Abstract
Objective
Individuals with anorexia nervosa (AN) and body dysmorphic disorder (BDD) exhibit distorted perception and negative evaluations of their own appearance; however, little is known about how they perceive others’ appearance, and whether or not the conditions share perceptual distortions.
Method
Thirty participants with BDD, 22 with AN, now weight-restored, and 39 healthy controls (HC) rated photographs of others’ faces and bodies on attractiveness, how overweight or underweight they were, and how much photographs triggered thoughts of their own appearance. We compared responses among groups by stimulus type and by level-of-detail (spatial frequency).
Results
Compared to HCs, AN and BDD had lower attractiveness ratings for others’ bodies and faces for high-detail and low-detail images, rated bodies as more overweight, and were more triggered to think of their own appearance for faces and bodies. In AN, symptom severity was associated with greater triggering of thoughts of own appearance and higher endorsement of overweight ratings for bodies. In BDD, symptom severity was associated with greater triggering of thoughts of own appearance for bodies and higher overweight ratings for low-detail images. BDD was more triggered to think of own facial appearance than AN.
Discussion
AN and BDD show similar behavioral phenotypes of negative appearance evaluations for others’ faces and bodies, and have thoughts of their own appearance triggered even for images outside of their primary appearance concerns, suggesting a more complex cross-disorder body-image phenotype than previously assumed. Future treatment strategies may benefit from addressing how these individuals evaluate others in addition to themselves.
INTRODUCTION
Anorexia nervosa (AN) and body dysmorphic disorder (BDD) each express anomalous concerns with appearance, yet they are separately classified in DSM-5: AN under the heading Feeding and Eating Disorder, BDD under Obsessive-Compulsive and Related Disorders1. It remains uncertain if the nosological separation is justified, as both AN and BDD have been shown to co-occur, they have a similar mean age of onset, each is highly co-morbid with anxiety and obsessive-compulsive disorders—anxiety disorders are familially transmitted in AN2 –and each is typically characterized by impaired insight3, 4. At the level of symptom phenomenology, individuals with AN are preoccupied mainly with weight and shape, whereas the most common appearance concern in BDD involves the face or head (typically skin, nose, and hair5, less commonly abdomen, hips, and thighs6); yet approximately 30% of individuals with BDD also report significant concerns with weight7. AN differs from BDD in its greater prevalence in females and a generally less robust acute response to conventionally available treatments 1.
Recently, we showed that there are common and unique abnormalities in visual information processing of emotionally-neutral faces stimuli for AN and BDD8–10 and that there are irregularities in white matter microstructure in BDD involving visual systems11, 12. Research in this aspect of perceptual distortion, as well as self-referential thought, is limited. In one study, when examining photographs of others’ bodies, participants with AN rated underweight bodies to be more attractive and of more normal weight than did healthy controls (HCs)13. In another, participants with AN and HCs demonstrated a negative correlation between own body mass index (BMI) and over-estimation of another’s BMI, and lower BMIs were associated with optimal attractiveness14, suggesting a dimensional association between visual perception/evaluation and one’s own weight. Similarly, individuals with BDD have been shown to scrutinize details of others’ appearance in addition to their own5, and an eye-tracking study showed that participants with BDD had more fixations and longer dwell time on the least attractive areas of others’ faces, particularly areas corresponding to areas of primary concern on their own face15. To what extent these patterns translate to negative evaluations of others’ appearance, and/or if gaze behaviors trigger thoughts about own appearance remains unknown5.
Here, we present the results of what, to our knowledge, is the first study to directly compare appearance evaluations of others’ faces (and bodies) in AN and of bodies (and faces) in BDD; that is, determining if body-image phenomenology characteristic of one disorder is also manifest in the other. While body parts - other than the face - are often of concern in BDD6, 7, face appearance evaluations have rarely been documented in AN16. An additional aim was to determine how different spatial frequencies of images affect judgments of appearance in these groups. Visual perception (in addition to attentional biases and cognitive and emotional factors) is an important contributor to appearance judgments. Early in the brain’s visual processing stream, images are filtered at multiple spatial scales that are tuned to different bandwidths of spatial frequencies, effectively decomposing the patterns with spatial frequency filters17. High-pass filtered, or “high spatial frequency” images convey information about contours, edges, and texture, and thus represent fine-grained details whereas low spatial frequency images convey low-grained, configural, and holistic elements 18–20. In a previous fMRI study, we found that brain activation for high spatial frequency images was inversely associated with how attractive individuals with BDD rated others’ faces21, perhaps suggesting a neural process that links greater detail extraction by the visual system to reduced perceived attractiveness of facial characteristics. This proposal is corroborated by previous studies by other investigators that have found lower visual preference for high or low spatial frequencies22–24.
This component of the current study represents a behavioral extension of our previous work; by presenting participants with high spatial frequency and low spatial frequency photos of faces and bodies (in addition to unaltered, normal spatial frequency photos) we were able to probe different specialized visual processing systems to determine how they contribute to appearance judgments. Moreover, we extended this to testing whether differences in spatial frequency affect overweight/underweight ratings and triggering of thoughts of own appearance (for example, instantiating self-referential thoughts).
The purpose of this study was to understand similarities and dissimilarities in behavioral phenotypes in AN and BDD in regards to appearance judgments of others. This has proximal clinical implications for nosology; it can provide a better understanding of overlapping and distinct clinical features that may account for the high shared comorbidity, which can assist in refining categorical or dimensional conceptualizations of these disorders. It also has potential relevance for treatment, as appearance evaluations of others can significantly impact interpersonal interactions and relationships. A further, more exploratory goal of the study was to contribute to understanding neural mechanisms related to visual processing that may underlie symptom phenomenology. We compared how individuals with AN and BDD subjectively experience photos of others’ bodies and faces on measures of attractiveness and overweight/underweight appearance (for body photos), and to what degree the photos triggered thoughts about their own appearance.
First, we predicted that participants with AN, in accord with their disorder-unique body image concern, would rate others’ bodies as less attractive, as more overweight, and would trigger thoughts about their own body compared to BDD and HC; second, that participants with BDD would rate others’ faces as less attractive and as triggering thoughts of their own appearance more than would AN or HC, due to the fact that they typically have face concerns; third, that participants with BDD would rate bodies as less attractive, more overweight, and trigger thoughts about their own appearance more than HC due to the fact that those with BDD often also have body concerns; fourth, in AN we predicted that disorder severity would be associated with lower attractiveness ratings for bodies but not faces, higher overweight ratings, and greater thoughts triggered of own appearance for bodies, and in BDD symptom severity would be associated with lower attractiveness ratings for faces and bodies, higher overweight ratings, and greater thoughts triggered of own appearance for faces and bodies. Finally, we hypothesized that groups would differ in their appearance ratings depending on the level of detail (normal, high, or low spatial frequency) in the image, with BDD and AN groups finding detailed (HSF) images to be less attractive than would HCs. This is based on the model of heightened detail relative to global processing in AN and BDD, in combination with findings in the aforementioned study of lower attractiveness ratings in BDD associated with greater brain activity for HSF images21, and previous studies from other groups that have found lower visual preference for high spatial frequency images22–24.
METHODS
Participants
We recruited BDD and AN participants and HC from UCLA and local outpatient treatment centers, as well as from the community through print and online advertisements. We recruited individuals between the ages of 13 and 40. Of the 33 potential AN participants recruited, 9 were excluded due to having BMI < 18.5, and 2 were excluded for being on medications. Of the 33 potential BDD participants recruited, 3 were excluded for being on medications. Ninety-one eligible participants enrolled: 30 with BDD (24F/6M), 22 with AN (20F/2M), and 39 HCs (33F/6M). The UCLA Institutional Review Board approved the study and all participants gave written informed consent.
JDF and MS performed clinical evaluations. All participants were administered the Mini International Neuropsychiatric Interview (MINI)25 and the BDD Diagnostic Module26 modeled after the DSM-IV. Severity of psychiatric symptoms was quantified using the Hamilton Anxiety Rating Scale (HAMA)27, the Brown Assessment of Beliefs Scale (BABS)28, 29, and the Montgomery-Åsberg Depression Rating Scale (MADRS)29, all clinician-rated scales. Participants with BDD were administered the BDD version of the Yale-Brown Obsessive Compulsive Scale (BDD-YBOCS)30 and participants with AN were administered a version (excluding bulimia questions) of the Eating Disorder Evaluation (EDE) Edition 16.0D31 , and the Yale-Brown-Cornell (YBC) eating disorder scale32.
