Abstract
Objective
To describe characteristics of industrial injury hospitalizations, and to test the hypothesis that industrial injuries were increasingly billed to non‐workers' compensation (WC) payers over time.
Data Sources
Hospitalization data for 1998–2009 from State Inpatient Databases, Healthcare Cost and Utilization Project, and Agency for Healthcare Research and Quality.
Study Design
Retrospective secondary analyses described the distribution of payer, age, gender, race/ethnicity, and injury severity for injuries identified using industrial place of occurrence codes. Logistic regression models estimated trends in expected payer.
Principal Findings
There was a significant increase over time in the odds of an industrial injury not being billed to WC in California and Colorado, but a significant decrease in New York. These states had markedly different WC policy histories. Industrial injuries among older workers were more often billed to a non‐WC payer, primarily Medicare.
Conclusions
Findings suggest potentially dramatic cost shifting from WC to Medicare. This study adds to limited, but mounting evidence that, in at least some states, the burden on non‐WC payers to cover health care for industrial injuries is growing, even while WC‐related employer costs are decreasing—an area that warrants further research.
Keywords: Workers' compensation, cost shifting, insurance coverage, occupational injuries, hospital discharge data
Occupational injuries and illnesses place a heavy burden on workers, employers, workers' compensation (WC) systems, and society as a whole. The total national medical and productivity cost for occupational injuries and illnesses has been estimated at $250 billion annually, larger than the total cost of cancer (Leigh 2011). There is evidence that underreporting of work‐related injuries and cost shifting from WC to other public or private health care coverage and/or to workers themselves is significant and potentially on the rise (Rosenman et al. 2000; Shannon and Lowe 2002; Morse et al. 2005; Fan et al. 2006; Friedman and Forst 2007; Lipscomb et al. 2009). Workers, employers, and/or health care providers may be reluctant to file a WC claim, workers may not report a work injury to their employers or health care providers to avoid retaliation or stigma, work may not be identified as the cause of an injury, and WC coverage and reporting requirements have changed over time (Murphy et al. 1996; Rosenman et al. 2000, 2006; Morse et al. 2001; Azaroff, Levenstein, and Wegman 2002; Shannon and Lowe 2002; Azaroff et al. 2004; Smith, Veazie, and Benjamin 2005; Alamgir et al. 2006; Fan et al. 2006; Friedman and Forst 2007). The traditional tests to establish legal causation for injuries have been tightened in many jurisdictions (Burton 2015). In a previous study using linked trauma registry and WC records from Washington State, we found that that 27 percent of work‐related injuries did not have WC listed as a payer, and 37 percent did not link to an accepted WC claim (Sears et al. 2013b). Other studies have found similar percentages of occupational injuries that did not have WC listed as a payer; for example, 25 percent in a study based on the Illinois Trauma Registry (Friedman and Forst 2008), and about 20 percent in several studies using hospital discharge or emergency department data (Sorock, Smith, and Hall 1993; Nicholson, Bunn, and Costich 2008). A study of construction worker injuries used national survey data to find that less than half (46 percent) of medical costs were paid by WC, and only 27 percent for Latino workers (Dong et al. 2007).
Few studies have assessed trends in the amount of work‐related injuries billed to WC, in part because identifying work‐related injuries independently of payer is not possible in most population‐based health care data sets. Two of the three studies we identified covered very short timeframes, which renders trend estimates highly dependent on the starting and ending years selected. One of these, using National Hospital Ambulatory Medical Care Survey data, found that the proportion of work‐related emergency department visits that did not have WC listed as primary payer increased from 32 percent in 2003 to 45 percent in 2006 (Groenewold and Baron 2013). A RAND study assessed the rate at which industrial accidents treated at hospitals in Massachusetts were billed to WC, and it found a significant decrease from 2005 to 2008, attributable either to health care reform in that state or to the contemporaneous recession (Heaton 2012). In a Washington State study using linked trauma registry and WC records, we observed no increase over time (1998–2008) in the percentage of work‐related trauma lacking an accepted WC claim (Sears et al. 2013b). However, Washington State is one of only four states with an exclusive state fund (i.e., no private WC insurance carriers operate within the state) and may well be at variance with other states in this regard.
Payer and insurance coverage have implications beyond reimbursement and cost shifting; a study using the National Trauma Data Bank (NTDB) found preliminary evidence that among patients with blunt injuries, those with no identified payer had the highest odds of death (Weygandt et al. 2012). In addition, there are critical occupational injury surveillance and research efforts that rely on health care databases, and that generally must rely on the payer field to identify work relatedness (Council of State and Territorial Epidemiologists (CSTE) 2015). These efforts are hampered by the inability to identify all work‐related injuries, and even more so by the unknown degree of bias introduced by temporal trends in WC coverage that could impact estimated trends in work‐related injuries.
This study had three aims. The first was to describe the distribution of expected primary payer and secondary payers for industrial injury hospitalizations (a specific subset of work‐related injuries occurring in industrial places, defined in the Methods section). The second was to assess the degree to which expected payer for industrial injury hospitalizations varied by age, gender, race/ethnicity, injury severity, and over time. The third was to estimate population‐based hospital charges for industrial injury hospitalizations billed to WC and to other payers. We hypothesized that industrial injury hospitalizations were increasingly billed to non‐WC payers over time.
Methods
Data Sources and Study Populations
In most occupational injury studies using hospital discharge data, WC as expected primary payer is used to identify work‐related injuries (Council of State and Territorial Epidemiologists [CSTE] 2015). For this study, we needed to identify a specific set of work‐related injuries using a method independent of payer, to examine which payers were billed. Few population‐based data sets contain information other than payer that is suitable for determining work relatedness. However, state hospital discharge databases are both population based and contain ICD‐9‐CM external cause of injury codes (E‐codes). For purposes of this study, we identified work‐related industrial injuries using the E‐code E849.3 (place of occurrence: industrial place and premises). E849.3 may also identify some injuries to nonworkers who happened to be injured on industrial premises. Using linked trauma registry and WC data from Washington State, we previously found industrial place of occurrence to be 57.2 percent sensitive (95% CI: 56.0–58.4) and 98.5 percent specific (95% CI: 98.4–98.6) in identifying work‐related traumatic injuries, using an accepted WC claim as the gold standard (unpublished data; data sources and procedures previously described, Sears et al. 2012b). As a matter of convenience, we refer throughout this manuscript to those incurring such injuries as workers, though based on a proxy measure. We did not attempt to identify only those work‐related injuries that were or should be covered by WC. The group of industrial injuries not billed to WC includes those not eligible for WC coverage, but that is central to this study's purpose. For example, as temporary work becomes more prevalent, work‐related injuries are more often covered by non‐WC payers, including workers themselves (Azaroff et al. 2004). Other possible E‐codes that indicate work‐relatedness (e.g., E849.2 indicates place of occurrence as mine and quarry; E800.0 indicates a railway accident involving a railway employee; other E‐codes indicate longshoremen or commercial aircraft crew) are rarely present, and use of those codes would be complicated by the possibility of federal programs or other atypical WC coverage.
