8%) | 1.5% | |
| Mode of transport | Ambulance | 2529 (49.9%) | 622 (88.5%) | 24.6% |
| Car | 849 (16.8%) | 21 (3%) | 2.5% | |
| Motorbike | 1104 (21.8%) | 3 (0.4%) | 0.3% | |
| Unknown | 582 (11.5%) | 57 (8.1%) | 9.8% | |
| Median admission weight (IQR)2 | 2600g (1850-3200g) | 2100g (1470–2870)g | ||
| Admission weight | <1000g | 63 (1.2%) | 32 (4.6%) | 50.8% |
| 1000-1499g | 490 (9.7%) | 146 (20.8%) | 29.8% | |
| 1500-2499g | 1685 (33.3%) | 256 (36.4%) | 15.2% | |
| ≥2500g | 2721 (53.7%) | 267 (38%) | 9.8% | |
| Unknown | 105 (2.1%) | 2 (0.28%) | 1.9% | |
1.Unless stated otherwise
2.Median and interquartile range
For those neonates who died, the median survival time from admission was 5 days (IQR 1–14 days). Most deaths (81.7%) occurred within the first 28 days of life. Only 3% (n = 21) of all deaths in this facility occurred within the first 24 hours of life, while 45.2% of all deaths were late neonatal deaths (between 7 and 28 days). Over one-third (38%) of neonates who died had an admission weight of ≥2500g. Although there were fewer deaths in number, the CFRs were highest for neonates <1000g (33.7%).
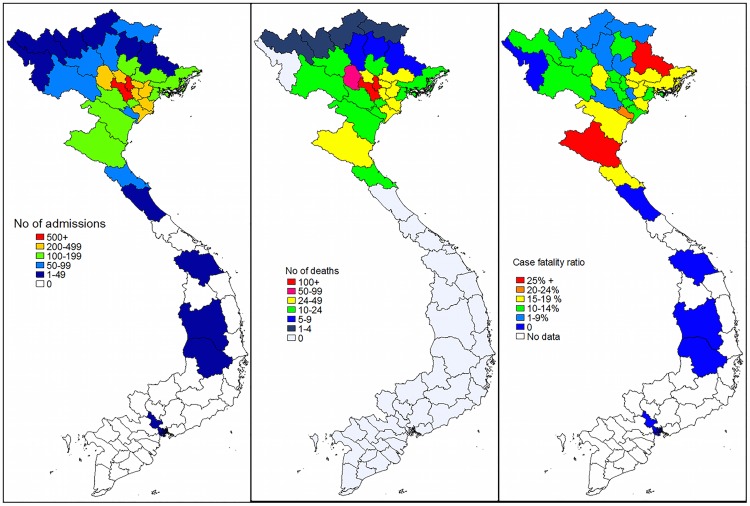
Most referrals came from Hanoi Province and its neighbouring provinces (Fig 1). Almost half of the self-referrals came from Hanoi Province (n = 548, 45%). There were few admissions and deaths from provinces that were more distant. However the CFRs were high from two distant provinces: Nghe An Province (CFR = 26.8%) and Lang Son Province (CFR = 25%).
Fig 1. The number of admissions (a), deaths (b), and case fatality ratio (c), to the Neonatal Department, National Hospital of Pediatrics, Hanoi, 1st July 2011 to 30th June 2012, by home province.