Inclusion criteria
All participants were right-handed and had normal or corrected visual acuity as verified by Snellen eye chart. For BDD, participants fulfilled criteria for BDD as determined by the BDD Diagnostic Module26, and scored ≥20 on the BDD-YBOCS. In AN, all participants must have previously met all DSM-IV criteria for AN, currently met criteria for AN except for the amenorrhea and weight criteria, and at the time of recruitment study had a minimum BMI of 18.5, to minimize confounding by starvation as all participants were also being enrolled in concurrent fMRI and EEG studies21, 33.
Exclusion criteria
Participants with AN and BDD were required to be free from psychoactive medications for the preceding 8 weeks. Given the common occurrence of other psychiatric disorders in these conditions, the presence of major depression, dysthymia, panic disorder, social phobia, and generalized anxiety disorder were allowed to assure our samples were representative of the general clinical population34–43. Persons with AN who also had a current or prior lifetime history of BDD were excluded, as were persons with BDD with current or lifetime AN (determined by the clinician administering the MINI). Also exclusionary was suicidal ideation, neurological disorders, pregnancy, conditions that affected cerebral metabolism, and current treatment with cognitive-behavioral therapy.
HC participants were unmedicated and without any current Axis I disorder or history of lifetime BDD, AN, bipolar disorder, or psychotic disorders, as determined by the BDD Module and the MINI.
Procedure
Face and body rating task
All participants viewed digitized grey-scale frontal-view photographs of emotionally-neutral male and female faces (50% of each) of varying ages, and male and female bodies (50% of each) with heads cropped and in bathing suits or underwear, selected from various websites; the bodies ranged from normal weight to overweight13, to provide a representation of average body types. The equal sex ratio of face and body stimuli was also to approximate the proportion of males and females in our society. The mean attractiveness rating for the unaltered images across groups was 4.2±2.5 (0 to 10); thus images were mostly in a medium range of attractiveness. The figures were taken from the Macbrain database, the UPenn Facial Emotional Stimuli, and the Psychological Image Collection at Stirling (http://pics.psych.stir.ac.uk/; see Figure 1).
Figure 1.
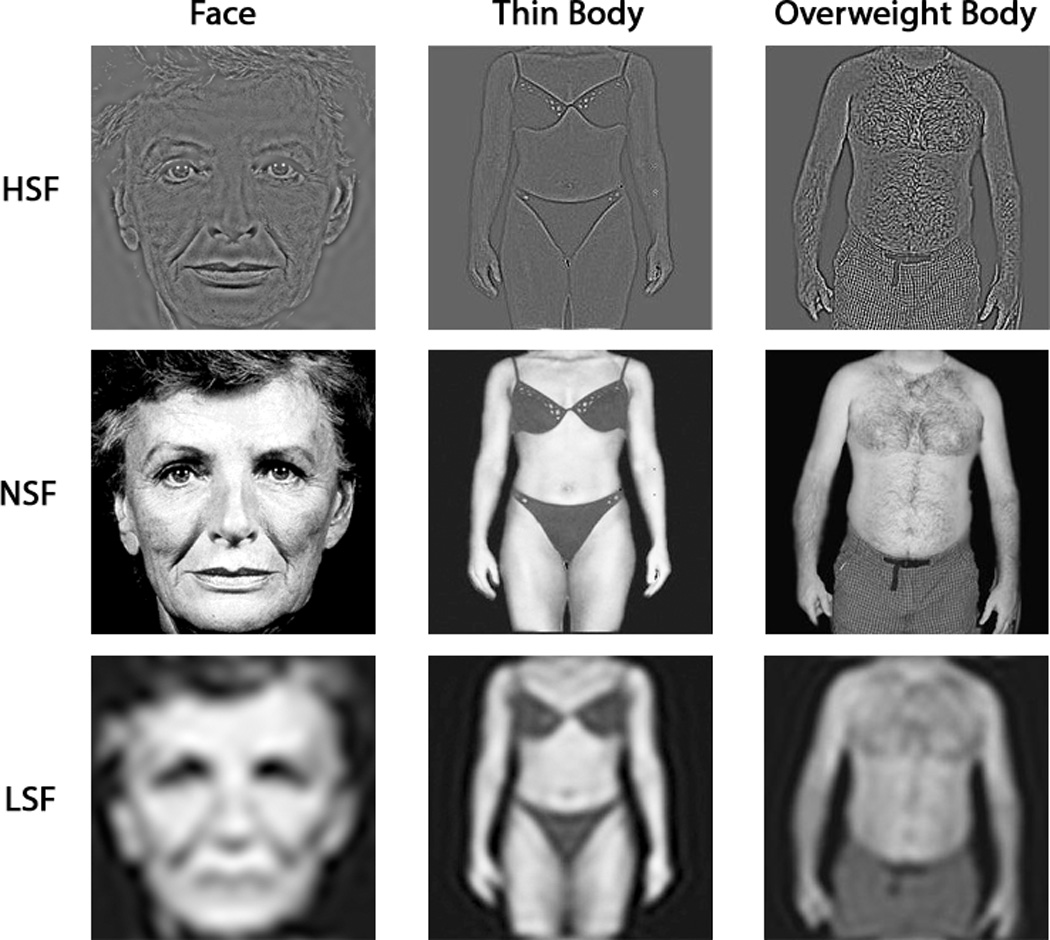
In addition to presenting the photos at normal spatial frequency (NSF) we also presented altered photos that were Fourier-transformed to filter out all but high spatial frequency (HSF), or all but low spatial frequency (LSF) components (using high-pass or low-pass filtering, respectively); the methods are described elsewhere44. Participants rated 16 faces each of NSF, LSF, and HSF photographs, and 16 bodies each of NSF, LSF, and HSF photographs, for a total of 48 faces and 48 bodies. There were two orders of randomly sorted faces/bodies that were counterbalanced across participants. (One order contained 15 rather than 16 bodies, due to experimental error.) Participants rated the face set then the body set. During image presentation, participants were asked to score faces and bodies on measures of attractiveness (“How attractive is this [face/body]?”), and how much they were triggered to think about their own appearance (“To what degree does the [face/body] trigger thoughts about your own appearance?”), all on a scale of 0 to 10. Additionally, the degree to which the body was perceived to be overweight or underweight was rated on a scale of −10 to 10, with −10 being extremely underweight, 0 being normal weight, and 10 being extremely overweight. Participants were seated in front of a computer to view the images on the screen. The investigator recorded their responses. There was no time limit on viewing and providing ratings of the images.
Analyses
We used linear mixed models implemented in SPSS to analyze ratings of faces and bodies at different spatial frequencies. We examined effects of group (AN, BDD, HC), stimuli (faces or bodies), spatial frequency (HSF, LSF, NSF), and the following interactions: group-by-stimuli-by-spatial frequency, group-by-stimuli, and group-by-spatial frequency. Significant interaction effects were followed up by post-hoc Tukey’s tests between groups to test specific hypotheses. P-values < 0.05 were considered to be significant. Analyses were conducted separately for the three ratings. To test associations with clinical variables we used linear mixed models with EDE scores (in the AN group only) and BDD-YBOCS scores (in the BDD group only) as covariates of interest, in addition to testing for spatial frequency-by-EDE/BDD-YBOCS interactions. In order to interpret the statistical size of the effects, we computed Cohen’s f2 for linear mixed models 45. Values of Cohen’s f2=0.02, 0.15, 0.35 are interpreted as being small, medium, and large, respectively 46.
RESULTS
Demographics
The groups did not differ significantly on age, gender, or years of education (Table 1). Prevalences of comorbid diagnoses were 32% and 50% in participants with AN and BDD, respectively. In the AN group 1 had MDD, 1 had dysthymic disorder, 2 had GAD, and 3 had MDD and GAD. In the BDD group 6 had MDD, 2 had dysthymic disorder, 1 had social phobia, 1 had agoraphobia, 1 had panic disorder with agoraphobia, 1 had MDD and GAD, 1 had MDD and social phobia, and 2 had MDD and social phobia and GAD. Nineteen AN participants met DSM-IV criteria for restricting type and 3 were classified as binge-eating/purging type. Ten BDD participants had face concerns only, 1 had body concerns only, and 19 had face and body concerns. The AN group had a mean EDE score of 3.16 ± 1.58. This is in the range of what is documented in underweight AN samples47, yet was expected given the inclusion criteria of needing to currently meet all DSM-IV criteria for AN aside from low weight and amenorrhea, and the fact that there was no minimum duration of weight-restoration.
