Abstract
Purpose
T2 magnetic resonance imaging (MRI) is recommended as the imaging modality for image-guided brachytherapy. In locally advanced cervical carcinoma, combined endocavitary and interstitial applicators are appropriate (Vienna or Utrecht). To cover extensive disease, Template Benidorm (TB) was developed. Treatment planning system applicator libraries are currently unavailable for the Utrecht applicator or the TB. The purpose of this work is to develop an applicator library for both applicators.
Material and methods
The library developed in this work has been used in the Oncentra Brachytherapy TPS, version 4.3.0, which has a brachytherapy module that includes a library of rigid applicators. To add the needles of the Utrecht applicator and to model the TB, we used FreeCAD and MeshLab. The reconstruction process was based on the points that the rigid section and the interstitial part have in common. This, together with the free length, allowed us to ascertain the position of the tip.
Results
In case of the Utrecht applicator, one of the sources of uncertainty in the reconstruction was determining the distance of the tip of needle from the ovoid. In case of the TB, the large number of needles involved made their identification time consuming. The developed library resolved both issues.
Conclusions
The developed library for the Utrecht and TB is feasible and efficient improving accuracy. It allows all the required treatment planning to proceed using just a T2 MRI sequence. The additional use of specific free available software applications makes it possible to add this information to the already existing library of the Oncentra Brachytherapy TPS. Specific details not included on this manuscript will be available under request. This library is also currently being implemented also into the Sagiplan v 2.0 TPS.
Keywords: brachytherapy, catheter reconstruction, gynecology, interstitial implants, clinical dosimetry
Purpose
For cervical cancers, T2 magnetic resonance imaging (MRI) is the preferred image modality for image guided brachytherapy [1, 2, 3, 4, 5, 6, 7, 8, 9, 10]. Traditionally, cervical cancer has been treated using only endocavitary applicators, i.e., uterine tandem plus ovoids/colpostats, or ring. Magnetic resonance imaging-guided brachytherapy has revealed the clinical target volume (CTV) coverage limits of these intracavitary applicators. In response, new applicators with interstitial components as well as the basic intracavitary applicator have been developed, e.g., the Vienna applicator (Nucletron, an Elekta company, Elekta AB, Stockholm, Sweden) [11], which uses plastic needles around the ring or the Utrecht applicator (Nucletron, an Elekta company, Elekta AB, Stockholm, Sweden) [12] with plastic needles on the ovoids.
For locally advanced cervical carcinoma with moderate extension to the parametrium, combined endocavitary and interstitial applicators are appropriate. Nevertheless, they cannot cover extensive disease affecting the distal vagina and/or parametrium. In these cases, interstitial treatments are recommended [6, 13, 14, 15, 16, 17, 18]. For instance, our institution has developed Template Benidorm (TB), a new combined endocavitary and interstitial applicator that is totally compatible with MRI [17]. Template Benidorm makes it possible to combine intracavitary brachytherapy with MRI-compatible transperineal interstitial needles. So, in our department, the Utrecht applicator or TB are selected depending on the lateral or vaginal extension of the disease.
Treatment planning based exclusively on MRI is preferred to other traditionally employed image modalities [10]. Thus, the exclusive use of MRI for planning reduces reconstruction uncertainty, saving time, and increasing patient comfort.
Groupe Européen de Curiethérapie and European Society for Radiotherapy and Oncology (GEC-ESTRO) has published recommendations for commissioning and applicator reconstruction in MRI based treatment planning for cervix cancer brachytherapy [10], and contrasted the reconstruction issues involved with the use of MRI or computed tomography (CT). While the source channel is well visualized in CT images, applicator reconstruction is more challenging when using MRI images. Availability of commercial dummy sources for MRI is limited, and image artifacts may occur with titanium applicators.
One of the most important recent advances in the TPS (Nucletron, an Elekta company, Elekta AB, Stockholm, Sweden) has been the availability of the applicator library. It allows whole applicator reconstruction based on just a few anchor points, improving the accuracy, and it overcomes the lack of adequate MRI dummies. However, to our knowledge, no such library is currently available with the interstitial components of the Utrecht and the TB. Moreover, in these cases, the final applicator configuration is implant specific, since the needle arrangement is necessarily patient dependent.
The purpose of this work is to present a method to add the specific interstitial component to an existing TPS rigid library for the Utrecht and TB templates, thereby allowing more efficient reconstruction using only T2 MRI-based planning.