Cause-specific morbidity
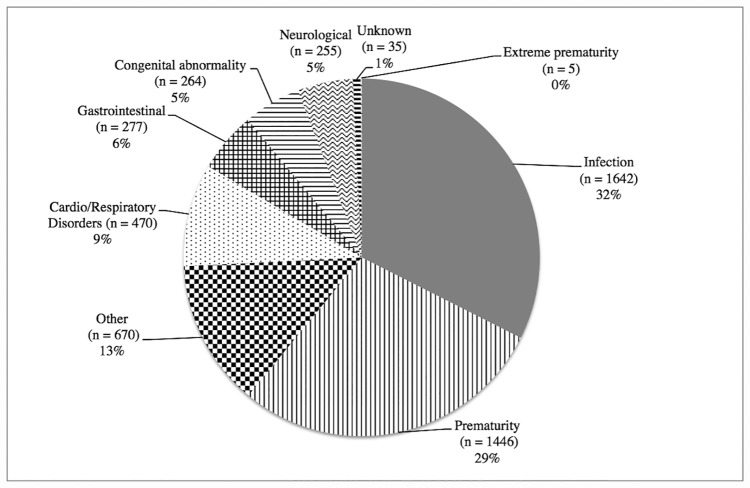
The two commonest discharge diagnoses were infection (32%) and prematurity (29%) (Fig 2). “Other causes” were the third commonest category (13%). The majority of these “other causes” had signs of jaundice (9% of all admissions) but no other diagnostic information was performed. Of all the cases with jaundice (n = 458), 12.9% had the diagnosis of kernicterus. Congenital abnormalities accounted for 5% of all admissions.
Fig 2. Discharge diagnoses1 of all admissions to the Neonatal Department, National Hospital of Pediatrics, Hanoi, 1st July 2011 to 30th June 2012 (n = 5064).
Cause-specific mortality
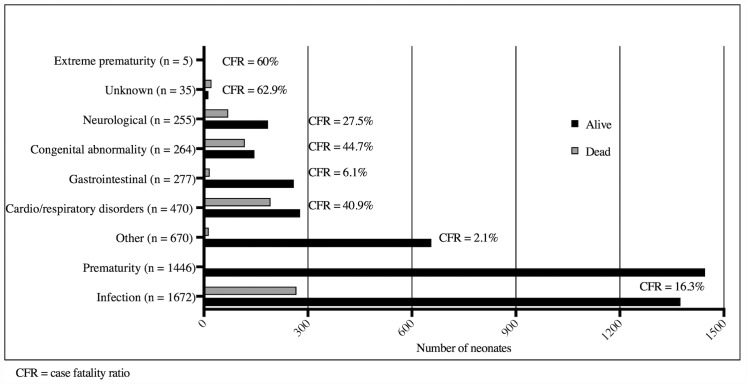
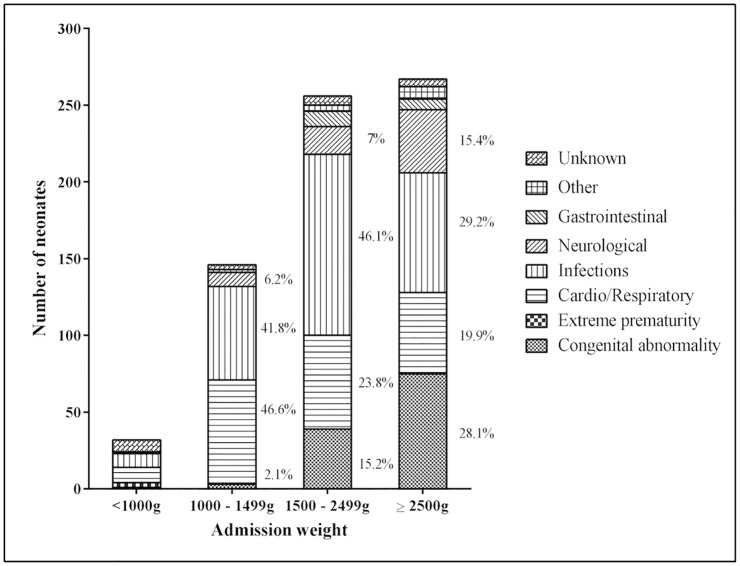
The commonest primary causes of death were infection (38%), cardio/respiratory disorders (27%), congenital abnormalities (17%) and neurological disorders (10%) (Fig 3). Excluding unknown causes of death and extreme prematurity (CFR 60%), congenital abnormalities had the highest CFR (44.7%), followed by cardio/respiratory disorders (40.9%). For neonates who died and had admission weights ≥ 1500g, the next most common causes of death after infection, were cardio/respiratory disorders and congenital abnormalities (Fig 4).
