Abstract
Recurrent and chronic rectal prolapse might lead to irreducibility and ultimately gangrene of the rectum if neglected. Gangrenous rectal prolapse is a surgical emergency and needs urgent surgical management. In view of irreducibility and gangrenous bowel, it is not advisable to attempt manual reduction of rectal prolapse. The only safe option that remains is perineal rectosigmoidectomy (Altemeier’s operation). Here, we present our experience of five such cases operated in our institute from 2000 to 2015 with available literature review.
Keywords: Perineal rectosigmoidectomy, Altemeier’s procedure, Gangrenous prolapse rectum, Emergency perineal rectosigmoidectomy
Introduction
Rectal prolapse is an uncommon condition. Recurrent attacks of prolapse and negligence in getting proper medical guidance lead to the progress of the condition. Gangrenous prolapse of the rectum is a surgical emergency requiring urgent intervention so as to get good end results [1]. Perineal rectosigmoidectomy (Altemeier’s operation) is the procedure of choice in this uncommon condition [2, 3].
Anatomy of Rectum
The rectum is 12 to 15 cm in length and lacks teniae coli or appendices epiploicae. It occupies the curve of the sacrum in the true pelvis, and the posterior surface is almost completely extraperitoneal. It is adherent to presacral tissues, thus the rectum is outside the peritoneal cavity. The anterior surface of the proximal third of the rectum is covered by the visceral peritoneum. The peritoneal reflection is 7 to 9 cm from the anal verge in men and 5 to 7.5 cm in women. This anterior peritonealized part is called pouch of Douglas or the pelvic cul-de-sac. The posterior aspect of the rectum is invested with a thick, closely applied mesorectum. A thin layer of investing fascia (fascia propria) coats the mesorectum and represents a distinct layer from the presacral fascia against which it lies. The lymphatics are contained within the mesorectum.
Rectal prolapse has been devided into three types [4]:
-
Type I.
Mucosal prolapse for about 1–3 cm associated with the prolapsed haemorrhoides
-
Type II.
It is essentially the intussusception of all the layers of the rectum and rectosigmoid through the rectum and anal canal without the associated cul-de-sac sliding hernia
-
Type III.
True or complete prolapse with cul-de-sac sliding hernia
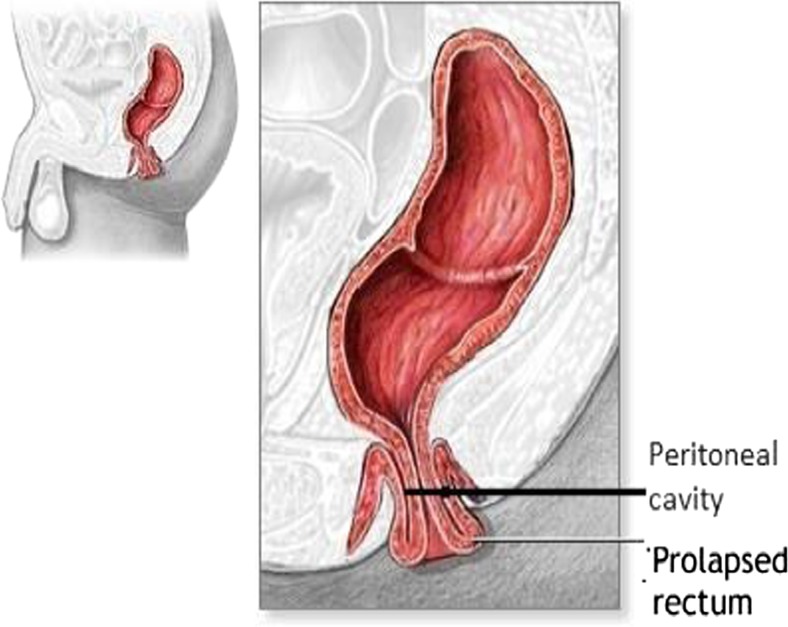
True or complete prolapse of the rectum is usually seen in extremes of life, in children, and in old persons. It is seen more commonly in females (Figs. 1 and 2).