Material and methods
Applicators, magnetic resonance imaging acquisition, and TPS
The Utrecht Interstitial CT/MRI Applicator Set (Nucletron, an Elekta company, Elekta AB, Stockholm, Sweden) has been specifically developed for combined intracavitary/interstitial treatment of gynecologic cancers [12]. Its design is based on the Fletcher CT/MRI Applicator Set (Nucletron, an Elekta company, Elekta AB, Stockholm, Sweden), and it uses the ovoids as a template for interstitial needle placement (up to 4 plastic needles in each). The insertion depth of the needles can be controlled using insertion tool. The final needle set-up is implant dependent in both trajectory and depth. However, although there are dummies for the endocavitary component, there are none for the interstitial one. Currently, the needle positions are reconstructed using their black tunnel signal on T2 MRI and their insertion depth.
The TB (Lorca Marin, Murcia, Spain) consists of a template to allocate multiple Titanium needles and a cylinder, uterine tandem [17, 18]. This template improves the existing MUPIT [14] template (Nucletron, an Elekta company, Elekta AB, Stockholm, Sweden) in that it implements both titanium needles and an intracavitary component, and is fully MRI compatible. The template consists of two perineal plates with two central holes that allow placement of a vaginal cylinder, available in different sizes to accommodate different vaginal lengths and intrauterine tubes of varying angles and lengths. Additionally, the plates are drilled with holes to introduce straight and angled titanium needles [18]. The plates have three dimples where three A-vitamin pellets are placed. These pellets produce a high signal in both T1 and T2 sequences and are used in the reconstruction process. The needles are reconstructed following their black tunnel signal and tip void. In T1 MRI, the positions can be determined properly but in T2, there is insufficient contrast [18]. Therefore, the depth of each needle must be obtained by measuring the free length with a ruler.
The MRI scans of the patients were acquired with a 1.5 T MRI imager (Optima MR 450w, software version DV24, GE Medical Systems, Milwaukee, Wisconsin, USA). An eight-channel phased array receiver coil was used following standard clinical MRI protocols. Following the GEC-ESTRO recommendations [6, 7, 8], the acquisition consisted of an axial T2 weighted fast recovery fast spin echo (FRFSE) sequence with the slice thickness reduced to 2 mm. This sequence was used for both delineation and reconstruction. Magnetic resonance imaging acquisition setting details have been described in a publication by Richart et al. [18].
The developed library has been implemented in the Oncentra Brachytherapy TPS, version 4.3.0, with a brachytherapy module that includes a library of rigid applicators. An independent program, the Library Manager Applicator (LMA), was used to add 3D models of the applicators to the Oncentra database.
Utrecht and Template Benidorm applicators implementation in the TPS library
In the Oncentra TPS (Nucletron, an Elekta company, Elekta AB, Stockholm, Sweden), the input files for the library application manager are a set of Extensible Markup Language (xml) files organized in a hierarchical structure. The main file has a rule.xml extension. In this main file, each applicator, with all its options, is configured for use in Oncentra. The blocks used in this file are separate files that include information about properties of channels, ovoids, etc. These blocks are divided in four kinds of files: tubes, ovoids, cylinders, and fixations. These files contain four subsections: 1) a description of the file, including the part ID and the type; 2) the set of anchor points; 3) the connectors used; 4) information about the surface of the element (called the cursive in Oncentra).
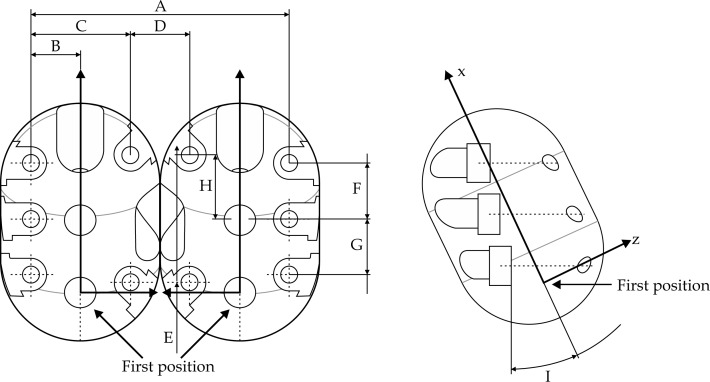
The Utrecht applicator
In this case, we started from a model provided by Elekta without the interstitial component. The first challenge was to determine distance from the surface of the ovoids of the output points of the needles. We used the technical information provided by Elekta to obtain the coordinates of the output points of the needles in the intrinsic reference system of the ovoids (Figure 1). To determine the coordinates in the reference system of the applicator, we had to find the required translation and a rotation. The translation is given by the tip position of each ovoid tube. To find the rotation, we obtained the plane of each of the ovoid tubes from the data in the file corresponding to the ovoid tube in the center curve section, using the minimum square method. After defining the planes, we had to match the x and z directions in both reference systems.
