Abstract
Pediatric medication nonadherence is a major problem in the United States health care system. Age of the child, lack of understanding about the disease or treatment, culture, socioeconomic status, family structure, schedule of medications, and taste can all contribute to this problem. Strategies that target interventions to the individual patient and family can be most effective. Pharmacists are at the forefront of patient care and can help children become more adherent to their medications through counseling and building a trusting relationship with the family. This article highlights some common problems to adherence and some solutions to increase adherence.
Keywords: adherence, compliance, counseling, patient education, pediatric medication adherence
Medication adherence is a multifaceted problem involving the patient, caregivers, and the entire interdisciplinary health care team, including pharmacists. Medication adherence can be defined as “the extent to which a person's behavior — taking medication, following a diet, and/or executing lifestyle changes, corresponds with agreed recommendations from a health care provider.”1 Former US Surgeon General Dr. C. Everett Koop once said, “Drugs don't work in patients who don't take them.”2 In other words, prescription medications can only be effective when they are taken correctly. To optimize patient outcomes and promote safe and effective therapy, health care providers should strive to improve adherence among all medication users.
The pediatric population accounts for approximately 25% of the United States population.3 Approximately 60% of pediatric patients filled a medication prescription within the last year, and half of the pediatric population suffers from a chronic medical condition requiring medications.4 A national survey found that young children aged 7 to 12 months are the highest medication consumers.5 The most common medications prescribed for these children include antibiotics, analgesics, and antipyretics to treat acute conditions such as infection.4 The data also reveal that children aged 12 to 17 years may use a significant number of medications, but most of these medications are to control chronic conditions.5
Medication adherence can be problematic for the pediatric population. Rates of medication adherence in this population are extremely variable; they range from 11% to 93%, with an estimated average of around 50%.6 Some chronic disease states such as juvenile rheumatoid arthritis, posttransplant therapy, cancer, and epilepsy have medication adherence rates that range between 50% and 60%.5 In patients with attention deficit–hyperactivity disorder (ADHD), it is estimated that most discontinue therapy after 4 months and approximately 20% stop after the first prescription.7 One particularly nonadherent group is adolescents 12 to 18 years old, with reported rates as low as 5% to 15%.8
Pediatric nonadherence may contribute to slower recovery times and increased costs to the family as well as the health care system.4 The National Council on Patient Information and Education (NCPIE) issued a statement in 1989 that pointed to the nonadherence to medications in pediatric patients of all ages, ethnicities, and socioeconomic status as a national problem that needed to be addressed.5,9 Unfortunately, this remains a problem for health professionals more than 25 years after the NCPIE statement.
Chronic illnesses typically require long-term treatment with medications as well as effective counseling to enhance self-care skills at home, such as monitoring blood glucose levels and ensuring proper use of asthma inhalers. Nonadherence in pediatric patients with chronic illnesses increases the number of emergency department visits and hospitalizations and is costly to the US health care system. Children who suffer from chronic conditions account for 16% of the youth of America, however, they were responsible for 53% of the hospital days.10 Seven studies showed that nonadherent asthmatic children and adolescents had increased emergency department visits.10 These data should foster further investigation into methods to improve adherence in children with asthma. This would reduce overall health care costs and possibly decrease morbidity and mortality resulting from nonadherence.10
The health care team including pharmacists should take an active approach to promote adherence through collaborative interventions. Medication adherence in the pediatric population, especially in those with chronic illnesses, is more complex than adherence in adults. There are multiple, unique reasons for nonadherence in pediatric patients that include parental and/or caregiver involvement, age of the child, cognitive factors, and social factors. This article aims to describe some of the barriers to pediatric medication adherence and explore possible solutions.
FACTORS AFFECTING PEDIATRIC ADHERENCE
Age
Age plays a significant role in pediatric nonadherence as a result of the cognitive and emotional development that occurs as the child grows. Younger children typically do not have the physical capacity or cognitive understanding to effectively administer their own medications. As a result, they are fully dependent on their caregivers to administer their medications. Factors that affect the caregivers' attitudes about medications, and that may affect adherence, will be discussed later. The influence of a caregiver on medication adherence may gradually decrease as the child ages and seeks greater autonomy and responsibility over his/her own therapy.