This approach was complicated by the fact that the place of occurrence E‐codes (E849.X) has been used inconsistently across states, and over time within states. To conduct this study, we needed to first identify a set of states having (1) hospital discharge data available via the Healthcare Cost and Utilization Project (HCUP) of the Agency for Healthcare Research and Quality, (2) state reporting of WC as a distinct payer category (not the case for many states), and (3) highly prevalent and temporally consistent usage of E849.X codes. Using data available via HCUP (HCUP State Inpatient Databases (SID) 1998) and hcupnet.ahrq.gov, we were able to identify only three states meeting these initial criteria: California, Colorado, and New York. These three states each had an average E849.X prevalence of at least 75 percent for the available years (shown in Table 1), no individual year with a prevalence below 70 percent, and no notable trend in usage across the years in question. A RAND study used E849.3 to identify work‐related injuries in Massachusetts (Heaton 2012); however, roughly 15 percent of hospital discharges in Massachusetts had E849.X codes, well below the threshold for inclusion in our study.
Table 1.
Characteristics of States and State Hospital Discharge Data
| Characteristic | California | Colorado | New York |
|---|---|---|---|
| Years available and included in this study | 2003–2009 | 1998–2009 | 1998–2009 |
| Number of payer fields in hospital discharge data | 1 | 1 | 3 |
| Percentage of dischargesa with any E‐code | 94.3% | 99.5% | 100.0% |
| Percentage of dischargesa with any E849.X code | 87.6% | 83.3% | 78.4% |
| Of dischargesa billed to WC, percentage with an E849.3 code | 46.4% | 35.9% | 31.0% |
| Of dischargesa with an E849.3 code, percentage billed to WC | 65.2% | 67.1% | 64.2% |
| Of dischargesa without an E849.3 code, percentage billed to WC | 2.0% | 3.2% | 3.2% |
| Percent share of WC benefits paid in 2009 by insurer type | |||
| State fund | 17.3% | 43.6% | 26.4% |
| Private insurance carriers | 51.7% | 27.8% | 43.3% |
| Self‐insured employers | 31.1% | 28.6% | 30.2% |
After application of all inclusion/exclusion criteria except for presence of E849.3.
WC, workers' compensation.
E849.3 identified roughly a third of all cases billed to WC in Colorado and New York, and nearly half in California, whereas the percentage of non‐E849.3 cases billed to WC was only 2–3 percent in all three states (Table 1). This comports with our previous findings that industrial place of occurrence is a highly specific, although not highly sensitive, indicator of work relatedness.
Population‐based community hospital discharge data for the three included states were obtained from the following HCUP Data Partners: California Office of Statewide Health Planning and Development, Colorado Hospital Association, and New York State Department of Health. All three states have a nonexclusive WC state fund, private WC insurers, and self‐insured employers; the mix for each state (Sengupta, Reno, and Burton 2011; table 8) is shown in Table 1, which also summarizes other characteristics of included states and their hospital discharge data sets.
Hospital discharges for inpatients ages 16 and over, who were residents of and treated within each included state, were included for all available years from 1998 through 2009 (see Table 1). Hospital discharges were included if E849.3 was present in any position; up to seven E‐codes were available per hospital discharge, depending on state and year. Hospital discharges were included if the principal diagnosis was a traumatic injury (defined below) to enhance the likelihood of workplace causation and immediate work attribution. There are fewer barriers to determining causality and WC reporting for traumatic injuries compared with chronic injuries or illnesses (Morse, Dillon, and Warren 2000; Azaroff, Levenstein, and Wegman 2002; Shannon and Lowe 2002; Fox et al. 2004). Traumatic injuries were defined using the ICD‐9‐CM diagnostic codes specified by the National Trauma Data Bank (2011). The definition required a first‐listed injury diagnostic code in the range 800–959.9, excluding the following injuries: 905–909.9 (late effects of injury), 910–924.9 (superficial injuries, including blisters, contusions, abrasions, insect bites), and 930–939.9 (foreign bodies). Burns (940–949.9) were excluded because the injury severity scoring system we used does not reliably classify burns due to the importance of inhalation injuries. Inclusion was based only on the principal diagnosis, an approach that avoids including injuries that occurred incidental or subsequent to hospital admission, and for the most part, captures the most severe injury (STIPDA: Injury Surveillance Workgroup 6 2008).
Measures and Data Analysis
The HCUP uniform data element for payer (PAY1, PAY2, and PAY3) has six categories: Medicare, Medicaid, Private insurance, Self‐pay, No charge/charity care, and Other. The Other category varies by state, but generally includes payers such as WC, Civilian Health and Medical Program of the Uniformed Services, Civilian Health and Medical Program of the Department of Veterans Affairs, Title V federal health programs, Indian Health Service, tobacco tax programs, government programs for the medically indigent, etc. For purposes of this study, we used the original data elements provided by the included states (PAY1_X, PAY2_X, and PAY3_X), which distinguish WC as a separate category. We recoded payer fields using the same categories as the uniform data element, but retaining WC as a separate seventh category. Finally, we combined the Self‐pay and No charge/charity care categories to reflect a single uninsured category. California and Colorado only had one payer field available, whereas New York had three. The operational definition of our outcome of interest, industrial injury hospitalizations not billed to WC, was based on any category other than WC being listed as expected primary payer.
Race/ethnicity was based on the HCUP uniform data element, which contains mutually exclusive race and ethnicity categories in one data element (RACE). When constructing the uniform data element from separate race and ethnicity data fields in state source data, HCUP gave ethnicity precedence over race. Native Americans were reclassified to the Other category because counts were too small to meet HCUP reporting requirements.
Total hospital charges were calculated using the HCUP uniform data element (TOTCHG), which contains cleaned total charges. Total charges do not include professional fees and noncovered charges.
The Abbreviated Injury Scale (AIS) was used to estimate injury severity from ICD‐9‐CM diagnosis codes (Association for the Advancement of Automotive Medicine 1990). AIS is an anatomically based consensus‐driven scoring system that rates injury severity based on threat to life and does not take comorbidity or complications into account. AIS‐based injury severity scores have been validated for prediction of mortality (Baker et al. 1974; Osler, Baker, and Long 1997; Meredith et al. 2002; Kilgo, Osler, and Meredith 2003; Harwood et al. 2006), and recent studies have established their association with occupational injury outcomes such as work disability and medical costs (Ruestow and Friedman 2013; Sears et al. 2013a). AIS was estimated from the first‐listed ICD‐9‐CM diagnosis code using ‐icdpic‐, a Stata user‐written program developed using NTDB data (Clark, Osler, and Hahn 2010). The most serious injury, usually listed first if the primary reason for admission, has been found to predict mortality as well or better than using all injuries (Kilgo, Osler, and Meredith 2003). The AIS ordinal scale ranges from 1 (minor) to 6 (maximal). We defined severe injury as an AIS of 3 or above; these injuries carry a high probability of hospital admission (Cryer and Langley 2008).
Unadjusted and adjusted logistic regression models were used to estimate the average annual change in the odds of industrial injuries not being billed to WC for each state, by including a continuous variable for discharge year. Robust variance estimates were used. Adjusted models included gender, race/ethnicity, a set of age category indicators (16–24, 25–34, 35–44, 45–54, 55–64, and 65+), and a severe injury indicator (AIS ≥3). All statistical tests were two‐tailed, with statistical significance defined as p ≤ .05. Analyses were performed using Stata/MP 13.1 for Windows (StataCorp LP, College Station, TX, USA).