Fig 3. Discharge diagnoses and cause-specific case fatality ratios by PSANZ-NDC diagnostic category, Neonatal Department, National Hospital of Pediatrics, Hanoi, 1st July 2011 and 30th June 2012 (n = 5064).
Fig 4. Cause-specific mortality by admission weight, Neonatal Department, National Hospital of Pediatrics, Hanoi, between 1st July 2011 and 30th June 2012.
Infection was the commonest cause of death irrespective of admission weight (Figs 3 and 4), and had a CFR of 16.3% (Fig 3). Infections were a contributory factor for an additional 35 (5%) deaths. Of the 267 infections that were fatal, 21.7% were in neonates admitted within the first 24 hours of life and a further 36.3% were admitted between days 1–6 of life. Of the 302 fatal infections (both primary and contributory), a pathogen specific aetiology was identified for 122 (40.4%) infections. Klebsiella spp. was the commonest cause (n = 26, 21%), while fungal infections (including Candida spp) accounted for 10% (n = 12) of these infections.
Congenital infections were responsible for 16% of infections. Neonatal tetanus occurred in one fatal case. This ethnic minority infant was born at home, and the umbilical cord was cut with scissors. No further information regarding antenatal or postnatal care was recorded. Thirty-eight deaths were classified as congenital rubella syndrome, comprising 31% of the infections with a known aetiology.
Hyaline-Membrane Disease/Respiratory Distress Syndrome (HMD/RDS) caused 15.5% of all deaths. Almost half (49.9%) were in neonates admitted to the NHP within 24 hours of life. Over one quarter (28.4%) of neonates who died from HMD/RDS died within 24 hours of admission. S1 Fig shows 84.9% of deaths from HMD/RDS were in neonates with admission weights 1000-2400g. Pneumothoraces caused 7.5% of all deaths. Almost all of these neonates (96.2%) had been referred from provincial hospitals. One quarter of these neonates died within the first 24 hours of admission.
Cardiovascular abnormalities were the cause of 78% of congenital abnormality deaths, representing 13.1% of deaths. Hypoxic ischaemic encephalopathy (HIE) (n = 39) accounted for 6.4% of deaths, and intracranial haemorrhages (n = 23) accounted for 3.3% of deaths. Almost all (94.9%) deaths from HIE were in neonates with an admission weight ≥1500g and 23.1% died within 24 hours of admission.
Discussion
Neonates admitted to tertiary health facilities represent an important subgroup that have a high risk of mortality. We identified areas where attention could be focused to improve outcomes in the largest neonatal department in northern Vietnam. We found that infection and prematurity were the commonest reasons for admission. In contrast, a study from a tertiary referral hospital in Ho Chi Minh City, in southern Vietnam, found that prematurity, asphyxia, and congenital malformations were underrepresented in admissions, and found one quarter of the diagnoses did not require specialist care [19], which may indicate differences in referral patterns to NHP. The commonest causes of death in our study were infection, cardio/respiratory disorders, and congenital abnormalities, accounting for 82% of deaths. This is similar to the tertiary referral hospital for Southern Vietnam which showed major causes of death were congenital abnormalities, severe infection and prematurity, comprising 80% of all deaths [20].
The CFR for newborn care units in LMICs is highly variable [21–25] and may relate to socio-cultural or health system factors affecting timeliness of referral, disease burden, and quality of care provided.
As NHP is a tertiary referral hospital, very sick neonates are referred for specialised care, so it is unsurprising that we found a CFR of 13.9%. The difference with the tertiary referral centre in Southern Vietnam, where the CFR was 5%, demonstrates significant variation even within countries [20].