The correlation between adolescent age and its impact on medication adherence is largely undefined. A study of asthmatic patients aged 8 to 16 years found that age was associated with increased knowledge of the disease but not with improved adherence.11 The authors speculate that adolescents may be less able and/or motivated to manage their chronic illness despite their increased knowledge. One reason for this may be caregivers who continue to assume responsibility for the teenager's therapy, directly conflicting with the adolescent's desire to develop independence and competence and leading to nonadherence.11 Conversely, when adolescents are given full, noncompetitive control and responsibility over their lives, they may not be ready for this responsibility or they may not believe that they need the medication to control their illness, and this may also result in nonadherence. Often adolescents believe that they are invincible and that avoiding medication will not have consequences.
Peer pressure also plays an important role in the behavior of adolescents. Adolescents seek a sense of normalcy and a desire to fit in. To some, this means sacrificing proper medication usage or omitting doses completely in an effort to appear just like everyone else, leading to decreased medication adherence.12 For example, a 13-year-old patient with HIV may be noncompliant with his medicines when he sleeps over at friend's house, because of the stigma of taking medications or the embarrassment of admitting to his condition. Children with ADHD provide similar context regarding the stigma they feel with their condition and the impact on adherence.7 Adolescents may not fully understand their condition or even perceive ADHD as an illness, which may result in them not accepting treatment for their condition.
Another important barrier to medication adherence among adolescents involves adverse effects of these medicines, particularly cosmetic side effects. These effects cause an emotional toll and impact body self-image during transitional and developmental years. Adolescents undergo rapid and significant change during this period, and body image becomes extremely important.5 Side effects such as acne or weight gain can have a negative impact on the adolescents' body image and self-esteem, which affects their decision to start the prescribed treatment or to continue therapy.6
Culture
Various cultural factors play a role in adherence with pediatric therapies. Language barriers can create a lack of understanding about information provided by a health care professional. A survey of underserved Hispanic communities found a negative correlation between adherence rates and lack of explanation of medicine side effects due to language barriers.13 Non-English-speaking patients or family members cannot read the prescription label or leaflet and they cannot understand the counseling points unless they are translated to their language.
How families perceive their child's chronic disease also plays a role in adherence rates. One study showed a significant difference in asthma controller adherence among Latino children in various geographical locations as compared to non-Latino Caucasians. 14 Family structure and parental beliefs about medications were contributing predictors of nonadherence. 14 The health care team needs a wide range of cultural competency to efficiently and properly counsel and educate caregivers.
Socioeconomic Status
Socioeconomic status impacts medication adherence. Studies have found differences in rates of adherence in certain underserved populations.15 One study found higher adherence rates in clinics located in suburban areas compared to inner city clinics among adolescents who were taking oral contraceptives.15 This could be due to lack of transportation, access to pharmacies, or funds to purchase medications.
Family Structure
Family size, parental marital status, general stress, and stability may be contributing factors to pediatric adherence. In a large family, there are demands on resources that may affect the caregiver's ability to afford medications and monitor medication compliance. A study to examine the causes of nonadherence in pediatric and adolescent cancer patients found an inverse relationship between the number of siblings and adherence.16 Nonadherent patients had statistically significantly more siblings than adherent ones (p = .008).16
The marital status of the child's caregivers is a contributing factor to medication adherence. Multiple studies have shown that patients who live in a married household have higher levels of adherence than those who live in a single parent/caregiver household. Many of these studies involved adolescents dealing with chronic conditions such as diabetes, renal transplant, and asthma.17
There is also a correlation between the interpersonal relationships within the family and its ability to achieve effective medication adherence goals in pediatric patients. A study showed that family conflict was associated with poor adherence among asthmatic adolescents. 18 Family conflict can serve as a strong predictor of poor self-management in adolescents with conditions such as diabetes and juvenile rheumatoid arthritis.19
Additional factors affecting adherence relate to the understanding that the child and parent have about the child's condition and fears about medication safety or efficacy.20 This is especially true with chronic conditions; medications are used to control the disease but do not necessarily make the child feel better. If the child looks healthy, the caregiver may think that the child does not need to be on medication that is known to have many side effects unless the child's condition declines.
