Abstract
Objective
To examine the relative influence of hospital and skilled nursing facilities (SNFs) on 30‐day rehospitalization.
Data Sources/Settings
Elderly Medicare beneficiaries newly admitted to a SNF following hospitalization.
Study Design
We ranked hospitals and SNFs into quartiles based on previous years’ adjusted rehospitalization rates (ARRs) and examined how rehospitalizations from a given hospital vary depending upon the admitting SNF ARR quartile. We examined whether the availability of SNFs with low rehospitalization rates influenced hospitals’ SNF readmission rates and whether changes in a hospital's ARR over 3 years is associated with changes in the SNFs to which they discharge.
Principal Findings
Hospital readmission rates from SNFs varied 5 percentage points between patients discharged to SNFs in the lowest and the highest rehospitalization quartiles. Low rehospitalization rate hospitals sent a larger fraction of their patients to the lowest rehospitalization SNFs available in the area. A 10 percent increase in hospital's share of discharges to the lowest rehospitalization quartile SNFs is associated with a 1 percentage point reduction in hospital's ARR.
Conclusions
The SNF rehospitalization rate has greater influence on patients’ risk of rehospitalization than the discharging hospital. Identifying high‐performing SNFs may be a powerful strategy for hospitals to reduce rehospitalizations.
Keywords: 30‐day rehospitalization rate, skilled nursing facilities, hospital discharge
Background
The reduction of rehospitalizations of Medicare beneficiaries has been a focus of policy initiatives and quality improvement programs for over a decade (Naylor et al. 1999; Coleman et al. 2006; Jack et al. 2009; Jencks, Williams, and Coleman 2009; Ouslander et al. 2011; Joynt and Jha 2013). This focus intensified since public reporting of hospital readmission rates began in 2009, readmission penalties were announced with the Affordable Care Act (ACA) in 2010, and hospitals were financially liable for excess readmissions beginning in 2012. Over this period, considerable progress has been made in developing and testing interventions designed to reduce rehospitalizations (Hansen et al. 2011). Effective programs include restructuring the predischarge planning process (Jack et al. 2009), enhancing patient/family education via coaching following discharge (Coleman et al. 2006), and postdischarge care coordination and management (Naylor et al. 1999). However, most of these and other interventions have focused on community discharges, smooth care plan transition to the primary care provider, and timely referral and visitation of home health services.
Over 20 percent of all Medicare beneficiaries are discharged to a skilled nursing facility (SNF; MedPAC 2015), and rehospitalizations of patients discharged to SNFs are higher than that associated with other discharge destinations (Mor et al. 2010). Prior literature reveals that both the discharging hospital and the patient play an important role in SNF choice decision (Rahman et al. 2014b; Rahman and Foster 2015). While some hospitals and health systems have developed “preferred” networks of closely aligned and/or higher quality providers to address the higher risk of patients discharged to SNF (Maly et al. 2012; Lage et al. 2015), most hospitals still adhere to the regulatory mandate requiring patient choice in discharge to a postacute provider. Regarding SNF care, hospitals have a multitude of choices; the median hospital sends about 32 percent of its discharges to the most frequently used SNF and about 90 percent of its discharges to the 10 most frequently used SNFs (Rahman et al. 2013a; Schoenfeld et al. 2016). Most patients, though, when discharged to a SNF, show preference to a facility close to their home. Unfortunately, if a patient's preferred SNF is low quality, the patient may be at risk for readmission or other adverse outcomes (Grabowski et al. 2013; Rahman et al. 2014a). Furthermore, with the advent of readmission penalties, the choices that patients make can have adverse effects on hospitals’ finances. Finally, currently available nursing home compare measures are only weakly correlated with hospital readmission rates (Neuman, Wirtalla, and Werner 2014).
The role of SNF's contribution to hospitals’ rate of rehospitalization has not been systematically explored. This paper examines whether the likelihood of rehospitalization of an SNF‐bound patient is more affected by the prior rehospitalization pattern of the admitting SNF than it is by the prior rehospitalization rate of the discharging hospital. If the degree of variation in rehospitalization from SNF depends more upon which SNF a patient enters than which hospital discharges the patient, hospitals and patients may need to choose more wisely where they receive postacute care.
Methods
Data Sources
We merged data covering the period of 2009–2011 from four sources: (1) the Medicare Standard Analytic File including all claims for Medicare fee‐for‐service (FFS) enrollees related to inpatient, SNF care, home health, outpatient and hospice services containing service dates, up to 25 ICD‐9 codes, special treatments, and diagnosis‐related groups (DRGs); (2) the Medicare enrollment file identifying individuals enrolled in Medicare in a given year, including demographic data, survival status, residential zip code, and program eligibility information for Parts A, B, and D, Medicare Advantage (managed care), and Medicaid; (3) SNF characteristics were obtained from the Online Survey Certification and Reporting System (OSCAR); and (4) hospital characteristics were obtained from the 2007 American Hospital Association survey.
Study Population
We include Medicare FFS patients aged 65 and older who had a hospitalization between 2009 and 2011 and were discharged to a SNF for postacute care no more than 3 days following hospital discharge. Managed Care patients were excluded due to the absence of hospital claims and because incentives vary substantially across plans. Medicare beneficiaries with age less than 65 years enrolled in Medicare because of disability and were excluded to reduce heterogeneities across patients.
We used data for 2009 and 2010 to calculate prior rehospitalization rates and used 2011 data to perform our main analysis, estimating the association of hospitals’ and SNFs’ prior rehospitalization rates on individual patients’ hospital readmission. Rehospitalization rates for hospitals and SNFs with low numbers of admissions are highly volatile from year to year, so to ensure stable facility‐level rehospitalization rates, we restricted our study to the 3,221 general hospitals with at least 80 discharges and the 12,390 SNFs with at least 40 admissions in 2009–2010. The difference in thresholds reflects the fact that an average general hospital sends patients to multiple nursing homes and has around twice as many beds as the average SNF. From these facilities, a total of 2,745,751 patients were used to calculate hospitals’ and SNFs’ rehospitalization rates for 2009–2010. Our main analyses were performed on 946,822 FFS community‐based Medicare beneficiaries newly discharged from hospital to SNF in 2011. We excluded individuals with any nursing home stay in the year before the hospital discharge because having been a nursing home resident before influences SNF choice.
