Abstract
Child abuse is a global problem, and parents with histories of childhood abuse are at increased risk of abusing their offspring. The objective of this systematic review is to provide a clear overview of the existing literature of randomized controlled trials evaluating the effectiveness of interventions to prevent child abuse. PubMed, PsychINFO, Web of Science, Sociological Abstracts, and CINAHL were systematically searched and expanded by hand search. This review includes all randomized controlled trials (RCTs) of interventions designed to prevent abuse among mothers identified as high-risk. Of the eight studies identified, only three found statistically significant reductions in abuse by any measure, and only two found reductions in incidents reported to child protective services. While much has been written about child abuse in high-risk families, few RCTs have been performed. Only home visitation has a significant evidence base for reducing child abuse, and the findings vary considerably. Also, data from low- and middle-income countries are limited.
Keywords: Systematic review, randomized controlled trial, child maltreatment, abuse, neglect, intergenerational transmission
Introduction
Child abuse, including both physical and sexual abuse, is a global problem. The prevalence of child physical abuse alone has been estimated at 22.6% worldwide (Stoltenborgh, Bakermans-Kranenburg, van Ijzendoorn, & Alink, 2013). Children who experience abuse are more likely to have physical and mental health problems in adulthood, including chronic inflammation (Bertone-Johnson, Whitcomb, Missmer, Karlson, & Rich-Edwards, 2012; Danese et al., 2009), asthma (Coogan et al., 2013), substance abuse (Banducci, Hoffman, Lejuez, & Koenen, 2014), depression (Chapman et al., 2004), suicidal behavior (Dube et al., 2001) and post-traumatic stress disorder (Frans, Rimmo, Aberg, & Fredrikson, 2005). Victims of childhood abuse are also at risk for re-victimization as adults, when they go on to experience high rates of intimate partner violence (Bensley, Van Eenwyk, & Wynkoop Simmons, 2003; Coid et al., 2001; Schaaf & McCanne, 1998), and their offspring are at increased risk for being abused (Berlin, Appleyard, & Dodge, 2011; Lee, 2009; Madigan et al., 2014; Milan, Lewis, Ethier, Kershaw, & Ickovics, 2004; Plant, Barker, Waters, Pawlby, & Pariante, 2013). For this reason, interventions with high-risk families are needed to prevent abuse of the next generation.
Interventions designed to interrupt this cycle have been developed to provide support and education to pregnant women and mothers of infants who are at risk for parenting difficulties. This both bridges a knowledge gap (Avellar & Supplee, 2013; Olds, Henderson, Chamberlin, & Tatelbaum, 1986; Olds et al., 2004; Olds, Sadler, & Kitzman, 2007) and provides new mothers with experiences of nurturing and care that many of them did not have in their own childhoods (Fraiberg, Adelson, & Shapiro, 1975). Home visiting interventions are the most widely used parenting interventions in the US, and their global popularity is growing (Alonso-Marsden et al., 2013; Astuto & Allen, 2009; Casillas, Fauchier, Derkash, & Garrido, 2016; Knerr, Gardner, & Cluver, 2013). Originally developed to improve medical outcomes in premature infants, home visiting has also been used to treat post-partum depression, improve parent-infant connectedness, decrease child abuse and improve child developmental outcomes (Avellar & Supplee, 2013; Olds et al., 2007). Other intervention types, including groups, have been tried but have not been widely adopted because participation rates have been low (Elliott, Sanjack, & Leverton, 1988; Stamp, Williams, & Crowther, 1995).
A recent meta-analysis assessed 156 home visiting interventions with a variety of study designs (Casillas et al., 2016). The study found that interventions targeting specific high-risk groups had greater effect sizes than those that targeted a general population. Implementation factors, including the training and supervision of those delivering the intervention, also impacted effect size. However, it was not clear which implementation factors were important for preventing abuse among which groups.
The objective of this report is to systematically review existing literature of randomized controlled trials evaluating the efficacy of interventions to prevent child abuse beginning at birth by mothers identified as high-risk based on financial factors, age, abuse history, mental illness, substance abuse or life stress. While the risk factors associated with child abuse are highly comorbid, some studies have found that particular sub-populations are more responsive to interventions, which has led to efforts to tailor interventions to specific groups. This report will seek to determine the impact of participant-specific factors and intervention-specific factors on intervention effectiveness.
Methods
Search strategy
A systematic search was conducted through searches of the electronic databases CINAHL, PsycINFO, PubMed, Sociological Abstracts, and Web of Science. The last search was conducted on April 4, 2016. Key search terms included caregiving, infant care, maternal-child relations, maternal behavior, pregnancy, pregnant women, therapy, violence, and child car*, maternal car*, parent* pregnan*, intervention*, therap* and treatment* as root searches. See Supplementary Material for search details. The titles of all retrieved articles were screened to exclude non-pertinent papers and duplicates, after which study abstracts were read. Full texts of the selected studies were then retrieved and read in full. The bibliographies of relevant articles were reviewed to identify other potentially relevant articles not otherwise indexed or discoverable.
Inclusion criteria
The literature search included interventional studies of human subjects with no limitation on the year of publication or language. An article was included if it met the following criteria: 1) the study was a randomized controlled trial (RCT); 2) participants were pregnant women or new mothers identified as being at elevated risk of abusing their offspring; 3) a stated goal of the intervention was to prevent child abuse. An article was excluded if 1) the study was not a RCT; 2) the participants were not pregnant women or mothers of infants; 3) participants were not assessed for a history of childhood abuse or other psychosocial risk factors for abusing their offspring; and finally 4) if the intervention was not designed to prevent offspring abuse. The quality of the studies was evaluated using
Quality assessment
After full text evaluation, the risk of bias and the quality of the selected studies was assessed by two reviewers (EJL & BG) separately, based on the Cochrane Collaboration tool for assessing risk of bias in intervention studies (Higgins, 2011). Key domains of the risk of bias assessment were sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting and any other relevant issues. The reviewers independently assessed risk of bias for each study and classified every study as low, high or unclear risk of bias. Final classifications and inclusion in this review were determined by consensus. For a detailed overview of the quality assessment, see Table 1.
Table 1.
