Abstract
Background
Breast and cervical cancers are significant causes of mortality and morbidity for Asian women, and poor English-speaking ability is a barrier to cancer prevention practices.
Materials and Methods
This project tested relationships among English-speaking ability and early detection practices regarding to breast and cervical cancer among female Chinese immigrants. A descriptive cross-sectional survey was used.
Results
175 female Chinese immigrants completed the survey in the breast cancer prevention section, and 35 of them also completed the cervical cancer prevention section. Some 63% of them had heard about the clinical breast exam (CBE), but only 54% had had a CBE. While 46% of the participants were aware of their need for a Pap smear, only 31% had heard about it and had undergone a pelvic exam.
Conclusions
English-speaking ability was strongly associated with immigrant women’s knowledge of female cancer early detection. Culturally and linguistic issues should be considered as the first step to access immigrant population in designing future education intervention.
Keywords: Chinese immigrants, women, communication, early detection, cancer
Introduction
Current U.S. immigrants maintain their own language, cultural heritage, and ethnic identity more strongly than did immigrants of the past (Han et al., 2011). For a variety of reasons, the set of risks for health problems affecting immigrants differs from those affecting non-immigrants (Chun, 2011). Breast and cervical cancers are especially significant causes of mortality and morbidity for Asian women, due in part to underutilization of screening practices (Chen, 2009).
Data that describe the specific healthcare needs and utilization patterns for the Chinese immigrant population are scarce, and most of the existing research includes Chinese immigrants only as one part of a larger Asian immigrant population. According to the 2004–2008 Surveillance, Epidemiology and End Results (SEER) Data (National Cancer Institute, 2011a), rates of invasive breast cancer (per 100,000 women) are lower in Asian American women than in women of other ethnicities; however, studies have found that breast cancer becomes a progressively greater health problem for successive generations of Asian women living in the United States (Aragones, 2009).
Caucasian women have a higher overall breast cancer incidence rate compared to Chinese women in the United States (86.5 per 100,000 vs. 54.0 per 100,000, respectively) (National Cancer Institute, 2011a); however, 5-year survival rates are lower for Chinese women (64%) than for Caucasian women (71%) (National Cancer Institute, 2011a). A higher rate of late-stage diagnosis resulting from cultural and institutional barriers also increases cancer mortality among Chinese women (Aragones et al., 2009). The incidence of breast cancer among Chinese women in the United States is substantially higher than that of Chinese women in Asia (Yu et al., 2010).
In the United States, health disparities exist by race and ethnicity, and this is reflected in cervical cancer rates (per 100,000) as follows: Hispanic 12.2, African American 10.0, Asian American 7.3, and White 8.0 (National Cancer Institute, 2011b). Comparing among women in southern California, one study reported that the rates of invasive cervical cancer in Chinese American and non-Latina White women were 12.3 and 7.2 per 100,000, respectively (Jackson et al., 2002). Other studies reported that only 68% of Asian women living in the United States had ever had a Pap smear (McCracken et al., 2007). Chinese immigrants in Canada present similar issues; the knowledge level of cervical cancer risk factors is low among Chinese Canadian women, particularly among those with less education and who receive their care from a male doctor (Hislop et al., 2004).
Health access indicators represent the ability to navigate the healthcare system, but immigrant populations need to be able to communicate with healthcare providers in order to get that access (Pourat et al., 2010). As a study reported, a low level of English-speaking ability is one of the key barriers to accessing healthcare in the immigrant population (Cheung, 2011). Immigrants who experience a language barrier are generally more stressed, which can lead to poorer health overall (Ding and Hargraves, 2009). Lack of English proficiency can affect both immigrants’ knowledge of available services and their ability to communicate with available healthcare providers, thus restricting healthcare access (Cheung et al., 2011).