Table 1.
Demographics and psychometric scores
| Characteristic | AN (N = 22) | BDD (N = 30) | CON (N = 39) | P Value | |||
|---|---|---|---|---|---|---|---|
| Mean | S.D. | Mean | S.D. | Mean | S.D. | ||
| Age (years) | 21.5 | 4.5 | 22.8 | 5.0 | 21.6 | 4.6 | NS |
| Female/male | 20/2 | 24/6 | 33/6 | NS | |||
| Education (years) | 13.9 | 3.2 | 14.7 | 3.4 | 13.8 | 2.8 | NS |
| Body mass index | 20.3 | 1.3 | 22.6 | 3.3 | 22.6 | 3.3 | P < 0.01 |
| EDE score | 3.16 | 1.58 | N/A | - | N/A | - | - |
| YBC scores | 21.5a | 10.5 | N/A | - | N/A | - | - |
| BDD-YBOCS score | N/A | - | 29.5 | 5.5 | N/A | - | - |
| HAMA score | 8.5 | 6.3 | 10.1 | 6.2 | N/A | - | NS |
| MADRS score | 13.1 | 9.9 | 15.0 | 7.6 | N/A | - | P=0.05 |
| BABS score | 9.0b | 6.8 | 14.3 | 3.5 | N/A | - | P <0.01 |
| Comorbid diagnoses | 7(32%) | 15(50%) | N/A | NS | |||
| BDD appearance concerns |
Face only: 10 Body only: 1 Face & Body: 19 |
||||||
Abbreviations: BDD, body dysmorphic disorder; BDD-YBOCS, BDD version of the Yale-Brown Obsessive-Compulsive Scale; BABS, Brown Assessment of Beliefs Scale; EDE; Eating Disorder Examination interview; MADRS, Montgomery-Åsberg Depression Rating Scale; N/A, not applicable, S.D., Standard deviation
YBC, Yale-Brown-Cornell eating disorder scale was available for 14 AN participants. HARS, Hamilton Anxiety Rating Scale.
BABS scores was available for 15 AN participants.
Attractiveness
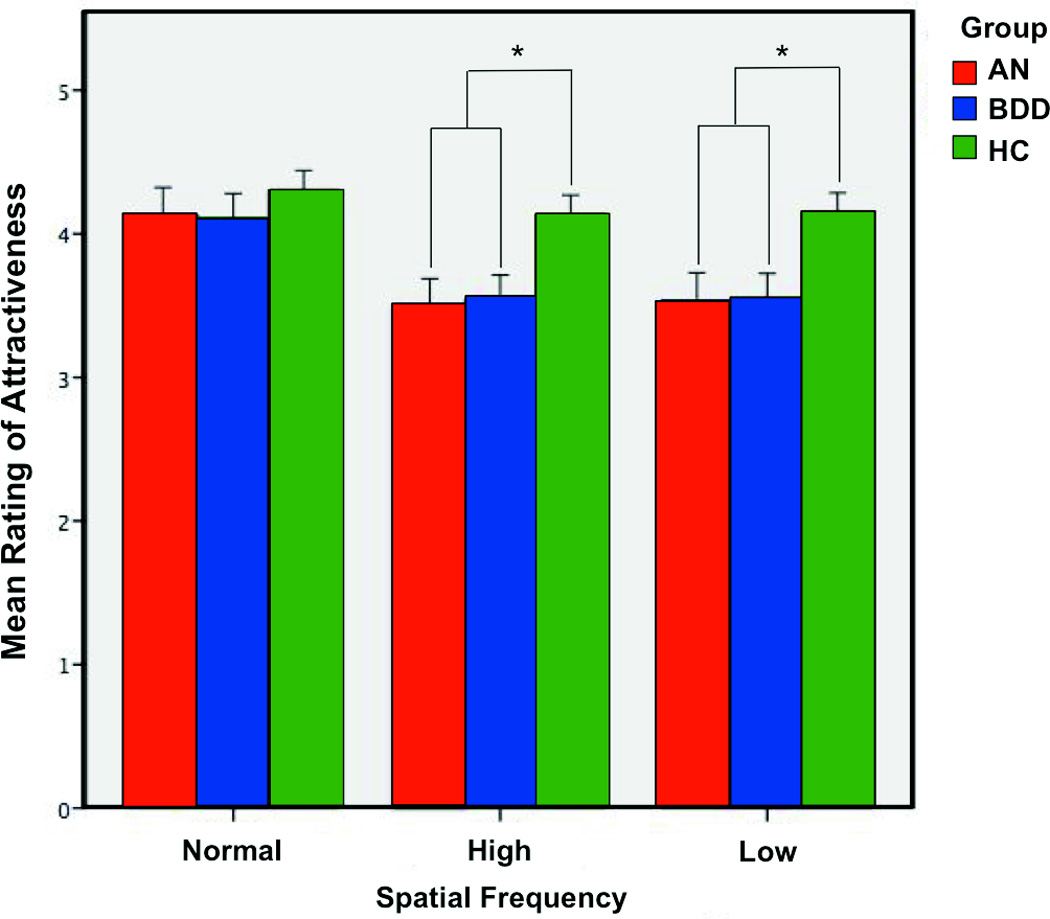
We did not find significant group-by-stimulus-by-spatial frequency (F4 8538 = 0.49, p = 0.74, Cohen’s f2<0.001) or group-by-stimulus (F2 8542 = 2.00, p = 0.14, Cohen’s f2=<0.001) interactions. However, there was a significant group-by-spatial frequency interaction (F4 8538 = 4.70, p = 0.001, Cohen’s f2= 0.001). This interaction was seen between the AN vs. HC groups (F2 5703 = 7.37, p = 0.001, Cohen’s f2=0.001) and BDD vs. HC groups (F2 6458 = 6.63, p = 0.001, Cohen’s f2= 0.001) but not for the AN vs. BDD comparison (F2 4915 = 0.08, p = 0.92, Cohen’s f2=<0.001); see Figure 2. Further follow-up analyses by spatial frequency revealed that at NSF, neither the BDD (p = 0.45) nor the AN group (p = 0.50) differed significantly from HC. At HSF, however, the AN group (p = 0.039) and BDD group (p = 0.046) had significantly lower attractiveness ratings than HCs, but the AN and BDD groups did not differ from each other (p = 0.70). This pattern was similar for LSF: the AN group (p = 0.031) and BDD group (p = 0.018) had significantly lower ratings of attractiveness than HCs, but the AN group did not differ significantly from the BDD group (p = 0.65). In brief, both AN and BDD had lower attractiveness ratings than HC for high-detail and low-detail images, but all groups had similar ratings for normal images.
Figure 2.