Characteristics of primary studies included in systematic review
| Author Year | Location (Country - State) | Population | Sample size | Intervention | Measures | Findings | Risk of bias | |
|---|---|---|---|---|---|---|---|---|
| Siegel 1980 | US- NC | Racially-diverse low-income women seeking prenatal care | 321 | Lay visitors made 9 visits from birth through 3mos PP | 12mos | CPS, MR, attachment inventory, PPVT | No significant differences observed in attachment, maltreatment or healthcare utilization | Low |
| Olds 1986 | US- NY | Pregnant women presenting for free care | 400 | Nurse visitors made biweekly visits during pregnancy, weekly visits for 6mos PP, then decreasing until 2yrs | 15yrs | CPS, HOME, IQ, MR | Fewer episodes of mother perpetrating abuse (p=0.01) or child experiencing abuse (p=0.04). Also decrease in chronic abuse (p=0.08), which significantly decreased EB (p=0.0001). | Low |
| Barth 1991 | US- CA | Low-income pregnant women | 191 | Lay visitors made 5–20 home visits from pregnancy through 6mos PP | 6mos | CPS, CAPI, CES-D, STAI, Pearlin, CRUS, SSP, ISSB, SSI, ITQ, Bayley | No significant impact on maternal mental health or abuse risk. | High |
| Schuler 2000 | US (multisite) | Substance abusers delivering at urban academic medical center | 131 | Lay visitors performed weekly parent-child interaction therapy from birth through 6mos PP | 6mos | Videotaped feeding interaction scored for maternal behavior | Among mothers with ongoing substance use, intervention increased maternal responsiveness (p<0.01). | Low |
| Stevens-Simon 2001 | US- CO | Teens (13–19) delivering at urban academic medical center, FSC>25 | 171 | Lay visitors came every 6 wks and called every 2wks from birth to 2yrs PP to encourage medical follow-up | 2yrs | CPS, MR, maternal achievement, repeat pregnancy, HSQ, Bayley | HV intervention did not impact health-care utilization, return to school, repeat pregnancy or abuse behavior; social support predicted adherence to intervention (p<0.0001). | High |
| Bugental 2002 | US- CA | Pregnant women or <1 yr PP, FSC moderate (25–40) | 96 | Lay visitors conducted 20 visits from birth to 1yr PP (Control, HV, HV w/ CBT) | 12mos | CTS, STAI, BDI, parent interview about child injury, illness and feeding problems | Intervention decreased harsh parenting (p=0.05), with greater effect for high-risk infants (p<0.05), and improved child health (p=0.02) | Unclear |
| Olds 2004 | US- CO | Low-income women seeking prenatal care | 735 | Nurses and lay visitors made visits from pregnancy through 2yrs PP with variable frequency, averaging monthly | 4yrs | HOME, interaction assessment , mother's report, assessments of child's language, executive functioning and emotion regulation | Lay visits increased maternal employment, sense of mastery and mental health (p=0.03); nurse visits delayed subsequent birth (p=0.01), and for high-risk mothers, children had better cognitive outcomes (p<0.05) | Low |
| Barlow 2007 | UK | Pregnant women, low-income or mentally ill | 121 | Lay visitors made weekly visits from pregnancy through 1yr PP | 12mos | Edinburgh, HOME, SSQ, PSI, CARE-Index, ITS, Bayley, MR | HV impacted maternal sensitivity (p<0.04) and infant cooperativeness (p<0.02) but not abuse risk | Low |
| Dumont 2008 | US- NY | Low-income women pregnant or <3mos PP | 1173 | Lay visitors made biweekly visits during pregnancy, then weekly PP for 2yrs | 5yrs | CPS, Self-report of abuse and harsh parenting | Less abuse and harsh parenting, particularly among early intervention group (p<0.05). More positive parenting (p<0.05). | Low |
| Barlow 2013 | US- AZ | Teens (12–19) receiving prenatal care through the Indian Health Service | 322 | Lay visitors made 43 visits from pregnancy through 3yrs PP targeting parenting skills, substance abuse prevention, maternal life skills | 3yrs | CES-D, PLOC, HOME, ITSEA | Better parenting knowledge (p=0.001), parental self-efficacy (p=0.01), home safety attitudes (p=0.03) and less EB by children at 12mos (p=0.03) | Low |
| Ammerman 2015 | US- OH, KY | Depressed low-income women age 16+ | 93 | Social workers performed 15 sessions of CBT over 15wks, beginning PP | 3–6mos (3mos post-treatment) | Edinburgh, Hamilton, SCID, PSI, HOME, ASQ:SE | CBT not better than standard HV in terms of maternal stress, depression, nurturing behavior, and child adjustment | Unclear |
| ASQ:SE | Ages & Stages Questionnaire: Social-Emotional |
| Bayley | Multiscale battery for assessing infant and toddler development |
| BDI | Beck Depression Inventory |
| CAPI | Child abuse potential inventory |
| CARE | Screening tool for assessing parent-infant interaction quality |
| CAS | Composite abuse scale |
| CES-D | Center for Epidemiologic Studies- Depression Scale |
| CPS | Child Protective Services records |
| CRUS | Community Resources Use Scale |
| CTS | Conflict Tactics Scale |
| EB | Externalizing behavior |
| EPDS | Edinburgh Postnatal Depression Scale |
| FSC | Family Stress Checklist |
| Hamilton | Hamilton Rating Scale for Depression |
| HOME | Home Observation for Measurement of the Environment |
| HSQ | Home screening questionnaire |
| HV | Home visit |
| ISSB | Inventory of Social Supportive Behaviors |
| ITQ | Infant Temperament Questionnaire |
| ITSEA | Infant and Toddler Social and Emotional Assessment |
| MOS | Medical Outcomes Scale |
| MR | Medical Record |
| Pearlin | Pearlin Mastery Scale |
| PLOC | Parent Locus of Control scale |
| PP | Postpartum |
| PPVT | Peabody Picture Vocabulary Test |
| PSI | Parenting Stress Index |
| SCID | Structured Clinical Interview for DSM |
| SF36 | 36-item health survey |
| SSI | Social Support Inventory |
| SSP | Social Supports and Preparation Scale |
| SSQ | Social Support Questionnaire |
| STAI | State-Trait Anxiety Inventory |
Data extraction
Information extracted from the selected papers included country, setting, study population, sample size, study design, measuring tools, follow-up period and outcomes. The PRISMA guidelines were used as a framework for this review (Moher, Liberati, Tetzlaff, Altman, & Group, 2009).
