Abstract
Gallstone ileus is a diagnosis of rarity, and a proximal site of obstruction in a young patient is even rare. Of the three cases in our experience, we found two cases of gallstone ileus (GSI) with typical epidemiology and presentation, one had combination of multiple rare associations. We report such a case, suspected to have gallstone ileus on ultrasound and confirmed diagnosis on computed tomography. Presence of biliary-enteric fistula, old age, and obstructive features, as in typical cases, was a bigger asset for diagnosis, but it was difficult to entertain diagnosis of GSI in young girl in absence of a demonstrable biliary-enteric fistula, with uncommon association of choledochal cyst and sickle cell disease. A very surprising finding, dilated major papilla, could however explain the pathogenesis which has also been reported in the past. Although differential opinions regarding management exist, we decided to follow two-stage surgery as our institute protocol. A minimal access approach has been immensely helpful in accurate diagnosis, and expedative management with early recovery has been proven in the past studies which we agreed with our experience.
Keywords: Gallstone ileus, Bilio-enteric fistula, Bouveret syndrome, Jejunal obstruction
Introduction
Gallstone ileus, actually a misnomer, is a well known but uncommon complication of gallstone disease. Though it carried high mortality in an initial period, with advent of improved treatment modalities, mortality has come down significantly. It has a very close association with bilio-enteric fistulization. Usually, it presents with recurrent episodes of “tumbling” obstruction culmination in frank obstruction, at sites from the stomach to the rectosigmoid colon. Due to its rarity and atypical presentation, a strong clinical suspicion is required to diagnose it, which is easily confirmed on radiological imaging like computed tomography. Selection of procedure, either one stage or two stage, can be decided depending upon the condition of the patient.