Many studies that measure immigrants’ health-seeking behaviors have failed to measure either English-speaking ability or attitudes toward health status and care, even though a higher level of English-speaking ability might enable individuals to utilize the healthcare system more effectively (Lee-Lin et al., 2007). The present study examined relationships between English-speaking ability and breast and cervical cancer early detection practice among female Chinese immigrants in the New York metropolitan area.
Theoretical framework
The Health Belief Model (HBM) includes personal estimates of vulnerability and personal faith in the efficacy of the healthcare provided. Health-seeking behaviors include activities that are goal-directed, aim at reducing a perceived threat, and indicate that health is valued (Herrick and Brown, 1998). When applied to healthcare providers and to their clients—especially as regards cues to action, susceptibility and behavioral beliefs—the HBM examines differences between the two groups in terms of attributes and relative perceptions of health and illness. According to the HBM, women who believe that breast cancer is a serious condition and/or that they are susceptible to breast cancer are more likely to perform practices to detect breast cancer (breast self-exam, clinic breast exam, and mammogram) (Poss, 2001).
The Theory of Reasoned Action (TRA) indicates that intentions to perform an action are determined by attitudes toward the behavior and the social norm (Poss, 2001). The goal of the TRA is to predict and understand directly observable behaviors that are primarily under the control of the individual (Poss, 2001). For the current study, a revised theoretical model was used that combines the HBM and the TRA (Figure 1). Table 1 explains how the study variables correspond to the HBM and the TRA. The combined model guided the survey design and question development for the current study.
Figure 1.
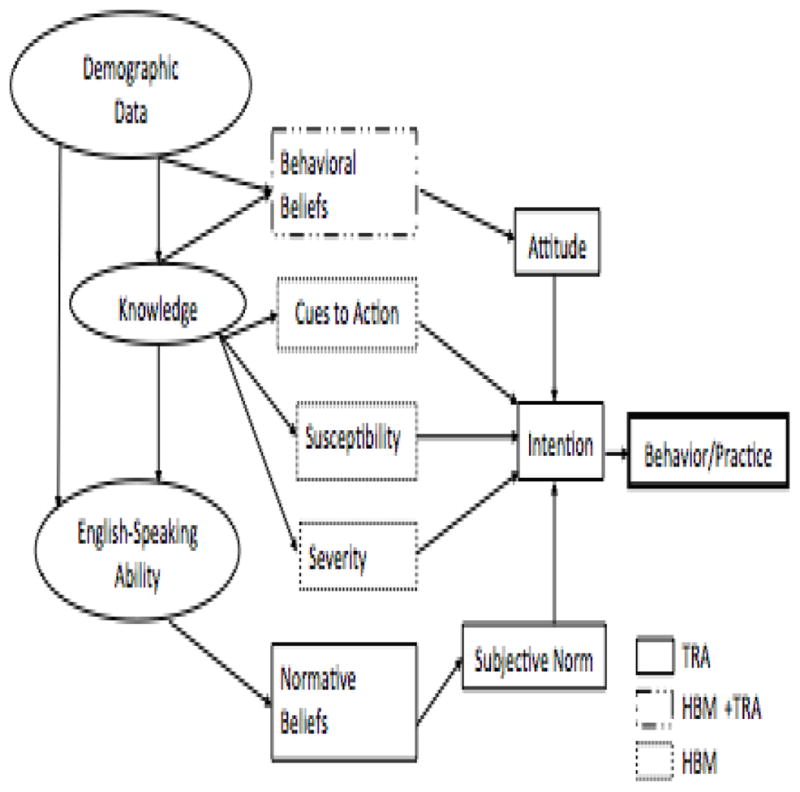
Combined Theoretical Model of HBM and TRA
Table 1.