Our study has some important differences from population-based studies of neonatal mortality, consistent with this hospital’s role as a tertiary centre rather than a place of birth. For example, intra-partum related deaths represented a low percentage of deaths, given this aetiology has been identified as one of the commonest causes of neonatal death worldwide [1]. We also found very few deaths (3%) occurred in the first 24 hours of life at NHP. Both community data from Northern Vietnam which showed 58.6% of deaths occurred within the first 24 hours [15], and that global data suggest the risk of death is greatest on the first day of life, suggests that for northern Vietnam, the majority of these neonatal deaths occur outside the tertiary system [1]. While neonatal deaths due to infections and preterm complications have effective interventions for LMICs, solutions for intra-partum complications are more challenging and require strengthening of all levels of the health system [1, 26, 27].
As all admissions to NHP are born elsewhere, the decision to present to NHP for admission is influenced by many factors. However, one critical factor is the rapid identification and referral of complications in the first days after birth. The referral pattern in this study suggests that the sickest neonates are cared for initially at local provincial hospitals, which is consistent with the referral protocol of Vietnam. However, there were also many self-referrals (that is, by the family themselves) and these had a low CFR. Another study in Vietnam suggests that bypassing district hospitals for health care is common [28]. If many of the self-referrals presenting to NHP have minor conditions, they may be contributing to an unnecessary admission overload, especially if they can be cared for by a nearby hospital. The extremely high bed occupancy rate at NHP, exacerbated by insufficient human resources, may impact on the quality of care provided. A study in India found that admission overload had a negative impact on CFR [21]. Understanding referral pathways and admission criteria is vital to reduce patient overload at the tertiary level.
Our findings highlight the need to further understand the care provided at provincial hospitals and the adequacy of the referral system. We found few admissions and deaths from provinces that were more distant from NHP, and disparate CFRs by referral province. In addition, we found neonates presenting to NHP with the preventable and treatable condition of kernicterus. HMD/RDS was the second commonest cause of mortality. It is not known whether exogenous surfactant was administered prior to referral, or whether pre-delivery corticosteroids were administered. Both findings raise concerns regarding the adequacy of pre-referral treatment at district or provincial levels. Previous studies have shown that prevention and early management of prematurity (including HMD/RDS) at the site of birth is important to survival [29].
Several of our findings have potential implications for the quality of care at NHP. Our data suggest hospital acquired infections are common, given the organisms involved, and the timing of the onset of infection (data not shown). This is consistent with data from a central Vietnamese neonatal unit, which showed that 80% of infections were nosocomial [30]. To reduce hospital acquired infection rates, enhanced infection control practices are being implemented within NHP. In addition, these guidelines should be implemented in all hospitals. We found pneumothoraces to be relatively common. Further understanding on the timing of the event and the type of supplemental ventilation used is required to ascertain whether less invasive forms of ventilation may be warranted. This again highlights the need for understanding and improving the quality of care at referral hospitals.
In this study, 38% of deaths occurred in neonates with admission weight of ≥2500g. This is similar to other LMICs [23]. This pattern may be partially explained by a larger caseload of congenital abnormalities of normal birth weight being transferred to NHP, and selective referral practices for very low and extremely low birth weight neonates. We found there were few very low birth weight neonates referred, but those that were referred had a high CFR. Smaller, more premature neonates may not be referred due to their likely poor prognosis. Worldwide data consistently shows that the lower the birth weight, the higher the risk of a poor outcome [31, 32]. The introduction of basic standards of neonatal care in the highlands of Papua New Guinea reduced CFR in very low birth weight neonates by 56% [33].
In our study, 17% of deaths were due to congenital abnormalities and many of these were due to cardiac defects. This is consistent with NHP’s role as a tertiary referral centre in providing expert diagnostic and treatment facilities. A large rubella outbreak resulted in many cases of congenital rubella syndrome [34]. Rubella vaccination has recently been implemented in Vietnam and should, over time, reduce the burden of congenital rubella syndrome.