Case 1
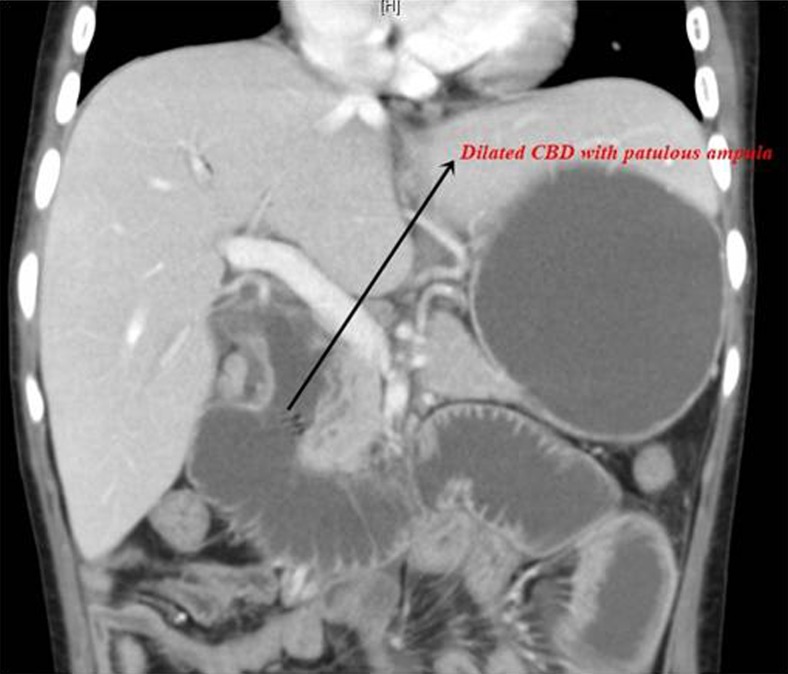
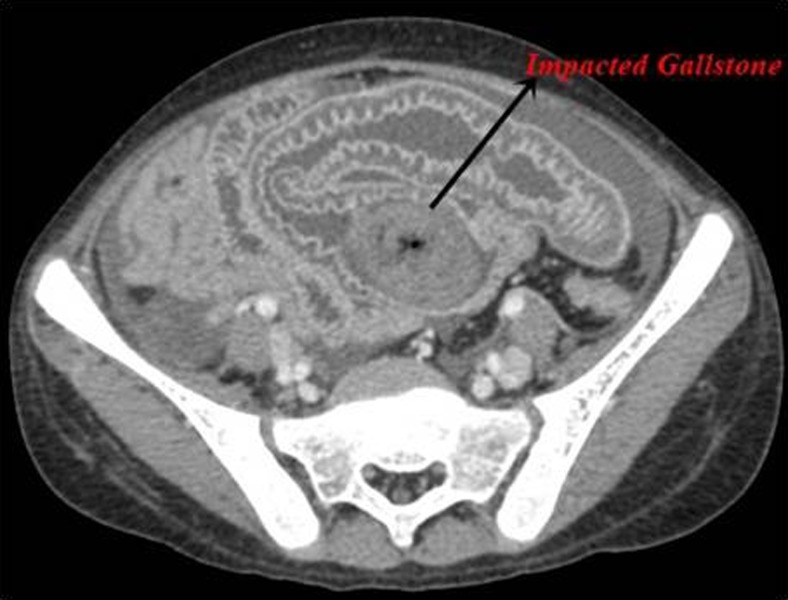
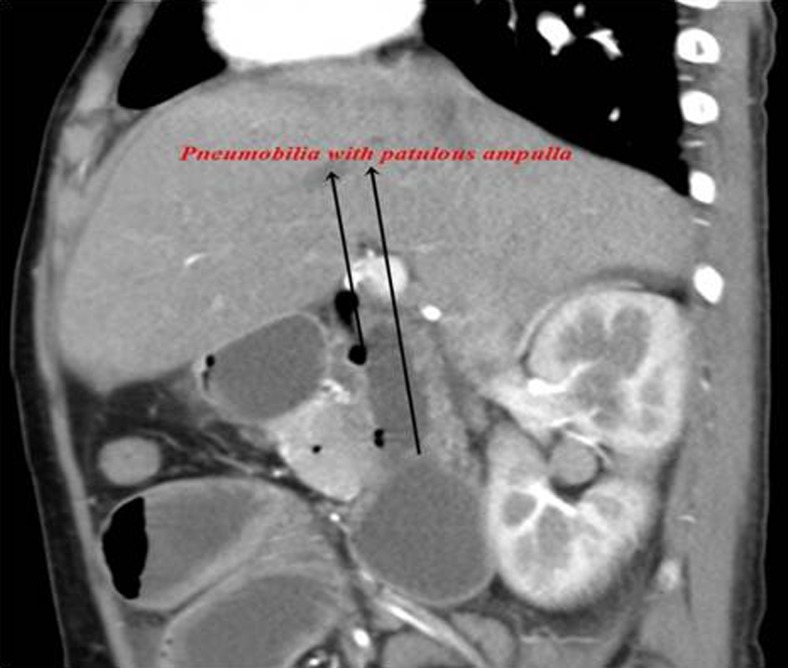
A 15-year-old girl with a known case of sickle cell disease and type I choledochal cyst diagnosed 5 years back presented with colicky umbilical region pain of 3-day duration associated with multiple bilious vomiting and with obstipation. She had history of hospitalization for cholangitis 10 days back which was managed conservatively without any intervention. On examination, she was febrile and icteric and had tachycardia. Per abdomen, she had right hypochondriac tenderness and hyperperistaltic bowel sounds. A hemogram showed leucocytosis and low hemoglobin, and a liver function test showed hyperbilirubinemia predominantly direct, with raised GGT and ALP with normal SGOT and SGPT. After admission, she was managed with IV fluids, IV antibiotics, and supportive management. On evaluation, her erect X-ray abdomen showed multiple air fluid levels. Ultrasonography of the abdomen showed a dilated proximal jejunum and duodenum with hypoechoic lesion intraluminally. Contrast-enhanced computed tomography abdomen was done which showed gallstone obstruction in the proximal jejunum, with a dilated fusiform common bile duct (CBD) measuring 34 mm with air pockets in it with patulous ampulla (Figs. 1, 2, and 3). She underwent laparoscopic exploration.
Fig. 1.
Choledochal cyst with patulous ampulla
Fig. 2.
Gallstone ileus CT
Fig. 3.
Pneumobilia with patulous ampulla
Intraoperatively, the proximal jejunum and duodenum were dilated with collapsed distal bowel loops with visible gallstone obstructing the proximal jejunum (Fig. 4). Enterotomy and extraction of the stone were done. Enterotomy was closed transversely. A postoperative course was uneventful. Ryle’s tube was removed on postoperative day (POD) 2, and she tolerated liquids from POD 2 and was discharged on POD 5.
Fig. 4.