Results
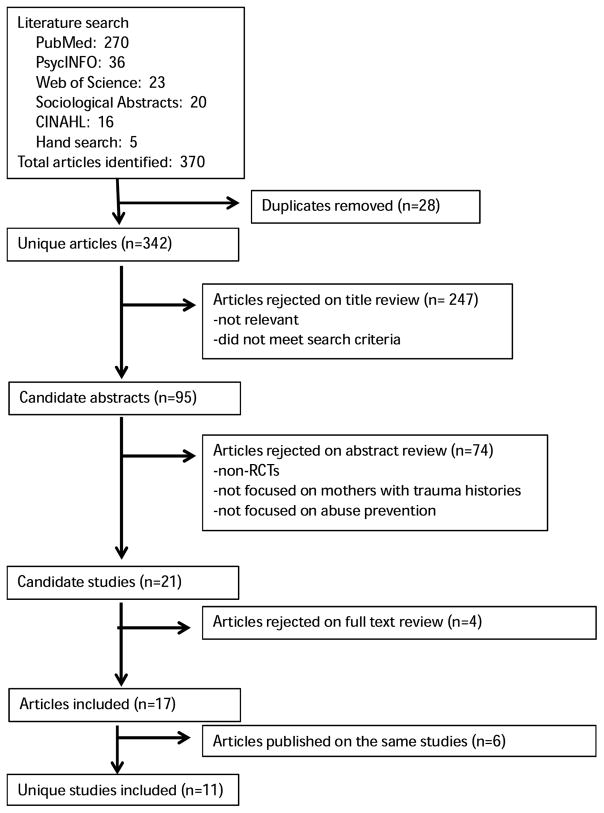
Through our electronic database search, we retrieved 365 potentially relevant articles (270 in PubMed, 36 in PsychINFO, 23 in Web of Science, 20 in Sociological Abstracts, and 16 in CINAHL). Five additional articles were identified by hand search. After duplicates were removed, there were 342 unique articles. Two hundred forty-seven articles were excluded based on title screen, and 74 were excluded based on abstract screen. Full text of the remaining 21 candidate articles were reviewed, and eight articles were excluded. Thirteen articles remained, representing eight unique studies. These studies were included in the final review (see Figure 1). The studies were published from 1980–2010 (see Table 1). Although this was not one of our inclusion criteria, in all eight studies, the intervention was a home visit.
Figure 1.
Flowchart of systematic literature review using PRISMA
Population
Seven of the studies were conducted in the United States (US) and one was conducted in the United Kingdom (UK). Studies took different approaches to identifying mothers at high risk of abusing their offspring. All of the studies recruited primarily low-income women, either by making this an explicit criterion for enrollment or by recruiting in a clinical setting that served a publicly-insured or free care population. Other risk factors included young age, maternal depression, family stress, lack of social support, and intimate partner violence. We found studies that recruited for maternal substance abuse, but none of these met our inclusion criteria. No studies were found that focused specifically on mothers with histories of childhood abuse.
Findings regarding the impact of participant age were mixed. Stevens-Simon et al (2001) specifically targeted adolescents and found that social support was particularly important. While there was no significant difference in abuse events between the intervention and control groups, participants with more social support were more likely to complete the intervention (p<0.0001). Only 33 of 58 (57%) of participants randomized to the intervention group completed at least 16 of the 22 home visits planned. Dumont et al. (2008) did a sub-group analysis and found that the prevention group, a sub-group of adolescent first-time mothers who were enrolled prior to 30 weeks gestation, had a particularly robust response to the intervention. Compared with the overall study population, they had a greater decrease in self-reported physical aggression and harsh parenting, and the difference was statistically significant (p=0.02).
Among depressed mothers, one study demonstrated decreased child abuse in response to home visiting (DuMont et al., 2008) while another study found other benefits but no significant impact upon abuse (J. Barlow et al., 2007). Dumont et al (2008) also did a sub-group analysis of psychologically vulnerable mothers with depressive symptoms or low sense of mastery and found that mothers in the intervention group were nearly a quarter as likely to report engaging in serious abuse or neglect, as compared with the control group (5% vs. 19%, p-value not reported), and the rates in the intervention group were similar to the overall rates in the less vulnerable group. The average number of self-reported events of serious physical abuse or neglect during their second year in the HFNY program was statistically significantly lower than their counterparts in the control group (0.02 vs. 0.62, p<0.05) (DuMont et al., 2008). Another study enrolled women in the UK with depression or housing insecurity (J. Barlow et al., 2007). This study found increased maternal sensitivity (p<0.04) and infant cooperativeness (p<0.02) but no significant impact upon child abuse events.
Three studies used family stress levels at the time of enrollment as a marker of risk (Bugental et al., 2002; DuMont et al., 2008; Stevens-Simon, Nelligan, & Kelly, 2001). A score of ≥25 (considered moderate to severe) on the Family Stress Checklist (Murphy, Orkow, & Nicola, 1985) was a criteria for enrollment in two studies (DuMont et al., 2008; Stevens-Simon et al., 2001), and a score of 25–40 (moderate) was the criteria in the third (Bugental et al., 2002). Two of these studies found a significant decrease in abuse events in the intervention groups (Bugental et al., 2002; DuMont et al., 2008). One study found that higher baseline scores on the Family Stress Checklist predicted abuse events in both the intervention and control groups, with no significant decrease in the intervention group (Stevens-Simon et al., 2001).
Eckenrode et al. (2000) found that intimate partner violence (IPV) negatively impacted response to home visiting. Among mothers who reported ≤28 incidents of IPV over a 15-year period, home visiting had a significant impact upon the number of reports of maltreatment to child protective services (CPS) during the same period (p=0.01); the intervention did not significantly impact child maltreatment in families reporting >28 IPV incidents (Eckenrode et al., 2000).