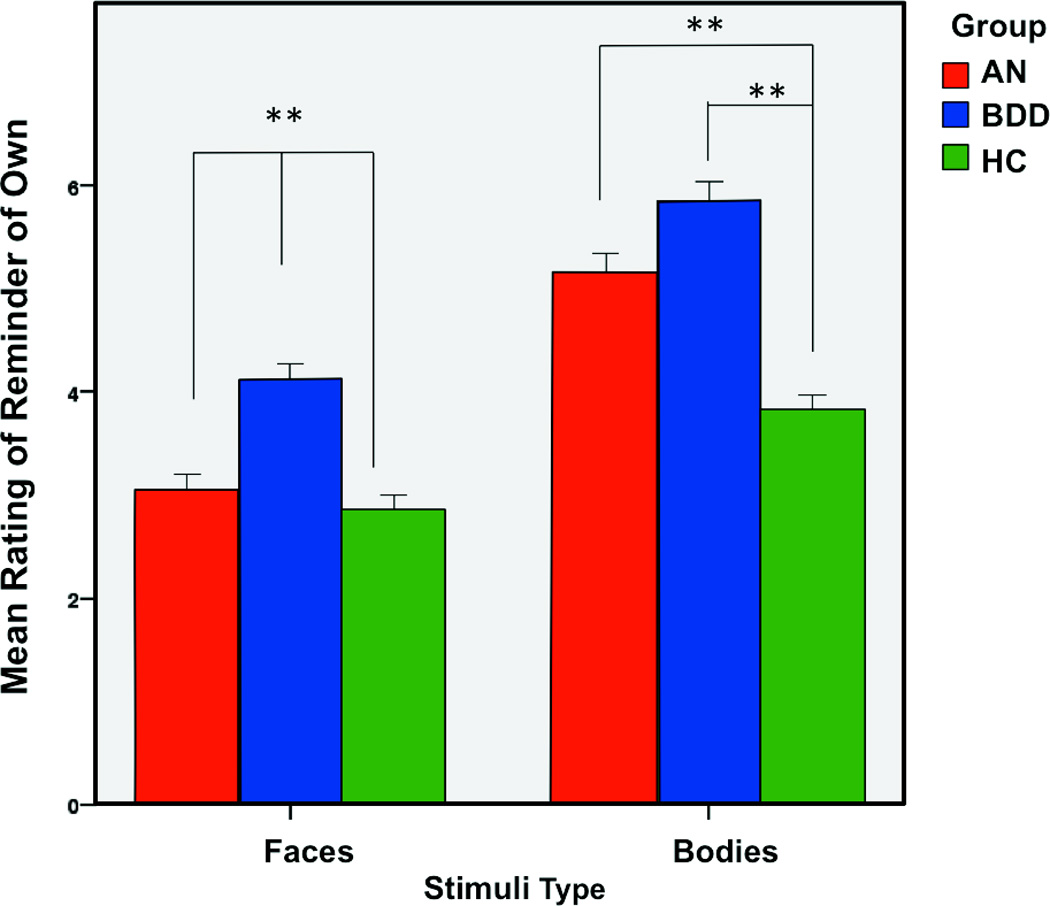
Thoughts triggered of own face/body
The three-way interaction among group, spatial frequency, and stimulus type for thoughts triggered of own face/body was not significant (F4 4306 = 0.78, p = 0.54, Cohen’s f2<0.001). There was a significant group-by-stimulus (F2 4339 = 18.24, p < 0.001, Cohen’s f2=0.004) interaction effect, but no significant group-by-spatial frequency (F4 4306 = 0.90, p = 0.46, Cohen’s f2=<0.001) interaction effect. Follow-up analyses revealed that there were significant group-by-stimulus effects for AN vs. BDD groups (F1 2932 = 7.76, p < 0.005, Cohen’s f2= 0.003), AN vs. HC groups (F1 4856 = 71.60, p < 0.001, Cohen’s f2=0.015) and HC vs. BDD groups (F1 3102 = 13.20, p < 0.001, Cohen’s f2= 0.004). All groups differed significantly in their ratings of thoughts triggered of their own appearance for faces, with BDD rating highest, followed by AN and then HC (all p’s < 0.001). For bodies, the BDD group had highest ratings, followed by AN, and then HC groups. Although the difference between AN and BDD groups (p = 0.07) was not significant, there was a significant difference between BDD and HC groups (p < 0.001) and between AN and HC groups (p < 0.001), see Figure 3. In sum, both faces and bodies stimuli elicited stronger triggering of thoughts of own appearance in a pattern of BDD > AN > HC, but for bodies the difference between BDD and AN was not significant.
Figure 3.
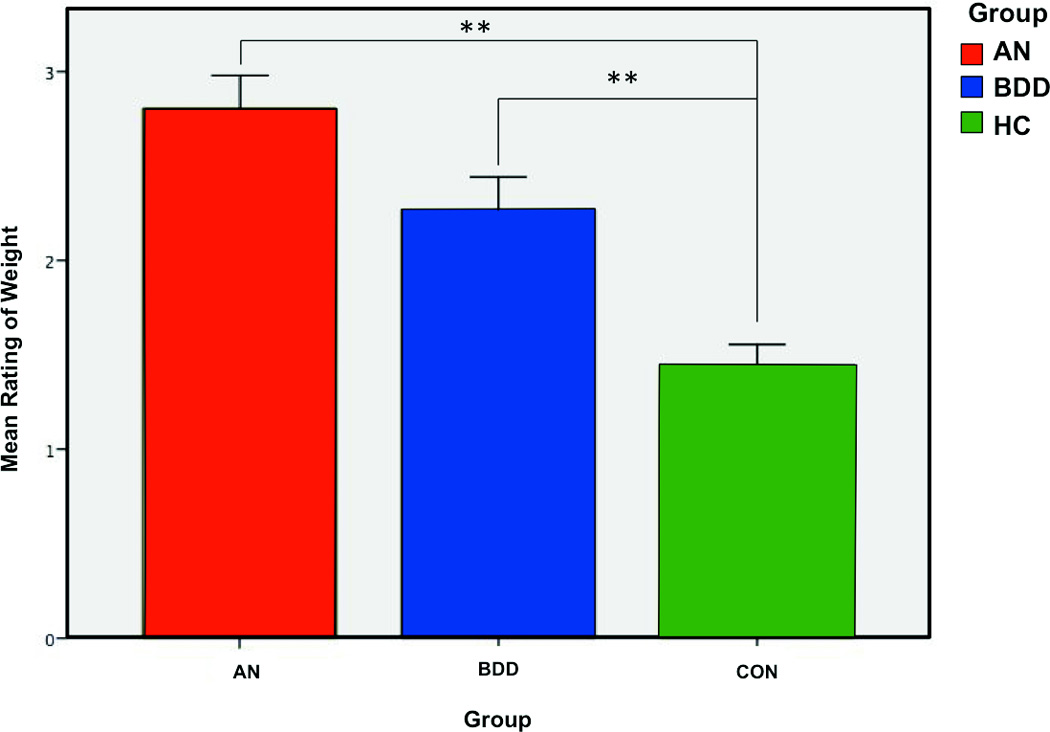
Overweight/underweight ratings of bodies
There was a significant group effect (F2 90 = 11.47, p < 0.001, Cohen’s f2=0.13) for ratings of overweight/underweight bodies, but no spatial-frequency effect (F2 4187 = 1.43, p = 0.24, Cohen’s f2<0.001) or group-by-spatial frequency effect (F4 4187 = 1.00, p = 0.41, Cohen’s f2<0.001). AN vs. BDD groups did not differ significantly from each other (p = 0.13), but other groups did differ: AN vs. HC groups (p < 0.001), and BDD vs. HC groups (p = 0 .001; see Figure 4), with the AN group rating bodies as most overweight, followed by the BDD group, and then the HC group. Similar to our results for attractiveness ratings and thoughts triggered of own body, when compared to HC, both BDD and AN differed in their assessments of overweight/underweight bodies, but the two groups did not differ from each other.
Figure 4.
Associations with clinical variables
As hypothesized, those with worse eating disorder symptoms (EDE scores) had significantly higher overweight ratings (F1 22.013 = 7.96, β = 0.52, p = 0.01) and were more triggered to think of their own appearance for bodies (F1 21.00 = 4.83, β = 0.48 p < 0.04). Also as predicted, eating disorder severity was not significantly associated with face attractiveness ratings (F1 22 = 0.06, β = −0.058, p = 0.80); however, contrary to our hypotheses, it was not significantly associated with lower bodies attractiveness ratings (F1 22 = 0.39, β = −0.097, p = 0.54).
As hypothesized, those with worse BDD symptoms (higher BDD-YBOCS scores) were more triggered to think of their own appearance for bodies (F1 29.99 = 5.16, β = 0.15 p < 0.03) although there was only a trend level association for faces (F1 29.99 = 3.37, β = 0.069, p < 0.08). There was not a significant association between BDD severity and higher overweight ratings (F1 29.93 = 1.94, β = 0.11, p = 0.17); however, the interaction between spatial frequency and BDD-YBOCS was significant (F2 1395 = 3.48, β = −0.091, p = 0.031). Follow-up analyses revealed that those with worse BDD symptoms had significantly higher overweight ratings specifically for LSF images (F1 30 = 5.15, β = 0.11, p < 0.03). There was not a significant association between BDD severity and lower attractiveness ratings for faces (F1 30.00 =0.093, β = 0.037, p = 0.76) or bodies (F1 29.98= 0.004, β = −0.021, p = 0.95), contrary to our hypotheses.