Although prematurity is not in itself a disease, it is a pathological state, and in this study we were unable to fully assess the role of prematurity to neonatal morbidity and mortality, despite prematurity being the commonest reason for admission. For future studies, it would be beneficial to provide an assessment of gestational age, although the additional workload needs to be considered.
There is increasing evidence in LMICs that auditing improves the quality of neonatal care. A systematic review of perinatal audits in LMICs demonstrated a 30% (95% CI, 21%-38%) reduction in perinatal deaths post audit introduction [35]. Our study demonstrates both the feasibility and the difficulties of implementing a mortality and morbidity database in a busy neonatal unit using existing clinical staff. In addition, the lack of testing facilities to diagnosis the common clinical sign of jaundice is a limitation. In this study we only recorded the primary cause of mortality but would recommend that secondary causes also be documented. Further training would also be required to avoid misclassification of some conditions and completeness of data collection. In this study we classified neonates with evidence of congenital rubella syndrome as “infection” as many did not have obvious abnormalities but had evidence of inflammation. This data could be further improved and more complete if collected by a trained audit committee, which should determine diagnostic classifications and also prioritize interventions [11].
Conclusions
We have provided a baseline assessment of the outcomes of neonates admitted to the largest tertiary referral hospital in northern Vietnam and have identified a number of areas for intervention so that further improvement in neonatal outcomes can be obtained. This study highlights the need for greater research into pre-referral care at first- and second-line facilities and for investigation of quality improvement activities such as audits to benefit neonatal care in all health facilities.
Supporting information
(TIF)
(XLSX)
Acknowledgments
We would like to thank the staff of the Neonatal Department, NHP, Hanoi. Fiona Russell held a National Health and Medical Research Council Early in Career Fellowship 2012–2015 (1035863).
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
Fiona Russell held a National Health and Medical Research Council Early in Career Fellowship 2012-2015 (1035863). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Lawn JE, Blencowe H, Oza S, You D, Lee AC, Waiswa P, et al. Every Newborn: progress, priorities, and potential beyond survival. Lancet. 2014;384(9938):189–205. Epub 19 May 2014. 10.1016/S0140-6736(14)60496-7 [DOI] [PubMed] [Google Scholar]
- 2.Liu L, Oza S, Hogan D, Perin J, Rudan I, Lawn JE, et al. Global, regional, and national causes of child mortality in 2000–13, with projections to inform post-2015 priorities: an updated systematic analysis. The Lancet. 2015;385(9966):430–40. [DOI] [PubMed] [Google Scholar]
- 3.Lawn JE, Kerber K, Enweronu-Laryea C, Cousens S. 3.6 million neonatal deaths—what is progressing and what is not? Seminars in Perinatology 2010;34(6):371–86. Epub 11 Sept 2010. 10.1053/j.semperi.2010.09.011 [DOI] [PubMed] [Google Scholar]
- 4.Kerber KJ, de Graft-Johnson JE, Bhutta ZA, Okong P, Starrs A, Lawn JE. Continuum of care for maternal, newborn, and child health: from slogan to service delivery. Lancet. 2007;370(9595):1358–69. 10.1016/S0140-6736(07)61578-5 [DOI] [PubMed] [Google Scholar]
- 5.Ganatra HA, Zaidi AK. Neonatal infections in the developing world. Seminars in Perinatology. 2010;34(6):416–25. 10.1053/j.semperi.2010.09.004 [DOI] [PubMed] [Google Scholar]
- 6.Darmstadt GL, Black RE, Santosham M. Research priorities and postpartum care strategies for the prevention and optimal management of neonatal infections in less developed countries. Pediatric Infectious Disease Journal. 2000;19(8):739–50. [DOI] [PubMed] [Google Scholar]
- 7.Darmstadt GL, Kinney MV, Chopra M, Cousens S, Kak L, Paul VK, et al. Who has been caring for the baby? Lancet. 2014;384(9938):174–88. Epub 19 May 2014. 10.1016/S0140-6736(14)60458-X [DOI] [PubMed] [Google Scholar]
- 8.Levels and trends in child mortality report 2015. United Nations Inter-Agency Group for Child Mortality Estimation, 2015.