Gallstone obstructing the proximal ileum
Case 2
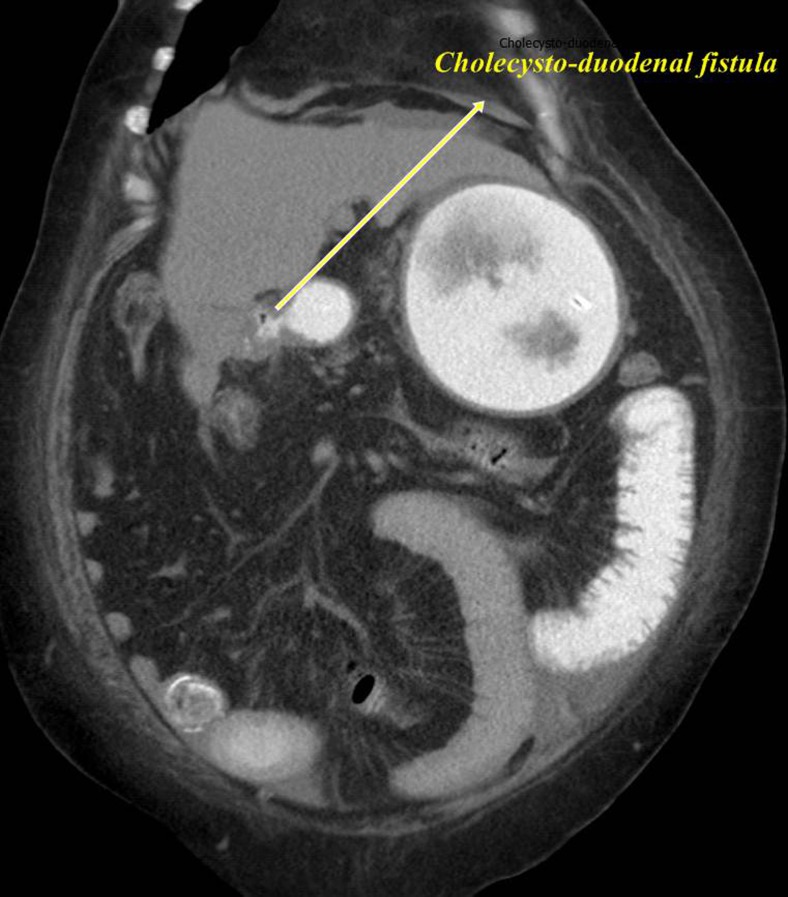
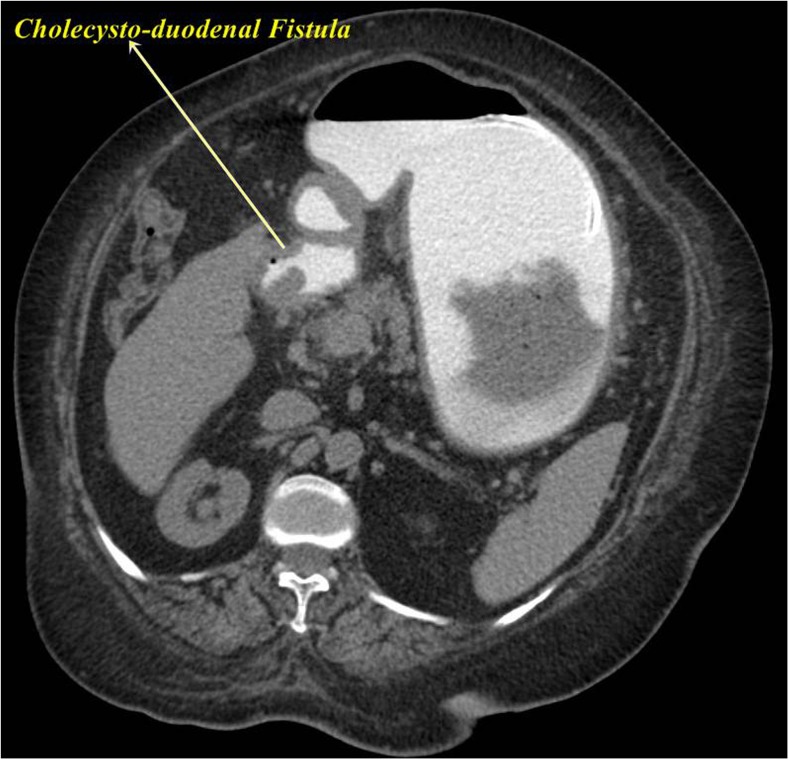
A 70-year-old diabetic hypertensive lady presented with diffuse abdominal pain with multiple bilious vomiting since 2 days associated with gradually increasing abdominal distension. She also had history of loose stools 1 week back which was managed conservatively on outpatient basis. She had recurrent episodes of colicky pain abdomen in last 3 years which was managed conservatively. On examination, she had abdominal distension associated with diffuse abdominal tenderness and presence of unbilical hernia. Laboratory investigations showed leukocytosis with hyponatremia and hypokalemia. Her serum creatinine was 2.1, and her liver function tests showed normal bilirubin and marginally elevated alkaline phosphatase (187 IU/L) and gamma glutamyl transferase (159 IU/L). Ultrasonography showed a contracted gallbladder with large calculus 15 mm in it with mild free fluid in the abdomen. She underwent plain CT whole abdomen with oral contrast which showed a contracted thick-walled gallbladder with evidence of cholecysto-duodenal fistula (Figs. 5 and 6). A 22-mm calculus was also noted in mid-ileum with proximal dilated bowel loops and distal collapsed bowel (Fig. 7).
Fig. 5.
Cholecysto-duodenal fistula coronal
Fig. 6.
Cholecysto-duodenal fistula (Axial)
Fig. 7.