Schedule
Timing and duration of medication therapy also influences medication adherence. In a study of 75 mothers, only 7 were adherent with providing the child's antibiotics at the appropriate time and dosing frequency.21 Administration of doses during the middle of the day may cause difficulties for children who are in school, resulting in missed doses. Another pediatric study of oral penicillin for the treatment of streptococcal pharyngitis or otitis media found that on the first day of treatment adherence levels were fairly high at 81%, however adherence rates decreased to 56% by the 10th day of treatment.22 Adherence rates decrease as medication dose frequency increases. It is estimated that adherence rates are on average 70% for twice-daily dosing and 20% for 4-times-a-day dosing.23
Taste/Formulation
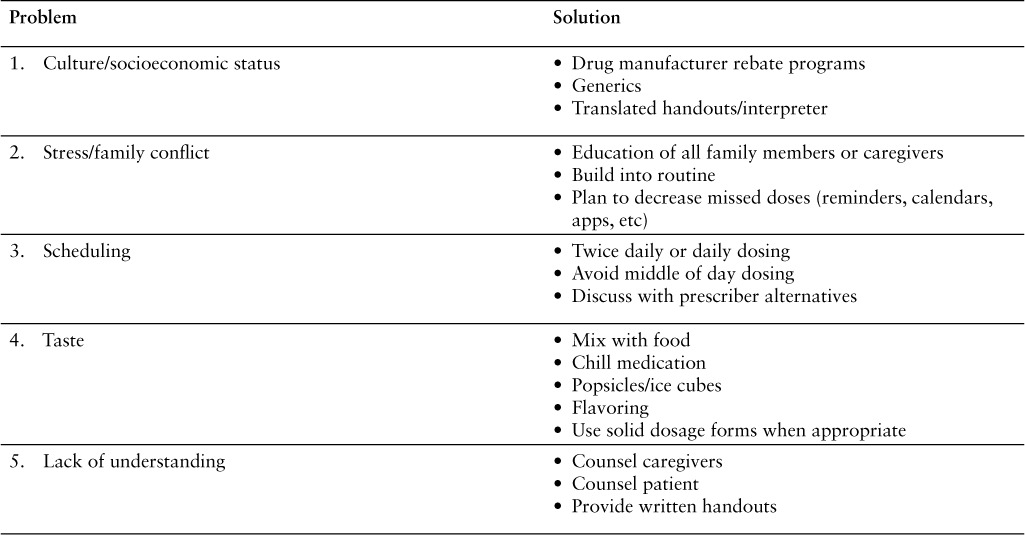
Medications administered to children come in a variety of different formulations, including solids, powders, suspensions, liquids, and topicals. These formulations have effects on adherence. Children can object to the taste, smell, aftertaste, or even texture of oral medications. In a preliminary survey conducted among 18 parents of HIV-positive children between 4 and 14.5 years of age receiving ART, adherence issues were assessed and specific features contributing to nonadherence were reported by the parents. More than 78% had difficulty with the treatment regimen, half of which was attributed to the taste of the medication. 24 Retrospective studies found that medications with negative palatability had a negative influence on adherence, whereas drugs with good palatability had a positive influence on adherence.8 Children may be reluctant to take bad-tasting medications, or they may spit or vomit out the preparation.6 This often results in improper use of the medicine, because the child is not taking the full amount required. This can lead to poor health outcomes. Additionally, formulations for pediatric patients are limited and may require special compounding. Table 1 lists problems and potential solutions.
Table 1.
Medication adherence barriers and solutions
SOLUTIONS
Education and Counseling
Education is essential for the child and the caregivers who are involved with the child. It is important for all family members to understand the basics of the child's disease state as well as the treatment plan in order to encourage adherence. If family members understand the disease state and have been educated on the negative consequences of the uncontrolled disease, they will feel increased responsibility for ensuring the child's adherence.5,8 Counseling should be nonthreatening, nonjudgmental, and individualized. Almost 60% of parents who were not counseled made errors in medicine administration compared to 25% who were counseled.5 Pharmacists should communicate with patients and caregivers, encouraging them to explain why and when specific doses are missed in order to work toward a solution.