Variables
Our outcome variable is 30‐day rehospitalization defined as any acute hospitalization within 30 days of the index hospital discharge.
Our main explanatory variables are prior risk‐adjusted 30‐day rehospitalization rate for SNFs and hospitals calculated based on 2009–2010 data. We ranked hospitals and SNFs based on their rehospitalization rates over the prior 2 years for two reasons: first, a patient's SNF or hospital choice might be based on recently reported data as is the case with Nursing Home and Hospital Compare, and second, ranking based on current rates contributes to both outcome and the explanatory variable and generates reverse causality.
Case mix adjustment variables include demographics (age, sex, race) from the Medicare enrollment file and clinical characteristics, including Elixhauser (Elixhauser et al. 1998) and Deyo (Deyo, Cherkin, and Ciol 1992) comorbidity indices, hospital length of stay, any ICU use during the hospital stay, and DRGs from the index hospitalization claim. As the objective of this paper was to assess the occurrence of rehospitalization relative to patients’ risk of rehospitalization at discharge, we used risk adjustors from the baseline hospitalization claims. While most of the literature considers the Elixhauser and Deyo indices as alternative approaches to controlling for morbidity and other adverse outcome risks, they are not perfectly collinear. Indeed, several prior studies published in HSR (Rahman, Zinn, and Mor 2013; Rahman et al. 2015) found a strong association between hospital readmission and both indexes while both were present in the models simultaneously. We included both of them because our objective was to maximize the predictive ability of our risk adjustment model.
We use several hospital and nursing home characteristics to compare facilities with different rehospitalization rates. Hospital characteristics include size (number of beds), HRR region, and total number of full‐time physicians and registered nurses per bed. The HRR represents the concentration of facilities caring for a population of Medicare patients in a region and thus would better represent the competitive environment regarding SNF availability and patient discharge patterns versus an urban/rural scale for the provider location.
Skilled nursing facility characteristics include location, bed size, share of Medicaid residents, membership in a chain, ownership status (Grabowski et al. 2013; Hirth et al. 2013), hospital affiliation (Rahman, Zinn, and Mor 2013), and the availability of physician extender and nurse staffing ratios (Harrington et al. 2000; Schnelle et al. 2004; Castle 2008; Castle and Anderson 2011; Hyer et al. 2011).
Statistical Analysis
We are interested in the influence of hospitals and SNFs on the 30‐day rehospitalization risk for patients discharged to SNF. In general, this will reflect care provided in the hospital, care provided in the SNF, and any care provided after SNF discharge (if less than 30 days posthospital discharge). As we want to understand the relative hospital and SNF influence and not how various aspects of hospital or SNF quality translate into rehospitalizations, we focus on the relationship between risk‐adjusted variation in hospital and SNF rehospitalization rates.
Given our main objective, our statistical analysis has two key steps. First, using 2009–2010 data, we calculated 30‐day adjusted rehospitalization rates (ARR) for each hospital and SNF, referred to as prior ARR. Second, we examined the relative influence of hospitals and SNFs on the rehospitalization of new SNF discharges in 2011 using the prior ARR of hospitals and SNFs as a proxy for quality of care.
As shown below, the ARR of a facility f (hospital or SNF) is calculated as the ratio of the observed rehospitalization rate to the predicted rehospitalization rate, multiplied by the national mean 30‐day rehospitalization rate.
The predicted number of rehospitalizations was calculated using a patient‐level linear probability model with DRG and regional fixed effects:
| (1) |
Here, Rehosp ihr indicates whether individual i discharged from hospital h in hospital referral region r was rehospitalized within 30 days. X i are patients’ demographic and clinical characteristics. θ DRG are patient's DRG fixed effects. γ r are hospital's referral region fixed effects that account for regional variation of rehospitalization rates and ensure that each HRR has hospitals and SNFs with high and low ARR relative to that region's average rehospitalization rate. Following prior studies on 30‐day rehospitalization (Rahman et al. 2013a; Thomas et al. 2014), we estimated this equation as a linear probability model. Given the size of the dataset and the use of two groups of fixed effects, estimation of fixed effect logit or probit model becomes computationally intensive and intractable.
To calculate the prior ARR for hospitals and SNFs, we aggregated the 2009–2010 actual number of rehospitalizations and the predicted number of rehospitalizations from our linear probabilistic regression model to our desired facility unit of analysis (hospital and SNF). As an individual facility‐level analysis would include a multitude of SNF–hospital pairs for each hospital and we are interested in the broader trend of relative facility influence on rehospitalization rate, we grouped hospitals and SNFs into quartiles based upon their 2009–2010 ARR. Facility/patient characteristics were reported for hospitals and SNFs in each ARR quartile.
The relative influence of hospitals and SNFs on 30‐day ARR was examined comparing the variation in rehospitalization among 2011 patients discharged from a given hospital across admitting SNFs with different ARR rankings based on earlier years. For each hospital, we calculated the 2011 ARR from each SNFs where patients were discharged (i.e., ARR of each hospital–SNF pair with at least one discharge). To assess whether the ARR for patients discharged from a hospital varied with respect to the ARR of the SNF, we plotted the mean 2011 ARRs and the associated 95 percent confidence intervals for hospitals in different prior ARR quartile, separately for SNFs with different prior ARR quartiles. The means and confidence intervals were calculated using number of discharges in 2011 between hospital and SNF pair as weights.