Exploratory Analyses
We conducted post hoc analyses to explore whether groups differed in ratings depending on the gender of the stimulus. Group differences in attractiveness ratings did not differ significantly depending on the gender of the stimulus (all p values > 0.1). Thoughts of own appearance when viewing faces and bodies were triggered to a greater degree in AN than HC depending on the stimulus gender, showing a greater effect for same gender stimuli (interaction effect between group and stimulus gender: F1 5681 = 30.06, p < 0.001, Cohen’s f2=0.005). A similar interaction effect was observed in BDD (F1 6433 = 19.90, p < 0.001, Cohen’s f2= 0.003) but AN and BDD did not differ significantly in this regard (F1 4912 = 0.224, p = 0.64, Cohen’s f2<0.001). Similarly, those with AN rated bodies as more overweight than HC depending on the stimulus gender, showing a greater effect for same gender stimuli (interaction effect between group and stimulus gender: F1 2789 = 12.74, p < 0.001, Cohen’s f2= 0.005). This was not the case for BDD (F1 3160 = 0.28, p = 0.60, Cohen’s f2<0.001). In addition, AN rated bodies as more overweight than BDD depending on the stimulus gender (F1 2418 = 5.32, p < 0.03, Cohen’s f2=0.002) showing a greater effect for same gender. Thus, while AN and BDD have more thoughts of their own appearance triggered when viewing faces and bodies than HC in general, the difference from HC is greater for same stimuli gender. A similar effect for overweight ratings is observed in AN but not BDD. However, the gender of the stimuli had no effect on group differences in attractiveness ratings.
We also conducted exploratory analyses to determine if there were differences in ratings based on type of appearance concern in BDD. We divided the BDD group into face-only concerns (n=10) and body-only plus body-and-face concerns (n=20). For the group-level analysis, the small sample size with face-only concerns precluded a meaningful separate analysis; thus, we re-analyzed the data using the body-only plus body-and-face concerns subgroup, comparing it to the AN and HC groups. For attractiveness ratings, the results were similar to the results from the whole BDD group, except that lower ratings for LSF images were only at trend level (p = 0.07, vs. p < 0.02 for the whole BDD group). For triggering thoughts of own appearance, the results were similar as for the whole BDD group except that there was only a trend-level group-by-stimulus effect for AN vs. BDD (F1 2327 = 2.75 p = 0.10, Cohen’s f2= 0.001), vs. F1 2932 = 7.77 p <0.005, Cohen’s f2= 0.003 for the whole BDD group). For overweight/underweight ratings, results were similar to the analysis using the whole BDD group. For associations with BDD-YBOCS in the BDD group, we used type of appearance concern as a covariate. There was no significant effect of type of appearance concern for attractiveness or overweight ratings. For triggering thoughts of own appearance, there was a significant interaction effect between BDD-YBOCS and type of appearance concern for bodies (F1 30 = 14.62, p < 0.001, β = −0.39) but not for faces (F1 30.00 = 0.83, p = 0.37, β = −0.15). Follow-up analyses for bodies revealed that the association with BDD-YBOCS was significant in the body-only plus body-and-face group (F1 20 = 20.33, β = 0.30, p < 0.001), but not in the face-only group (F1 10 = 1.46, β = −0.09, p = 0.25) such that worse symptoms were associated with bodies triggering thoughts of their own appearance to a greater degree.
In sum, individuals with BDD whose appearance concerns include their body rate attractiveness of faces and bodies with low detail more similarly to HC, but they may be more similar to AN in terms of thoughts of own appearance being triggered by faces or bodies. In addition, the association between severity of BDD symptoms and triggering thoughts of own appearance when viewing bodies is more specific to those whose concerns include their own body.
Exploratory analyses of associations between BMI ratings are reported in Supplementary Materials. We conducted these to examine associations between this important physical characteristic in participants with how they perceive others’ appearance, as has been documented in previous studies14, 48.
DISCUSSION
In summary, individuals with AN and BDD differ from a non-clinical population in their perceptions of attractiveness and weight, and the extent to which face and body stimuli trigger them to think of their own appearance. Specifically: (1) Each clinical group rates others’ bodies as being more overweight compared to the ratings of controls; (2) they are triggered to think more of their own appearance for faces and bodies than controls; and (3) attractiveness ratings for AN and BDD are more influenced by coarse- and fine-level visual information than controls.
Since face images are not related to their primary appearance concern, it is perhaps surprising that AN participants rate faces as less attractive and as triggering more thoughts of their own appearance than HC participants do. Thus, AN and BDD exhibit similar abnormalities in appearance valuations that extend beyond themselves to others’ appearance, and for physical features that are related and unrelated to their primary appearance concern. Our recent imaging data (the results of which were available only after we had formulated hypotheses and conducted the current study) might suggest that the neural underpinnings of this finding could be related to a common abnormality in visual processing of emotion-neutral stimuli, 8, 21 but this idea should be considered with circumspection given that we did not directly measure neural responses in this study.
Attractiveness Rating
When evaluating attractiveness of bodies and faces at a naturalistic, normal spatial frequency, AN and BDD individuals did not show significantly different ratings than HC. However, when only high or low levels of detail are present, individuals with AN and BDD perceive attractiveness as significantly lower than HC. Previous brain imaging studies in BDD have shown aberrant patterns of hypoactivation in visual systems for low detail (LSF) images of own face, familiar face, and object stimuli 9, 10, 44. As mentioned above, a study that included AN and BDD showed that both groups, compared to healthy controls, displayed hypoactivity in the dorsal ventral stream and early secondary visual processing regions when viewing LSF faces21. While future studies will be required to investigate this, these results may reflect common, diminished global and holistic information processing, uncovered by the same LSF image “probes” as in the current study, which could contribute to facial perception that is lower in attractiveness. Also in that study21, greater activity in fusiform cortex in BDD correlated with lower attractiveness ratings of faces, consistent with our current findings of decreased attractiveness ratings for HSF faces. An EEG event-related potential study that tested responses to the same image types found abnormal P100 amplitudes in AN and delayed N170 latencies in AN (and at trend level in BDD); however the patterns were not specific to LSF and HSF images and thus their relationship to lower attractiveness ratings found in the current study is not clear 33.
Another study demonstrated that for both own-face and familiar-face processing, individuals with BDD with higher levels of anxiety exhibited greater neural activation in the ventral visual stream when viewing images of their own face and a familiar (famous) face 49. Thus, being in an anxious state may enhance detail extraction performed by the ventral visual stream. We speculate that this could result in a perception of lower attractiveness when viewing faces, as detailed/analytic visual processing may be required to detect flaws and imperfections. As anxiety is commonly experienced by individuals with BDD and AN, this may represent a phenotypic feature that contributes to their abnormal subjective perception.
With respect to the normal detail faces, results in the current study differ somewhat from a previous study in BDD of attractiveness ratings of others’ faces15, 50. That study used three categories of face images—”average,” “attractive,” and “unattractive”—as determined by four independent investigators15. The BDD group rated these “attractive” faces as more attractive than the HC and an obsessive-compulsive disorder comparison group, and rated the attractiveness of their own faces significantly lower. The authors posited that individuals with BDD might have maladaptive perfectionistic beliefs about physical attractiveness, such that they undervalue their own attractiveness and overvalue the attractiveness of those they believe to be closer to possessing ideal facial characteristics. However, due to methodological differences and possible differences in overall attractiveness level of the face stimuli, these results are difficult to compare to those of the current study. A study of weight-restored individuals with AN found no significant differences from HC in attractiveness ratings of faces or bodies16, which is consistent with the findings in the current study for unaltered photos.
Attractiveness ratings for bodies by AN participants were investigated in a study by Horndasch et al. 13 who found that AN is associated with lower attractiveness ratings for normal or overweight bodies13. Indeed, that study found participants with AN rated only extremely underweight bodies as more attractive than HCs did. Our study did not include photos of extremely underweight bodies; therefore, our thin and overweight bodies could have resulted in lower ratings of attractiveness in the AN group.