Combined TRA and HBM Models with Study Variables
| Models | Study Variables |
|---|---|
| TRA | |
| Behavioral Beliefs | Traditional Chinese Health Beliefs and Practices |
| Normative Beliefs | General Cancer Beliefs |
| Attitude | Health Care Access |
| Intention | Concepts of General Cancer |
| Subjective Norm | General Health Practice |
| HBM | |
| Behavioral Beliefs | Traditional Chinese Health Beliefs and Practices |
| Cues to Action | English Speaking Ability, Knowledge of Breast and Cervical Cancer Risks |
| Susceptibility | History of Self and/or Family Members with Cancer diagnosis |
| Severity | Concept of Healthcare |
| Outcome Practices | Breast and Cervical Cancer Screening Practices |
TRA- Theory of Reasoned Action, HBM- Health Belief Model
Materials and Methods
Participants and data collection
Two hundred and ten Chinese women were approached at various community activities in the New York metropolitan area within a 6-month period. Of the 195 questionnaires distributed, 135 were returned, for return rate of 70%. Of the 135 returned surveys, 35 of the respondents completed the questions related to cervical cancer screening practices. (Due to the length of the questionnaires and time constraints for the study participants, the cervical cancer early detection surveys were made optional).
The study was a cross-sectional study that used paper-and-pencil self-administered Chinese-language questionnaires. To recruit and assess breast and cervical cancer prevention knowledge, beliefs, and behaviors among female Chinese immigrants, we approached 4 community events planners and asked them if we could set up a table to recruit immigrant women who might be interested in participating in a study. Most of the participants (N=78) were recruited from 3 childbirth classes, church (N=18) and temple (N=23) gathering events, and at a community center (N=10). The rest were recruited at local health fairs (N=6). To meet criteria for inclusion in the study, participants had to be female, of Chinese descent, literate in the Chinese language, and at least 18 years of age. A trained researcher approached potential participants before the start of childbirth class, and a private conference room was used for data collection. For those recruited at community activities, the researcher waited until they had finished the activity. After the researcher had explained the study in Chinese, distributed the information sheet to the study recruits, and secured permission from the participant, a private office was arranged inside the community center for participants to fill out the study survey. It took approximately 40 to 60 minutes for participants to answer the survey for the breast cancer early detection and another 40–60 minutes if they are willing to complete the cervical cancer early detection portion of the survey. After the surveys were completed, health education and cancer prevention booklets were given to participants. The proposal for the study was approved by the IRB at Columbia University Medical Center (CUMC).
Sample size
Based on a pilot data, a sample size of 100 study subjects will have 80% power with alpha at 0.05 to detect a small to median effect size (Cumulated R of 0.15 or higher) in the multiple regression analysis with 9 independent variables. Also with 100 study subjects there is at least 80% power with alpha at 0.05 to detect a 30% or higher correlation between scores of English-speaking ability and the beliefs and practices regarding to breast and cervical cancer prevention. In this study, one hundred and thirty-five completed surveys were returned regarding breast cancer prevention, however, only 35 of the study participants complete the cervical cancer prevention portion of the survey.
Measures
The Chinese-version survey instrument was adapted from the California Pathway study (Lee, 1996). It assesses the level of knowledge of cancer prevention among Chinese women. The survey contains 137 questions covering six subscales: demographics, acculturation, knowledge and access to medical care, attitudes toward healthcare and cancer, breast and cervical screening practices, and barriers to cancer screening practices (Lee et al., 1996). The scales’ reliabilities ranged from 0.54–0.96; for cervical cancer screening practice, the range was from 0.86 (Pap screening practices) to 0.96 (knowledge of cervical cancer risk). The study confirmed the reliability of the measurement of knowledge of breast and cervical risk factors in accordance with Cronbach’s α reliability scores of 0.94 (breast cancer) and 0.96 (cervical cancer). In order to adapt the survey for use by Chinese immigrants in the New York metropolitan area, we asked two Chinese-speaking bilingual researchers to proofread the survey instrument to ensure that there were be good comprehension.
Demographic data
Participants’ legal status and residential zip codes were added to the revised questionnaire used in the study. Legal status is a determinant factor in degree of assimilation into U.S. culture (Kim, 2005). A question about access to e-mail and telephone assessed participants’ ability to stay in touch with friends, relatives, and others in the United States and around the world. Questions about insurance, support system, length of stay in the United States, educational level, working hours, number of children, original country, religion, annual income were also included in the survey.