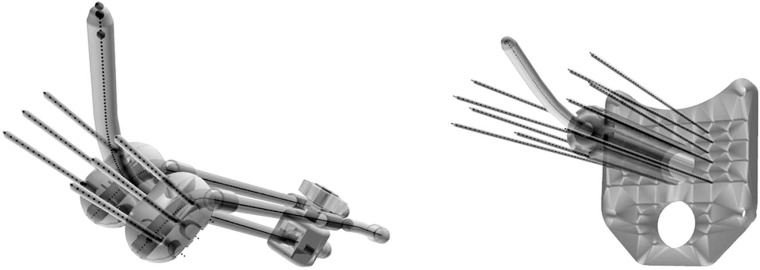
Fig. 1.
Intrinsic reference system of ovoid from technical data provided by Elekta
Once we had the output points, the next step was to create a file corresponding to each needle. A 3D model of each needle was created with FreeCAD (version 0.14, http://www.freecadweb.org/) and open parametric modeler software. By exporting this model to an Wavefront .obj file (obj) and processing it in Excel, we got the cursive section. The connector for the needle in this new file was also obtained using a FreeCAD model. The connectors defined in the ovoid tube file are the outputs points for the ovoid computed in the Utrecht applicator reference system.
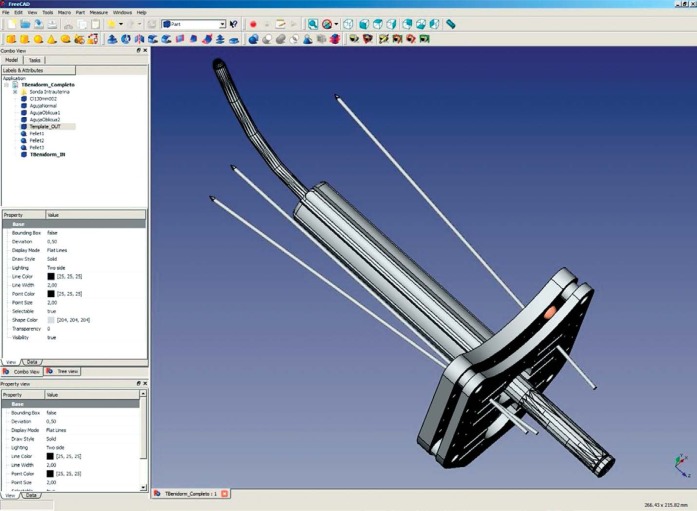
Template Benidorm
The modeling process for TB was different. Because only intrauterine tubes from the vaginal applicator set were included in the Oncentra data base, we had to use FreeCAD to create a new 3D model of the template. Using this program, we translated the real prototype to a vector file and modeled titanium needles, 4 cylinders (45 mm, 80 mm, 100 mm, and 135 mm), and the perineal plates with the A-vitamin pellets (Figure 2). This step gave us the necessary information regarding the skin of the applicator, and provided data we needed for the relative positions of all the parts that configured the applicator, so that the connectors could be created. With all this information, we created different files and their links using techniques described in previous sections.
Fig. 2.
Template Benidorm modeling using FreeCAD
Reconstruction procedure
For the Utrecht applicator, the MRI T2 reconstruction process was based on the points that the rigid section and the interstitial part have in common. First, the rigid part was reconstructed using the specific dummies that existed for the tandem and ovoids, which were clearly visible in T2 sequence, together with the cursive of the applicator. These have been described in a previous publication [19] and the dummies are currently provided to users by Elekta. These dummies consist of catheters filled with a saline and iodine mixture. Just water provides sufficient visibility, and the iodine colors the liquid to facilitate checking for bubbles. The distal end of the dummy corresponds with the maximum source-to-indexer distance of the high-dose-rate afterloader. The tip position of both ovoids and the tip position of the intrauterine tandem (MRI markers) are used as anchor points to locate the applicator. Small corrections to better fit the signal void and the MRI markers are made, using the indentations in the cursive of the ovoids and tandem. Unlike tandem and ovoids, this type of dummy is incompatible with plastic needles, due to their narrower diameter. Because the needles are not perfectly rigid, slight deviations in the modeled positions of the needle tips can be present. To account for this, small corrections can be made by rotating the needles at their exit points on the ovoids.