Impacted gallstone
She underwent laparoscopic exploration. Calculus measuring 22 mm × 25 mm was noted in the distal ileum 80 cm proximal to ileocecal (IC) junction. Enterotomy and extraction of the stone were done which were closed transversely in two layers. Cholecysto-duodenal fistula was not operated considering the present poor general condition. Postoperatively, she had ileus which was managed conservatively and tolerated orals on POD 5 and was discharged on POD 8.
Case 3
A 79-year-old diabetic male presented with colicky pain in the periumbilical region associated with multiple bilious vomiting of 1-week duration. He had associated low-grade fever without chills. He gave history of hospitalization for subacute intestinal obstruction which was managed conservatively 2 years back. His physical examination showed dehydration with tachycardia and hypotension. His hematological investigations showed Hb of 9 g/dL, leukocytosis (19,870/cm3), and electrolyte disturbances. Ultrasonography showed a thick-walled contracted gallbladder with a prominent 7-mm CBD with dilated bowel loops. He underwent plain CT abdomen without contrast which showed a hyperdense intraluminal lesion in the distal ileum with proximal bowel dilatation. The thick-walled gallbladder was seen with multiple calculi and air foci in it. There was no evidence of intrahepatic biliary radical dilatation.
After resuscitation, he underwent laparoscopy-assisted exploration. A contracted gallbladder was seen adherent to the duodenum with dense adhesion in hepato-duodenal ligament. Impacted gallstone was found proximal to partial stricture in the proximal ileum 100 cm proximal to IC junction. Enterotomy, stone extraction, and subsequent stricturoplasty were done after taking biopsy from the stricture. Postoperatively, he had pulmonary complications which were managed conservatively. He recovered well and was discharged on POD 10.
Discussion
In our experience in the last 2 years, we came across three cases of gallstone ileus, of which the first case is peculiar in view of proximal jejunal gallstone obstruction in a young female without any evidence of biliary enteric fistula, in presence of a choledochal cyst while the other two are of a typical presentation. Very few cases of proximal jejuna gallstone ileus have been reported in literature [1]. And to our knowledge, only one case of gallstone ileus has been reported in choledochal cyst by Gaiani et al. [2]. Gallstone ileus (GSI), ideally a misnomer, first described in 1654 by Bartolin [3], is a rare cause of small-bowel obstruction with its incidence ranging from 0.5–5% [4–7]. The incidence starkly increases to 23–25% [8] for aged patients >65 years [9].
Epidemiology
A patient group is usually elderly females with age >70 years with multiple medical comorbidities amounting >70% [10, 11] of the total patient pool, but although uncommon, younger patients have also been reported [12]. The youngest patient reported was 13 years old [13]. GSI is more common in women, with the ratio of females to males being 3.5 to 1 [4, 5, 11], but some studies have shown male preponderance (69%) [14]. Our “case 1” was an unusually younger age of presentation at a relatively unusual site without any presence of bilio-enteric fistula with a rare association of choledochal cyst whereas other tows had more or less typical presentation.
Pathophysiology
The classic gallstone ileus is preceded by an acute cholecystitis episode. Inflammation and gallbladder bowel adhesions (usually at the level of the fundus of the gallbladder), associated with the ischemic effect and local pressure exerted by the gallstone, facilitates creation of a bilio-enteral fistula. A carcinoma gallbladder can also lead to fistulization to small intestine which perpetuates in passage of stones to end up into gallstone ileus [6, 15]. It occurs in approximately 0.06–0.5% of the patients with cholelithiasis [14, 16, 17] and about 15% patients with biliary-enteric fistula [18]. Although 80–90% [19] gallstones discharged into the bowel pass through the intestine, only about 6% result in gallstone ileus [20]. Cholecysto-duodenal fistula (60–92%) [21] is the most commonly associated biliary enteric fistula with gallstone ileus, but cholecysto-colonic, cholecysto-duodeno-colonic, cholecysto gastric, cholecysto-jejunal, and choledoco-duodenal fistula have also been reported. Sometimes, there may not be any evidence of fistula, but a patulous opening of ampulla of Vater which seems likely in our case 1; endoscopic sphincterotomy and hepaticojejunostomy have been reported as the causes for passage of stone into the small intestine. These stones may not be large enough to obstruct the bowel lumen initially but tend to grow in size or conglomerate to form large stone [16] and cause intermittent “tumbling obstruction” [22]. Obstructing stone ranges from 2–5 cm in size [23], while the largest stone was of 17.7 cm reported by Grey-Turner in 1932 [24].