We calculated partial R 2 statistics to determine whether hospital's or SNF's 2009–2010 ARR levels explain more variation in 30‐day rehospitalization in 2011. To calculate the partial R 2 of hospital's prior ARR and SNF's prior ARR, we estimated equation (1) with three different specifications: (a) including dummy variables indicating SNF's prior ARR quartile, (b) including dummy variables indicating hospital's prior ARR quartile, and (c) including dummy variables for both hospital's and SNF's ARR quartile. The partial R 2 of hospital's prior ARR is calculated as one minus the ratio of the residual sum of squares from specification (a) and the residual sum of squares from specification (c). Similarly, the partial R 2 of SNF's prior ARR is one minus the ratio of the residual sum of squares from specification (b) and the residual sum of squares from specification (c). As a sensitivity analysis, we examined partial R 2 for relatively homogeneous subgroups of patients. As SNFs may specialize in a particular type of patient, thus influencing the ARR of that SNF, we performed our analysis separately for patients with same primary diagnosis (knee replacement, acute myocardial infarction, congestive heart failure, and hip fracture). As Medicaid eligibility plays a key role in SNF selection (Rahman et al. 2014a,b), we performed separate analysis for patients with and without Medicaid eligibility. Additionally, we included hospital length of stay as a risk adjustor to increase predictive ability of our statistical model. However, longer length of hospital stay may reflect complications due to poor care. In such a scenario, ARR for hospitals with relatively higher length of stay will be underestimated. To address this issue, we performed a separate analysis without length of hospital stay as a risk adjustor.
As bed availability has a direct influence on patient choice of SNF, we examined the availability of beds in SNFs with different ARRs that are geographically proximate to the discharging hospital. For simplicity, we defined the hospitals’ choice set of SNFs, that is, the set of SNFs where they could have sent patients, as the nearest 15 SNFs from the hospital. We calculated the availability of SNFs in different ARR quartiles in each hospital's choice set in terms of the share of SNF beds in each SNF ARR quartile. We compared the availability of SNF beds in each SNF ARR quartile and the proportion of 2011 discharges to SNFs in ARR quartile 1 and quartile 4 from hospitals with different prior ARRs.
Finally, given the changing relationships between hospitals and SNFs, we exploited the panel nature of our data to examine whether a change in a hospital's rehospitalization rate is associated with a change in the SNFs to which its patients are discharged. Thus, we calculated the change in share of discharges to SNFs in different ARR quartiles between 2009–2010 and 2011 for each hospital. We then regressed within hospital, the change in the hospital's ARR onto changes in their share of discharges to SNFs in quartile 1, quartile 2, and quartile 3 (using the share of discharges to SNFs in quartile 4 as the reference group).
All analyses were performed using STATA version 14. The Brown University IRB approved this study as being exempt under Centers for Medicare/Medicaid Data Use Agreement 18900.
Results
We first calculated the ARR of hospitals and SNFs using prior 2009–2010 data. The estimated regression model that predicts the number of rehospitalizations revealed that the 30‐day rehospitalization was positively associated with greater patient complexity as measured by hospital length of stay, Charlson/Deyo and Elixhauser indices, and DRGs regardless of HRR (see column 1 of Table S1). We also estimated the same regression model using newly admitted SNF patients in 2011 (column 2 of Table S1), which was used to predict likelihood of 30‐day rehospitalization of these individuals.
Table 1 compares patient demographics and clinical characteristics of persons treated in 2011 in hospitals and SNFs in the bottom and top ARR quartiles as defined based upon 2009–2010 ARR. Patients in hospitals with higher prior ARR rates have more comorbid conditions as reflected by higher predicted rehospitalizations. On average, patients treated in quartile 4 SNFs have a slightly higher predicted likelihood of rehospitalization than do patients in quartile 1 SNFs (21.27 percent vs. 20.14 percent). Similarly, patients treated in quartile 4 hospitals have about a 1.5 percentage point higher predicted likelihood of rehospitalization than do patients in quartile 1 hospitals (20.7 percent vs. 19.2 percent). Actual rehospitalization rates vary considerably more, around 7 percentage points; from 23.4 percent to 16.4 percent among hospitals’ quartiles, and from 24.2 percent to 17.7 percent among SNFs’ quartiles. Comparisons of patient characteristics as well as facility characteristics across facilities in all four quartiles of ARR are detailed in Tables S2 and S3.
Table 1.
Comparison of Patient Characteristics Treated in Selected ARR Quartile Hospitals and SNFs in 2011
| Variable | Hospitals in ARR Quartile 1 | Hospitals in ARR Quartile 4 | SNFs in ARR Quartile 1 | SNFs in ARR Quartile 4 |
|---|---|---|---|---|
| Number of patients | 164,866 | 168,531 | 217,268 | 194,108 |
| Age | 81.43 | 81.17 | 81.42 | 81.26 |
| Female | 0.66 | 0.64 | 0.66 | 0.64 |
| Black | 0.05 | 0.12 | 0.05 | 0.1 |
| White | 0.93 | 0.84 | 0.92 | 0.86 |
| Dual eligible | 0.22 | 0.29 | 0.2 | 0.29 |
| Hospital length of stay | 6.43 | 7.58 | 6.56 | 7.52 |
| Any ICU use | 0.32 | 0.38 | 0.33 | 0.38 |
| Deyo index | 1.66 | 1.87 | 1.63 | 1.88 |
| Elixhauser index | 2.79 | 2.85 | 2.77 | 2.88 |
| Actual 30‐day rehospitalization rate | 16.36 | 23.42 | 17.74 | 24.2 |
| Predicted 30‐day rehospitalization rate | 19.15 | 20.68 | 20.14 | 21.27 |
| Adjusted 30‐day rehospitalization rate (ARR) | 17.37 | 23.01 | 17.85 | 23.12 |
Adjusted rehospitalization rate (ARR) quartiles are based on ARR for patients in 2009–2010.
Hospitals in different ARR quartiles are relatively evenly distributed across different U.S. regions and have similar numbers of physicians and RNs per bed (see Table S2). Hospitals in quartiles 1 and 4 are smaller in size than hospitals in quartile 2 and 3. SNFs in ARR quartile 4 have a higher share of Medicaid patients, are more likely to be for‐profit, and are less likely to be hospital‐based. No consistent patterns were observed with respect to staffing levels or occupancy rate.