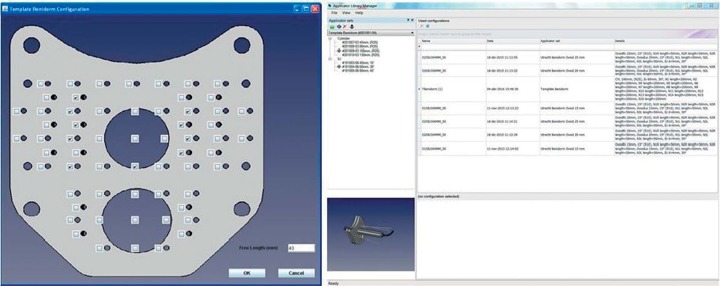
The correct modeling of the intracavitary component gives us the location of the needle output points; these are the exit points at the ovoid’s surface. Combining this information with the free length, enables us to know the complete needle position. In case of TB, once the choice of the needles was made, we entered the configuration of needles and the free length data into a home-made java application (Figure 3) to generate xml files and then imported them to the LMA from Oncentra. In the LMA, we chose the cylinder and the intrauterine components and then exported that information to Oncentra. After selecting the previously composed model, we located the three pellets in the image to determine the position of the applicator. As in the Utrecht case, we made some small corrections using the cursive data to improve the position of the cylinder and the intrauterine tandem, and verified these changes using the signal void data from the MRI image. Slight deviations from the modeled positions of the needles were corrected as described above with the aim of matching the theoretical position with the black signal on the MRI image. A good match is important because the position of tip of the needle is inter-related to the free-length data (Figure 4).
Fig. 3.
Home-made application produced using JAVA to generate Template Benidorm model (left) and library manager applicator screenshot (right)
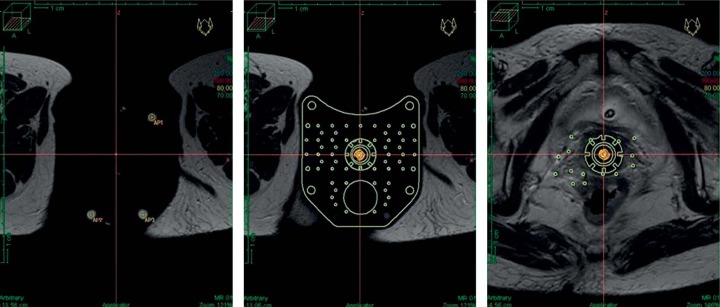
Fig. 4.
Illustration of the Template Benidorm plate alignment using the three A-vitamin pellets as anchor points (left and middle). On the right, the orientation of the needles is determined
Results
This library procedure has been applied in 25 patients. We have found that the generation of different needle arrangements can accommodate many clinical circumstances (number of needles, insertion depths, etc.). With the TB, as previously explained, a specific utility has been developed to manage various needle length values. Figure 5 shows both applicators after implementation in the Oncentra system. Figure 6 illustrates Utrecht and TB reconstruction on MR T2 images. This reconstruction procedure is very efficient, reducing uncertainty. Moreover, all reconstruction and planning is performed with a single T2 MRI sequence, which is the imaging modality recommended as optimal for contouring [6, 7, 8, 9].
Fig. 5.