Site of Obstruction
The most common site for the small intestinal obstruction is the physiologically or pathologically narrowed portions of the gastrointestinal tract like the distal ileum 60–65% followed by the jejunum (16.1%), stomach (14.2%), colon (0.5–4.1%), and duodenum 3.5–10% [4, 16, 25, 26]. Sigmoid colonic obstruction is also known in 2–8% cases [27, 28]. Less common sites like descending rectosigmoid colon are also reported [15, 29, 30]. Gallstone ileus has also been reported in a pathologically narrowed intestinal lumen secondary to Crohn’s disease [7, 31], colonic divericulitis [32], or postoperative ileostomy [33]. Although it has been observed as a de novo complication of long-standing gallstone disease, it has also been seen postoperatively even after cholecystectomy [20, 34], hepaticojejunostomy [11], choledocho-duodenostomy, or cholecysto-jejunal anastomosis in bilio-enteric bypass for morbid obesity as reported by Micheletto et al. [35]. The recurrent episodes of gallstone ileus can occur if the pathology is not treated at the first occasion [36–38].
In case 1 patient, none of these risk factors were present, but the presence of choledochal cyst could be a nidus for choledocholithiasis. Still, the question “where did the stone pass through?” was unanswered. This can be explained by a patulous ampulla or passage of small stone per ampulla and has grown in size in the enteral lumen. There are few of such cases reported [39]. However, in case 2, definite fistula was demonstrated preoperatively while suspicious biliary enteric fistula diagnosis was made in case 3 as we could demonstrate air foci in the gallbladder and intraoperatively adhered the duodenum to the gallbladder.
Clinical Presentation and Investigations
Patient presents with signs and symptoms of small-bowel obstruction, viz., nausea, vomiting, and abdominal distension with preceding episodes of diarrhea in background history of recurrent cholecystitis or biliary colic. There may be recurrent episodes of pain secondary to tumbling intermittent obstruction. Rarely, patients may present with jaundice [23]. Diagnosis of this condition requires high degree of suspicion and careful examination. Erect X-ray abdomen, which carries a sensitivity of 40–70% [6], usually shows Rigler’s triad, viz., pneumobilia present in approximately 17–36% [40], ectopic stone opacity in 8%, multiple air fluid levels in 97% [41], and sometimes Rigler’s tetrad adding shift of position of gallstone in serial examination [16]. Half of the patients show at least two of these signs [23] while only 7–33% of them show a typical Rigler’s triad [17, 42]. Since these findings are difficult to appreciate on plain X-ray, it carries a low sensitivity. Ultrasonography of the abdomen helps in detecting the gallstones, air in biliary tree, and gallbladder with occasionally delineation of the biliary enteric fistula. Computed tomography is more sensitive in delineating the biliary enteric fistula (air or dye in the gallbladder and biliary tree) and probable site of obstruction with more sensitivity, specificity, and diagnostic accuracy of 93, 100, and 99%, respectively [4, 43]. Magnetic resonance cholangio-pancreaticography has a minimal role in this condition just for delineating the biliary anatomy and fistulae.
Management
We managed obstruction by laparoscopic exploration. But in view of recent cholangitic episodes and electrolyte disturbances in the first case and poor general condition and electrolyte disturbances in other two cases, definitive surgery for biliary-enteric communications was deferred for a later date. Management solely depends upon performance status of the patient and the site of the obstruction. Just contrary to the saying “a sun should neither rise nor set over a mechanical acute obstruction”, it has shown spontaneous passage of gallstone in approximately 1.3% [4]. Stones impacted in a gastric outlet and those in the distal colon amendable to endoscopy can be managed by lithotripsy and endoscopic stone extraction [44, 45]. Even retrieval of small-bowel gallstone through a single- or double-balloon enteroscopy has also been tried successfully [46, 47]. Even cases treated by ESWL alone are also reported [48]. Relieving the obstruction and taking down the fistula can be done in a single setting provided that general condition of patient can withstand the duration of anesthesia and surgery. But in high-risk patients, just relieving the obstruction may be done, leaving the fistula repair for a later date [49]. Fistula may not be repaired in elderly if no residual stones are present. Enterotomy and stone extraction alone have been a safe approach and shown better results than the other procedures [10], letting the patient to earn the next procedure depending upon his recovery and clinical status, since >50% of the fistulas heal spontaneously provided that there is no distal obstruction [4] leaving a small but significant risk (5–9%) for recurrence as stated by Reisner et al. [27]. But enterotomy with taking down fistula had lower rates of postoperative development of recurrence and gallbladder malignancy in some studies [11] weighing against increased mortality [6]. Adding a minimally invasive approach has a cutting edge in selected patients in terms of faster recovery and excellent outcome [50].
In the presence of residual stones, the estimated prevalence of recurrence ranged from 5 to 17% [4] which is common in the first 6 months [19, 27]. In a hospital, mortality of 5–27% [6, 8, 10, 14] and morbidity of 35.4% were reported [49] owing to the elderly morbid population affected and delayed in the diagnosis. But the mortality is steadily decreasing from as high as 60% reported in early twentieth century to as low as zero mortality in some series, with advent of good medical and surgical care [26]. Bowel resection alone had shown the highest complication rate, and the most common among the morbidities are acute renal failure approximately 30%, surgical site infection, and urinary tract infection [10, 49]. Other complications in a postoperative period have also been reported when bilio-enteric fistula was not addressed like cholecystitis, choangitis, recurrent obstruction, fistulous bleeding, fat malabsorption, and gallbladder carcinoma (15%) [23].