English-speaking ability
Five levels of English-speaking ability were used: none at all, poor (need assistance on most occasions), average (can communication on some occasions), good (can function in day-to-day living), and fluent (like a native). Acculturation factors (e.g., social skills, food preferences) were not included in the study analysis since this paper is focusing on the immigrants’ language ability and their early detection practices.
To ensure understanding of the study questions, the researcher described “mammogram” (in Chinese) as the “breast X-ray.” In addition to clarifying the medical terms used, visual aids were added to the questionnaire; for example, a graph was attached at the front of the BSE questions to help participants understand the term “breast self-exam.”
Concepts of healthcare
This section of the questionnaire was re-organized to present a logical sequence of questions. General questions concerning participants’ beliefs and practices about seeking healthcare were presented first. Questions related to routine check-up practices came second; questions concerning traditional Chinese health practices, third. The last group of questions was designed to afford insight into participants’ general attitudes toward cancer and access to healthcare (e.g., “Does the word ‘cancer’ scare you?”).
Breast cancer screening practice
The breast cancer screening instrument was adapted from the California Pathway study (Lee et al., 1996). with revisions made according to the American Cancer Society guidelines which recommend yearly mammograms for women, starting at age 40 and continuing for as long as a woman is in good health (American Cancer Society, 2011). To help participants understand the word “mammogram,” a picture of a mammographic X-ray was attached to the questionnaire.
Cervical cancer screening practice
According to the American Cancer Society’s suggested guidelines, all women should begin cervical cancer screening about 3 years after they start having vaginal intercourse. A woman should start screening at the age of 21. A regular Pap test should be done every three year if the results are normal and without any other risk (e.g., HIV-positive) (American Cancer Society, 2011). The survey questions related to cervical cancer screening were adapted from California Pathway study (Lee et al., 1996) with revisions mad according to the ACS guideline.
Data analysis
Analyses were conducted using Statistical Package of Social Science (SPSS) Version 17.0. Descriptive data analysis and logistic regression were used to determine the significant predictors of the level of the English-speaking ability regarding to beliefs and practices in cervical and breast cancer prevention.
Results
Ages ranged from 18–77 among the 135 study participants. Fewer than half (44%) of the study participants had completed high school. Many of the participants were currently working (55%) and the great majority (94%) were living in the metropolitan area of New York City, which includes the boroughs of Queens, Brooklyn, and Manhattan. The average stay in the U.S. for these participates was approximately 11 years; however, they had only stayed in the New York metropolitan area for an average of about 2 years. Most of them (74%) were married with one to two children. Of the 35 participants who completed the cervical cancer screening section of the surveys, 7 (20%) were age 40 or older, and a majority (60%) had public health insurance. Details of the demographic data for participants are presented in Table 2.
Table 2.