Several previous studies have found attentional biases in regards to attractive and unattractive features associated with eating disorder symptoms or BMI, when viewing own and others’ bodies48, 51, 52. In one study that utilized eye-tracking, individuals with high degree of eating disorder severity attended more to the most attractive features of others’ bodies than did controls, who attended more to the least attractive features of others’ bodies51. When viewing their own body, this pattern in the high eating disorder severity group was reversed. Roefs, et al. (2008) similarly found enhanced attention to others’ attractive body parts and to own unattractive body parts that was correlated with both their BMI and how unattractive they rated themselves48. Another study found that individuals’ drive for thinness was associated with attentional bias specifically to waist, hips, legs, and arms in photos of others53. These are body regions that could convey information about body fat and hence an individual’s weight. Smeets et al. (2011) experimentally induced visual attentional bias towards own unattractive body parts, which resulted in lower self-body satisfaction; conversely enhancing attention to own attractive body parts resulted in higher self-body satisfaction52. In another study, individuals with eating disorders showed greater attentional bias than controls towards “negative shape” pictures of others’ body parts (e.g. large thighs) as well as “neutral shape” pictures (e.g. elbows), but no bias for “positive shape” pictures (e.g. slim figures)54. Although these findings may seem to diverge from the previous ones, it is important to note that in this study the attentional biases were measured to each image in its entirely (which may have been a body part, or a whole body, for example) rather than measuring attention directed to specific body areas in the context of a whole body, as in the previous studies. Moreover, the latter study was conducted in a clinical eating disorder population while the previous ones were in nonclinical samples.
In sum, biased attention to specific body parts could be a factor that influences appraisals of attractiveness, yet also could be influenced by the attractiveness of the image. This could potentially set up a negative feedback loop in which negative self body image is perpetuated by where visual attention is directed. Moreover, executive functioning disturbances such as those related to set-shifting, which have been identified in both AN and BDD55–57, could further contribute to individuals being “locked on” to specific areas or body parts where the attention is focused. In the current study, such attentional biases could have similarly influenced attractiveness ratings. However, this remains to be determined, as we did not measure directed attention towards specific body parts with eye-tracking or other methods.
Triggering thoughts of own appearance
Our results support the hypothesis that individuals with BDD are more triggered to think of their own faces when viewing others’ faces than individuals with AN or HC. This is in agreement with clinical observations that individuals with BDD often report comparing others’ facial features with their own; individuals with BDD commonly assert that, while interacting with others, they scrutinize aspects of the other person’s appearance that they believe to be flawed on their own face5. Previous studies have revealed that individuals with BDD have an attentional bias for flaws in their own faces and in unfamiliar faces 58, and it follows that viewing unfamiliar faces might trigger BDD participants to think of their own face if they perceive flaws in both. To our knowledge, no previous studies have examined attractiveness ratings for bodies in individuals with BDD.
We found that participants with AN were more triggered to think of their own bodies when viewing others’ bodies than the HC group, and the degree of triggering thoughts of own appearance was associated with severity of eating disorder symptoms. To our knowledge a similar study has not previously been conducted. However, Blechert et al.59, found that individuals with AN had an attentional bias for self-photos over other-photos, and this bias was associated with their body dissatisfaction. One possible explanation of those results is that a tendency for self-referential thinking may have influenced the attentional bias. Interestingly, those with AN were more triggered to think of their own appearance when viewing faces. However, it is important to note that faces can convey information about an individuals’ weight. Because of this, we cannot rule out the possibility that the apparent weight of the individual in the photograph could have contributed to triggering thoughts of AN participants’ own appearance, as we did not acquire overweight/underweight ratings of faces.
Similarly, individuals with BDD were more triggered to think of their own appearance when viewing bodies. Moreover, BDD symptom severity was associated with greater triggering of thoughts of own appearance. Similar previous studies have not been conducted in BDD, although one study found that individuals with BDD have negative interpretative biases for body-related scenarios50.
Overweight/underweight ratings
As expected, the AN group rated others’ bodies to be more overweight than the HC group, and the degree of overweight rating was associated with severity of eating disorder symptoms. This is consistent with previous studies that suggest individuals with AN tend to assess underweight women as being of normal weight (and more attractive) than do HCs 13, 60. Previous studies have also found abnormal weight-overestimation in AN13, 14, 16, 33. Weight overestimation of own and others’ bodies could therefore signify that this is a general characteristic of the disorder. Further supporting this is the observation in the current study that the degree of overweight ratings was even greater than HC for opposite gender stimuli. A possible neural correlate is suggested by the finding that AN and BDD have neural hypoactivity in dorsal visual areas (that process holistic perceptions of images, such as weight) when viewing LSF images of faces and houses21, although it has yet to be confirmed when viewing bodies. Interestingly, in the current study worse BDD symptoms were associated with higher overweight ratings specifically for LSF bodies, though tentative, this suggests that a similar physiological phenomenon may be operative at least in the BDD group.
Clinical relevance
Our findings provide evidence that individuals with AN and BDD have abnormal judgments of others’ appearance, which may have implications for developing and testing new treatment strategies. Current treatments that only target self-perception may not be sufficient to adequately treat these disorders, as more general attentional biases and visual processing patterns may be operative. Furthermore, continued negative judgments of others could affect social-interpersonal relationships. Some current CBT treatments involve modifying attentional biases towards others’ appearance (see, for example 61). New research treatments protocols could test the effectiveness of targeting the perception of others as well as of the self. In addition, as thoughts of own appearance were triggered to a high degree in AN and BDD, it is very possible that they were engaging in social comparisons. Engaging in social comparisons, including negative comparisons of own body to those of other women, has been linked to eating disorder symptoms62, and is a common behavior in BDD5. Modification of cognitions or behaviors related to social comparison could be useful targets for treatment strategies.
Limitations
A limitation to consider is that we studied weight-restored AN, and thus results may not necessarily be generalizable to underweight AN populations. However, we conducted exploratory analyses of the relationship between BMI and subjective ratings in a slightly larger dataset that included underweight (n=11) and weight-restored (n=22) AN. In AN, BMI was positively associated with attractiveness ratings for bodies (but not faces), but not with triggering thoughts of own appearance or with overweight ratings. The mean ages (21.5 ± 4.5 for AN, 22.8 ± 5.0 for BDD, and 21.6 ± 4.6 for HC) were relatively young, which limits generalizability to older samples. Another limitation is that we did not collect subjective ratings on weight for photographs of faces; thus, we were unable to assess whether perceptions of weight applied to both bodies and faces. Additionally, we did not present body stimuli that represented extremely underweight bodies, which could possibly have elicited increased ratings of attractiveness from the AN group. The order of ratings of faces followed by bodies was not counterbalanced. History of previous CBT was not assessed, which could have influenced attentional biases in participants.
Conclusions and future directions
Overall, our findings suggest that appearance judgments in individuals with AN and BDD extend beyond the self to negative judgments of others as well. A particularly interesting finding is the response of individuals with AN to faces: despite faces not being typically part of their primary concerns, AN had lower attractiveness ratings (for high-detail and low-detail images) and higher triggering thoughts of own appearance ratings than controls. Similarly, in BDD, overweight ratings and triggering thoughts of own appearance ratings for bodies were higher than in controls. Only for faces did BDD score higher for triggering thoughts of own appearance than AN; otherwise differences between these groups were not significant. However, those with BDD whose appearance concerns included their body did not show significant differences in thoughts triggered of their appearance from the AN group. These results suggest similarities in phenotypes of appearance judgments of others in these two disorders, that may further intersect when their own appearance concerns overlap.
Future research should investigate how these ratings change before and after current standard-of-care treatments for AN and BDD. Other future avenues of investigation could include measuring implicit vs. explicit attractiveness beliefs 63, 64 and how mood or anxiety state influences appearance ratings. In addition, future studies using neuroimaging could test for abnormalities associated with appearance judgments and self-referential thinking that may occur while viewing faces and bodies in BDD and AN, to provide an understanding of the neurobiological processes underlying these phenomena. Another promising avenue of research is in applying perceptual retraining techniques65, 66 to correct/re-adjust proposed abnormalities in visual information processing pathways8, 12, 21, 33.
Supplementary Material
Acknowledgments
We thank Tsz Man Lai for his assistance in data collection and Francesca Morfini for reviewing the manuscript.
Footnotes
Disclosures
Authors Moody, Shen, Hutcheson, Lawrence, Kalsa, Madsen, Strober, Henretty, and Feusner report no competing interests.