Conclusion
Rare diagnosis like gallstone ileus needs a great degree of suspicion since many atypical presentations exist. The treatment plan needs to be individualized as per patient’s general condition and clinical presentation. The laparoscopic approach is safe, feasible, and rewarding with early postoperative recovery.
Compliance with Ethical Standards
Disclosure
The corresponding author is not a recipient of research fellowship.
The paper is not based on a previous communication to any society or meeting.
This case report was presented as a free poster in IASG 2015 held in Pune.
Conflict of Interest
The authors declare that they have no conflict of interest.
Footnotes
Method
The review is prepared by searching the following terms in Google scholar, Pubmed, and Pubmed central and exploring the related articles popped on the side of a page. The terms were gallstone ileus, bilio-enteric fistula, Bouveret syndrome, jejunal obstruction.
References
- 1.Spaziani E, Picchio M, Di Filippo A, De Angelis F, Marino G, Stagnitti F. Gallstone ileus. Report of two cases. Ann Ital Chir. 2010;81(1):53–55. [PubMed] [Google Scholar]
- 2.Gaiani S, Serra C, Cervellera M, Campione O, Bolondi L, Miglioli M. Gallstone ileus in Caroli’s disease. Am J Gastroenterol. 2000;95(12):3642–3643. doi: 10.1111/j.1572-0241.2000.03303.x. [DOI] [PubMed] [Google Scholar]
- 3.Gupta M, Goyal SLS, Singal R, Goyal R, Goyal SLS, Mittal A. Gallstone ileus and jejunal perforation along with gangrenous bowel in a young patient: a case report. N Am J Med Sci. 2010;2(9):442–443. doi: 10.4297/najms.2010.2442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dai X-Z, Li G-Q, Zhang F, Wang X-H, Zhang C-Y. Gallstone ileus: case report and literature review. World J Gastroenterol. 2013;19(33):5586–5589. doi: 10.3748/wjg.v19.i33.5586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chou J-W, Hsu C-H, Liao K-F, Lai H-C, Cheng K-S, Peng C-Y, et al. Gallstone ileus: report of two cases and review of the literature. World J Gastroenterol. 2007;13(8):1295–1298. doi: 10.3748/wjg.v13.i8.1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tucker A, Garstin I (2013) A peculiar cause of bowel obstruction. Int J Surg Case Rep 4(5):473–476 [DOI] [PMC free article] [PubMed]
- 7.Toelen C, Huyghe M. Gallstone ileus in a patient with Crohn’s disease: a case report. Acta Chir Belg. 2012;112(5):390–392. doi: 10.1080/00015458.2012.11680859. [DOI] [PubMed] [Google Scholar]
- 8.Reports C, Giese A, Zieren J, Winnekendonk G, Henning BF. Development of a duodenal gallstone ileus with gastric outlet obstruction (Bouveret syndrome) four months after successful treatment of symptomatic gallstone disease with cholecystitis and cholangitis: a case report. J Med Case Rep. 2010;4(1):376. doi: 10.1186/1752-1947-4-376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Casella R, Müller W. Gallstone ileus—still a current disease. Schweiz Rundsch Med Prax. 1992;81(20):654–660. [PubMed] [Google Scholar]
- 10.Halabi WJ, Kang CY, Ketana N, Lafaro KJ, Nguyen VQ, Stamos MJ, et al. Surgery for gallstone ileus: a nationwide comparison of trends and outcomes. Ann Surg. 2014;259(2):329–335. doi: 10.1097/SLA.0b013e31827eefed. [DOI] [PubMed] [Google Scholar]
- 11.He J, Xu K, Tang J. Intestinal obstruction caused by gallstone: report of 5 cases and review of the literature. Zhonghua Wei Chang Wai Ke Za Zhi. 2010;13(10):751–754. [PubMed] [Google Scholar]
- 12.Chatterjee S, Chaudhuri T, Ghosh G, Ganguly A. Gallstone ileus—an atypical presentation and unusual location. Int J Surg. 2008;6(6):e55–e56. doi: 10.1016/j.ijsu.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 13.Cooperman AM, Dickson ER, ReMine WH (1968) Changing concepts in the surgical treatment of gallstone ileus: a review of 15 cases with emphasis on diagnosis and treatment. Ann Surg 167(3):377–383 [DOI] [PMC free article] [PubMed]