Visitor training and background
Six of the studies used paraprofessionals to conduct the intervention, one used nurses, and one used both nurses and paraprofessionals and compared the groups. In the majority of the studies, the home visitor was a paraprofessional from the same community as the participant, with some training and experience with parenting. Three of these studies described the training and supervision procedures for their paraprofessionals, which included at least 40 hours of training and weekly supervision (Barth, 1991; DuMont et al., 2008; Siegel, Bauman, Schaefer, Saunders, & Ingram, 1980). In most cases, paraprofessional visitors did not have college degrees, or their educational background was not reported, but in one study they did have bachelor’s degrees (Stevens-Simon et al., 2001).
There has been some debate about whether home visits should be performed by nurses, rather than lay visitors. Nurse visitors are more costly, and the evidence for greater benefit is mixed. Studies that have assessed the impact of gaining the mothers’ trust have found that it is an important predictor of program success (A. Barlow, B. Mullany, et al., 2013; Olds et al., 2007). While some researchers report that nurses are better able to gain trust because the mothers respect their training and expertise (Olds et al., 2004; Olds et al., 2007), others have found that mothers are most comfortable with women from a similar ethnic and cultural background, regardless of education (A. Barlow, Mullany, et al., 2013). The study that used nurse visitors had a significant impact on child abuse and neglect (Eckenrode et al., 2000; Olds et al., 1986), as did two of the six studies of paraprofessional visitors (Bugental et al., 2002; DuMont et al., 2008).
One study compared nurses and lay visitors and found that while lay visitors were more successful in helping mothers to feel a sense of mastery and self-empowerment, nurse visitors were more effective in supporting depressed mothers with limited psychological resources and improving cognitive outcomes for their children (Olds et al., 2004). CPS records were not used, and no differences were reported in other measures of abuse.
Visit frequency and duration
The duration of the intervention varied from as short as three months to as long as three years, and the follow up period varied from six months to 15 years. Four studies started the home visiting intervention during pregnancy (J. Barlow et al., 2007; Barth, 1991; Olds et al., 1986; Olds et al., 2004). While only one of these studies found a significant impact upon child abuse events, all reported that beginning during pregnancy helped establish a sense of trust between the mother and the visitor that allowed the mother to rely on the visitor immediately after birth. In two studies, home visits stopped three to six months post-partum (Barth, 1991; Siegel et al., 1980). Two of the studies continued home visits through the first year (J. Barlow et al., 2007; Bugental et al., 2002). There were four studies that continued home visits until the child was two years old (DuMont et al., 2008; Olds et al., 1986; Olds et al., 2004; Stevens-Simon et al., 2001). In the majority of studies, the visit frequency was weekly or biweekly in the immediate postpartum period, gradually decreasing to monthly or bimonthly.
Siegel et al (1980) continued follow-up for an additional nine months post-intervention. Olds et al (2004) had assessments two years post-intervention, and Dumont et al (2008) continued to follow participants for three years after the intervention was completed. Olds et al (1986) followed families for 13 years post-intervention, until the children were 15 years old. The two studies with the longest follow-up periods, Dumont et al (2008) and Olds et al (1986), were also the two studies that found a significant difference in reported child abuse events. For the rest of the studies, the follow-up period was as long as the intervention period.
Intervention content
Intervention targets included accessing prenatal care and pediatric care, understanding infant development, enhancing parent-infant interaction, mobilizing psychosocial support, delaying repeat pregnancy and improving maternal life trajectory. In early studies, the goals of the intervention and the content of the home visits were more loosely defined; later studies were more specific about the content of the home visits. Siegel et al (1980) stated that the goal of the home visits in their studies was “to promote the mothers’ involvement with their infants and to support mothers in coping with the range of situational stresses that might be confronting them.” The Child Parent Enrichment Program (CPEP) and the Comprehensive Adolescent-oriented Maternity Program (CAMP) focused primarily on increasing access to healthcare, as well as developing parenting skills (Barth, 1991; Stevens-Simon et al., 2001). The Family Partnership Model (FPM) focused on the parent-infant interaction (J. Barlow et al., 2007).
Studies with more explicitly-defined intervention content demonstrated more significant impact. The Nurse Family Partnership (NFP) focused on educating mothers about infant development and improving their access to social support and social services for which they were eligible (Eckenrode et al., 2000; Eckenrode et al., 2001; Olds et al., 1997; Olds et al., 1986; Olds, Henderson, & Kitzman, 1994). Healthy Families New York (HFNY) proposed a broad range of goals, including understanding infant development, enhancing parent-infant interaction, addressing maternal mental illness and substance use, mobilizing family support, accessing prenatal care, pediatric care, and social services (DuMont et al., 2008; Rodriguez, Dumont, Mitchell-Herzfeld, Walden, & Greene, 2010). The CBT intervention had a control condition that consisted of home visits focused on parenting education, accessing social support networks, and anger management. The enhanced condition consisted of the same home visiting structure with the addition of a CBT intervention that involved the parents discussing a problem they were having, making a causal appraisal and designing a strategic plan that was assessed at the next visit (Bugental et al., 2002). With 96 participants, this was the smallest study, and it was the only study with fewer than 700 participants to report a significant impact upon any measure of child abuse.
Outcome measures
In 13 articles representing eight studies, 32 distinct outcome measures were used to assess parenting behavior, parent-infant interaction, maternal mental health, child health and developmental outcomes. To assess child abuse, studies used the child abuse potential inventory, self-report of abuse or harsh parenting, child protective services (CPS) records, and substantiated reports.
Bugental et al (2002) did not report on CPS records but used the Conflict Tactics Scale as a primary outcome, which captures parent self-report of harsh parenting or abuse. An ANOVA across the three conditions (control, home visiting without CBT and home visiting with CBT) found a significant effect (p = 0.05).
Siegel et al (1980) found that some attachment measures, including interaction, acceptance and consoling behavior were slightly increased in the intervention arms, but the differences were not statistically significant and were attenuated over the course of follow-up. Abuse, neglect and healthcare utilization were not statistically significantly altered as a result of the intervention. CPEP did not demonstrate a significant impact on maternal wellbeing or child abuse events. The intervention did not impact parenting behavior or healthcare utilization by the mothers. In CAMP, mothers with more social support were more likely to remain in the study and participate in a majority of visits scheduled (94% vs. 44%, p<0.0001) (Stevens-Simon et al., 2001).