Results
Table 2 presents the characteristics of industrial injury hospitalizations by expected payer, for each of the three states. In general, patterns were quite similar across the three states. In each state, those 65 and older were much more likely not to have their industrial injury billed to WC. Roughly a third of industrial injuries were not billed to WC, overall and stratified by most characteristics. However, roughly two thirds of industrial injuries among those 65 and older were not billed to WC; Medicare was billed for 82 percent of that subset in California, 69 percent in Colorado, and 79 percent in New York. Women were more likely than men to have their hospitalizations billed to non‐WC payers, particularly Medicare.
Table 2.
Characteristics of Industrial Injury Hospitalizations by Expected Primary Payer
| State/Characteristic | Billed to WC versus Non‐WC | Non‐WC Payer Distribution (for Non‐WC Discharges Only) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Total (N) | WC % of Total | Non‐WC % of Total | Non‐WC (N) | Percentage of Non‐WC Discharges Billed to Each Payer | |||||
| Medicare | Medicaid | Private Insurance | Other Coverage | Self‐Pay/No Charge | |||||
| California overall | 24,131 | 65.2 | 34.8 | 8,387 | 13.6 | 12.3 | 36.5 | 15.9 | 21.7 |
| Gender | 21,954 | 7,768 | |||||||
| Male | 18,605 | 66.1 | 33.9 | 6,313 | 8.6 | 13.3 | 35.5 | 18.3 | 24.4 |
| Female | 3,349 | 56.6 | 43.5 | 1,455 | 40.3 | 8.7 | 37.4 | 5.7 | 8.0 |
| Age | 24,131 | 8,387 | |||||||
| 16–24 | 2,981 | 71.3 | 28.8 | 857 | DS | 18.6 | 25.2 | 22.6 | 32.9 |
| 25–34 | 5,216 | 70.3 | 29.7 | 1,547 | DS | 15.2 | 27.2 | 24.5 | 32.5 |
| 35–44 | 5,307 | 66.6 | 33.4 | 1,774 | 1.9 | 15.0 | 38.1 | 19.2 | 25.8 |
| 45–54 | 5,765 | 66.5 | 33.5 | 1,932 | 3.2 | 12.1 | 48.2 | 15.2 | 21.4 |
| 55–64 | 3,169 | 65.5 | 34.5 | 1,094 | 5.7 | 8.5 | 61.1 | 11.2 | 13.5 |
| 65 and older | 1,693 | 30.1 | 69.9 | 1,183 | 81.8 | 3.6 | 12.4 | DS | 1.7 |
| Race/ethnicity | 24,131 | 8,387 | |||||||
| Non‐Latino White | 9,049 | 61.8 | 38.2 | 3,460 | 23.2 | 6.7 | 46.5 | 10.2 | 13.3 |
| Latino/Hispanic | 8,640 | 67.7 | 32.3 | 2,791 | 5.6 | 19.6 | 21.3 | 23.3 | 30.1 |
| Black/African‐American | 598 | 57.5 | 42.5 | 254 | 12.6 | 10.6 | 38.2 | 18.5 | 20.1 |
| Asian/Pacific Islander | 645 | 53.3 | 46.7 | 301 | 20.3 | 14.6 | 34.6 | 13.3 | 17.3 |
| Other/multiple | 419 | 65.9 | 34.1 | 143 | 14.0 | 17.5 | 35.0 | 13.3 | 20.3 |
| Unknown/missing | 4,780 | 69.9 | 30.1 | 1,438 | 4.5 | 10.8 | 42.0 | 15.7 | 27.1 |
| Injury severity | 23,974 | 8,338 | |||||||
| Minor (AIS 1–2) | 17,767 | 66.9 | 33.2 | 5,889 | 8.8 | 12.3 | 37.2 | 17.6 | 24.2 |
| Severe (AIS 3–6) | 6,207 | 60.5 | 39.5 | 2,449 | 25.3 | 12.2 | 34.7 | 11.9 | 15.9 |
| Colorado overall | 5,793 | 67.1 | 32.9 | 1,905 | 8.4 | 1.8 | 41.6 | 6.8 | 41.4 |
| Gender | 5,793 | 1,905 | |||||||
| Male | 5,072 | 67.7 | 32.3 | 1,637 | 4.7 | 1.9 | 40.5 | 7.4 | 45.5 |
| Female | 721 | 62.8 | 37.2 | 268 | 31.0 | DS | 48.1 | DS | 16.4 |
| Age | 5,793 | 1,905 | |||||||
| 16–24 | 854 | 74.1 | 25.9 | 221 | DS | DS | 25.3 | 7.2 | 64.7 |
| 25–34 | 1,386 | 70.6 | 29.4 | 407 | DS | DS | 31.5 | 7.9 | 58.7 |
| 35–44 | 1,430 | 66.6 | 33.4 | 478 | DS | 2.3 | 41.8 | 8.6 | 46.9 |
| 45–54 | 1,157 | 66.8 | 33.2 | 384 | DS | DS | 56.8 | 6.5 | 34.6 |
| 55–64 | 635 | 67.1 | 32.9 | 209 | 5.3 | DS | 64.1 | 7.2 | 20.6 |
| 65 and older | 331 | 37.8 | 62.2 | 206 | 69.4 | DS | 27.2 | DS | DS |
| Race/ethnicity | 5,793 | 1,905 | |||||||
| Non‐Latino White | 2,959 | 65.2 | 34.8 | 1,031 | 11.6 | 1.7 | 47.8 | 7.7 | 31.2 |
| Latino/Hispanic | 1,371 | 70.4 | 29.6 | 406 | DS | DS | 20.4 | 7.4 | 67.7 |
| Black/African‐American | 91 | 62.6 | 37.4 | 34 | DS | DS | DS | DS | 44.1 |
| Asian/Pacific Islander | 33 | 60.6 | 39.4 | 13 | DS | DS | DS | DS | DS |
| Other/multiple | 132 | 70.5 | 29.6 | 39 | DS | DS | 28.2 | DS | 59.0 |
| Unknown/missing | 1,207 | 68.4 | 31.7 | 382 | 5.5 | DS | 50.0 | 3.7 | 39.5 |
| Injury severity | 5,739 | 1,897 | |||||||
| Minor (AIS 1–2) | 4,084 | 68.8 | 31.2 | 1,275 | 6.1 | 0.9 | 41.5 | 7.1 | 44.3 |
| Severe (AIS 3–6) | 1,655 | 62.4 | 37.6 | 622 | 13.2 | 3.5 | 41.6 | 6.1 | 35.5 |
| New York overall | 19,894 | 64.2 | 35.8 | 7,126 | 10.2 | 15.3 | 37.3 | 2.4 | 34.8 |
| Gender | 19,891 | 7,125 | |||||||
| Male | 17,457 | 65.0 | 35.0 | 6,104 | 5.1 | 16.2 | 37.7 | 2.4 | 38.6 |
| Female | 2,434 | 58.1 | 42.0 | 1,021 | 40.7 | 10.2 | 34.9 | 2.2 | 12.1 |
| Age | 19,894 | 7,126 | |||||||
| 16–24 | 2,259 | 62.2 | 37.8 | 854 | DS | 20.1 | 26.4 | 3.8 | 49.7 |
| 25–34 | 4,360 | 66.7 | 33.3 | 1,450 | DS | 18.1 | 29.3 | 3.0 | 49.3 |
| 35–44 | 5,187 | 66.7 | 33.3 | 1,726 | 1.4 | 17.5 | 38.4 | 1.8 | 40.9 |
| 45–54 | 4,372 | 66.4 | 33.7 | 1,471 | 2.2 | 16.1 | 49.3 | 2.5 | 30.0 |
| 55–64 | 2,449 | 66.2 | 33.9 | 829 | 4.7 | 12.6 | 60.0 | 2.3 | 20.5 |
| 65 and older | 1,267 | 37.2 | 62.8 | 796 | 78.6 | 1.9 | 15.2 | DS | 3.3 |
| Race/ethnicity | 19,894 | 7,126 | |||||||
| Non‐Latino White | 10,942 | 67.4 | 32.6 | 3,563 | 15.7 | 8.5 | 49.4 | 2.3 | 24.1 |
| Latino/Hispanic | 3,301 | 61.6 | 38.4 | 1,268 | 2.8 | 26.3 | 21.3 | 3.1 | 46.5 |
| Black/African‐American | 1,979 | 60.4 | 39.6 | 783 | 5.8 | 20.4 | 32.4 | 2.3 | 39.1 |
| Asian/Pacific Islander | 537 | 52.5 | 47.5 | 255 | 5.9 | 26.3 | 24.3 | DS | 42.0 |
| Other/multiple | 2,497 | 59.8 | 40.2 | 1,003 | 4.0 | 19.7 | 23.3 | 1.1 | 51.8 |
| Unknown/missing | 638 | 60.2 | 39.8 | 254 | 12.6 | 11.4 | 29.5 | 6.3 | 40.2 |
| Injury severity | 19,767 | 7,085 | |||||||
| Minor (AIS 1–2) | 15,903 | 64.8 | 35.2 | 5,594 | 6.7 | 16.2 | 37.8 | 2.4 | 37.0 |
| Severe (AIS 3–6) | 3,864 | 61.4 | 38.6 | 1,491 | 23.8 | 12.1 | 35.3 | 2.2 | 26.6 |
Chi‐squared tests of independence were used to test associations between characteristics and payer distribution; all associations presented in this table were statistically significant, with p ≤ .01.