Demographic Data of Breast and Cervical Cancers Early Detection Survey
| Breast Cancer N=135 (%) |
Cervical Cancer N=35 (%) |
|
|---|---|---|
| Education (years) | ||
| <9 (up to secondary school) | 59 (44) | 15 (42.9) |
| >10 (post-secondary and up) | 76 (56) | 14 (40) |
| Age (years) Range from 18–77 years old | ||
| <39 | 55 (47) | 28 (80) |
| >40 | 61 (53) | 7 (20) |
| Employed Full- or Part-Time | 70 (55) | 9 (25.7) |
| Married/Live with Someone | 91 (74) | 27 (77.1) |
| Number of Children | ||
| None | 24 (21) | 21 (60) |
| One to three children | 91 (79) | 13 (37.2) |
| Religious Affiliation | ||
| Buddhist | 70 (56) | 13 (37.1) |
| Christian | 27 (21) | 4 (11.4) |
| Yearly Household Income | ||
| ≤$5,000 | 21 (14.2) | 11 (31.4) |
| $5,001–$30,000 | 44 (29.8) | 14 (40) |
| ≥$30,001 | 43 (29) | 3 (8.6) |
| Number of Persons Per Household | ||
| ≤2 | 31 (25) | 29 (82.9) |
| ≥3 | 91 (75) | 5 (14.3) |
| Health Insurance | ||
| No insurance | 36 (29) | 9 (25.7) |
| Public health insurance | 33 (26) | 21 (60) |
| Private health insurance | 53 (42) | 3 (8.6) |
| Ability to Speak English | ||
| Not at all | 32 (21.6) | 14 (40) |
| Poor | 31 (20.9) | 7 (20) |
| Average | 72 (48.7) | 14 (40) |
| Legal Status | ||
| No legal residency status | 29 (23) | 16 (45.7) |
| Legal resident | 85 (67) | 16 (45.7) |
Total N might not be 135 or 35 due to missing data
Approximately 54% (N=73) of the total participants had heard of the breast self-exam (BSE) but only 46% (N=34) of those who had heard of the BSE had practiced one. Sixty-three percent (N=85) of the participants had heard about the clinical breast exam (CBE), but only 54% (N=46) had had a CBE. Although 60% (N=81) of the women had heard about mammograms, a relatively small number (23%, N=19) of the participants who were over 40 years old had ever had a baseline mammogram. Approximately one third (29%, N=24) of the study participants expressed that they did not conduct these breast cancer detection screening activities because their doctor had not recommended them. Among the participants with mammogram experience, 86% (N=16) had had their mammogram during the 5 years prior to the study. Among those who completed the cervical cancer early detection survey, close to half (46%, N=16) were aware of the need for a Pap smear even for unmarried women; however, only 31% (N=11) had actually undergone a pelvic exam including a Pap smear.
None of the participants rated their English-speaking ability as “good” or “fluent.” Therefore, these two categories were excluded from the analysis. In the final calculation, only three levels of English-speaking ability (“none at all,” “poor,” and “average”) were used in the analysis. Of the women who assessed their English-speaking ability as average, 38% had heard of the clinical breast exam (CBE), compared with the women who judged their language abilities as either totally lacking (15%) or else poor (13%). Participants who had better English-speaking ability also believed that they should practice cervical cancer screening routinely (p<0.01), and had had a CBE (p<0.05) and Pap smear within a year of the survey (p<0.0001). There were significant differences related to English-speaking ability, breast exam practice and Pap smear tests. Detailed relationships among other subscales are presented in Table 3.
Table 3.
Beliefs and Practices vs. English-speaking Ability
| Not at all N (%) |
Poor N (%) |
Average N (%) |
Total N (%) |
χ2 | P | ||
|---|---|---|---|---|---|---|---|
| English-Speaking Ability | 14 (40) | 7 (20) | 14 (40) | 35 (100) | |||
| Beliefs | I need a Pap smear at my age | 3 (21.4) | 4 (57.1) | 9 (64.3) | 16 (45.7) | 21.11 | 0.00* |
| Women need a Pap smear even if not sexually active | 4 (28.6) | 2 (28.6) | 7 (50) | 13 (37.1) | 18.83 | 0.00* | |
| Women need a Pap smear even after menopause | 6 (42.9) | 4 (57.1) | 13 (92.9) | 23 (65.7) | 31.63 | 0.00* | |
| Women need a Pap smear even after hysterectomy | 4 (28.6) | 4 (57.1) | 7 (50) | 15 (42.9) | 15.17 | 0.00* | |
| Practices | Had a Clinical Breast Exam | 16 (19.3) | 18 (21.7) | 49 (59) | 83 (67.5) | 4.24 | 0.04* |
| Have examined own breasts | 12 (17.1) | 15 (21.4) | 43 (61.4) | 70 (53.8) | 5.07 | 0.08 | |
| Had a Pap smear | 4 (28.6) | 2 (28.6) | 7 (50) | 13 (37.1) | 17.37 | 0.00* | |
p≤0.05
Discussion
In this study, English-speaking ability, cancer-prevention beliefs, and health practice are highly associated. Without a high level of English-speaking ability, Chinese immigrants are less likely to practice screening for any of the preventable cancers. Therefore, English communication skills are one of the factors of early cancer detection practice. Clearly, with English language ability, women can communicate with the English-only healthcare providers more easily, and are more likely to practice cancer prevention. Studies have confirmed that Chinese immigrant women around the world have lower rates of cancer prevention practices (Cheung et al., 2011).