The 2011 ARR, depending upon the 2009–2010 SNF ARR to which the patients were discharged, stratified by hospitals’ 2009–2010 ARR rank is plotted in Figure 1. Each vertical data point in a given type of hospital represents the 2011 mean and 95 percent confidence intervals of the ARR for their patients discharged to SNFs in different quartiles of ARRs. Hospitals with the lowest 2009–2010 ARR had a 2011 ARR of 16 percent among patients discharged to SNFs with the lowest 2009–2010 ARR but an average ARR of 21 percent among their patients discharged to SNFs in the highest historical SNF ARR quartile. At the other end of the spectrum, hospitals with the highest historical ARR had a 2011 ARR of around 20 percent when discharging their patients to SNFs with a low 2009–2010 ARR but an average close to 25 percent when discharging patients to SNFs with a historically high ARR. Thus, regardless of their overall ARR in 2009–2010, hospitals experience rehospitalization rates that are approximately 20 percent higher when their patients are sent to SNFs in the highest SNF ARR quartile and comparably lower rehospitalization rates when their patients are sent to facilities in the lowest SNF ARR quartile.
Figure 1.
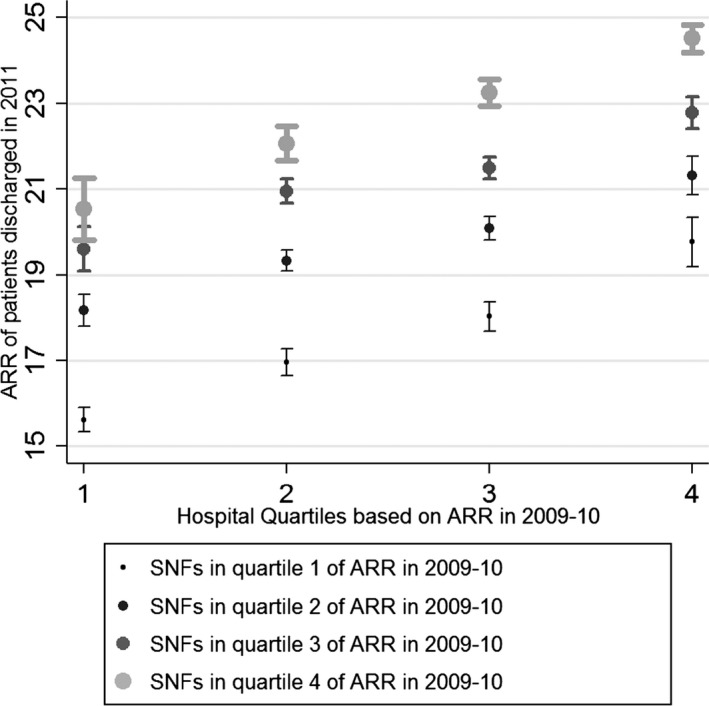
Plot of Adjusted Rehospitalization Rate (ARR) among Patients in 2011 with Respect to Discharging Hospital's and Admitting SNFs Adjusted Rehospitalization Rate in 2009–2010
Notes. National rehospitalization rate in 2011 for new admission SNF cohort was 20.4 percent. Thus, an ARR greater than 20.4 percent in the y‐axis implies the rehospitalization rate is higher than expected.
Table 2 presents the regression results testing the effect of hospitals’ and SNFs’ prior ARR quartile on the 30‐day rehospitalization risk of patients discharged from hospital and admitted to SNFs in 2011, controlling for patient's clinical and demographic characteristics, hospitalization DRG fixed effects, hospitalization month fixed effects, and HRR fixed effects. Compared to patients admitted to a quartile 1 SNF, patients treated in quartile 4 SNFs are 4.2 percentage points more likely to be rehospitalized. On the other hand, compared to the patients in quartile 1 hospitals, patients treated in quartile 4 hospitals are 2.6 percentage points more likely to be rehospitalized. Estimating the model without SNF ARR quartile effects (Table 2, column 2) increases the residual sum of squares, implying a partial R 2 for the SNF quartile dummies of 0.0012. Based on the model's residual sum of squares without 2009–2010 hospital ARR effects, the hospital dummy partial R 2 is 0.0004. As the unrestricted model R 2 (Table 2, column 1) is 0.0514, these partial R 2 imply that the historical SNF ARR explains 2.24 percent of the 30‐day rehospitalization variation compared to just 0.73 percent of explained variation attributable to the historical hospitals’ ARR. Partial R 2 analyses using patients with same primary diagnosis and Medicaid eligibility (see Table S6) show that historical ARR of SNFs consistently performs better in predicting hospital readmission than historical ARR of discharging hospital.
Table 2.
Regression Results of 30‐day Rehospitalization Risk among New SNF Patients in 2011: Effect of 2009–2010 Adjusted Rehospitalization Rates of the Treating Hospital and SNF
| Variables | 30‐day Rehospitalization | ||
|---|---|---|---|
| (1) | (2) | (3) | |
| Treated in a SNF in quartile 2 of ARR in 2009–2010 | 0.0143*** (12.14) | 0.0166*** (14.36) | |
| Treated in a SNF in quartile 3 of ARR in 2009–2010 | 0.0262*** (21.54) | 0.0311*** (26.38) | |
| Treated in a SNF in quartile 4 of ARR in 2009–2010 | 0.0418*** (31.59) | 0.0493*** (39.24) | |
| Treated in a hospital in quartile 2 of ARR in 2009–2010 | 0.00670*** (4.988) | 0.0133*** (10.10) | |
| Treated in a hospital in quartile 3 of ARR in 2009–2010 | 0.0151*** (11.31) | 0.0256*** (19.83) | |
| Treated in a hospital in quartile 4 of ARR in 2009–2010 | 0.0259*** (17.10) | 0.0415*** (28.76) | |
| Observations | 946,822 | 946,822 | 946,822 |
| R 2 | 0.0514 | 0.0503 | 0.0511 |
| Residual sum of squares | 145,822.94 | 145,990.80 | 145,877.74 |
All the models adjust for patient's clinical and demographic characteristics, hospitalization DRG fixed effects, hospitalization month fixed effects, and HRR fixed effects. Errors are clustered by HRR.