AIS, Abbreviated Injury Scale; DS, data suppressed due to small cell size (fewer than 11 discharges); WC, workers' compensation.
Figure 1 shows the percentages of industrial injury hospitalizations billed to WC and non‐WC payers by state and year. The percentage billed to non‐WC payers appeared to be growing over time in California and Colorado, but not in New York. This was confirmed using logistic regression models (Table 3). In models adjusted for gender, age, race/ethnicity, and injury severity, the null hypothesis of no trend for each of the three included states was rejected. We found that there was a 3.6 percent average annual increase in the odds of an industrial injury not being billed to WC in California, a 2.9 percent average annual increase in the odds of an industrial injury not being billed to WC in Colorado, but in New York, there was a 1.8 percent average annual decrease. Hospitalizations for more severe injuries had higher odds of not being billed to WC. Hospitalizations for those 65 and older had three to four times the odds of not being billed to WC, compared with those for ages 45–54. After adjustment for age in these models, gender was no longer significantly associated with billing to WC.
Figure 1.
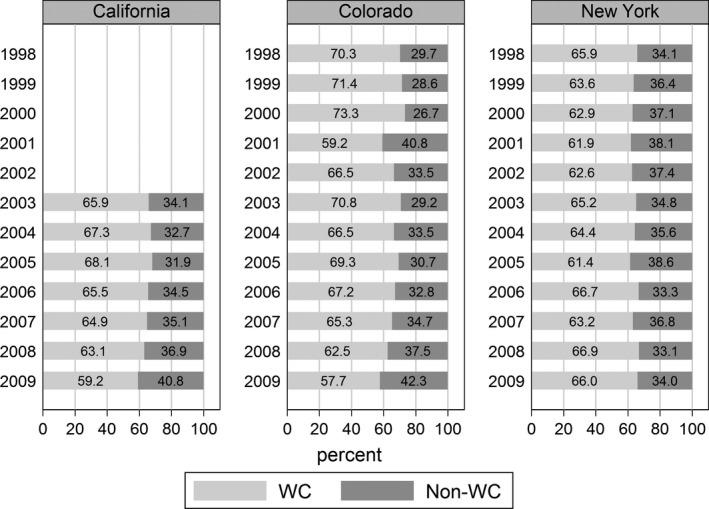
Percentage of Industrial Injury Hospitalizations Billed to Workers' Compensation (WC) or Non‐WC Payers by Year
Table 3.
Odds of Industrial Injury Hospitalizations Being Billed to Payers Other Than Workers' Compensation (Logistic Regression Models)
| Characteristic | California (N = 21,809) | Colorado (N = 5,739) | New York (N = 19,764) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p‐value | OR | 95% CI | p‐value | OR | 95% CI | p‐value | |
| Unadjusted model | |||||||||
| Year (annual trend) | 1.047 | 1.032, 1.063 | <.001 | 1.036 | 1.019, 1.052 | <.001 | 0.993 | 0.985, 1.002 | .11 |
| Adjusted model | |||||||||
| Year (annual trend) | 1.036 | 1.020, 1.051 | <.001 | 1.029 | 1.013, 1.046 | .001 | 0.982 | 0.974, 0.991 | <.001 |
| Gender | |||||||||
| Male | 1.000 | Reference | .43 | 1.000 | Reference | .48 | 1.000 | Reference | .12 |
| Female | 1.033 | 0.952, 1.123 | 0.939 | 0.788, 1.119 | 1.077 | 0.981, 1.182 | |||
| Age | |||||||||
| 16–24 | 0.811 | 0.731, 0.899 | <.001 | 0.730 | 0.598, 0.890 | <.001 | 1.144 | 1.028, 1.274 | <.001 |
| 25–34 | 0.845 | 0.774, 0.923 | 0.875 | 0.737, 1.040 | 0.941 | 0.859, 1.030 | |||
| 35–44 | 0.967 | 0.889, 1.051 | 1.033 | 0.875, 1.221 | 0.960 | 0.880, 1.046 | |||
| 45–54 | 1.000 | Reference | 1.000 | Reference | 1.000 | Reference | |||
| 55–64 | 0.964 | 0.876, 1.060 | 0.958 | 0.778, 1.181 | 1.030 | 0.926, 1.145 | |||
| 65 and older | 4.203 | 3.704, 4.770 | 3.144 | 2.416, 4.093 | 3.546 | 3.085, 4.076 | |||
| Race/ethnicity | |||||||||
| Non‐Latino White | 1.000 | Reference | <.001 | 1.000 | Reference | .40 | 1.000 | Reference | <.001 |
| Latino/Hispanic | 0.937 | 0.877, 1.001 | 0.890 | 0.770, 1.028 | 1.460 | 1.342, 1.589 | |||
| Black/African‐American | 1.322 | 1.111, 1.574 | 1.174 | 0.770, 1.790 | 1.470 | 1.329, 1.626 | |||
| Asian/Pacific Islander | 1.380 | 1.170, 1.627 | 1.081 | 0.536, 2.179 | 2.047 | 1.715, 2.444 | |||
| Other/multiple | 0.898 | 0.725, 1.111 | 0.821 | 0.557, 1.212 | 1.537 | 1.403, 1.685 | |||
| Unknown/missing | 0.902 | 0.818, 0.993 | 0.901 | 0.779, 1.041 | 1.381 | 1.168, 1.631 | |||
| Injury severity | |||||||||
| Minor (AIS 1–2) | 1.000 | Reference | .005 | 1.000 | Reference | .002 | 1.000 | Reference | .16 |
| Severe (AIS 3–6) | 1.097 | 1.028, 1.170 | 1.213 | 1.073, 1.372 | 1.055 | 0.979, 1.138 | |||
AIS, Abbreviated Injury Scale; OR, odds ratio.