According to the HBM and TRA frameworks, acculturation influences immigrant women’s beliefs about when and why they need to practice breast and cervical cancer screening. In addition, English-speaking ability is one of the key elements of acculturation. Knowledge of breast and cervical cancer prevention in general will affect immigrant women’s behavioral beliefs, giving them a sense of whether they should seek out a clinic that provides these screening tests (Chen and Bakken, 2004). Basic cancer prevention knowledge can also give these women a sense as to whether they are at high risk of getting breast and/or cervical cancer (Lu et al., 2007). knowledge of breast and cervical cancer can establish the severity of these cancers in immigrant women’s minds, motivating them more strongly to seek out screening (Chen, 2009). Thus, to design interventions that targeting immigrant populations, we need to measure immigrants’ knowledge level on preventive screening tests, while evaluating the English-speaking ability of those women who are likely to rely solely on English-only health education materials and healthcare providers.
As regards beliefs on cervical cancer screening, this study has shown that immigrant Chinese women with a higher English-ability were aware that they should get Pap smears starting at the proper age and continuing even after menopause. And in fact, these participants did practice cervical cancer screening routinely, and had received CBE and Pap smears within a year of the survey. The study thus revealed that immigrant women with good English communication skills believed that cancer screening was a good preventive practice. Traditionally, Chinese people tend to attribute the cause of cancer to fate, broken promises to a god, or an imbalance between hot and cold elements (humors) in the body (Kwong et al., 2008). Researchers have reported that Chinese immigrants often hold to a traditional belief that seeking a preventive examination invites illness or that seeking treatment is an “admission” of illness, which can then bring stigma (Wong and Fielding, 2007).
Currently in the New York metropolitan area, there is no citywide campaign focusing on Chinese immigrant gynecological health screening and cancer prevention. One recent study showed that cancer screening rates in the Chinese immigrant population in New York City were largely dependent on healthcare provider recommendations; however, physicians serving the Chinese community in New York City follow cancer screening guidelines inadequately (Aragones et al., 2009). Therefore, cancer early detection screening could be improved by targeting healthcare providers as part of a larger effort to improve their awareness of guidelines and recommended best practices for immigrant health.
Women in this study presented varying degrees of inclination toward screening for early detection of breast and cervical cancer. Knowledge of breast and cervical cancer risks was generally limited, though, and experience with breast exams and Pap smears was not common. Gaining cultural and linguistic competence should be considered as the first step for clinicians who wish to access immigrant populations in designing future interventions. To design an effective health promotion program, healthcare providers should have a high degree of cultural competence, which is the key to successfully targeting immigrant populations for cancer screening practices (Woltman and Newbold, 2007). Meanwhile, enhanced understanding of the importance of preventive behaviors in the areas of breast and cervical cancer should be encouraged by healthcare providers.