FPM did not find a significant difference in reported abuse events (J. Barlow et al., 2007). There was a higher rate of removal from the home for children in the intervention group (0% vs. 6%), which was not significant. The intervention group had higher maternal sensitivity, with a mean (standard deviation) of 9.27 (2.67) for the intervention group, compared with 8.2 (3.26) for the control group (p<0.04) as measured by the CARE Index Scale (J. Barlow et al., 2007). The same scale also identified an increase in child cooperativeness 9.35 (3.08), as compared with 7.92 (3.7) for the control group (p<0.02).
HFNY (DuMont et al., 2008) found that while there was no difference in the number of substantiated abuse events by CPS records and no difference in self-reported abuse or harsh parenting in the overall sample, the average number of events of serious physical abuse or neglect reported by a sub-sample of mothers with depressive symptoms or low sense of mastery during their second year in the HFNY program was statistically significantly lower than their counterparts in the control group (0.02 vs. 0.62, p<0.05) (DuMont et al., 2008). In the overall sample, positive parenting strategies were more prevalent in the HFNY group when interacting with their three-year-olds around the completion of three distinct tasks: Puzzle (97% vs. 92%), Delay (17% vs. 11%) and Cleanup (85% vs. 78%), (p<0.05 for all) (Rodriguez et al., 2010).
In NFP, mothers who received the extended home visit intervention had a lower mean number of reported abuse events over the 15 year follow up period in which they were perpetrators (0.32) compared with controls (0.65). The log difference reported was 0.81, with a p-value of 0.01. There was also a lower mean number of reported abuse events involving their children (0.44 vs. 0.73, log difference=0.59, p=0.04) (Eckenrode et al., 2000). In a subsequent trial, Olds et al (Olds et al., 2004) compared nurse visitors with lay visitors and both groups with a control condition. This study did not use CPS records, and child abuse was not a primary outcome. There were no statistically significant differences between the nurse-visited and lay-visited groups, but each group differed from the control condition on some measures. In a sub-sample of psychologically vulnerable mothers as defined by mental health, sense of mastery and intellectual functioning, comparing nurse-visited mothers with controls, their children had improved development outcomes, including better language development on the Preschool Language Scale (effect size=0.31, standard error=2.30, p=0.04) and superior executive functioning as measured by the Day-Night Inhibition Test (effect size=0.47, standard error=1.60, p=0.004). Mothers assigned to the lay visitor condition had better mental health (scale not reported) (effect size=0.03, standard error=0.94, p=0.03) and greater sense of mastery on the Pearlin Scale (effect size=0.2, standard error=0.89, p=0.03).
Significance
The size of the studies varied considerably, ranging from 96 to 1,173 participants. The studies of HFNY (DuMont et al., 2008; Rodriguez et al., 2010) NFP (Eckenrode et al., 2000; Eckenrode et al., 2001; Olds et al., 1997; Olds et al., 1986; Olds et al., 1994; Olds et al., 2004), and CBT (Bugental et al., 2002) all documented statistically significant reductions in child abuse. HFNY and NFP used CPS records to ascertain the occurrence of child abuse; the CBT study relied on parent self-report. HFNY and NFP also had the longest duration of home visitation, continuing until the child was two years old. HFNY and NFP were among the largest studies, with 1,173 and 400 (735 in the nurse vs. lay visitors study (Olds et al., 2004)), respectively, making it more probable to detect a difference in this relatively rare outcome. The CBT study was able to detect a significant difference in self-reported abuse events with only 96 participants randomized. HFNY and NFP were found to be at low risk of bias, as were Siegel et al (1980), Olds et al (2004) and Barlow et al (2007). CBT had an unclear risk of bias because selection and detection procedures were not described. The remaining two studies were found to have high risk of bias.
Overall findings
In these studies, home visits were found to impact child abuse, as well as mother-infant interaction, maternal depression, repeat pregnancy, maternal employment, and cognitive development and externalizing behaviors of children. Factors associated with greater efficacy included: intervention starting in pregnancy and continuing for at least two years, weekly visit frequency in the immediate post-partum period, longer follow-up post-intervention, and specificity of intervention content. The evidence on visitor training varied across studies. NFP demonstrated a significant reduction in child abuse with nurse visitors (Olds et al., 1986), and HFNY and CBT demonstrated significant reductions with lay visitors (Bugental et al., 2002; DuMont et al., 2008). Nor was there clear evidence for an association between length of visitor training and effect size. HFNY did describe the amount of training the visitors received (DuMont et al., 2008), but NFP and CBT did not (Bugental et al., 2002; Olds et al., 1986).
In terms of participant factors, maternal depression was associated with greater efficacy, while IPV and lack of social support negatively impacted response to the intervention. Findings were mixed with regard to participant age. While HFNY found a larger effect size within a sub-sample of adolescent mothers compared with the overall study sample (DuMont et al., 2008), CAMP, a study of only adolescent mothers, did not find a significant impact, and nearly half of participants did not complete the intervention (Stevens-Simon et al., 2001).
Discussion
This systematic review identified eight unique RCTs designed to decrease child abuse. All of the studies identified used a home visiting intervention. Initially developed to increase access to prenatal care and improve neonatal outcomes, home visits have expanded their goals to target parenting and child development (Olds et al., 2007). Home visiting programs have generally targeted low-income mothers. One study targeted adolescents; another targeted women with depression. Despite what is known about the impact of maternal mental illness and abuse history upon risk of offspring abuse (Berlin et al., 2011; Lee, 2009; Madigan et al., 2014; Milan et al., 2004; Plant et al., 2013), only three of eight studies assessed for maternal depression (J. Barlow et al., 2007; Barth, 1991; Bugental et al., 2002), two asked about some depressive symptoms (DuMont et al., 2008; Olds et al., 2004), and three did not assess depression at all (Olds et al., 1986; Siegel et al., 1980; Stevens-Simon et al., 2001). Only one study reported data on maternal abuse history, and it did not describe the impact on response to the intervention (DuMont et al., 2008). This study did find that high incidence of IPV negatively impacted intervention response (DuMont et al., 2008).