- 14.Rojas-Rojas DJA, Martínez-Ordaz JL, Romero-Hernández T. Biliary ileus: 10-year experience. Case series. Cir Cir. 2012;80(3):228–232. [PubMed] [Google Scholar]
- 15.Vaughan-Shaw PG, Talwar A (2013) Gallstone ileus and fatal gallstone coleus: the importance of the second stone. BMJ Case Rep. doi:10.1136/bcr-2012-008008 [DOI] [PMC free article] [PubMed]
- 16.Beuran M, Ivanov I, Venter MD. Gallstone ileus—clinical and therapeutic aspects. J Med Life. 2010;3(4):365–371. [PMC free article] [PubMed] [Google Scholar]
- 17.Chang CW, Shih SC, Lin SC, Chu CH, Wang TE, Chang WH. Gallstone ileus: a disease easily ignored in the elderly. Int J Gerontol. 2008;2(1):18–21. doi: 10.1016/S1873-9598(08)70004-8. [DOI] [Google Scholar]
- 18.Jian-song JI, Si-zheng Z, Chu-xiao S, Zhong-wei Z, Zu-fei W, Gui-jian LÜ, et al. (2014) Imaging diagnosis of two unusual forms of gallstone ileus. (10):29–31. [PubMed]
- 19.Martín-Pérez J, Delgado-Plasencia L, Bravo-Gutiérrez A, Burillo-Putze G, Martínez-Riera A, Alarcó-Hernández A, et al. Gallstone ileus as a cause of acute abdomen. Importance of early diagnosis for surgical treatment. Cirugía española. 2013;91(8):485–489. doi: 10.1016/j.ciresp.2013.01.021. [DOI] [PubMed] [Google Scholar]
- 20.Zens T, Liebl RS (2010) Gallstone ileus 30 years status postcholecystectomy. 109(6):332–335 [PubMed]
- 21.Mondragón Sánchez A, Berrones Stringel G, Tort Martínez A, Soberanes Fernández C, Domínguez Camacho L, Mondragón SR. Surgical management of gallstone ileus: fourteen year experience. Rev Gastroenterol México. 2005;70(1):44–49. [PubMed] [Google Scholar]
- 22.Anseline P. Colonic gall-stone ileus. Postgrad Med J. 1981;57(663):62–65. doi: 10.1136/pgmj.57.663.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Szajnbock I, Lorenzi F, Rodrigues Júnior a J, Zantut LF, Poggetti RS, Steinman E, et al. Gallstone ileus as a cause of upper intestinal obstruction. Sao Paulo Med J 1996;114(4):1239–1243. [DOI] [PubMed]
- 24.Turner GGA. Giant gall-stone impacted in the colon and causing acute obstruction. Br J Surg. 1932;20(77):26–33. doi: 10.1002/bjs.1800207704. [DOI] [Google Scholar]
- 25.Langhorst J, Schumacher B, Deselaers T, Neuhaus H. Successful endoscopic therapy of a gastric outlet obstruction due to a gallstone with intracorporeal laser lithotripsy: a case of Bouveret’s syndrome. Gastrointest Endosc. 2000;51(2):209–213. doi: 10.1016/S0016-5107(00)70421-4. [DOI] [PubMed] [Google Scholar]
- 26.Ozbalci GS, Tanrikulu Y, Kismet K, Dinc S, Akkus MA (2012) Gallstone ileus with a giant stone and associated multiple stones. Bratisl Lek Listy 113(8):503–505 [DOI] [PubMed]
- 27.Reisner RM, Cohen JR. Gallstone ileus: a review of 1001 reported cases. Am Surg. 1994;60(6):441–446. [PubMed] [Google Scholar]
- 28.Swinnen L, Sainte T. Colonic gallstone ileus. J Belg Radiol. 1994;77(6):272–274. [PubMed] [Google Scholar]
- 29.Donati M, Cardì F, Brancato G, Calò P, Donati A. The surgical treatment of a rare complication: gallstone ileus. Ann Ital Chir. 2010;81(1):57–62. [PubMed] [Google Scholar]
- 30.Ball WR, Elshaieb M, Hershman MJ (2013) Rectosigmoid gallstone coleus: a rare emergency presentation. BMJ Case Rep. doi:10.1136/bcr-2013-201136 [DOI] [PMC free article] [PubMed]
- 31.Toelen C, Huyghe M. (2012) Gallstone Ileus in a patient with crohn’s disease: a case report. Acta Chir Belg 112(5):390–392 [DOI] [PubMed]
- 32.Sun R, Theilmann L, Vöhringer U, Abdel Samie A. Gallstone ileus in underlying stenosis of the sigmoid due to recurrent diverticulitis—a rare complication of cholelithiasis. Med Klin (Munich) 2010;105(6):433–436. doi: 10.1007/s00063-010-1074-y. [DOI] [PubMed] [Google Scholar]
- 33.Ayeni I V, Williams NJ (2012) An unusual cause of a non-functioning stoma in an 87-year-old gentleman. BMJ Case Rep. doi:10.1136/bcr-03-2012-6008 [DOI] [PMC free article] [PubMed]