References
- 1.American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. 5th. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 2.Strober M, Freeman R, Lampert C, Diamond J. The association of anxiety disorders and obsessive compulsive personality disorder with anorexia nervosa: Evidence from a family study with discussion of nosological and neurodevelopmental implications. International Journal of Eating Disorders. 2007;40:S46–S51. doi: 10.1002/eat.20429. [DOI] [PubMed] [Google Scholar]
- 3.Hartmann AS, Greenberg JL, Wilhelm S. The relationship between anorexia nervosa and body dysmorphic disorder. Clin Psychol Rev. 2013;33(5):675–685. doi: 10.1016/j.cpr.2013.04.002. [DOI] [PubMed] [Google Scholar]
- 4.Hartmann AS, Thomas JJ, Wilson AC, Wilhelm S. Insight impairment in body image disorders: delusionality and overvalued ideas in anorexia nervosa versus body dysmorphic disorder. Psychiatry Res. 2013;210(3):1129–1135. doi: 10.1016/j.psychres.2013.08.010. [DOI] [PubMed] [Google Scholar]
- 5.Phillips KA. The Broken Mirror. New York: Oxford University Press; 2005. [Google Scholar]
- 6.Grant JE, Phillips KA. Is anorexia nervosa a subtype of body dysmorphic disorder? Probably not, but read on. Harv Rev Psychiatry. 2004;12(2):123–126. doi: 10.1080/10673220490447236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kittler JE, Menard W, Phillips KA. Weight concerns in individuals with body dysmorphic disorder. Eat Behav. 2007;8(1):115–120. doi: 10.1016/j.eatbeh.2006.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moody TD, Sasaki MA, Bohon C, Strober MA, Bookheimer SY, Sheen CL, Feusner JD. Functional connectivity for face processing in individuals with body dysmorphic disorder and anorexia nervosa. Psychological medicine. 2015;45(16):3491–3503. doi: 10.1017/S0033291715001397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feusner JD, Hembacher E, Moller H, Moody TD. Abnormalities of object visual processing in body dysmorphic disorder. Psychological medicine. 2011:1–13. doi: 10.1017/S0033291711000572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Feusner JD, Moody T, Bohon C, Arienzo D, Klomhaus A, Mason K, Strober M. Visual processing in anorexia nervosa and body dysmorphic disorder. American College of Neuropsychopharmacology. 2010;35:S265. [Google Scholar]
- 11.Feusner JD, Arienzo D, Li W, Zhan L, GadElkarim J, Thompson PM, Leow AD. White matter microstructure in body dysmorphic disorder and its clinical correlates. Psychiat Res-Neuroim. 2013;211(2):132–140. doi: 10.1016/j.pscychresns.2012.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arienzo D, Leow A, Brown JA, Zhan L, GadElkarim J, Hovav S, Feusner JD. Abnormal Brain Network Organization in Body Dysmorphic Disorder. Neuropsychopharmacology. 2013;38(6):1130–1139. doi: 10.1038/npp.2013.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Horndasch S, Heinrich H, Kratz O, Mai S, Graap H, Moll G. Perception and evaluation of women’s bodies in adolescents and adults with anorexia nervosa. European archives of psychiatry and clinical neuroscience. 2015:1–11. doi: 10.1007/s00406-015-0603-3. [DOI] [PubMed] [Google Scholar]
- 14.Tovee MJ, Emery JL, Cohen-Tovee EM. The estimation of body mass index and physical attractiveness is dependent on the observer’s own body mass index. Proc Biol Sci. 2000;267(1456):1987–1997. doi: 10.1098/rspb.2000.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Buhlmann U, Etcoff NL, Wilhelm S. Facial attractiveness ratings and perfectionism in body dysmorphic disorder and obsessive-compulsive disorder. J Anxiety Disord. 2008;22(3):540–547. doi: 10.1016/j.janxdis.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 16.Watson KK, Werling DM, Zucker NL, Platt ML. Altered social reward and attention in anorexia nervosa. Frontiers in psychology. 2010;1:36. doi: 10.3389/fpsyg.2010.00036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Campbell FW, Robson JG. Application of Fourier analysis to the visibility of gratings. The Journal of physiology. 1968;197(3):551–566. doi: 10.1113/jphysiol.1968.sp008574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morrison DJ, Schyns PG. Usage of spatial scales for the categorization of faces, objects, and scenes. Psychonomic bulletin & review. 2001;8(3):454–469. doi: 10.3758/bf03196180. [DOI] [PubMed] [Google Scholar]
- 19.Costen NP, Parker DM, Craw I. Effects of high-pass and low-pass spatial filtering on face identification. Perception & psychophysics. 1996;58(4):602–612. doi: 10.3758/bf03213093. [DOI] [PubMed] [Google Scholar]
- 20.Norman J, Ehrlich S. Spatial frequency filtering and target identification. Vision research. 1987;27(1):87–96. doi: 10.1016/0042-6989(87)90145-3. [DOI] [PubMed] [Google Scholar]
- 21.Li W, Lai TM, Bohon C, Loo SK, McCurdy D, Strober M, et al. Anorexia nervosa and body dysmorphic disorder are associated with abnormalities in processing visual information. Psychological medicine. 2015:1–12. doi: 10.1017/S0033291715000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spehar B, Wong S, van de Klundert S, Lui J, Clifford CW, Taylor RP. Beauty and the beholder: the role of visual sensitivity in visual preference. Frontiers in human neuroscience. 2015;9:514. doi: 10.3389/fnhum.2015.00514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Spehar B, Clifford CWG, Newell BR, Taylor RP. Universal aesthetic of fractals. Comput Graph-Uk. 2003;27(5):813–820. [Google Scholar]
- 24.Juricevic I, Land L, Wilkins A, Webster MA. Visual discomfort and natural image statistics. Perception. 2010;39(7):884–899. doi: 10.1068/p6656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;(59 Suppl 20):22–33. quiz 4-57. [PubMed] [Google Scholar]
- 26.Dufresne RG, Phillips KA, Vittorio CC, Wilkel CS. A screening questionnaire for body dysmorphic disorder in a cosmetic dermatologic surgery practice. Dermatol Surg. 2001;27(5):457–462. doi: 10.1046/j.1524-4725.2001.00190.x. [DOI] [PubMed] [Google Scholar]
- 27.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32(1):50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 28.Eisen JL, Phillips KA, Baer L, Beer DA, Atala KD, Rasmussen SA. The Brown Assessment of Beliefs Scale: reliability and validity. Am J Psychiatry. 1998;155(1):102–108. doi: 10.1176/ajp.155.1.102. [DOI] [PubMed] [Google Scholar]
- 29.Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- 30.Phillips KA, Hollander E, Rasmussen SA, Aronowitz BR, DeCaria C, Goodman WK. A severity rating scale for body dysmorphic disorder: development, reliability, and validity of a modified version of the Yale-Brown Obsessive Compulsive Scale. Psychopharmacology Bulletin. 1997;33(1):17–22. [PubMed] [Google Scholar]
- 31.Fairburn CG, Cooper Z. M.E. O. Cognitive Behavior Therapy and Eating Disorders. New York: The Guilford Press; 2008. [Google Scholar]
- 32.Mazure CM, Halmi KA, Sunday SR, Romano SJ, Einhorn AM. The Yale-Brown-Cornell Eating Disorder Scale: development, use, reliability and validity. J Psychiatr Res. 1994;28(5):425–445. doi: 10.1016/0022-3956(94)90002-7. [DOI] [PubMed] [Google Scholar]
- 33.Li W, Lai TM, Loo SK, Strober M, Mohammad-Rezazadeh I, Khalsa S, Feusner J. Aberrant early visual neural activity and brain-behavior relationships in anorexia nervosa and body dysmorphic disorder. Frontiers in human neuroscience. 2015;9:301. doi: 10.3389/fnhum.2015.00301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Veale D, Boocock A, Gournay K, Dryden W, Shah F, Willson R, Walburn J. Body dysmorphic disorder. A survey of fifty cases. British Journal of Psychiatry. 1996;169(2):196–201. doi: 10.1192/bjp.169.2.196. [DOI] [PubMed] [Google Scholar]