Children also need active involvement with their therapy and to know more about their disease state and treatment.25 But in a survey of 341 pharmacists, it was found that almost three-quarters communicated with the children some of the time or rarely.26 Pharmacists should ask open-ended questions or closed-ended questions, depending on which may be more helpful; sometimes asking close-ended questions is best with younger children because it helps them understand what information is needed. Questions should be tailored toward their life, schedule, and how many caregivers will be involved in their therapy. It also should be determined whether the child has any environmental constraints that will serve as barriers to adherence.
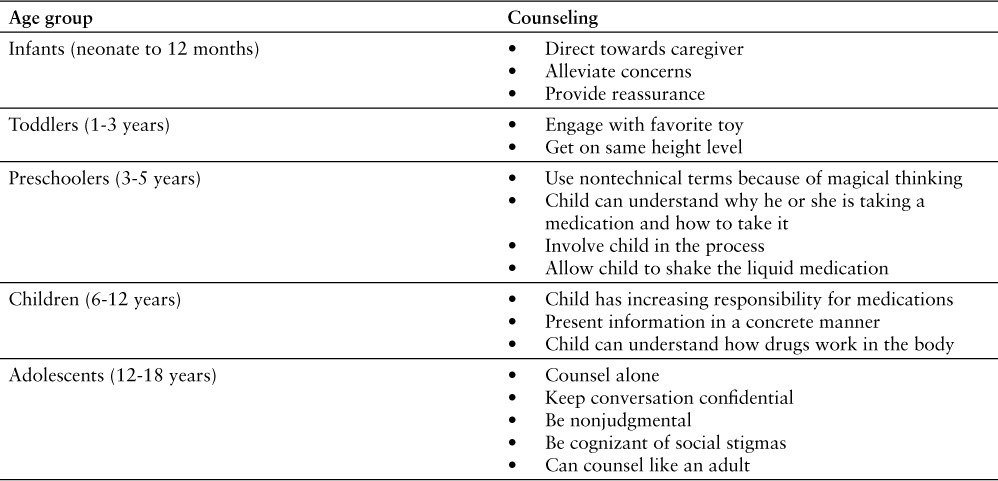
As a child grows older and develops cognitively, the medication counseling should be tailored to match each developmental stage. Counseling for infant patients (neonate to 12 months) is exclusively directed toward the caregivers of the child. The pharmacists' main role is to help the caregiver navigate through the child's medication uses, proper dosing, and technique. Pharmacists should be reassuring and alleviate fears or concerns that caregivers might have in regard to the child's illness.
The next major stage of cognition is in toddlers, aged 1 to 3 years old. Counseling is focused toward the caregiver. Children at this stage of development are not prepared to receive complex information about their illness or medication, but they can understand simple explanations about what is going on. For example, a pharmacist could say, “Your mommy and I know you don't feel good. Taking this medicine will make you feel much better.”9 Pharmacists can engage children in a playful and energetic manner, if they are open and feel comfortable. Pharmacists can crouch down on the child's level, use a stuffed animal, and speak in basic nonmedical terms. However not every toddler will be receptive. The child's social behavior and comfort level among strangers should be assessed before initiating any interactions. Exhibiting a nonintimidating, nonthreatening, reassuring demeanor toward toddlers and caregivers is the best approach to allow them to feel more relaxed and open to counseling advice.
The next age group of children is preschoolers (3–5 years old). This is a very dynamic age category; at this stage, children tend to engage in “magical thinking.” Perception of reality and make believe overlap.9 Pharmacists should be very careful in their word selection when speaking to this age group. For example, telling a child with an ear infection that he or she has a “bug” in the ear might be frightening and potentially result in detrimental effects. A better approach could be to show the child a diagram of an animated ear that has a red dot on it, point to that location, and explain that the red spot is why their ear hurts and the medicine will make the red dot go away.9 Pharmacists should refrain from using too many technical medical terms in their explanations. Other ways to involve the child is allow them to shake up an antibiotic solution or place a sticker on a prescription bottle. This may help the child become a part of the process helping to “make the prescription.” Education, however, should still be primarily directed to the caregivers.