Existing RCTs lack evidence regarding the effects of maternal history of childhood abuse on response to home visiting. Observational studies have identified patterns of abuse that impact a woman’s experience of pregnancy and motherhood (Berlin et al., 2011; Madigan et al., 2014). For example, women who were neglected often experience antepartum anxiety that remits after birth (Madigan et al., 2014). Further, women who were sexually abused avoid seeking prenatal care (Heritage, 1998) and experience higher rates of postpartum depression (Madigan et al., 2014), while women who were physically abused have offspring who experience less maltreatment when the women have greater social support (Berlin et al., 2011). Given these differences based on childhood exposures, women with abuse histories may benefit from distinct interventions and may need specific types of support to help them access these interventions. One possibility is that a group intervention could help normalize the experience of pregnancy and prenatal care and could also allow women to experience a greater sense of social support.
Evidence on interventions other than home visitation is limited. Two studies have assessed the efficacy and cost differential of postpartum groups as compared to home visits. The studies suggest that groups can improve parenting knowledge (McNeil & Holland, 1972) and maternal mental health (de Camps Meschino, Philipp, Israel, & Vigod, 2016) at a lower cost. However, these studies did not measure the impact upon child abuse events, and neither study was an RCT.
The effects of specific psychotherapeutic modalities upon child abuse should also be further explored. Two studies included a psychotherapy intervention, one of which demonstrated a decrease in harsh parenting by addressing misrepresentations of the infant’s state of mind (Bugental et al., 2002). This suggests that other cognitive interventions could be beneficial. For example, mentalization-based treatment (MBT) has been shown to be effective for reducing self-harm among adolescents with borderline personality disorder (Rossouw & Fonagy, 2012). Because patients with borderline personality disorder have difficulty navigating attachments and seeing others as separate from themselves, which are among the tasks of new mothers, it has been suggested that psychologically vulnerable pregnant women and new mothers might benefit from MBT (Markin, 2013).
It is notable that seven of the eight studies were conducted in the US, and the other was conducted in the UK. Observational studies suggest that intergenerational cycles of violence are a significant problem in many low- and middle-income countries (LMICs), particularly in post-conflict societies where exposure to violence is high (Crombach & Bambonye, 2015; Saile, Ertl, Neuner, & Catani, 2016), but more intervention research is needed. RCTs of parenting interventions in LMICs have not focused specifically on parents with histories of abuse or mental illness but have instead targeted whole populations in low-resource settings (Knerr et al., 2013). Moreover, these studies have not reported on child abuse outcomes (Cooper et al., 2009; Knerr et al., 2013; Rahman, Iqbal, Roberts, & Husain, 2009). Many LMICs have different cultural norms around physical punishment, which impacts what is considered to be abuse. Further characterizing these norms using qualitative and observational studies will allow for more accurate assessment of abuse and will also inform intervention development.
There are a number of limitations to this systematic review. While we took steps to eliminate bias when possible, we are aware that the selection of databases, determination of inclusion criteria and interpretation of the findings all introduced potential sources of bias. Our search criteria were designed to identify studies of interventions targeting child abuse prevention. Studies that were primarily focused on increasing positive parenting but did not assess abuse or abuse risk were excluded. Many recent studies of novel interventions have not chosen to track abuse as an outcome because it is relatively rare and a large sample with a long follow up period is needed to detect significance. They have focused instead on markers of parental sensitivity and child developmental outcomes. These studies were therefore excluded, leaving this review with a small number of studies meeting our inclusion criteria. While these other markers are highly correlated with child abuse and may provide more information about the downstream impact of abuse, it is also important to identify abuse events and understand their impact.
Conclusion
Available published evidence indicates promising possibilities for decreasing child abuse in high-risk families. Future research should specifically assess the needs of mothers who experienced childhood abuse and identify interventions that can help them. Thus far, only home visitation has a significant evidence base for reducing child abuse, and the findings vary considerably. Data from LMICs are limited; there would be benefit to studying groups and other lower-cost interventions in these settings, in addition to home visits.
Acknowledgments
This research was supported by awards from the National Institutes of Health (T32-MH-093310 and R01-HD-059835).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alonso-Marsden S, Dodge KA, O'Donnell KJ, Murphy RA, Sato JM, Christopoulos C. Family risk as a predictor of initial engagement and follow-through in a universal nurse home visiting program to prevent child maltreatment. Child Abuse Negl. 2013;37(8):555–565. doi: 10.1016/j.chiabu.2013.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Astuto J, Allen L. Home visitation and young children: An approach worth investing. Social Policy Report. 2009;XXII(IV):3–21. [Google Scholar]
- Avellar SA, Supplee LH. Effectiveness of home visiting in improving child health and reducing child maltreatment. Pediatrics. 2013;132(Suppl 2):S90–99. doi: 10.1542/peds.2013-1021G. [DOI] [PubMed] [Google Scholar]