- 35.Gunstad J, Phillips KA. Axis I comorbidity in body dysmorphic disorder. Comprehensive Psychiatry. 2003;44(4):270–276. doi: 10.1016/S0010-440X(03)00088-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zimmerman M, Mattia JI. Body dysmorphic disorder in psychiatric outpatients: recognition, prevalence, comorbidity, demographic, and clinical correlates. Compr Psychiatry. 1998;39(5):265–270. doi: 10.1016/s0010-440x(98)90034-7. [DOI] [PubMed] [Google Scholar]
- 37.Phillips KA, Stout RL. Associations in the longitudinal course of body dysmorphic disorder with major depression, obsessive-compulsive disorder, and social phobia. Journal of psychiatric research. 2006;40(4):360–369. doi: 10.1016/j.jpsychires.2005.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Phillips KA, Didie ER, Menard W, Pagano ME, Fay C, Weisberg RB. Clinical features of body dysmorphic disorder in adolescents and adults. Psychiatry Reseach. 2006;141(3):305–314. doi: 10.1016/j.psychres.2005.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hollander E, Cohen LJ, Simeon D. Body dysmorphic disorder. Psychiatric Annals. 1993;23:359–364. [Google Scholar]
- 40.Perugi G, Akiskal HS, Giannotti D, Frare F, Di Vaio S, Cassano GB. Gender-related differences in body dysmorphic disorder (dysmorphophobia) J Nerv Ment Dis. 1997;185(9):578–582. doi: 10.1097/00005053-199709000-00007. [DOI] [PubMed] [Google Scholar]
- 41.Swinbourne JM, Touyz SW. The co-morbidity of eating disorders and anxiety disorders: a review. Eur Eat Disord Rev. 2007;15(4):253–274. doi: 10.1002/erv.784. [DOI] [PubMed] [Google Scholar]
- 42.Kennedy SH, Kaplan AS, Garfinkel PE, Rockert W, Toner B, Abbey SE. Depression in anorexia nervosa and bulimia nervosa: discriminating depressive symptoms and episodes. J Psychosom Res. 1994;38(7):773–782. doi: 10.1016/0022-3999(94)90030-2. [DOI] [PubMed] [Google Scholar]
- 43.S Ruffolo J, Phillips KA, Menard W, Fay C, Weisberg RB. Comorbidity of body dysmorphic disorder and eating disorders: severity of psychopathology and body image disturbance. International Journal of Eating Disorders. 2006;39(1):11–19. doi: 10.1002/eat.20219. [DOI] [PubMed] [Google Scholar]
- 44.Feusner JD, Townsend J, Bystritsky A, Bookheimer S. Visual information processing of faces in body dysmorphic disorder. Arch Gen Psychiatry. 2007;64(12):1417–1425. doi: 10.1001/archpsyc.64.12.1417. [DOI] [PubMed] [Google Scholar]
- 45.Cohen J. Statistical power analysis for the behavioral sciences. 2nd. Hillsdale, N.J: L. Erlbaum Associates; 1988. [Google Scholar]
- 46. [Accessed on June 14, 2016];FAQ: How is effect size used in power analysis? http://wwwatsuclaedu/stat/mult_pkg/faq/general/effect_size_power/effect_size_powerhtm [serial on the Internet]
- 47.Beumont PJV, Kopecschrader EM, Talbot P, Touyz SW. Measuring the Specific Psychopathology of Eating Disorder Patients. Aust Nz J Psychiat. 1993;27(3):506–511. doi: 10.3109/00048679309075810. [DOI] [PubMed] [Google Scholar]
- 48.Roefs A, Jansen A, Moresi S, Willems P, van Grootel S, van der Borgh A. Looking good. BMI, attractiveness bias and visual attention. Appetite. 2008;51(3):552–555. doi: 10.1016/j.appet.2008.04.008. [DOI] [PubMed] [Google Scholar]
- 49.Bohon C, Hembacher E, Moller H, Moody TD, Feusner JD. Nonlinear relationships between anxiety and visual processing of own and others’ faces in body dysmorphic disorder. Psychiatry Research: Neuroimaging. 2012;204(2–3):132–139. doi: 10.1016/j.pscychresns.2012.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Buhlmann U, Wilhelm S, McNally R, Tuschen-Caffier B, Baer L, Jenike M. Interpretive biases for ambiguous information in body dysmorphic disorder. CNS Spectrums. 2002;7(6):435–443. doi: 10.1017/s1092852900017946. [DOI] [PubMed] [Google Scholar]
- 51.Jansen A, Nederkoorn C, Mulkens S. Selective visual attention for ugly and beautiful body parts in eating disorders. Behav Res Ther. 2005;43(2):183–196. doi: 10.1016/j.brat.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 52.Smeets E, Jansen A, Roefs A. Bias for the (un)attractive self: on the role of attention in causing body (dis)satisfaction. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 2011;30(3):360–367. doi: 10.1037/a0022095. [DOI] [PubMed] [Google Scholar]
- 53.Hewig J, Cooper S, Trippe RH, Hecht H, Straube T, Miltner WH. Drive for thinness and attention toward specific body parts in a nonclinical sample. Psychosomatic Medicine. 2008;70(6):729–736. doi: 10.1097/PSY.0b013e31817e41d3. [DOI] [PubMed] [Google Scholar]
- 54.Shafran R, Lee M, Cooper Z, Palmer RL, Fairburn CG. Attentional bias in eating disorders. The International journal of eating disorders. 2007;40(4):369–380. doi: 10.1002/eat.20375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kerwin L, Hovav S, Hellemann G, Feusner JD. Impairment in local and global processing and set-shifting in body dysmorphic disorder. Journal of psychiatric research. 2014;57:41–50. doi: 10.1016/j.jpsychires.2014.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Labuschagne I, Rossell SL, Dunai J, Castle DJ, Kyrios M. A comparison of executive function in Body Dysmorphic Disorder (BDD) and Obsessive-Compulsive Disorder (OCD) J Obsess-Compuls Rel. 2013;2(3):257–262. [Google Scholar]
- 57.Wu M, Brockmeyer T, Hartmann M, Skunde M, Herzog W, Friederich HC. Set-shifting ability across the spectrum of eating disorders and in overweight and obesity: a systematic review and meta-analysis. Psychological medicine. 2014;44(16):3365–3385. doi: 10.1017/S0033291714000294. [DOI] [PubMed] [Google Scholar]
- 58.Grocholewski A, Kliem S, Heinrichs N. Selective attention to imagined facial ugliness is specific to body dysmorphic disorder. Body image. 2012;9(2):261–269. doi: 10.1016/j.bodyim.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 59.Blechert J, Ansorge U, Tuschen-Caffier B. A body-related dot-probe task reveals distinct attentional patterns for bulimia nervosa and anorexia nervosa. Journal of abnormal psychology. 2010;119(3):575. doi: 10.1037/a0019531. [DOI] [PubMed] [Google Scholar]
- 60.Reichel VA, Schneider N, Grunewald B, Kienast T, Pfeiffer E, Lehmkuhl U, Korte A. “Glass fairies” and “bone children”: adolescents and young adults with anorexia nervosa show positive reactions towards extremely emaciated body pictures measured by the startle reflex paradigm. Psychophysiology. 2014;51(2):168–177. doi: 10.1111/psyp.12160. [DOI] [PubMed] [Google Scholar]
- 61.Wilhelm SPK, Steketee G. Cognitive-Behavioral Therapy for Body Dysmorphic Disorder: A Treatment Manual. New York: The Guilford Press; 2013. [Google Scholar]
- 62.Corning AF, Krumm AJ, Smitham LA. Differential social comparison processes in women with and without eating disorder symptoms. J Couns Psychol. 2006;53(3):338–349. [Google Scholar]
- 63.Buhlmann U, Teachman BA, Kathmann N. Evaluating implicit attractiveness beliefs in body dysmorphic disorder using the Go/No-go Association Task. J Behav Ther Exp Psychiatry. 2011;42(2):192–197. doi: 10.1016/j.jbtep.2010.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cserjesi R, Vermeulen N, Luminet O, Marechal C, Nef F, Simon Y, Lenard L. Explicit vs. implicit body image evaluation in restrictive anorexia nervosa. Psychiatry research. 2010;175(1–2):148–153. doi: 10.1016/j.psychres.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 65.De Voogd EL, Wiers RW, Prins PJ, Salemink E. Visual search attentional bias modification reduced social phobia in adolescents. J Behav Ther Exp Psychiatry. 2014;45(2):252–259. doi: 10.1016/j.jbtep.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 66.Wilhelm S, Phillips KA, Didie E, Buhlmann U, Greenberg JL, Fama JM, et al. Modular Cognitive-Behavioral Therapy for Body Dysmorphic Disorder: A Randomized Controlled Trial. Behav Ther. 2014;45(3):314–327. doi: 10.1016/j.beth.2013.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