Limitations, there were several limitations to this study. First, there were 137 questions in the complete paper-and-pencil survey, which was a total of 19 pages. In order to avoid imposing burden on the Chinese immigrant women taking the survey, the researcher gave them the choice of completing the whole survey, including both the breast and cervical cancer early detection questions, or completing only the breast cancer early detection part. Thus, many study participants chose to complete the first half of the questions addressing breast cancer prevention instead of completing all 19 pages. Only about a quarter (26%) of the study participants completed both sections of the survey. Therefore, the cervical cancer early detection survey could not detect the effect size of the Chinese immigrant women. Second, given small sample size and potential sample bias, especially on the cervical cancer early detection survey, the study should not be generalized to all female Chinese immigrants in the New York metropolitan area or elsewhere in the United States. However, it should be noted that this study does present results similar to those of other studies of Chinese and Asian populations indicating that immigrant women need to be targeted in cancer prevention campaigns (Goggins, 2009 #1397). Third, in the current study, English-speaking ability was the only factor used to assess participants’ acculturation level. Future studies should therefore assess other acculturation factors (e.g., social skills, food preferences) in order to understand how immigrants interact with the dominant society. Fifth and finally, future studies should focus on a larger Chinese female population to assess preferred health beliefs and health-seeking behaviors regarding cancer prevention. Use of a regression method to predict the behaviors in this population should be tested.
In conclusion, Chinese women continue to have the relatively low rate of conducting breast and cervical cancer screening practices (Yu et al., 2010), so there is an urgent need to encourage Chinese women, and especially immigrants, to obtain information and increase their awareness of public health services for breast and cervical cancer screening. The current low rate of screening is especially disconcerting because BSE, CBE, mammograms and Pap smears are inexpensive, effective tests that are widely covered by insurance plans. As the results of this study show, English-speaking ability significantly affects immigrant individuals’ health-seeking behaviors. The study also suggests that breast and cervical cancer healthcare interventions should be conducted in the native language of the population group being targeted for the intervention. When these interventions are targeted at immigrant groups, for example, Chinese American women, they must be easy to understand to encourage immigrants with limited English-speaking ability to seek for breast and cervical cancer screening.
Acknowledgments
The study was supported by Sigma Theta Tau International Alpha Zeta Chapter Research Grant Award, Foundation of New York State Nurses Association Center for Nursing Research, Rita C. Kopf Memorial Research Grant and University of Washington 2010 Institute for Ethnic Studies in the United States (IESUS).
References
- American Cancer Society. American Cancer Society Guidelines for the Early Detection of Cancer. 2011 Retrieved 5/17, 2011, from http://www.cancer.org/docroot/PED/content/PED_2_3X_ACS_Cancer_Detection_Guidelines_36.asp?sitearea=PED.
- Aragones A, Trinh-Shevrin C, Gany F. Cancer screening practices among physicians serving Chinese immigrants. J Health Care Poor Underserved. 2009;20:64–73. doi: 10.1353/hpu.0.0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen WT. Predictors of breast examination practices of Chinese immigrants. Cancer Nurs. 2009;32:64–72. doi: 10.1097/01.NCC.0000343366.21495.c1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen WT, Bakken S. Breast cancer knowledge assessment in female Chinese immigrants in New York. Cancer Nurs. 2004;27:407–12. doi: 10.1097/00002820-200409000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung NW, Li SCh, Tang KC. Participation in cardiovascular risk factor and cancer screening among Australian Chinese. Health Promot J Austr. 2011;22:147–52. doi: 10.1071/he11147. [DOI] [PubMed] [Google Scholar]