*** implies statistically significant at 1% level.
Figure 2 plots two variables with respect to hospital's historical 2009–2010 ARR: (1) the percentage of hospitals’ patients discharged to SNFs in the lowest (left panel) and the highest (right panel) ARR quartiles and (2) the percentage of SNF beds in the hospital's choice set that are in SNFs in the lowest (left panel) and the highest (right panel) SNF ARR quartiles based upon 2009–2010. Results for all hospital and SNF quartile combinations are presented in Table S4. Comparing the two panels in Figure 2, it is evident that hospitals with higher ARRs have relatively fewer low ARR SNFs in their choice set (downward sloping solid line in left panel) and more high ARR SNFs in their choice set (upward sloping solid line in right panel). Thus, the availability of low rehospitalization SNFs appears to influence hospitals’ rehospitalization rate substantially (also see Table S5). Nonetheless, historically low rehospitalization hospitals discharged more patients in 2011 to low rehospitalization SNFs than the share that those quartile 1 SNFs had of the total number of SNF beds locally available to the hospital (left panel), and sent a smaller share of patients to quartile 4 SNFs than the bed availability in such SNFs (right panel). This implies that, although there exists an imbalance in terms of availability of low ARR SNFs for high ARR hospitals, there may be sufficient available excess capacity of SNFs in the best ARR quartile that the hospitals could use.
Figure 2.
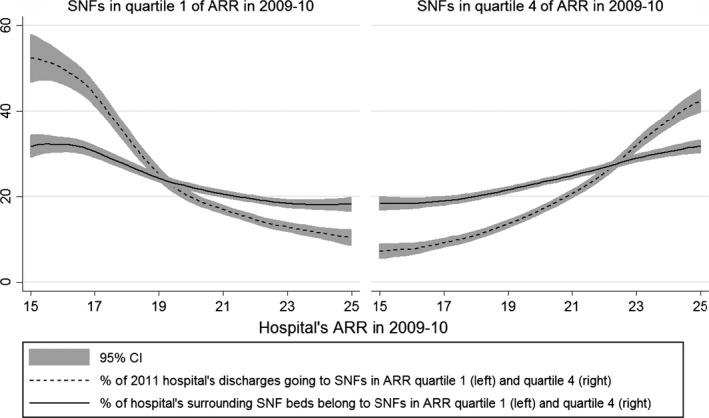
Share of Hospitals’ 2011 Discharges to and the Proportion of SNF Beds in the Hospitals’ Area That Are in SNFs in Low and High ARR Quartile Based on 2009–2010
Table 3 presents the statistical association between changes in the within‐hospital ARR between 2009–2010 and 2011 and changes in the share of discharges to SNFs in different historical ARR quartiles. A 10 percent increase in the share of discharges to quartile 1 SNFs is associated with a 1 percentage point decrease in a hospital's ARR; all other variables held constant (implying a decrease of 10 percent in the share of discharges to quartile 4 SNFs). A similar increase in the share of discharges to quartile 2 SNFs is associated with a decrease of hospital's ARR by 0.3 percentage points.
Table 3.
Regression of Change in Hospital's Rehospitalization Rates between 2009–2010 and 2011 onto Change of Hospital's Share of Discharges to SNFs in Different ARR Quartiles
| Variables | (1) |
|---|---|
| Change in Hospital's Adjusted Rehospitalization Rate between 2009–2010 and 2011 | |
| Change in hospital's share of discharges to SNFs in ARR quartile 1 between 2009–2010 and 2011 | −0.0983*** (−6.092) |
| Change in hospital's share of discharges to SNFs in ARR quartile 2 between 2009–2010 and 2011 | −0.0334** (−2.131) |
| Change in hospital's share of discharges to SNFs in ARR quartile 3 between 2009–2010 and 2011 | −0.0317** (−2.048) |
| Change in hospital's number of discharges to SNF between 2009–2010 and 2011 | 1.83E‐05 (0.107) |
| Constant | −0.0129 (−0.126) |
| Observations | 3,194 |
| R 2 | 0.012 |
Errors are clustered by HRR.
** implies statistically significant at 5% level; *** implies statistically significant at 1% level.
As the final sensitivity analysis, we examined the implications of length of hospital stay as a risk factor. We found that the Spearman's rank correlation coefficient between ARR for SNFs measured with and without length of hospital stay as a risk adjustor is 0.99, implying that they are roughly the same. The Spearman's rank correlation coefficient between ARRs for hospitals is 0.96, implying that hospitals’ ARRs are relatively more affected by the exclusion of length of stay. Additionally, exclusion of hospital length of stay reduces the R 2 substantially from 0.0514 to 0.0476 (see Table S6). However, the relative influence of hospital and SNF ARR quartile dummies remained mostly the same (comparing column 1 and 9 of Table S6).
Summary and Implications
Since 2009, when rehospitalization rates began to be publicly reported to the passage of the ACA, which introduced penalties for hospitals with rehospitalization rates higher than expected, policy makers and hospital leaders have been focused on this measure that is increasingly considered the ultimate indicator of quality. While much attention has focused on discharges to the community, rehospitalization rates from SNF are higher and little is known about the relative influence of a patient's hospital and SNF choices on rehospitalization rates. This paper aimed to examine the relative influence of the discharging hospital and the admitting SNF on 30‐day rehospitalization rates of new SNF admissions from hospital in 2011.
We ranked SNFs and hospitals by quartile based on prior years’ adjusted 30‐day rehospitalization rate and examined whether rehospitalization among patients from hospitals with a given ranking varies depending on the ranking of the SNF. We found that SNFs played a larger role in rehospitalization than hospitals. Regardless of the ranking of a hospital, the rehospitalization rate of patients admitted to SNFs in the highest rehospitalization quartile was 5 percentage points higher than those admitted to SNFs in the lowest rehospitalization quartile. While patients in high rehospitalization rate hospitals were 2.6 percentage points more likely to be rehospitalized than patients in the lowest quartile hospitals, the difference in the highest and lowest quartile SNFs was 4.2 percentage points. While the ability of our model to predict 30‐day rehospitalization is only about 5 percent, the partial R 2 analysis suggest that variation attributable to SNF rehospitalization rate quartiles is three times higher than that attributable to historical hospital rehospitalizations rates. Furthermore, we found that hospitals with low rehospitalization rates discharged more of their patients to low rehospitalization SNFs than the availability of beds in those facilities in the area and that between 2009–2010 and 2011, hospitals that increased their share of discharges to low rehospitalization SNFs experienced a reduction in their rehospitalization rate. These results suggest that there is a marginal benefit, in terms of reducing hospitals’ rehospitalization rates, to referring patients to SNFs with low rehospitalization rates.