In early school age (6 to 12 years old), children's cognitive and logical skills expand and their thinking becomes more concrete, critical, and advanced. Their interpretation of reality mirrors reality itself.8 They understand concepts such as germs, their ability to cause disease, and the importance of hygiene. Although caregivers still have the responsibility for medication administration, pharmacists can direct counseling to both children and caregivers. Pharmacists can help shift control of medication adherence toward the children by encouraging them to remind caregivers when their next dose is due.9 By this age, children should be able to use the correct names of their medications, instead of describing them as the blue tablet or white inhaler.
There is no definitive age at which children should assume greater or full responsibility for taking their own medications in the literature; however there are a few published articles that present data to help identify an approximate age. In a cohort study of children and adolescents who received liver transplants, the age range in which half the responders and half the caregivers said the children should assume responsibility was 11 to 12 years.27 Further assessment validated that age category; it was found that early adolescence (9–16 years; average age, 12) is the typical age at which children assume responsibility for the management of their therapy regimen.27 Caregiver oversight however is essential to avoid incorrect medication use and potential overdose situations.
Patient education and reinforcement is essential to ensuring safe and effective care in the pediatric population. Studies show that only 50% of the instructions provided during a pediatric clinic visit are recalled immediately following the visit.23 This can be improved through both oral and written counseling methods to reinforce information. Patient education materials and counseling sheets that are simplified should be given to children and parents. Table 2 lists abbreviated counseling techniques.
Table 2.
Counseling tips for age groups
Adherence Tools
Some of the ways pharmacists can promote medication adherence include offering adherence tools to the caregivers. Technology to promote adherence, such as smart phone apps and calendars, can be convenient reminders of the medication schedule. Community pharmacies can provide GlowCaps for medicine bottles. These caps light up during a designated time to remind the caregiver to administer the medication. Connecting medication administration times with activities of daily living, such as getting up in the morning or brushing teeth, will likely serve as a helpful tactic for both the caregiver and children who are participating in their own therapy.
Family Factors
Socioeconomic status, cultural differences, and family struggle are some factors that pharmacists can help to alleviate. If a patient's insurance will not cover a medication, a copay is too high, or a patient does not have insurance, the pharmacist can research manufacturer assistance programs, refer the patient to various insurance programs, or contact the prescriber to discuss alternatives. If language barriers exist that affect communication with the family or patient, interpreters and translated patient information handouts should be used. Because there will likely be multiple caregivers involved in the child's care, education of as many family members as possible is optimal.
Simplification of Regimens
The relationship between dosing schedules and adherence rates has been examined in an array of studies. The simpler the dosing schedule, in terms of frequency and duration, the greater likelihood of adherence.23 To promote adherence in children, pharmacists should work collaboratively with prescribers to identify simpler medication regimens with an easier administration schedule. For example, various studies show that once-daily budesonide is as effective as twice (or more) daily dosing regimens of inhaled corticosteroids for asthmatic children.28 Simplified regimens can decrease the dosing burden placed on caregivers and can possibly alleviate scheduling conflicts. For school aged or adolescent children, less frequent dosing may help reduce the stigma associated with taking medications at school. If multiple dosing is required, alternative schedules can be implemented in some cases. Children may take their medication first thing in the morning, after school, and at bedtime as long as this approach works best for the child's condition and their caregiver.
Taste
Patients, especially younger children, may refuse to take medications due to poor palatability. Improving or masking the taste of medications can have a positive effect on adherence. Giving ice cubes or popsicles to children before the medicine will numb their taste buds and hide the unpleasant taste. Graham crackers or acidic juices such as orange juice may be used to dissipate the taste of medications with a bad aftertaste. Salty tasting medications, such as potassium chloride, can be hidden by butterscotch, cinnamon, or peanut butter. Caregivers may use chocolate, coffee flavoring, or licorice to conceal the bitterness of some medications. FlavoRx is one company that offers custom flavorings for liquid medications, which may improve palatability in children.29 Pharmacists should counsel caregivers about which medications are not to be taken with food. Also, mixing the medication with food or juice can help mask the taste but this should be done with some caution for fear of food aversion. Pharmacists should be aware of medication stability issues. If a medication is stable at refrigerated temperatures, the chilled medication may be more easily tolerated. The use of oral syringes may improve compliance by making it easier for caregivers to measure and administer medications as well as minimizing exposure to an unpleasant smell.