In New York, the only included state with more than one available payer field, the primary payer field identified 12,768 discharges billed to WC. The secondary payer field identified 230 additional WC discharges, and the tertiary payer field identified 68 additional WC discharges. Together, data from the two additional payer fields increased the count of discharges potentially billed to WC to 13,066, an increase of only 2.3 percent over the count based solely on the primary payer field.
Table 4 presents the distribution of payer categories based on all three payer fields for New York. Latinos were most likely to have only WC listed as a payer and were less likely to have other insurance listed in any payer field, with or without WC. More severe injuries were more likely to have other insurance listed in any payer field, with or without WC, and less likely to have only WC listed as a payer.
Table 4.
Payer Distribution (Percentages) for Industrial Injury Hospitalizations in New York, Using All Payer Fields (N = 19,894)
| Characteristic | Payer Categorya | p‐valueb | |||
|---|---|---|---|---|---|
| WC Only (N = 8,927) | WC and Other Insurance (N = 3,872) | Other Insurance Only (N = 4,734) | No Insurance (N = 2,361) | ||
| Overall | 44.9 | 19.5 | 23.8 | 11.9 | |
| Gender | |||||
| Male | 46.3 | 18.9 | 21.9 | 12.9 | <.001 |
| Female | 34.9 | 23.3 | 37.1 | 4.8 | |
| Age | |||||
| 16–24 | 49.2 | 13.2 | 19.8 | 17.8 | <.001 |
| 25–34 | 51.3 | 15.7 | 17.2 | 15.8 | |
| 35–44 | 48.0 | 19.0 | 20.2 | 12.9 | |
| 45–54 | 42.9 | 23.6 | 24.0 | 9.5 | |
| 55–64 | 40.8 | 25.5 | 27.2 | 6.5 | |
| 65 and older | 17.1 | 20.1 | 61.0 | 1.8 | |
| Race/ethnicity | |||||
| Non‐Latino White | 43.2 | 24.4 | 25.2 | 7.2 | <.001 |
| Latino/Hispanic | 51.6 | 10.2 | 20.8 | 17.4 | |
| Black/African‐American | 43.1 | 17.4 | 24.8 | 14.8 | |
| Asian/Pacific Islander | 41.3 | 11.4 | 28.1 | 19.2 | |
| Other/multiple | 45.2 | 14.7 | 19.5 | 20.6 | |
| Unknown/missing | 46.6 | 13.8 | 26.0 | 13.6 | |
| Injury severity | |||||
| Minor (AIS 1–2) | 46.3 | 18.6 | 22.7 | 12.4 | <.001 |
| Severe (AIS 3–6) | 38.7 | 23.0 | 28.6 | 9.8 | |
California and Colorado were excluded because only one payer field was available.
Payer categories are mutually exclusive; constructed from all three available payer fields.
Pearson's chi‐squared test of independence.
AIS, Abbreviated Injury Scale; WC, workers' compensation.
Lastly, we calculated total charges for identified industrial injury hospitalizations, by expected primary payer. In California, WC was billed for an estimated $103.9M (million) for industrial injury hospitalizations in 2009, Medicare for $11.0M, Medicaid for $15.1M, other governmental coverage for $10.3M, private insurance for $21.1M, and self‐pay/no charge accounted for $9.2M. In Colorado, WC was billed for an estimated $8.7M for industrial injury hospitalizations in 2009, Medicare for $1.0M, Medicaid for $0.1M, other governmental coverage for $0.7M, private insurance for $2.4M, and self‐pay/no charge accounted for $3.9M. In New York, WC was billed for an estimated $24.0M for industrial injury hospitalizations in 2009, Medicare for $3.5M, Medicaid for $3.2M, other governmental coverage for $0.2M, private insurance for $3.4M, and self‐pay/no charge accounted for $2.7M.
In these three states alone, we estimated that roughly $137M was billed to WC for identified industrial injury hospitalizations in 2009, whereas non‐WC payers were billed roughly $88M. Governmental programs were billed for about 51 percent of the charges not billed to WC, private insurance for about 30 percent, and self‐pay/no charge accounted for about 19 percent.
Discussion
We hypothesized that industrial injury hospitalizations were increasingly billed to non‐WC payers over time. In logistic regression models adjusted for gender, age, race/ethnicity, and injury severity, we found that there was a 3.6 percent average annual increase in the odds of an industrial injury not being billed to WC in California, and a 2.9 percent average annual increase in Colorado. However, contrary to our hypothesis, there was a 1.8 percent average annual decrease in the odds of an industrial injury not being billed to WC in New York. We cannot be certain what might be behind the variation in findings; however, there are significant differences between states in terms of changes to WC policy over time. According to a ProPublica report (Qiu and Grabell 2015), California and Colorado implemented several policies during the timeframe of this study that might restrict access to WC coverage, for example, expanded use of preexisting conditions to deny WC, expanded use of outside medical reviewers, or new exclusions of specific categories of workers. No similar policy changes were reported for New York or for Washington State during this timeframe. In an earlier Washington State study, we did not find an increase from 1998 through 2008 in the percentage of injuries covered by payers other than WC (Sears et al. 2013b). Washington State is also one of only four states with an exclusive state fund (no private WC insurance carriers). This highlights the role of state variation in WC policy, and it may explain some of the variance in findings of previous studies.
In general, patterns of association between characteristics and payer were quite similar across the three included states. Of particular note, older workers were much more likely to have their industrial injury hospitalizations billed to a non‐WC payer, primarily Medicare. Of industrial injury hospitalizations among workers aged 65 and over (Table 2), WC was billed for 30 percent in California, 38 percent in Colorado, and 37 percent in New York, whereas Medicare was billed for 57 percent in California, 43 percent in Colorado, and 49 percent in New York. This may signify potentially dramatic cost shifting of occupational injury costs from WC to Medicare. Older workers are the group most likely to have health insurance coverage as a potential alternative to WC. In New York, only 1.8 percent of industrial injury hospitalizations for workers aged 65+ had no insurance listed (Table 4), and 70 percent of that group had Medicare listed in at least one payer field regardless of whether WC was also listed. For workers with Medicare, there is no question that WC should be the expected primary payer for occupational injuries. According to Medicare.gov, “If you have Medicare and get injured on the job, workers' compensation pays first on health care items or services you got because of your work‐related illness or injury” (Centers for Medicare and Medicaid Services 2015). It is possible that some of these injuries were not truly occupational injuries. However, using Washington State trauma registry data linked to an accepted WC claim as the gold standard, we found that industrial place of occurrence was actually more specific for workers aged 65+ (99.0 percent) compared with those under 65 (97.8 percent) (unpublished data; data sources and procedures previously described, Sears et al. 2012b). This disparity between older and younger workers in the likelihood of WC billing deserves further attention to determine whether financial drivers are influencing billing decisions or if other factors are contributing.