The recent decline in the rehospitalization rate of fee‐for‐service Medicare beneficiaries has been attributed to the introduction of the Medicare rehospitalization penalty and its increasing bite (Daughtridge, Archibald, and Conway 2014). However, many argue that factors out of the hospital's control such as market pressure, regional practice patterns, local poverty rates, and local community resources better explain variation in rehospitalization rates than do patients’ clinical characteristics (Epstein, Jha, and Orav 2011; Herrin et al. 2014). While this may be true, our study clearly demonstrates another source of variation that can be responsible for some of hospitals’ rehospitalization rates—their pattern of discharges to SNFs, which could be better managed by the hospital.
The factors associated with rehospitalization from SNF are well documented, including having clinical staff in the SNF consistent with the acuity of the patients admitted (Ouslander et al. 2010; Grabowski et al. 2013; Rahman, Zinn, and Mor 2013). Furthermore, recent evidence that hospital‐based SNFs have lower rehospitalization rates and that hospitals that disproportionately discharge their SNF patients to a more select group of SNFs have lower rehospitalization rates suggests SNFs’ organizational linkage to the referring hospital is a critical factor to consider (Rahman, Zinn, and Mor 2013; Rahman et al. 2013b).
The literature on the impact of effective transition management strategies designed to reduce patients’ return to hospital has focused on coaches and navigators helping patients and families adjust to community living with more complex medical regimens that accompany hospitalization (Naylor et al. 1999; Coleman et al. 2006; Jack et al. 2008). Interventions designed to minimize failures of interorganizational transition between the hospital and SNF or to encourage discharges to higher quality postacute providers have received less attention. While some literature documents the importance of establishing preferred provider networks, there is little empirical evidence regarding the organizational agreements necessary to facilitate patient care transition management, rapid transmission of critical clinical information, clinical care pathways that span care settings, and even cross‐coverage by hospitalists and postacute care specialists. These are areas where careful study of the relative effectiveness of certain care practices is necessary.
One challenge hospitals face in building a viable postacute network and differentially discharging patients to preferred providers is the federal requirement that patients be offered choice (Centers for Medicare and Medicaid Services 2014). Historically, this has been translated by discharge planners into offering patients and their families a list of SNF names, without guidance regarding quality. Patients, in the absence of clinical guidance, routinely select the SNF that is geographically closest to their home and neighborhood (Rahman et al. 2013b), often resulting in poor patients entering SNFs of poorer quality that are located in poor neighborhoods (Rahman et al. 2014a,b). Whether patients would be willing to go to a SNF that is further away, were the hospital to recommend it, is not known.
Hospitals are increasingly establishing formal postacute networks to which they attempt to refer their patients, although their willingness to do so in the face of considerable pressure to have patients and families make the choice (Luke 2014; Mor, Rahman, and McHugh 2015). Accountable Care Organizations and providers participating in bundles are currently grappling with precisely this problem while building their own postacute provider networks (Lage et al. 2015). Regardless, current practice that emphasizes patients’ choice and often defaults to proximity rather than quality may need reengineering. If possible, choosing SNFs with a lower rehospitalization rate is both good for patients to avoid the trauma of needless transitions and for hospitals to potentially avoid a payment penalty.
Our study has a number of limitations. First, our approach necessarily assumes that patients with higher unobservable risk are not systematically selected into high ARR SNFs. While the risk adjustment methodology accounts for patient demographics and clinical risk, any risk adjustment is going to be inexact and there is likely unadjusted risk that biases results. For instance, an SNF could select lower risk patients based on meetings with patients and/or conversations with discharge planners to uncover unobserved risk factors, which could deem a patient at higher risk for readmission. We did perform several sensitivity analyses to understand the role of such unobservable risk. For example, we found that the expected rehospitalization rate varies more widely across hospitals in different ARR quartiles than SNFs in different ARR quartiles. Additionally, our results hold even if we restrict patients to the more homogeneous population (see Table S6). Finally, prior studies using similar risk adjustors to those we applied but which used causal inference methods to correct for selection bias did not find much influence of unobserved risk factors on SNF selection (Grabowski et al. 2013).
Second, we infer that hospitals have a choice regarding the SNF to which they refer their patients, but this may not always be true. We could not account for any real‐time occupancy rate fluctuations among SNFs in a hospitals’ choice set; those with low rehospitalization rates may have higher occupancy rates, although we do not observe this relationship in our data. Furthermore, given SNF location is the number‐one determinant of patients’ choice of SNF, they may not have equal access to all SNFs in the hospital's choice set.
Our analysis also ignores a hospital's decision to use other types of postacute care like home health or independent rehabilitation facilities. In markets with many long‐term acute care hospitals (LTACHs) and inpatient rehabilitation facilities (IRFs), there may be different effects, particularly if we consider rehospitalization rates from SNF after patients have been discharged from IRFs or LTACHs. However, in those instances, determining accountability for the rehospitalization is much more ambiguous. Additionally, some rehospitalizations are planned and our analysis assumes that these planned rehospitalizations are randomly distributed across hospitals and SNFs.
Finally, our study represents discharge patterns that predate the hospital systems and postacute networks that are emerging across the country in response to various provisions of the ACA. While the study period of time is prior to readmission penalties, public reporting of readmission rates began in 2009 and the ACA, which announced the penalty, was signed into law in 2010. Unfortunately, documenting the different types of hospital systems and their postacute networks is beyond the scope of the current paper. Furthermore, we do not know if there are other risk arrangements between hospitals and insurers which could influence discharge patterns.
In summary, our study suggests that the admitting nursing home plays a larger role in patient's hospital readmission rate than does the discharging hospital. Sending patients to historically low rehospitalization SNFs is likely to improve patients’ outcomes and reduce the likelihood of rehospitalization and Medicare penalties.
Supporting information
Appendix SA1: Author Matrix.