Studies have evaluated the dosage forms of medication preference and their subsequent outcomes on adherence rates. Larger volumes of medication may serve as a contributing factor to a child's unwillingness to take their medicine. One suggestion would be to use a solid dosage form if possible. Most children around the age of 8 years old are able to swallow solid dosage forms. In a randomized, crossover clinical trial of children aged 10 to 18 years with familial hypercholesterolemia, the acceptability and adherence of 2 different dosage forms of cholestyramine were assessed and analyzed. After the 16-week study was completed, it was found that 82% of children preferred the tablet form, 16% the powder form, and 2% preferred neither. The form of cholestyramine increased adherence by at least 25% for 42% of the patients.30 In a randomized trial in Africa of 30 infants and children aged 0 to 5 years, the authors found 42% compliance with liquid formulations and 91% with the prepacked tablet formulation for antimalarial medications over a 6-week period.31 Caregivers preferred the tablet formulation and reported a greater ease of administration because the liquid formulation had to be measured (prior to administration).
CONCLUSIONS
Pediatric medication adherence is a major issue for the health care system in regard to outcomes and cost. There are many solutions to enhance medication adherence in pediatric patients, including individualized counseling, simplified regimens, use of technology, and strategies to improve taste. As medication experts, pharmacists should be involved in educating children and families about medications to reduce this nationwide problem. By creating a collaborative partnership with the family members and understanding their particular needs, pharmacists can help to address barriers to adherence and suggest ways to resolve them.
REFERENCES
- 1. Sabate E. Adherence to long-term therapies: Evidence for action. World Health Organization. 2003. http://www.who.int/chp/knowledge/publications/adherence_full_report.pdf?ua=1. Accessed September 28, 2016.
- 2. Osterberg L, Blaschke T.. Adherence to medication. N Engl J Med. 2005; 353: 487– 497. [DOI] [PubMed] [Google Scholar]
- 3. United States Census Bureau. . Annual estimates of the population by sex and selected age groups for the United States: April 1, 2012 to July 1, 2013. https://factfinder.census.gov/faces/nav/jsf/pages/index.xhtml. Accessed September 28, 2016.
- 4. 2009/2010 National Survey of Children with Special Health Care Needs. . Child and Adolescent Health Measurement Initiative. http://www.childhealthdata.org. Accessed September 28, 2016.
- 5. National Council on Patient Information and Education. . Children and America's other drug problem: Guidelines for improving prescription medicine use among children and teenagers. 1989. http://www.talkaboutrx.org/assocdocs/TASK/376/ChildAmericaOtherDrugProblem.pdf. Accessed September 28, 2016.
- 6. Matsui DM. Current issues in pediatric medication adherence. Pediatr Drugs. 2007; 9( 5): 283– 288. [DOI] [PubMed] [Google Scholar]
- 7. Chacko A, Newcorn JH, Fiersen N, Uderman JZ.. Improving medication adherence in chronic pediatric health conditions: A focus on ADHD in youth. Curr Pharm Des. 2010; 16( 22): 2416– 2423. [DOI] [PubMed] [Google Scholar]
- 8. Winnick S, Lucas DO, Hartman AL, Toll D.. How do you improve compliance? Pediatrics. 2005; 115( 6): 718– 724. [DOI] [PubMed] [Google Scholar]
- 9. Dundee FD, Dundee DM, Noday DM.. Pediatric counseling and medication management services: Opportunities for community pharmacists. J Amer Pharm Assoc. 2002; 42( 2): 556– 567. [DOI] [PubMed] [Google Scholar]
- 10. McGrady ME, Hommel KA.. Medication adherence and health care utilization in pediatric chronic illness: A systematic review. Pediatrics. 2013; 132( 4): 730– 740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. McQuaid EL, Kopel SJ, Klein RB, Fritz GK.. Medication adherence in pediatric asthma: Reasoning, responsibility, and behavior. J Ped Psychol 2003; 28: 323– 333. [DOI] [PubMed] [Google Scholar]