Resulted rendering of Utrecht applicator (left) and Template Benidorm (right)
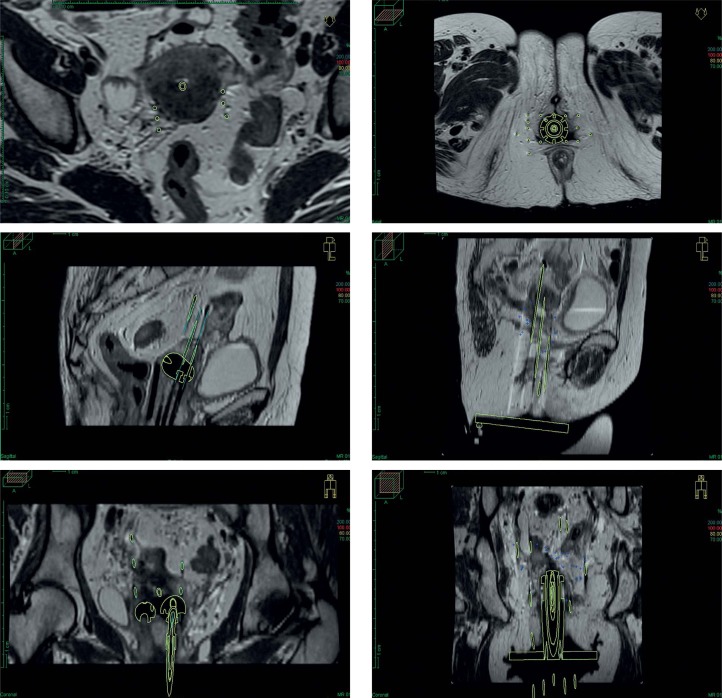
Fig. 6.
Three T2 magnetic resonance imaging views (transversal, sagittal, and coronal) with the applicator in place and with applicator mask superposed. Utrecht (left) and Template Benidorm (right)
Discussion
Traditionally, reconstruction methods based on applicator libraries are not used in cases involving interstitial components, because the whole applicator may not be considered rigid and the needle arrangement is patient dependent. However, we think that this option would be helpful in treatment planning procedures. Therefore, in this work, we present a method to include interstitial applicators in the Oncentra TPS library, and we describe a reconstruction method for planning purposes.
In case of the Utrecht applicator, the lack of dummies makes setting the needles challenging. Locating needle tips is essential to accurately determine the maximum source-to-indexer distance; however, the black line available on T2 MRI makes this determination very difficult. Prior to the development of the library presented in this work, we used the following procedure in Utrecht applicator reconstruction: 1) the positions of the catheters of the tandem and ovoid were determined from that of the existing saline dummy; 2) needles were reconstructed using the methodology described in Perez-Calatayud et al. [20]. Briefly, this consisted of using insertion depth information, i.e., the depth from the ovoid’s surface to the needle tip, provided by the radiation oncologist. Then a software ruler set to the insertion depth was placed on the reconstructed plane and used to define the different catheter points, including the needle tips. As was reported previously [20], the insertion depth reproduced using the software ruler, corresponds to the distance from the ovoid’s surface but with an offset of –0.7 cm, to account for the maximum source-to-indexer distance of 129 cm in the afterloader (microSelectron, version 2 or 3 from Elekta). This procedure is laborious and involves some amount of uncertainty in setting the exit point of the needle from the ovoid together with the assumption that the needle is perfectly straight.
In our opinion, the use of the library we have developed significantly improves efficiency. First, a virtual applicator can be selected according to the needle depths; the tandem and ovoids can be quickly set because the rigid applicator structure allows the use of dummies and applicator’s cursive. Once the ovoids are established, the needles exit points can be obtained and only slight corrections are needed to adjust their position according to their signal void at the tip boundaries.
To assess the improvement in accuracy, both reconstruction methods have been used in three different plans. One of the benefit of the new proposed method is evidenced with the more precise tip determination for both catheters, tandem, and ovoid, improving the 2-mm uncertainty due to the partial volume effect because the MRI slice thickness. In the case of needles, the proposed method reduces previous uncertainties of about 2 mm on the exit point from the ovoid, and up to 5 mm at needle tip. Larger deviations on needle tip determination are due to the assumption of perfectly straight needles. By using the developed library, it is also possible to blend the virtual needle to better fit curved trajectories of the real one.
In the case of the TB, which uses titanium needles, the reconstruction can usually be based on needle artifacts that can be seen in T1 MRI sequences, using the void at the tip as the needle tip position. Nevertheless, tissues surrounding the needles can present heterogeneities that complicate the accurate identification of these artifact patterns, and this difficulty is more pronounced in T2 sequences, which is the preferred sequence for contouring.
Before we had the library solution proposed here, we did TB reconstruction as previously described [18]. Briefly, this method is based on knowing the free needle lengths and the positions of typical MRI pellet markers. Template Benidorm uses three small A-vitamin pellets (which are hyper-intense on MRI images), compressed by both applicator plates to define the central plane of the plates’ arrangement. Typically, needles 20 cm in length are used. Two points are selected on each needle to define the straight line. From such line and the plane data, the intersection can be obtained. Then, using the free length (knowing the offset distance), the coordinates of the needle tips can be obtained. This method requires an external spreadsheet to compute the tip and plate needle coordinates to be introduced into the Oncentra TPS. Although this procedure is usable, identifying the positions of large numbers of needles is time consuming.