- 9.Malqvist M, Eriksson L, Nguyen TN, Fagerland LI, Dinh PH, Wallin L, et al. Unreported births and deaths, a severe obstacle for improved neonatal survival in low-income countries; a population based study. BMC Int Health Hum Rights. 2008;8:4 Epub 1 April 2008. 10.1186/1472-698X-8-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The United Nations Children's Fund. At a glance: Viet Nam 2013 [cited 2016 September]. http://www.unicef.org/infobycountry/vietnam_statistics.html
- 11.Wallin L, Malqvist M, Nga NT, Eriksson L, Persson LA, Hoa DP, et al. Implementing knowledge into practice for improved neonatal survival; a cluster-randomised, community-based trial in Quang Ninh province, Vietnam. BMC Health Services Research. 2011;11:239 Epub 29 Sept 2011. 10.1186/1472-6963-11-239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Graner S, Klingberg-Allvin M, Phuc HD, Huong DL, Krantz G, Mogren I. Adverse perinatal and neonatal outcomes and their determinants in rural Vietnam 1999–2005. Paediatr Perinat Epidemiol. 2010;24(6):535–45. Epub 10 Jun 2010. 10.1111/j.1365-3016.2010.01135.x [DOI] [PubMed] [Google Scholar]
- 13.Almroth S, Arts M, Quang ND, Hoa PT, Williams C. Exclusive breastfeeding in Vietnam: an attainable goal. Acta Paediatrica. 2008;97(8):1066–9. Epub 17 May 2008. 10.1111/j.1651-2227.2008.00844.x [DOI] [PubMed] [Google Scholar]
- 14.Sutton J, He M, Despard C, Evans A. Barriers to breastfeeding in a Vietnamese community: a qualitative exploration. Can J Diet Pract Res. 2007;68(4):195–200. 10.3148/68.4.2007.195 [DOI] [PubMed] [Google Scholar]
- 15.Nga NT, Hoa DTP, Målqvist M, Persson L-Å, Ewald U. Causes of neonatal death: results from NeoKIP community-based trial in Quang Ninh province, Vietnam. Acta Paediatrica. 2012;101(4):368–73. 10.1111/j.1651-2227.2011.02513.x [DOI] [PubMed] [Google Scholar]
- 16.NHP. National Hospital of Pediatrics Hanoi [cited 2012 8 Aug]. http://www.nhp.org.vn/list.aspx?cat=001002
- 17.General Statistics Office of Viet Nam. Population and employment 2012 [cited 2014 September]. http://www.gso.gov.vn/default_en.aspx?tabid=467&idmid=3&ItemID=14459
- 18.PSANZ Clinical Practice Guidelines for Perinatal Mortality ACT2011 [cited 2012 Aug 8th]. http://www.psanz.com.au/special-interest/perinatal-mortality-group/psanzcpg
- 19.Kruse AY, Ho BT, Phuong CN, Stensballe LG, Greisen G, Pedersen FK. Prematurity, asphyxia and congenital malformations underrepresented among neonates in a tertiary pediatric hospital in Vietnam. BMC Pediatr [Internet]. 2012. 29 December 2013; 12(199). Available from: http://www.biomedcentral.com/1471-2431/12/199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kruse AY, Phuong CN, Ho BTT, Stensballe LG, Pedersen FK, Greisen G. Identification of important and potentially avoidable risk factors in a prospective audit study of neonatal deaths in a paediatric hospital in Vietnam. Acta Paediatrica. 2014;103(2):139–44. 10.1111/apa.12423 [DOI] [PubMed] [Google Scholar]
- 21.Neogi SB, Malhotra S, Zodpey S, Mohan P. Assessment of special care newborn units in India. J Health Popul Nutr [Internet]. 2011. October 2012 Source: NLM. PMC3225112]; 29(5):[500–9 pp.]. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3225112/pdf/jhpn0029-0500.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mukhtar-Yola M, Iliyasu Z. A review of neonatal morbidity and mortality in Aminu Kano Teaching Hospital, northern Nigeria. Tropical Doctor. 2007;37(3):130–2. Epub 25 Aug 2007. 10.1258/004947507781524683 [DOI] [PubMed] [Google Scholar]