Based on previous exploratory studies (Friedman and Forst 2008; Sears, Bowman, and Silverstein 2012a; Sears et al. 2013b), we expected that Latinos would be more likely than other groups to have WC listed as the expected payer, and less likely to have other insurance listed. In fact, that was the pattern we found. In New York (Table 4), Latinos were most likely to have only WC listed as a payer and were less likely to have other insurance listed in any payer field, with or without WC. Higher barriers to claim filing among more vulnerable populations might be expected to more heavily impact Latino workers (Azaroff et al. 2004; Scherzer, Rugulies, and Krause 2005). However, lower insurance rates for Latinos may provide a counterbalance. Hospitals are highly motivated to recoup costs and would perhaps be particularly motivated to ensure a WC claim was filed if no other payer was available. It is possible that Latinos more often had WC listed as expected payer simply due to their disproportionate lack of other insurance coverage.
In the logistic regression models for all three states, we found that more severe injuries had higher odds of not being billed to WC (not statistically significant for New York, but same direction of effect). A possible explanation can be found in Table 4, showing that more severe injuries were more likely to have other insurance listed as a payer, alone or in addition to WC. This comports with previous findings from Washington State (Sears et al. 2013b) and Ohio (Nahm, Patterson, and Vallier 2012). This pattern could be related to hospitals being more highly motivated to identify all potential payers for more severe (and presumably more costly) injuries. Hospitals have been under increasing financial pressures and are implementing creative reimbursement strategies, including increasingly intensive efforts to identify potential payers (Helling, Watkins, and Robb 1995; Cole, Flics, and Levine 1998; Mann et al. 2005; Barnes et al. 2008; Zarzaur, Croce, and Fabian 2012). Financial incentives can affect whether physicians classify conditions as work related for reimbursement purposes (Butler, Hartwig, and Gardner 1997). Older workers tend to have more severe and costly injuries, and our finding that they are also more likely to have those injuries billed to Medicare rather than WC may also play a role in producing the observed pattern.
This study adds to existing evidence that the employer‐funded WC system only partially covers the costs of work‐related traumatic injuries. Differential access to non‐WC health insurance coverage and adaptations by health care providers to changing economies and financial pressures affect trends in WC billing. The shift to value‐based reimbursement under the Affordable Care Act (ACA) may have an impact on billing trends, related to provider preference for the fee‐for‐service reimbursement used by most WC insurers. Depending on the state, WC may or may not provide the highest reimbursement rate. Growth in temporary work and contracted employment also affects population‐based penetration of WC coverage (Quinlan and Mayhew 1999; Azaroff et al. 2004). Collectively, these issues impact measurement of occupational injury incidence and trends, especially when using WC as a proxy for work relatedness.
Strengths and Limitations
To our knowledge, this was the first study to assess trends in expected payer for industrial injury hospitalizations over a timeframe of more than a few years and for more than one state. We used a highly specific, albeit insensitive, method of identifying industrial injuries (E849.3). We were careful to include only states with a history of consistent usage of the E849.X set of codes. Due to the extreme variation in usage of E849.X across states and even across years within individual states, it would be inappropriate in our view to use E849.3 to calculate rates and trends of industrial injuries for most states or nationally, as was done in at least one study (Fontcha et al. 2015). Despite being able to identify only three eligible states, California, Colorado, and New York happen to be large diverse states, and together represent about 20 percent of the U.S. population according to 2014 Census estimates. Most of the observed associations between characteristics and expected payer were similar across the three states, lending robustness to the findings.
Most work‐related injuries do not require hospitalization, and thus the use of SID data imposes an important limitation on generalizability; however, hospitalized injuries do represent the most serious subset aside from fatalities. Our findings do not generalize beyond occupational injuries due to study inclusion criteria, but they are conservative in the sense that occupational illnesses are less often recognized as work related. It would have been useful to be able to control for health insurance status in the regression models, but that approach was not feasible based on the available billing data. We cannot be certain that workers having no insurance listed in addition to WC actually had no such insurance, as identifying WC as primary expected payer may have effectively displaced recording of other potential payers. The extent of cost shifting and its relationship to insurance status is an area that warrants further research. Two of the three states only had one payer field available, which increases the chance of undercounting hospitalizations billed to WC and limits the ability to observe patterns for multiple payers. However, in New York, using all three available payer fields increased the count of discharges potentially billed to WC by only 2.3 percent over the count based solely on the primary payer field.
Our estimates of charges for work‐related industrial injury hospitalizations must be considered underestimates, as our identification method was restricted to the subset of cases that occurred in an industrial location, and that had a place of occurrence specified. In addition, charges are not a direct reflection of actual costs or payments.
Conclusions
This study assessed trends in expected payer for industrial injury hospitalizations in three states for up to 12 years. In California and Colorado, we found a significant increase over time in the odds of an industrial injury not being billed to WC. In New York, we found a significant decrease, and in a previous Washington State study, found no significant trend. These states have had markedly different histories with regard to WC policy, which could in part account for these differences. This study adds to limited but mounting evidence that, in at least some states, the relative burden on non‐WC payers to cover health care for industrial injuries is growing, even while direct WC‐related costs to employers are decreasing. For the United States as a whole, both WC benefits and WC costs as a percentage of payroll were lower in 2009 than they were in 1998 (Burton 2015). In particular, the payer distribution we observed for older workers suggests that there may be potentially dramatic cost shifting of industrial injury costs from WC to Medicare. This state of affairs may further deteriorate as the working population ages and more workers continue working past age 65. Payer and insurance coverage have implications beyond reimbursement and cost shifting; for example, patients with no identified payer have the highest odds of death (Weygandt et al. 2012). Workers who do not have accepted WC claims do not have access to compensation for time lost from work due to the injury, and those who are permanently disabled may ultimately rely on governmental programs such as Social Security Disability Insurance instead of WC pensions (Franklin et al. 2015). There are critical occupational injury surveillance and research efforts that generally must rely on the expected payer data fields in health care databases to identify work‐related events—efforts that are hampered by the inability to identify all work‐related injuries. Using all‐payer claims data may provide an opportunity in the near future to study these trends, and the impact of the ACA on occupational injuries and WC billing also merits future research. This study reinforces the importance of developing more comprehensive methods to identify work‐related events in health care databases independently of payer. In the meantime, the place of occurrence E‐codes is underutilized but potentially highly useful to occupational injury surveillance and research efforts. Use of these codes (with placement below the first‐listed E‐code) should be encouraged by policy makers and data stewards within state health departments and hospital associations.
Supporting information
Appendix SA1: Author Matrix.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This work was funded in part by the National Institute for Occupational Safety and Health (NIOSH), grant number R21OH010307. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NIOSH.
Disclosures: None.
Disclaimers: None.