- Banducci AN, Hoffman EM, Lejuez CW, Koenen KC. The impact of childhood abuse on inpatient substance users: specific links with risky sex, aggression, and emotion dysregulation. Child Abuse Negl. 2014;38(5):928–938. doi: 10.1016/j.chiabu.2013.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow A, Mullany B, Neault N, Compton S, Carter A, Hastings R, … Walkup JT. Effect of a paraprofessional home-visiting intervention on American Indian teen mothers' and infants' behavioral risks: a randomized controlled trial. Am J Psychiatry. 2013;170(1):83–93. doi: 10.1176/appi.ajp.2012.12010121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow A, Mullany B, Neault N, Compton S, Carter A, Hastings R, … Walkup JT. Effect of a paraprofessional home-visiting intervention on American Indian teen mothers' and infants' behavioral risks: a randomized controlled trial. Am J Psychiatry. 2013;170(1):83–93. doi: 10.1176/appi.ajp.2012.12010121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow J, Davis H, McIntosh E, Jarrett P, Mockford C, Stewart-Brown S. Role of home visiting in improving parenting and health in families at risk of abuse and neglect: results of a multicentre randomised controlled trial and economic evaluation. Arch Dis Child. 2007;92(3):229–233. doi: 10.1136/adc.2006.095117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barth RP. An experimental evaluation of in-home child abuse prevention services. Child Abuse Negl. 1991;15(4):363–375. doi: 10.1016/0145-2134(91)90021-5. [DOI] [PubMed] [Google Scholar]
- Bensley L, Van Eenwyk J, Wynkoop Simmons K. Childhood family violence history and women's risk for intimate partner violence and poor health. Am J Prev Med. 2003;25(1):38–44. doi: 10.1016/s0749-3797(03)00094-1. [DOI] [PubMed] [Google Scholar]
- Berlin LJ, Appleyard K, Dodge KA. Intergenerational continuity in child maltreatment: mediating mechanisms and implications for prevention. Child Dev. 2011;82(1):162–176. doi: 10.1111/j.1467-8624.2010.01547.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertone-Johnson ER, Whitcomb BW, Missmer SA, Karlson EW, Rich-Edwards JW. Inflammation and early-life abuse in women. Am J Prev Med. 2012;43(6):611–620. doi: 10.1016/j.amepre.2012.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bugental DB, Ellerson PC, Lin EK, Rainey B, Kokotovic A, O'Hara N. A cognitive approach to child abuse prevention. J Fam Psychol. 2002;16(3):243–258. doi: 10.1037//0893-3200.16.3.243. [DOI] [PubMed] [Google Scholar]
- Casillas KL, Fauchier A, Derkash BT, Garrido EF. Implementation of evidence-based home visiting programs aimed at reducing child maltreatment: A meta-analytic review. Child Abuse Negl. 2016;53:64–80. doi: 10.1016/j.chiabu.2015.10.009. [DOI] [PubMed] [Google Scholar]
- Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, Anda RF. Adverse childhood experiences and the risk of depressive disorders in adulthood. J Affect Disord. 2004;82(2):217–225. doi: 10.1016/j.jad.2003.12.013. [DOI] [PubMed] [Google Scholar]
- Coid J, Petruckevitch A, Feder G, Chung W, Richardson J, Moorey S. Relation between childhood sexual and physical abuse and risk of revictimisation in women: a cross-sectional survey. Lancet. 2001;358(9280):450–454. doi: 10.1016/s0140-6736(01)05622-7. [DOI] [PubMed] [Google Scholar]
- Coogan PF, Wise LA, O'Connor GT, Brown TA, Palmer JR, Rosenberg L. Abuse during childhood and adolescence and risk of adult-onset asthma in African American women. J Allergy Clin Immunol. 2013;131(4):1058–1063. doi: 10.1016/j.jaci.2012.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper PJ, Tomlinson M, Swartz L, Landman M, Molteno C, Stein A, … Murray L. Improving quality of mother-infant relationship and infant attachment in socioeconomically deprived community in South Africa: randomised controlled trial. BMJ. 2009;338:b974. doi: 10.1136/bmj.b974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crombach A, Bambonye M. Intergenerational violence in Burundi: Experienced childhood maltreatment increases the risk of abusive child rearing and intimate partner violence. Eur J Psychotraumatol. 2015;6:26995. doi: 10.3402/ejpt.v6.26995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danese A, Moffitt TE, Harrington H, Milne BJ, Polanczyk G, Pariante CM, … Caspi A. Adverse childhood experiences and adult risk factors for age-related disease: depression, inflammation, and clustering of metabolic risk markers. Arch Pediatr Adolesc Med. 2009;163(12):1135–1143. doi: 10.1001/archpediatrics.2009.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Camps Meschino D, Philipp D, Israel A, Vigod S. Maternal-infant mental health: postpartum group intervention. Arch Womens Ment Health. 2016;19(2):243–251. doi: 10.1007/s00737-015-0551-y. [DOI] [PubMed] [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. JAMA. 2001;286(24):3089–3096. doi: 10.1001/jama.286.24.3089. [DOI] [PubMed] [Google Scholar]
- DuMont K, Mitchell-Herzfeld S, Greene R, Lee E, Lowenfels A, Rodriguez M, Dorabawila V. Healthy Families New York (HFNY) randomized trial: effects on early child abuse and neglect. Child Abuse Negl. 2008;32(3):295–315. doi: 10.1016/j.chiabu.2007.07.007. [DOI] [PubMed] [Google Scholar]
- Eckenrode J, Ganzel B, Henderson CR, Jr, Smith E, Olds DL, Powers J, … Sidora K. Preventing child abuse and neglect with a program of nurse home visitation: The limiting effects of domestic violence. JAMA: Journal of the American Medical Association. 2000;284(11):1385–1391. doi: 10.1001/jama.284.11.1385. [DOI] [PubMed] [Google Scholar]
- Eckenrode J, Zielinski D, Smith E, Marcynyszyn LA, Henderson CR, Jr, Kitzman H, … Olds DL. Child maltreatment and the early onset of problem behaviors: can a program of nurse home visitation break the link? Dev Psychopathol. 2001;13(4):873–890. [PubMed] [Google Scholar]
- Elliott S, Sanjack M, Leverton T. Parents' groups in pregnancy: a preventive intervention for postnatal depression? In: Gottlieb B, editor. Marshaling Social Support: Formats, Processes, and Effects. Los Angeles, CA: SAGE Publications; 1988. [Google Scholar]
- Fraiberg S, Adelson E, Shapiro V. Ghosts in the nursery. A psychoanalytic approach to the problems of impaired infant-mother relationships. J Am Acad Child Psychiatry. 1975;14(3):387–421. doi: 10.1016/s0002-7138(09)61442-4. [DOI] [PubMed] [Google Scholar]
- Frans O, Rimmo PA, Aberg L, Fredrikson M. Trauma exposure and post-traumatic stress disorder in the general population. Acta Psychiatr Scand. 2005;111(4):291–299. doi: 10.1111/j.1600-0447.2004.00463.x. [DOI] [PubMed] [Google Scholar]
- Heritage C. Working with childhood sexual abuse survivors during pregnancy, labor, and birth. J Obstet Gynecol Neonatal Nurs. 1998;27(6):671–677. doi: 10.1111/j.1552-6909.1998.tb02637.x. [DOI] [PubMed] [Google Scholar]
- Higgins J. Assessing risk of bias in included studies. Higgins JGS, editor. Cochrane handbook for systematic reviews of interventions. 2011 (Vol. 5.1.0). Retrieved from http://handbook.cochrane.org/chapter_8/8_assessing_risk_of_bias_in_included_studies.htm.