Table S1. Regression Used to Predict Likelihood of 30‐Day Rehospitalization.
Table S2. Comparison of Patient and Facility Characteristics across Hospitals in Different Quartiles of Adjusted Rehospitalization Rate from SNF.
Table S3. Comparison of Patient and Facility Characteristics across SNFs in Different Quartiles of ARR.
Table S4. Share of Discharges to and Availability of SNFs in Different ARR Quartile.
Table S5. Regression of Hospital's Rehospitalization Rate onto Availability of SNFs in Different ARR Quartile.
Table S6. Regression Results of 30‐Day Rehospitalization Risk among New SNF Patients with Selected Primary Diagnosis in 2011: Effect of 2009–2010 Adjusted Rehospitalization Rates of the Treating Hospital and SNF.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This work was supported by the National Institute on Aging Grants P01 AG027296 (PI: Vincent Mor).
Disclosures: None.
Disclaimers: None.
The abstract for this paper was recognized as a winner at the 2015 AcademyHealth Annual Research Meeting and was invited to be published as part of the Health Services Research 2015 Best of ARM special section.
References
- Castle, N. G. 2008. “Nursing Home Caregiver Staffing Levels and Quality of Care.” Journal of Applied Gerontology 27 (4): 375–405. [Google Scholar]
- Castle, N. G. , and Anderson R. A.. 2011. “Caregiver Staffing in Nursing Homes and Their Influence on Quality of Care: Using Dynamic Panel Estimation Methods.” Medical Care 49 (6): 545–52. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services . 2014. “42 CFR Ch. IV §482.43: Condition of Participation: Discharge Planning.”
- Coleman, E. A. , Parry C., Chalmers S., and Min S. J.. 2006. “The Care Transitions Intervention: Results of a Randomized Controlled Trial.” Archives of Internal Medicine 166 (17): 1822–8. [DOI] [PubMed] [Google Scholar]
- Daughtridge, G. W. , Archibald T., and Conway P. H.. 2014. “Quality Improvement of Care Transitions and the Trend of Composite Hospital Care.” Journal of the American Medical Association 311 (10): 1013–4. [DOI] [PubMed] [Google Scholar]
- Deyo, R. A. , Cherkin D. C., and Ciol M. A.. 1992. “Adapting a Clinical Comorbidity Index for Use with ICD‐9‐CM Administrative Databases.” Journal of Clinical Epidemiology 45 (6): 613–9. [DOI] [PubMed] [Google Scholar]
- Elixhauser, A. , Steiner C., Harris D. R., and Coffey R. M.. 1998. “Comorbidity Measures for Use with Administrative Data.” Medical Care 36 (1): 8–27. [DOI] [PubMed] [Google Scholar]
- Epstein, A. M. , Jha A. K., and Orav E. J.. 2011. “The Relationship between Hospital Admission Rates and Rehospitalizations.” New England Journal of Medicine 365 (24): 2287–95. [DOI] [PubMed] [Google Scholar]
- Grabowski, D. C. , Feng Z., Hirth R., Rahman M., and Mor V.. 2013. “Effect of Nursing Home Ownership on the Quality of Post‐Acute Care: An Instrumental Variables Approach.” Journal of Health Economics 32 (1): 12–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen, L. O. , Young R. S., Hinami K., Leung A., and Williams M. V.. 2011. “Interventions to Reduce 30‐day Rehospitalization: A Systematic Review.” Annals of Internal Medicine 155 (8): 520–8. [DOI] [PubMed] [Google Scholar]
- Harrington, C. , Zimmerman D., Karon S. L., Robinson J., and Beutel P.. 2000. “Nursing Home Staffing and Its Relationship to Deficiencies.” Journals of Gerontology: Series B, Psychological Sciences and Social Sciences 55 (5): S278–87. [DOI] [PubMed] [Google Scholar]
- Herrin, J. , St Andre J., Kenward K., Joshi M. S., Audet A. M., and Hines S. C.. 2014. “Community Factors and Hospital Readmission Rates.” Health Services Research 50 (1): 20–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirth, R. A. , Grabowski D. C., Feng Z. L., Rahman M., and Mor V.. 2013. “Effect of Nursing Home Ownership on Hospitalization of Long‐Stay Residents: An Instrumental Variables Approach.” International Journal of Health Care Finance & Economics 14 (1): 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyer, K. , Thomas K. S., Branch L., Harman J., Weech‐Maldonado R., and Johnson C. E.. 2011. “The Influence of Nurse Staffing Levels on Quality of Care in Nursing Homes.” The Gerontologist 51 (5): 610–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jack, B. , Greenwald J., Forsythe S., O'Donnell J., Johnson A., Schipelliti L., Goodwin M., Burniske G. M., Hesko C., Paasche‐Orlow M., Manasseh C., Anthony D., Martin S., Hollister L., Jack M., Jhaveri V., Casey K., and Chetty V. K.. 2008. “Developing the Tools to Administer a Comprehensive Hospital Discharge Program: The ReEngineered Discharge (RED) Program (Vol. 3: Performance and Tools).” [PubMed]
- Jack, B. W. , Chetty V. K., Anthony D., Greenwald J. L., Sanchez G. M., Johnson A. E., Forsythe S. R., O'Donnell J. K., Paasche‐Orlow M. K., Manasseh C., Martin S., and Culpepper L.. 2009. “A Reengineered Hospital Discharge Program to Decrease Rehospitalization: A Randomized Trial.” Annals of Internal Medicine 150 (3): 178–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jencks, S. F. , Williams M. V., and Coleman E. A.. 2009. “Rehospitalizations among Patients in the Medicare Fee‐for‐Service Program.” New England Journal of Medicine 360 (14): 1418–28. [DOI] [PubMed] [Google Scholar]
- Joynt, K. E. , and Jha A. K.. 2013. “A Path Forward on Medicare Readmissions.” New England Journal of Medicine 368 (13): 1175–7. [DOI] [PubMed] [Google Scholar]
- Lage, D. E. , Rusinak D., Carr D., Grabowski D. C., and Ackerly D. C.. 2015. “Creating a Network of High‐Quality Skilled Nursing Facilities: Preliminary Data on the Postacute Care Quality Improvement Experiences of an Accountable Care Organization.” Journal of the American Geriatrics Society 63 (4): 804–8. [DOI] [PubMed] [Google Scholar]