Fig. 1.
True or complete prolapse of the rectum is usually seen in extremes of life, in children, and in old persons. It is seen more commonly in femalesᅟ
Fig. 2.
True or complete prolapse of the rectum
All the patients were treated at our institute presented in an emergency room. They had incarceration and strangulation with complete rectal prolapse. Complete evaluation and necessary investigations were carried out. Patients were started on broad-spectrum antibiotics and intravenous fluids. The procedure was discussed in detail with relatives, and all the complications were explained. Then, the patients underwent definitive surgery, which is Altemeier’s perineal rectosigmoidectomy.
Method and Operative Steps
Altemeier’s procedure of perineal rectosigmoidectomy was done in all the patients. All patients were under spinal anesthesia and were placed in the lithotomy position, and a Foley catheter was placed in situ. A local infiltration of adrenaline 1:100,000 was used. Full-thickness circumferential incision was made 1.5 cm proximal to the dentate line. The low peritoneal reflection can usually be incised anteriorly and peritoneal cavity entered. The mesentery of the rectum and sigmoid colon was sequentially clamped and ligated until no redundant bowel remained. The colon was divided at this point and an anastomosis established between the proximal sigmoid colon and the anal canal with interrupted sutures.
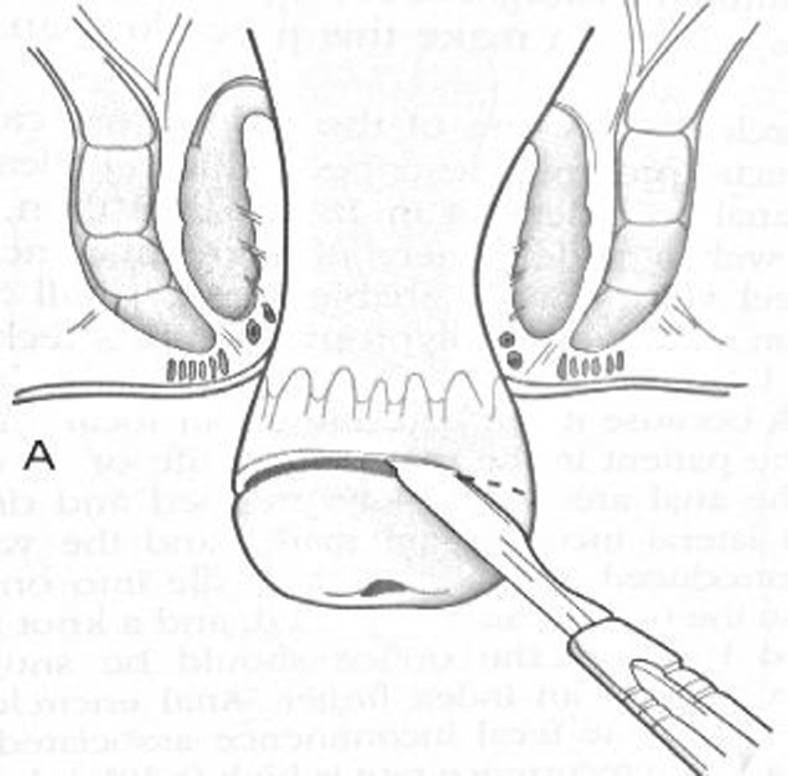
A full-thickness circumferential incision is made 1.5 cm proximal to the dentate line (Figs. 3 and 4).
The low peritoneal reflection was opened and the peritoneal cavity entered. A redundant loop of the sigmoid colon was visualized (Figs. 5 and 6).
The mesentery of the rectum and sigmoid colon was sequentially clamped, ligated, and divided (Figs. 7 and 8).