- Chun KM, Chesla CA, Kwan CM. “So We Adapt Step by Step”: Acculturation experiences affecting diabetes management and perceived health for Chinese American immigrants. Soc Sci Med. 2011;72:256–64. doi: 10.1016/j.socscimed.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding H, Hargraves L. Stress-associated poor health among adult immigrants with a language barrier in the United States. J Immigr Minor Health. 2009;11:446–52. doi: 10.1007/s10903-008-9200-0. [DOI] [PubMed] [Google Scholar]
- Goggins WB, Wong G. Cancer among Asian Indians/Pakistanis living in the United States: low incidence and generally above average survival. Cancer Causes Control. 2009;20:635–43. doi: 10.1007/s10552-008-9275-x. [DOI] [PubMed] [Google Scholar]
- Han HR, Kim J, Kim MT, et al. Measuring health literacy among immigrants with a phonetic primary language: a case of Korean American women. J Immigr Minor Health. 2011;13:253–9. doi: 10.1007/s10903-010-9366-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrick CA, Brown HN. Underutilization of mental health services by Asian-Americans residing in the United States. Issues in Mental Health Nurs. 1998;19:225–40. doi: 10.1080/016128498249042. [DOI] [PubMed] [Google Scholar]
- Hislop TG, Teh C, Lai A, et al. Pap screening and knowledge of risk factors for cervical cancer in Chinese women in British Columbia, Canada. Ethn Health. 2004;9:267–81. doi: 10.1080/1355785042000250102. [DOI] [PubMed] [Google Scholar]
- Jackson JC, Do H, Chitnarong K, et al. Development of cervical cancer control interventions for Chinese immigrants. J Immigr Health. 2002;4:147–57. doi: 10.1023/A:1015650901458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SH. Confucian bioethics and cross-cultural considerations in health care decision-making. J Nurs Law. 2005;10:161–6. doi: 10.1891/107374705780645529. [DOI] [PubMed] [Google Scholar]
- Kwong A, Cheung PS, Wong AY, et al. The acceptance and feasibility of breast cancer screening in the East. The Breast. 2008;17:42–50. doi: 10.1016/j.breast.2007.06.005. [DOI] [PubMed] [Google Scholar]
- Lee-Lin F, Pett M, Menon, et al. Cervical cancer beliefs and pap test screening practices among chinese american immigrants. Oncol Nur Forum. 2007;34:1203–9. doi: 10.1188/07.ONF.1203-1209. [DOI] [PubMed] [Google Scholar]
- Lee M. Pathways to early breast and cervical detection for Chinese American women. Hlth Edu Quarterly. 1996;23:76–88. [Google Scholar]
- Lu W, Cui Y, Zheng Y, et al. Impact of newly diagnosed breast cancer on quality of life among Chinese women. Breast Cancer Res Treat. 2007;102:201–10. doi: 10.1007/s10549-006-9318-5. [DOI] [PubMed] [Google Scholar]
- McCracken M, Olsen M, Chen, et al. Cancer incidence, mortality, and associated risk factors among Asian Americans of Chinese, Filipino, Vietnamese, Korean, and Japanese ethnicities. CA Cancer J Clin. 2007;57:190–205. doi: 10.3322/canjclin.57.4.190. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute. SEER Stat Fact Sheets: Breast. 2011a from http://seer.cancer.gov/statfacts/html/breast.html.
- National Cancer Institute. SEER Stat Fact Sheets: Cervix. 2011b from http://seer.cancer.gov/statfacts/html/cervix.html.
- Poss JE. Developing a new model for cross-cultural research: synthesizing the health belief model and the theory of reasoned action. Advance in Nur Sci. 2001;23:1–15. doi: 10.1097/00012272-200106000-00002. [DOI] [PubMed] [Google Scholar]
- Pourat N, Kagawa-Singer M, Breen N, et al. Access versus acculturation: identifying modifiable factors to promote cancer screening among Asian American women. Med Care. 2010;48:1088–96. doi: 10.1097/MLR.0b013e3181f53542. [DOI] [PubMed] [Google Scholar]
- Woltman KJ, Newbold KB. Immigrant women and cervical cancer screening uptake: a multilevel analysis. Can J Public Health. 2007;98:470–5. doi: 10.1007/BF03405441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong WS, Fielding R. Change in quality of life in Chinese women with breast cancer: changes in psychological distress as a predictor. Support Care Cancer. 2007;15:1223–30. doi: 10.1007/s00520-006-0190-y. [DOI] [PubMed] [Google Scholar]
- Yu TC, Chou CF, Johnson PJ, et al. Persistent disparities in pap test use: assessments and predictions for Asian women in the U.S., 1982–2010. J Immigr Minor Health. 2010;12:445–53. doi: 10.1007/s10903-009-9255-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