- 34.Ivanov I, Beuran M, Venter MD, Iftimie-Nastase I, Smarandache R, Popescu B, et al. Gallstone ileus after laparoscopic cholecystectomy. J Med Life. 2012;5(3):335–341. [PMC free article] [PubMed] [Google Scholar]
- 35.Micheletto G, Danelli P, Morandi A, Panizzo V, Montorsi M. Gallstone ileus after biliointestinal bypass: report of two cases. J Gastrointest Surg. 2013;17(12):2162–2165. doi: 10.1007/s11605-013-2290-6. [DOI] [PubMed] [Google Scholar]
- 36.Aslam J, Patel P, Odogwu S (2014) A case of recurrent gallstone ileus: the fate of the residual gallstone remains unknown. BMJ Case Rep. doi:10.1136/bcr-2013-203345 [DOI] [PMC free article] [PubMed]
- 37.Gandamihardja TAK, Kibria SMG (2014) Recurrent gallstone ileus: beware of the faceted stone. BMJ Case Rep. doi:10.1136/bcr-2014-205795. [DOI] [PMC free article] [PubMed]
- 38.Webb LH, Ott MM, Gunter OL. Once bitten, twice incised: recurrent gallstone ileus. Am J Surg. 2010;200(6):e72–e74. doi: 10.1016/j.amjsurg.2010.02.025. [DOI] [PubMed] [Google Scholar]
- 39.Armitage G, Fowweather FS, Johnstone AS. Observations on bile-acid enteroliths with an account of a recent case. Br J Surg. 1950;38(149):21–25. doi: 10.1002/bjs.18003814906. [DOI] [PubMed] [Google Scholar]
- 40.Freitag M, Elsner I, Günl U, Albert W, Ludwig K. Clinical and imaging aspects of gallstone ileus. Experiences with 108 individual observations. Chirurg. 1998;69(3):265–269. doi: 10.1007/s001040050410. [DOI] [PubMed] [Google Scholar]
- 41.Hildebrandt J, Herrmann U, Diettrich H. Gallstone ileus. A report of 104 cases. Chirurg. 1990;61(5):392–395. [PubMed] [Google Scholar]
- 42.Halleran DR, Halleran DR (2014) Colonic perforation by a large gallstone: a rare case report. Int J Surg Case Rep 5(12):1295–1298 [DOI] [PMC free article] [PubMed]
- 43.C-Y Y, Lin C-C, Shyu R-Y, Hsieh C-B, H-S W, Tyan Y-S, et al. Value of CT in the diagnosis and management of gallstone ileus. World J Gastroenterol. 2005;11(14):2142–2147. doi: 10.3748/wjg.v11.i14.2142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhao J, Barrera E, Salabat M, Denham W, Leung D, Ujiki M. Endoscopic treatment for Bouveret syndrome. Surg Endosc. 2013;27(2):655. doi: 10.1007/s00464-012-2533-8. [DOI] [PubMed] [Google Scholar]
- 45.Shin KH, Kim DU, Choi MG, Kim WJ, Ryu DY, Lee BE, et al. A case of gallstone ileus treated with electrohydraulic lithotripsy guided by colonoscopy. Korean J Gastroenterol. 2011;57(2):125–128. doi: 10.4166/kjg.2011.57.2.125. [DOI] [PubMed] [Google Scholar]
- 46.Heinzow HS, Meister T, Wessling J, Domschke W, Ullerich H (2010) Ileal gallstone obstruction: single-balloon enteroscopic removal. 2(9):321–324 [DOI] [PMC free article] [PubMed]
- 47.Kim YG, Byeon J-S, Lee SK, Yang D-H, Kim K-J, Ye BD, et al. Gallstone ileus successfully treated with endoscopic fragmentation by using double-balloon endoscopy (with video) Gastrointest Endosc. 2011;74(1):228–230. doi: 10.1016/j.gie.2010.12.018. [DOI] [PubMed] [Google Scholar]
- 48.Muratori R, Cennamo V, Menna M, Cecinato P, Eusebi LH, Mazzella G, et al. Colonic gallstone ileus treated with radiologically guided extracorporeal shock wave lithotripsy followed by endoscopic extraction. Endoscopy. 2012;44(Suppl 2):E88–E89. doi: 10.1055/s-0031-1291641. [DOI] [PubMed] [Google Scholar]
- 49.Mallipeddi MK, Pappas TN, Shapiro ML, Scarborough JE. Gallstone ileus: revisiting surgical outcomes using National Surgical Quality Improvement Program data. J Surg Res. 2013;184(1):84–88. doi: 10.1016/j.jss.2013.05.027. [DOI] [PubMed] [Google Scholar]
- 50.Lujan HJ, Bisland WB. Two-stage minimally invasive surgical management of colonic gallstone ileus. Surg Laparosc Endosc Percutan Tech. 2010;20(4):269–272. doi: 10.1097/SLE.0b013e3181e1abb7. [DOI] [PubMed] [Google Scholar]