- 12. Taddeo D, Egedy M, Frappier JY.. Adherence to treatment in adolescents. Paediatr Child Health. 2008; 13( 1): 19– 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. David RA, Rhee M.. The impact of language as a barrier to effective health care in an underserved urban Hispanic Community. Mt Sinai J Med. 1998; 65( 5–6): 393– 397. [PubMed] [Google Scholar]
- 14. McQuaid EL, Everhart RS, Seifer R, . et al. Medication adherence among Latino and Non-Latino white children with asthma. Pediatrics. 2012; 129: 1404– 1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Emans SJ, Grace W, Woods ER, . et al. Adolescents' compliance with the use of oral contraceptives. JAMA. 1987; 257( 24): 3377– 3381. [PubMed] [Google Scholar]
- 16. Tebbi CK, Cummings KM, Zevon MA, . et al. Compliance of pediatric and adolescent cancer patients. Cancer 1986; 58: 1179– 1184. [DOI] [PubMed] [Google Scholar]
- 17. Staples B, Bravender T.. Drug compliance in adolescents: Assessing and managing modifiable risk factors. Pediatr Drugs 2002; 4( 8): 503– 513. [DOI] [PubMed] [Google Scholar]
- 18. Bender B, Wamboldt FS, O'Connor SL, . et al. Measurement of children's asthma medication adherence by self report, mother report, canister weight, and Doser CT. Ann Allergy Asthma Immunol. 2000; 85( 5): 416– 421. [DOI] [PubMed] [Google Scholar]
- 19. Chaney J, Peterson L.. Family variables and disease management in juvenile rheumatoid arthritis. J Pediatr Psychol. 1989; 14: 389– 403. [DOI] [PubMed] [Google Scholar]
- 20. Gardiner P, Dvorkin L.. Promoting medication adherence in children. Am Fam Physician. 2006; 74: 793– 798. [PubMed] [Google Scholar]
- 21. Dawson A, Newell R.. The extent of parental compliance with timing of administration of their children's antibiotics. J Adv Nurs. 1994; 20: 383– 390. [DOI] [PubMed] [Google Scholar]
- 22. Charney E, Bynum R, Eldredge D, . et al. How well to patients take oral penicillin? A collaborative study in private practice. Pediatrics 1967; 40: 188– 195. [PubMed] [Google Scholar]
- 23. Butz A. Evidence-based practice: What is the evidence for medication adherence in children. J Pediatr Health Care. 2006; 20: 338– 341. [DOI] [PubMed] [Google Scholar]
- 24. Goode M, McMaugh A, Crisp J, . et al. Adherence issues in children and adolescents receiving highly active antiretroviral therapy. AIDS Care. 2003; 15: 403– 408. [DOI] [PubMed] [Google Scholar]
- 25. Sleath B, Bush PJ, Pradel FG.. Communicating with children about medicines: A pharmacists' perspective. Am J Health Syst Pharm. 2003; 60: 604– 607. [DOI] [PubMed] [Google Scholar]
- 26. Ranelli P. Bartsch K, London K.. Pharmacists' perceptions of children and families as medicine consumers. Psychol Health. 2000; 15: 829– 840. [Google Scholar]
- 27. Shemesh E, Shneider BL, Savitzky JK, . et al. Medication adherence in pediatric and adolescent liver transplant recipients. Pediatrics 2004; 113( 4): 825– 832. [DOI] [PubMed] [Google Scholar]
- 28. Boulet LP. Once-daily inhaled corticosteroids for the treatment of asthma. Curr Opin Pulm Med. 2004; 10: 15– 21. [DOI] [PubMed] [Google Scholar]
- 29. Bunupuradah T, Wannachai S, Chuamchaitrakool A, . et al. Use of taste-masking product, FlavoRx, to assist Thai children to ingest generic antiretrovirals. AIDS Res Ther. 2006; 3( 30). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. McCrindle BW, O'Neill MB, Cullen-Dean G, . et al. Acceptability and compliance with two forms of cholestyramine in the treatment of hypercholesterolemia in children: A randomized, crossover trial. J Pediatr. 1997; 130: 266– 273. [DOI] [PubMed] [Google Scholar]
- 31. Ansah EK, Gyapong JO, Agyepong IA, Evans DB.. Improving adherence to malaria treatment for children: The use of prepacked chloroquine tablets vs. chloroquine syrup. Trop Med Int Health. 2001; 6: 496– 504. [DOI] [PubMed] [Google Scholar]