- Knerr W, Gardner F, Cluver L. Improving positive parenting skills and reducing harsh and abusive parenting in low- and middle-income countries: a systematic review. Prev Sci. 2013;14(4):352–363. doi: 10.1007/s11121-012-0314-1. [DOI] [PubMed] [Google Scholar]
- Lee Y. Early motherhood and harsh parenting: the role of human, social, and cultural capital. Child Abuse Negl. 2009;33(9):625–637. doi: 10.1016/j.chiabu.2009.02.007. [DOI] [PubMed] [Google Scholar]
- Madigan S, Wade M, Plamondon A, Vaillancourt K, Jenkins JM, Shouldice M, Benoit D. Course of depression and anxiety symptoms during the transition to parenthood for female adolescents with histories of victimization. Child Abuse Negl. 2014;38(7):1160–1170. doi: 10.1016/j.chiabu.2014.04.002. [DOI] [PubMed] [Google Scholar]
- Markin RD. Mentalization-based psychotherapy interventions with mothers-to-be. Psychotherapy (Chic) 2013;50(3):360–365. doi: 10.1037/a0031993. [DOI] [PubMed] [Google Scholar]
- McNeil HJ, Holland SS. A comparative study of public health nurse teaching in groups and in home visits. Am J Public Health. 1972;62(12):1629–1637. doi: 10.2105/ajph.62.12.1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milan S, Lewis J, Ethier K, Kershaw T, Ickovics JR. The impact of physical maltreatment history on the adolescent mother-infant relationship: mediating and moderating effects during the transition to early parenthood. J Abnorm Child Psychol. 2004;32(3):249–261. doi: 10.1023/b:jacp.0000026139.01671.fd. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. W264. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- Murphy S, Orkow B, Nicola RM. Prenatal prediction of child abuse and neglect: a prospective study. Child Abuse Negl. 1985;9(2):225–235. doi: 10.1016/0145-2134(85)90015-8. [DOI] [PubMed] [Google Scholar]
- Olds DL, Eckenrode J, Henderson CR, Jr, Kitzman H, Powers J, Cole R, … Luckey D. Long-term effects of home visitation on maternal life course and child abuse and neglect. Fifteen-year follow-up of a randomized trial. Jama. 1997;278(8):637–643. [PubMed] [Google Scholar]
- Olds DL, Henderson CR, Jr, Chamberlin R, Tatelbaum R. Preventing child abuse and neglect: a randomized trial of nurse home visitation. Pediatrics. 1986;78(1):65–78. [PubMed] [Google Scholar]
- Olds DL, Henderson CR, Jr, Kitzman H. Does prenatal and infancy nurse home visitation have enduring effects on qualities of parental caregiving and child health at 25 to 50 months of life? Pediatrics. 1994;93(1):89–98. [PubMed] [Google Scholar]
- Olds DL, Robinson J, Pettitt L, Luckey DW, Holmberg J, Ng RK, … Henderson CR., Jr Effects of home visits by paraprofessionals and by nurses: age 4 follow-up results of a randomized trial. Pediatrics. 2004;114(6):1560–1568. doi: 10.1542/peds.2004-0961. [DOI] [PubMed] [Google Scholar]
- Olds DL, Sadler L, Kitzman H. Programs for parents of infants and toddlers: recent evidence from randomized trials. J Child Psychol Psychiatry. 2007;48(3–4):355–391. doi: 10.1111/j.1469-7610.2006.01702.x. [DOI] [PubMed] [Google Scholar]
- Plant DT, Barker ED, Waters CS, Pawlby S, Pariante CM. Intergenerational transmission of maltreatment and psychopathology: the role of antenatal depression. Psychol Med. 2013;43(3):519–528. doi: 10.1017/s0033291712001298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman A, Iqbal Z, Roberts C, Husain N. Cluster randomized trial of a parent-based intervention to support early development of children in a low-income country. Child Care Health Dev. 2009;35(1):56–62. doi: 10.1111/j.1365-2214.2008.00897.x. [DOI] [PubMed] [Google Scholar]
- Rodriguez ML, Dumont K, Mitchell-Herzfeld SD, Walden NJ, Greene R. Effects of Healthy Families New York on the promotion of maternal parenting competencies and the prevention of harsh parenting. Child Abuse Negl. 2010;34(10):711–723. doi: 10.1016/j.chiabu.2010.03.004. [DOI] [PubMed] [Google Scholar]
- Rossouw TI, Fonagy P. Mentalization-based treatment for self-harm in adolescents: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2012;51(12):1304–1313. e1303. doi: 10.1016/j.jaac.2012.09.018. [DOI] [PubMed] [Google Scholar]
- Saile R, Ertl V, Neuner F, Catani C. Children of the postwar years: A two-generational multilevel risk assessment of child psychopathology in northern Uganda. Dev Psychopathol. 2016;28(2):607–620. doi: 10.1017/S0954579415001066. [DOI] [PubMed] [Google Scholar]
- Schaaf KK, McCanne TR. Relationship of childhood sexual, physical, and combined sexual and physical abuse to adult victimization and posttraumatic stress disorder. Child Abuse Negl. 1998;22(11):1119–1133. doi: 10.1016/s0145-2134(98)00090-8. [DOI] [PubMed] [Google Scholar]
- Siegel E, Bauman KE, Schaefer ES, Saunders MM, Ingram DD. Hospital and home support during infancy: impact on maternal attachment, child abuse and neglect, and health care utilization. Pediatrics. 1980;66(2):183–190. [PubMed] [Google Scholar]
- Stamp GE, Williams AS, Crowther CA. Evaluation of antenatal and postnatal support to overcome postnatal depression: a randomized, controlled trial. Birth. 1995;22(3):138–143. doi: 10.1111/j.1523-536x.1995.tb00689.x. [DOI] [PubMed] [Google Scholar]
- Stevens-Simon C, Nelligan D, Kelly L. Adolescents at risk for mistreating their children. Part II: A home- and clinic-based prevention program. Child Abuse Negl. 2001;25(6):753–769. doi: 10.1016/s0145-2134(01)00237-x. [DOI] [PubMed] [Google Scholar]
- Stoltenborgh M, Bakermans-Kranenburg MJ, van Ijzendoorn MH, Alink LR. Cultural-geographical differences in the occurrence of child physical abuse? A meta-analysis of global prevalence. International journal of psychology : Journal international de psychologie. 2013;48(2):81–94. doi: 10.1080/00207594.2012.697165. [DOI] [PubMed] [Google Scholar]