- 23.Omoigberale A, Sadoh W, Nwaneri D. A 4 year review of neonatal outcome at the University of Benin Teaching Hospital, Benin City. Nigerian Journal of Clinical Practice [Internet]. 2010. September 2014; 13(3):[321–5 pp.]. Available from: http://www.njcponline.com/temp/NigerJClinPract133321-238018_063641.pdf. [PubMed] [Google Scholar]
- 24.Jimmy S, Kemiki AD, Vince JD. Neonatal outcome at Modilon Hospital, Madang: a 5-year review. P N G Med J. 2003;46(1–2):8–15. [PubMed] [Google Scholar]
- 25.Ahmed SH, Sarkis NN, Fikry SI. A study of neonatal morbidity and mortality at Damanhour Teaching Hospital Newborn Unit. J Egypt Public Health Assoc. 2004;79(5–6):399–414. [PubMed] [Google Scholar]
- 26.Bhutta ZA, Darmstadt GL, Hasan BS, Haws RA. Community-based interventions for improving perinatal and neonatal health outcomes in developing countries: a review of the evidence. Pediatrics. 2005;115(2 Suppl):519–617. 10.1542/peds.2004-1441 [DOI] [PubMed] [Google Scholar]
- 27.Bhutta ZA, Das JK, Bahl R, Lawn JE, Salam RA, Paul VK, et al. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? Lancet. 2014;384(9940):347–70. Epub 19 May 2014. 10.1016/S0140-6736(14)60792-3 [DOI] [PubMed] [Google Scholar]
- 28.Save the Children. A Situational Analysis of Newborn Health and Interventions in Vietnam: Towards the Development of a Newborn Health Action Plan 2006 [cited July 2013]. http://www.healthynewbornnetwork.org/sites/default/files/resources/Vietnam_English.pdf
- 29.March of Dimes, PMNCH, Save the Children, WHO. Born Too Soon: The Global Action Report on Preterm Birth. Geneva: World Health Organisation, 2012.
- 30.Tran H D H, Lee K, Dang N, Graham S M. A high burden of late-onset sepsis among newborns admitted to the largest neonatal unit in central Vietnam. Journal of Perinatology. 2015;35:846–51. Epub 9th July 2051. 10.1038/jp.2015.78 [DOI] [PubMed] [Google Scholar]
- 31.UNICEF/WHO. Low Birthweight Country, Regional and Global Estimates 2004 [18 April 2012]. http://www.unicef.org/publications/files/low_birthweight_from_EY.pdf
- 32.Mmbaga BT, Lie RT, Olomi R, Mahande MJ, Kvale G, Daltveit AK. Cause-specific neonatal mortality in a neonatal care unit in Northern Tanzania: a registry based cohort study. BMC Pediatr. 2012;12(1):116. Epub 9 Aug 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Duke T, Willie L, Mgone JM. The effect of introduction of minimal standards of neonatal care on in-hospital mortality. P N G Med J. 2000;43(1–2):127–36. [PubMed] [Google Scholar]
- 34.Toda K, Reef S, Tsuruoka M, Iijima M, Dang TH, Duong TH, et al. Congenital rubella syndrome (CRS) in Vietnam 2011-2012—CRS epidemic after rubella epidemic in 2010–2011. (1873–2518 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pattinson R, Kerber K, Waiswa P, Day LT, Mussell F, Asiruddin SK, et al. Perinatal mortality audit: counting, accountability, and overcoming challenges in scaling up in low- and middle-income countries. International Journal of Gynaecology & Obstetrics. 2009;107(Suppl 1):s113–22. Epub 11 July 2009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(TIF)
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.