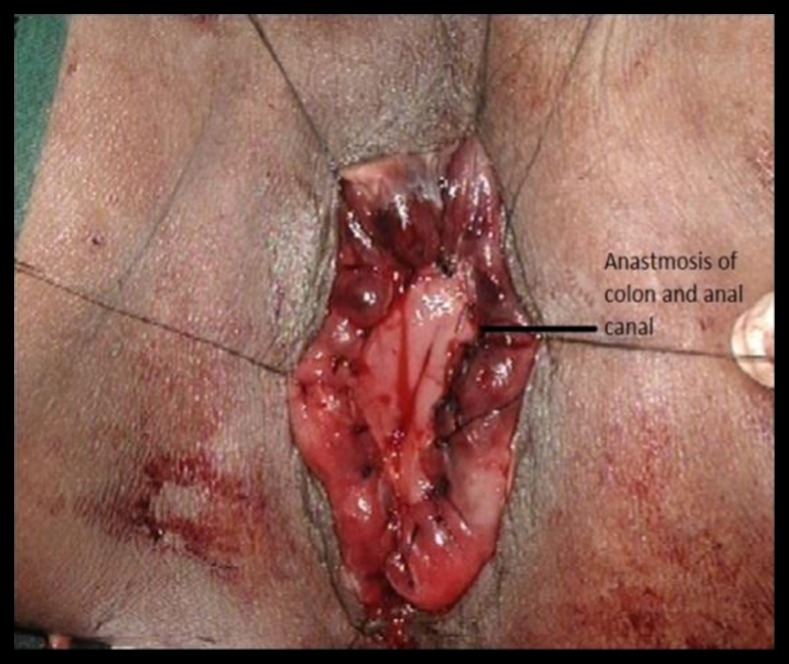
Colonic resection and anastomosis were performed between the colon and anal canal with sutures (Figs. 9 and 10).
Immediate postoperative anus (Fig. 11)
Fig. 3.
A full-thickness circumferential incision is made 1.5 cm proximal to the dentate line
Fig. 4.
A full-thickness circumferential incision
Fig. 5.
Low peritoneal reflection was opened and the peritoneal cavity entered
Fig. 6.
A redundant loop of the sigmoid colon was visualized
Fig. 7.
The mesentery of the rectum and sigmoid colon was sequentially clamped, ligated, and divided
Fig. 8.
The mesentery of the rectum and sigmoid colon
Fig. 9.
Colonic resection and anastomosis were performed between the colon and anal canal with sutures
Fig. 10.
Colonic resection and anastomosis between the colon and anal canal with sutures
Fig. 11.
Immediate postoperative anus
Discussion
Perineal rectosigmoidectomy was first introduced by Milkutz in 1899 and remained the favored treatment for prolapse in Europe for many years. Milkutz advocated this procedure in the UK, and it was promoted in the USA by Altemeier at the University of Cincinnati [4, 5].
Altemeier’s procedure combines perineal proctosigmoidectomy with levatorplasty [4]. The latter procedure is performed to correct the levator diastases commonly associated with this condition. Theoretically, restoration of fecal continence is enhanced by this additional maneuver.
The mortality rate from 0 to 5 and 0 to 16 % of recurrence is seen. The patients with incarcerated, strangulated, or gangrenous prolapsed rectal segment and even recurrence after the transabdominal approach are best treated with perineal rectosigmoidectomy. The abdominal approach is not suitable in these situations even in fit patients. There is an increased risk of impotence in males in the abdominal approach than in perineal.
Covering colostomy was done in two patients as bowel was found to be loaded with feces (Fig. 12).
Fig. 12.
Covering colostomy was done in two patients as bowel was found to be loaded with feces
In our series, hospital stay for patients with colostomy was longer (Fig. 13).
Fig. 13.
In our series, hospital stay for patients with colostomy was longer
All the patients had smooth recovery.
Even though recurrence rate after Altemeier’s procedure has been claimed to be more [4], in our series it was not observed.
Cases operated in our institute are shown in Table 1.
Table 1.