References
- Alamgir, H. , Koehoorn M., Ostry A., Tompa E., and Demers P.. 2006. “An Evaluation of Hospital Discharge Records as a Tool for Serious Work Related Injury Surveillance.” Occupational and Environmental Medicine 63 (4): 290–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Association for the Advancement of Automotive Medicine . 1990. The Abbreviated Injury Scale, 1990 Revision. Des Plaines, IL: AAAM. [Google Scholar]
- Azaroff, L. S. , Levenstein C., and Wegman D. H.. 2002. “Occupational Injury and Illness Surveillance: Conceptual Filters Explain Underreporting.” American Journal of Public Health 92 (9): 1421–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azaroff, L. S. , Lax M. B., Levenstein C., and Wegman D. H.. 2004. “Wounding the Messenger: The New Economy Makes Occupational Health Indicators Too Good to Be True.” International Journal of Health Services 34 (2): 271–303. [DOI] [PubMed] [Google Scholar]
- Baker, S. P. , O'Neill B., Haddon W. Jr, and Long W. B.. 1974. “The Injury Severity Score: A Method for Describing Patients with Multiple Injuries and Evaluating Emergency Care.” Journal of Trauma 14 (3): 187–96. [PubMed] [Google Scholar]
- Barnes, S. L. , Robinson B. R., Richards J. T., Zimmerman C. E., Pritts T. A., Tsuei B. J., Butler K. L., Muskat P. C., Davis K. Jr, and Johannigman J. A.. 2008. “The Devil is in the Details: Maximizing Revenue for Daily Trauma Care.” Surgery 144 (4): 670–5; discussion 75‐6. [DOI] [PubMed] [Google Scholar]
- Burton Jr, F. 2015. Workers' Compensation Resources Research Report, Issue 9. Princeton, NJ: Workers' Disability Income Systems, Inc. [Google Scholar]
- Butler, R. J. , Hartwig R. P., and Gardner H.. 1997. “HMOs, Moral Hazard and Cost Shifting in Workers' Compensation.” Journal of Health Economics 16 (2): 191–206. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services . 2015. “Which Insurance Pays First” [accessed on July 11, 2015]. Available at http://www.medicare.gov/supplement-other-insurance/how-medicare-works-with-other-insurance/who-pays-first/which-insurance-pays.html#collapse-2507
- Clark, D. E. , Osler T. M., and Hahn D. R.. 2010. “ICDPIC: Stata Module to Provide Methods for Translating International Classification of Diseases (Ninth Revision) Diagnosis Codes into Standard Injury Categories and/or Scores” [accessed on March 2, 2012, 2010]. Available at http://ideas.repec.org/c/boc/bocode/s457028.html
- Cole, B. J. , Flics S., and Levine D. B.. 1998. “Optimizing Hospital Reimbursement Through Physician Awareness: A Step Toward Better Patient Care.” Orthopedics 21 (1): 79–83. [DOI] [PubMed] [Google Scholar]
- Council of State and Territorial Epidemiologists (CSTE) . 2015. “Occupational Health Indicators: A Guide for Tracking Occupational Health Conditions and Their Determinants” [accessed on July 9, 2015]. Available at http://www.cste.org/resource/resmgr/PDFs/2015_Ed_of_OHI_Guidance_Manu.pdf
- Cryer, C. , and Langley J.. 2008. “Developing Indicators of Injury Incidence that Can Be Used to Monitor Global, Regional and Local Trends” [accessed on May 2, 2014]. Available at http://ipru3.otago.ac.nz/ipru/ReportsPDFs/OR070.pdf
- Dong, X. , Ringen K., Men Y., and Fujimoto A.. 2007. “Medical Costs and Sources of Payment for Work‐Related Injuries Among Hispanic Construction Workers.” Journal of Occupational and Environmental Medicine 49 (12): 1367–75. [DOI] [PubMed] [Google Scholar]
- Fan, Z. J. , Bonauto D. K., Foley M. P., and Silverstein B. A.. 2006. “Underreporting of Work‐Related Injury or Illness to Workers' Compensation: Individual and Industry Factors.” Journal of Occupational and Environmental Medicine 48 (9): 914–22. [DOI] [PubMed] [Google Scholar]
- Fontcha, D. S. , Spooner K., Salemi J. L., Naik E., Aliyu M. H., Mogos M. F., Zoorob R., and Salihu H. M.. 2015. “Industry‐Related Injuries in the United States from 1998 to 2011: Characteristics, Trends, and Associated Health Care Costs.” Journal of Occupational and Environmental Medicine 57 (7): 814–26. [DOI] [PubMed] [Google Scholar]
- Fox, S. , Dembe A. E., Lawthers A., and Himmelstein J.. 2004. “Access to Quality Workers' Compensation Medical Care” In The Future of Workers' Compensation: Opportunities and Challenges, edited by Victor R., pp. 19–42. Cambridge, MA: Workers Compensation Research Institute. [Google Scholar]
- Franklin, G. , Wickizer T., Coe N., and Fulton‐Kehoe D.. 2015. “Workers Compensation: Poor Quality Health Care and the Growing Disability Problem in the United States.” American Journal of Industrial Medicine 58 (3): 245–51. [DOI] [PubMed] [Google Scholar]
- Friedman, L. S. , and Forst L.. 2007. “The Impact of OSHA Recordkeeping Regulation Changes on Occupational Injury and Illness Trends in the US: A Time‐Series Analysis.” Occupational and Environmental Medicine 64 (7): 454–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman, L. S. , and Forst L.. 2008. “Ethnic Disparities in Traumatic Occupational Injury.” Journal of Occupational and Environmental Medicine 50 (3): 350–8. [DOI] [PubMed] [Google Scholar]
- Groenewold, M. R. , and Baron S. L.. 2013. “The Proportion of Work‐Related Emergency Department Visits not Expected to Be Paid by Workers' Compensation: Implications for Occupational Health Surveillance, Research, Policy, and Health Equity.” Health Services Research 48 (6): 1939–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harwood, P. J. , Giannoudis P. V., Probst C., Van Griensven M., Krettek C., and Pape H. C.. 2006. “Which AIS Based Scoring System Is the Best Predictor of Outcome in Orthopaedic Blunt Trauma Patients?” Journal of Trauma 60 (2): 334–40. [DOI] [PubMed] [Google Scholar]
- HCUP State Inpatient Databases (SID) . 1998. ‐2009. Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research and Quality (AHRQ). [PubMed] [Google Scholar]
- Heaton, P. 2012. The Impact of Health Care Reform on Workers' Compensation Medical Care: Evidence from Massachusetts. Santa Monica, CA: RAND Corporation. [PMC free article] [PubMed] [Google Scholar]
- Helling, T. S. , Watkins M., and Robb C. V.. 1995. “Improvement in Cost Recovery at an Urban Level I Trauma Center.” Journal of Trauma 39 (5): 980–3. [DOI] [PubMed] [Google Scholar]
- Kilgo, P. D. , Osler T. M., and Meredith W.. 2003. “The Worst Injury Predicts Mortality Outcome the Best: Rethinking the Role of Multiple Injuries in Trauma Outcome Scoring.” Journal of Trauma 55 (4): 599–606; discussion 06‐7. [DOI] [PubMed] [Google Scholar]
- Leigh, J. P. 2011. “Economic Burden of Occupational Injury and Illness in the United States.” Milbank Quarterly 89 (4): 728–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipscomb, H. J. , Dement J. M., Silverstein B., Kucera K. L., and Cameron W.. 2009. “Health Care Utilization for Musculoskeletal Back Disorders, Washington State Union Carpenters, 1989‐2003.” Journal of Occupational and Environmental Medicine 51 (5): 604–11. [DOI] [PubMed] [Google Scholar]