- Luke, J. 2014. “CMS to Address Allowing Hospitals More Say in Selecting Post Acute Care Providers.” The American Journal of Accountable Care Available at https://www.nationalreadmissionprevention.com/content/documents/finally-cms-to-address-allowing-hospitals-more-say-in-selecting-post-acute-care-providers.pdf [Google Scholar]
- Maly, M. B. , Lawrence S., Jordan M. K., Davies W. J., Weiss M. J., Deitrick L., and Salas‐Lopez D.. 2012. “Prioritizing Partners across the Continuum.” Journal of the American Medical Directors Association 13 (9): 811–6. [DOI] [PubMed] [Google Scholar]
- MedPAC . 2015. “A Data Book: Health Care Spending and the Medicare Program” Available at http://medpac.gov/-documents-/data-book [Google Scholar]
- Mor, V. , Rahman M., and McHugh J.. 2015. “Accountability of Hospitals for Medicare Beneficiaries’ Postacute Care Discharge Disposition.” Journal of the American Medical Association Internal Medicine 176 (1): 119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor, V. , Intrator O., Feng Z., and Grabowski D. C.. 2010. “The Revolving Door of Rehospitalization from Skilled Nursing Facilities.” Health Affairs (Millwood) 29 (1): 57–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naylor, M. D. , Brooten D., Campbell R., Jacobsen B. S., Mezey M. D., Pauly M. V., and Schwartz J. S.. 1999. “Comprehensive Discharge Planning and Home Follow‐Up of Hospitalized Elders: A Randomized Clinical Trial.” Journal of the American Medical Association 281 (7): 613–20. [DOI] [PubMed] [Google Scholar]
- Neuman, M. D. , Wirtalla C., and Werner R. M.. 2014. “Association between Skilled Nursing Facility Quality Indicators and Hospital Readmissions.” Journal of the American Medical Association 312 (15): 1542–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouslander, J. G. , Lamb G., Perloe M., Givens J. H., Kluge L., Rutland T., Atherly A., and Saliba D.. 2010. “Potentially Avoidable Hospitalizations of Nursing Home Residents: Frequency, Causes, and Costs [see editorial comments by Drs. Jean F. Wyman and William R. Hazzard, pp. 760‐1].” Journal of the American Geriatrics Society 58 (4): 627–35. [DOI] [PubMed] [Google Scholar]
- Ouslander, J. G. , Lamb G., Tappen R., Herndon L., Diaz S., Roos B. A., Grabowski D. C., and Bonner A.. 2011. “Interventions to Reduce Hospitalizations from Nursing Homes: Evaluation of the INTERACT II Collaborative Quality Improvement Project.” Journal of the American Geriatrics Society 59 (4): 745–53. [DOI] [PubMed] [Google Scholar]
- Rahman, M. , and Foster A. D.. 2015. “Racial Segregation and Quality of Care Disparity in US Nursing Homes.” Journal of Health Economics 39: 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman, M. , Zinn J. S., and Mor V.. 2013. “The Impact of Hospital‐Based Skilled Nursing Facility Closures on Rehospitalizations.” Health Services Research 48 (2 Pt 1): 499–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman, M. , Foster A. D., Grabowski D. C., Zinn J. S., and Mor V.. 2013a. “Effect of Hospital‐SNF Referral Linkages on Rehospitalization.” Health Services Research 48 (6pt1): 1898–1919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman, M. , Grabowski D. C., Intrator O., Cai S., and Mor V.. 2013b. “Serious Mental Illness and Nursing Home Quality of Care.” Health Services Research 48 (4): 1279–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman, M. , Gozalo P., Tyler D., Grabowski D. C., Trivedi A., and Mor V.. 2014a. “Dual Eligibility, Selection of Skilled Nursing Facility, and Length of Medicare Paid Postacute Stay.” Medical Care Research and Review 71 (4): 384–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman, M. , Grabowski D. C., Gozalo P. L., Thomas K. S., and Mor V.. 2014b. “Are Dual Eligibles Admitted to Poorer Quality Skilled Nursing Facilities?” Health Services Research 49 (3): 798–817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman, M. , Tyler D., Thomas K. S., Grabowski D. C., and Mor V.. 2015. “Higher Medicare SNF Care Utilization by Dual‐Eligible Beneficiaries: Can Medicaid Long‐Term Care Policies Be the Answer?” Health Services Research 50 (1): 161–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnelle, J. F. , Simmons S. F., Harrington C., Cadogan M., Garcia E., and M. Bates‐Jensen B.. 2004. “Relationship of Nursing Home Staffing to Quality of Care.” Health Services Research 39 (2): 225–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoenfeld, A. J. , Zhang X., Grabowski D. C., Mor V., Weissman J. S., and Rahman M.. 2016. “Hospital‐Skilled Nursing Facility Referral Linkage Reduces Readmission Rates among Medicare Patients Receiving Major Surgery.” Surgery 159 (5): 1461–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas, K. S. , Rahman M., Mor V., and Intrator O.. 2014. “Influence of Hospital and Nursing Home Quality on Hospital Readmissions.” American Journal of Managed Care 20 (11): e523–31. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Table S1. Regression Used to Predict Likelihood of 30‐Day Rehospitalization.
Table S2. Comparison of Patient and Facility Characteristics across Hospitals in Different Quartiles of Adjusted Rehospitalization Rate from SNF.
Table S3. Comparison of Patient and Facility Characteristics across SNFs in Different Quartiles of ARR.
Table S4. Share of Discharges to and Availability of SNFs in Different ARR Quartile.
Table S5. Regression of Hospital's Rehospitalization Rate onto Availability of SNFs in Different ARR Quartile.
Table S6. Regression Results of 30‐Day Rehospitalization Risk among New SNF Patients with Selected Primary Diagnosis in 2011: Effect of 2009–2010 Adjusted Rehospitalization Rates of the Treating Hospital and SNF.