Cases operated in our institute
| Sr. no. | Age | Sex | Diagnosis | Procedure | Covering colostomy | Postoperative fecal incontinence |
|---|---|---|---|---|---|---|
| 1 | 52 | M | Gangrenous rectal prolapse | Perineal rectosigmoidectomy | Done | No |
| 2 | 58 | F | Gangrenous rectal prolapse | Perineal rectosigmoidectomy | Done | No |
| 3 | 65 | F | Gangrenous rectal prolapse | Perineal rectosigmoidectomy | Not done | No |
| 4 | 60 | M | Gangrenous rectal prolapse | Perineal rectosigmoidectomy | Not done | No |
| 5 | 65 | M | Gangrenous rectal prolapse | Perineal rectosigmoidectomy | Not done | No |
Impotence has been reported to be less common after Altemeier’s procedure [6].
Anastomotic leakage has been found to be very rare. [7].
Agachan et al. reported that addition of levatorplasty during Altemeier’s procedure leads to less chances of recurrence. [5] Altemeier’s operation involves removal of the rectal ampulla, with loss of its function as a fecal reservoir. For this reason, a full restoration of continence is rarely achieved, despite the significant improvement of the continence scores. [5] Combining dynamic graciloplasty with Altemeier’s procedure, it was found to give better control over fecal incontinence to liquids and solids as reported by Mongardini et al [8]. In our series of patients, the anal canal along with the sphincter complex was preserved, hence no additional procedure was necessary and patients had good continence.
In his iconic original article in 1971, Altemeier has mentioned that the correction of prolapse has relieved the patients of problem of soiling due to rectal discharge and disagreeable odor. [9].
Conclusion
Altemeier’s procedure, though rarely carried out, is a procedure of choice for gangrenous rectal prolapse in emergency. It can be carried out even under spinal anesthesia for frail and elderly patients. During the operation, both external and internal sphincters are saved, thus avoiding sphincter damage and issues related to incontinence.
Since this type of clinical situation is uncommon, many surgeons are not exposed to this operation during surgical training.
References
- 1.Abdelhedi C, Frikha F, Bardaa S, Kchaw A, Mzali R. Altemeier operation for gangrenous rectal prolapse. Afr J Surg. 2014;52(3):88. doi: 10.7196/sajs.1409. [DOI] [PubMed] [Google Scholar]
- 2.Nishimoria FHH, Akihiko SITY, Ishiyama NY. A simple and safe procedure to repair rectal prolapse perineally using stapling devices. Case Rep Gastroenterol. 2014;8:39–43. doi: 10.1159/000354970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Di Lena M, Angarano E, Giannini I, Guglielmi A, Donato FA. Strangulated ileal trans-coloanal-anastomotic hernia: a complication of Altemeier’s procedure previously never reported. World J Gastroenterol. 2013;19(5):776–777. doi: 10.3748/wjg.v19.i5.776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seenivasagam T, Gerald H, Ghassan N, Vivek T, Bedi AS, Suneet S. Irreducible rectal prolapse: emergency surgical management of eight cases and a review of the literature. Med J Malaysia. 2011;66(2):105–107. [PubMed] [Google Scholar]
- 5.Altomare DF, Binda G, Ganio E, De Nardi P, Giamundo P, Pescatori M, Rectal Prolapse Study Group (2009) Long-term outcome of Altemeier’s procedure for rectal prolapse. Dis Colon rectum 52:698Y703 [DOI] [PubMed]
- 6.Bhandari RS, Lakhey PJ. Altemeier rectosigmoidectomy for strangulated rectal prolapse. J Nepal Health Res Counc. 2011;9(19):189–191. [PubMed] [Google Scholar]
- 7.Yoon S-G. Rectal prolapse: review according to the personal experience. J Korean Soc Coloproctol. 2011;27(3):107–113. doi: 10.3393/jksc.2011.27.3.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mongardini M, Iachetta RP, Cola A, Effetti ED, Custureri F. Altemeier operation associated with dynamic graciloplasty: a case report. J Med Case Rep. 2009;3:9317. doi: 10.1186/1752-1947-3-9317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Altemeire WA, Culbertson WR, Schowengerdt C, Hunt J. Nineteen years’ experience with the one-stage perineal repair of rectal prolapse. Ann Surg. 1971;173(6):993–1001. doi: 10.1097/00000658-197106010-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]