- Mann, N. C. , Mackenzie E., Teitelbaum S. D., Wright D., and Anderson C.. 2005. “Trauma System Structure and Viability in the Current Healthcare Environment: A State‐by‐State Assessment.” Journal of Trauma 58 (1): 136–47. [DOI] [PubMed] [Google Scholar]
- Meredith, J. W. , Evans G., Kilgo P. D., MacKenzie E., Osler T., McGwin G., Cohn S., Esposito T., Gennarelli T., Hawkins M., Lucas C., Mock C., Rotondo M., Rue L., and Champion H. R.. 2002. “A Comparison of the Abilities of Nine Scoring Algorithms in Predicting Mortality.” Journal of Trauma 53 (4): 621–8; discussion 28‐9. [DOI] [PubMed] [Google Scholar]
- Morse, T. , Dillon C., and Warren N.. 2000. “Reporting of Work‐Related Musculoskeletal Disorders (MSD) to Workers' Compensation.” New Solutions 10 (3): 281–92. [DOI] [PubMed] [Google Scholar]
- Morse, T. , Dillon C., Warren N., Hall C., and Hovey D.. 2001. “Capture‐Recapture Estimation of Unreported Work‐Related Musculoskeletal Disorders in Connecticut.” American Journal of Industrial Medicine 39 (6): 636–42. [DOI] [PubMed] [Google Scholar]
- Morse, T. , Dillon C., Kenta‐Bibi E., Weber J., Diva U., Warren N., and Grey M.. 2005. “Trends in Work‐Related Musculoskeletal Disorder Reports by Year, Type, and Industrial Sector: A Capture‐Recapture Analysis.” American Journal of Industrial Medicine 48 (1): 40–9. [DOI] [PubMed] [Google Scholar]
- Murphy, P. L. , Sorock G. S., Courtney T. K., Webster B. S., and Leamon T. B.. 1996. “Injury and Illness in the American Workplace: A Comparison of Data Sources.” American Journal of Industrial Medicine 30 (2): 130–41. [DOI] [PubMed] [Google Scholar]
- Nahm, N. J. , Patterson B. M., and Vallier H. A.. 2012. “The Impact of Injury Severity and Transfer Status on Reimbursement for Care of Femur Fractures.” Journal of Trauma and Acute Care Surgery 73 (4): 957–65. [DOI] [PubMed] [Google Scholar]
- National Trauma Data Bank . 2011. “National Trauma Data Standard: Data Dictionary. 2012 Admissions” [accessed on August 27, 2012, 2011]. Available at http://www.ntdsdictionary.org/dataElements/documents/NTDS2012_xsd.PDF
- Nicholson, V. J. , Bunn T. L., and Costich J. F.. 2008. “Disparities in Work‐Related Injuries Associated with Worker Compensation Coverage Status.” American Journal of Industrial Medicine 51 (6): 393–8. [DOI] [PubMed] [Google Scholar]
- Osler, T. , Baker S. P., and Long W.. 1997. “A Modification of the Injury Severity Score That Both Improves Accuracy and Simplifies Scoring.” Journal of Trauma 43 (6): 922–5; discussion 25‐6. [DOI] [PubMed] [Google Scholar]
- Qiu, Y. , and Grabell M.. 2015. “Workers' Compensation Reforms by State” [accessed on July 11, 2015]. Available at http://projects.propublica.org/graphics/workers-comp-reform-by-state?state=undefined
- Quinlan, M. , and Mayhew C.. 1999. “Precarious Employment and Workers' Compensation.” International Journal of Law and Psychiatry 22 (5–6): 491–520. [DOI] [PubMed] [Google Scholar]
- Rosenman, K. D. , Gardiner J. C., Wang J., Biddle J., Hogan A., Reilly M. J., Roberts K., and Welch E.. 2000. “Why Most Workers with Occupational Repetitive Trauma Do Not File for Workers' Compensation.” Journal of Occupational and Environmental Medicine 42 (1): 25–34. [DOI] [PubMed] [Google Scholar]
- Rosenman, K. D. , Kalush A., Reilly M. J., Gardiner J. C., Reeves M., and Luo Z.. 2006. “How Much Work‐Related Injury and Illness Is Missed by the Current National Surveillance System?” Journal of Occupational and Environmental Medicine 48 (4): 357–65. [DOI] [PubMed] [Google Scholar]
- Ruestow, P. S. , and Friedman L. S.. 2013. “Characterizing the Relationship Between in‐Hospital Measures and Workers' Compensation Outcomes among Severely Injured Construction Workers Using a Data Linkage Strategy.” American Journal of Industrial Medicine 56 (10): 1149–56. [DOI] [PubMed] [Google Scholar]
- Scherzer, T. , Rugulies R., and Krause N.. 2005. “Work‐Related Pain and Injury and Barriers to Workers' Compensation among Las Vegas Hotel Room Cleaners.” American Journal of Public Health 95 (3): 483–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sears, J. M. , Bowman S. M., and Silverstein B. A.. 2012a. “Trends in the Disproportionate Burden of Work‐Related Traumatic Injuries Sustained by Latinos.” Journal of Occupational and Environmental Medicine 54 (10): 1239–45. [DOI] [PubMed] [Google Scholar]
- Sears, J. M. , Bowman S. M., Silverstein B. A., and Adams D.. 2012b. “Identification of Work‐Related Injuries in a State Trauma Registry.” Journal of Occupational and Environmental Medicine 54 (3): 356–62. [DOI] [PubMed] [Google Scholar]
- Sears, J. M. , Blanar L., Bowman S. M., Adams D., and Silverstein B. A.. 2013a. “Predicting Work‐Related Disability and Medical Cost Outcomes: Estimating Injury Severity Scores from Workers' Compensation Data.” Journal of Occupational Rehabilitation 23 (1): 19–31. [DOI] [PubMed] [Google Scholar]
- Sears, J. M. , Bowman S. M., Adams D., and Silverstein B. A.. 2013b. “Who Pays for Work‐Related Traumatic Injuries? Payer Distribution in Washington State by Ethnicity, Injury Severity, and Year (1998‐2008).” American Journal of Industrial Medicine 56 (7): 742–54. [DOI] [PubMed] [Google Scholar]
- Sengupta, I. , Reno V., and Burton J. F. Jr. 2011. Workers' Compensation: Benefits, Coverage, and Costs, 2009. Washington, DC: National Academy of Social Insurance. [Google Scholar]
- Shannon, H. S. , and Lowe G. S.. 2002. “How Many Injured Workers Do Not File Claims for Workers' Compensation Benefits?” American Journal of Industrial Medicine 42 (6): 467–73. [DOI] [PubMed] [Google Scholar]
- Smith, G. S. , Veazie M. A., and Benjamin K. L.. 2005. “The Use of Sentinel Injury Deaths to Evaluate the Quality of Multiple Source Reporting for Occupational Injuries.” Annals of Epidemiology 15 (3): 219–27. [DOI] [PubMed] [Google Scholar]
- Sorock, G. S. , Smith E., and Hall N.. 1993. “An Evaluation of New Jersey's Hospital Discharge Database for Surveillance of Severe Occupational Injuries.” American Journal of Industrial Medicine 23 (3): 427–37. [DOI] [PubMed] [Google Scholar]
- STIPDA: Injury Surveillance Workgroup 6 . 2008. Assessing an Expanded Definition for Injuries in Hospital Discharge Data Systems. Atlanta, GA: State and Territorial Injury Prevention Directors Association. [Google Scholar]
- Weygandt, P. L. , Losonczy L. I., Schneider E. B., Kisat M. T., Licatino L. K., Cornwell E. E. III, Haut E. R., Efron D. T., and Haider A. H.. 2012. “Disparities in Mortality after Blunt Injury: Does Insurance Type Matter?” Journal of Surgical Research 177 (2): 288–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarzaur, B. L. , Croce M. A., and Fabian T. C.. 2012. “Play or Pay: A Financial Model for Trauma Care in a Regional Trauma System.” Journal of Trauma and Acute Care Surgery 72 (1): 78–83; discussion 83‐5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.