With the new method presented here, the time required to identify needle positions is greatly reduced, at least up to 50%. The virtual applicator with the required needle depth is selected in Oncentra and, using the three A-vitamin pellets as guides, is set on the MRI T2 image study. Then each needle orientation is set using just an axial plane image, in which the void at the tip of the titanium needle is clearly visible with good contrast. Typically, just two axial planes are sufficient to set all the needles.
The advantages of this approach for the TB are the time savings (we estimated it in at least around 50%, averaging the time benefice in different cases and different physicist) and the reduction of the probability of catheter misidentification, which can be an issue because of the large numbers of needles number typically used in clinical practice (minimum 14 needles).
The method proposed here is specific for the Oncentra TPS, and also the Elekta Utrecht and TB applicators. However, it can be adapted to other TPS and interstitial applicators taking into account their specific applicator library management. For example, this methodology is currently being developed also for the TPS Sagiplan (Eckert & Ziegler, Bebig, Germany). In Sagiplan, there is a set of pieces (called cursive), with which we compose the applicators (called cursive). Inside each cluster configuration, we obtain the relative position between all of pieces that conform that cluster. So, in an example of an applicator with an interstitial part, as Vienna applicator [11], with a 3D model with the output points of needles perfectly determined, we could configure a similar system as described above. There is a work in progress within this project.
Conclusions
The interstitial component library that has been developed for the Utrecht applicator and TB is feasible and efficient, saving time and improving accuracy. It allows all the required treatment planning (contouring, reconstruction, and optimization) to proceed using just a T2 MRI sequence. The additional use of specific free available software applications makes it possible to add this information to the already existing library of the Oncentra Brachytherapy TPS. Specific details not included on this manuscript will be available under request. This library is also currently being implemented also into the Sagiplan v 2.0 TPS (Eckert & Ziegler, BEBIG).
Acknowledgments
The current study was supported in part by Spanish Government under Project No. FIS2013-42156. Authors want to give special thanks to Franks Kuippers from Elekta for the technical details of the Utrecht applicators and Mr. David Carpenter for editorial assistance.
Disclosure
Authors report no conflict of interest.
References
- 1.Galalae R, Tharavichitkul E, Wanwilairat S, et al. University Cooperation Platform (UCP) between Christian-Albrechts- University Kiel (Germany) and Chiang Mai University (Thailand): implementation of image-guided gynecological brachytherapy. J Contemp Brachytherapy. 2015;7:86–92. doi: 10.5114/jcb.2015.49444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Okuma K, Yamashita H, Kobayashi R, et al. A study of high-dose-rate intracavitary brachytherapy boost for curative treatment of uterine cervical cancer. J Contemp Brachytherapy. 2015;7:128–134. doi: 10.5114/jcb.2015.50720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tan P, Koh V, Tang J. Outpatient combined intracavitary and interstitial cervical brachytherapy: barriers and solutions to implementation of a successful programme – a single institutional experience. J Contemp Brachytherapy. 2015;7:259–263. doi: 10.5114/jcb.2015.52625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bailleux C, Falk A, Chand-Fouche M, et al. Concomitant cervical and transperineal parametrial high-dose-rate brachytherapy boost for locally advanced cervical cancer. J Contemp Brachytherapy. 2016;8:23–31. doi: 10.5114/jcb.2016.57535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murakami N, Kobayashi K, Kato T, et al. The role of interstitial brachytherapy in the management of primary radiation therapy for uterine cervical cancer. J Contemp Brachytherapy. 2016;8:391–398. doi: 10.5114/jcb.2016.62938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Viswanathan A, Thomadsen B American Brachytherapy Society Cervical Cancer Recommendations Committee; American Brachytherapy Society. American Brachytherapy Society consensus guidelines for locally advanced carcinoma of the cervix. Part I: general principles. Brachytherapy. 2012;11:33–46. doi: 10.1016/j.brachy.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 7.Haie-Meder C, Pötter R, Van Limbergen E, et al. Gynaecological (GYN) GEC-ESTRO Working Group. Recommendations from Gynecological (GYN) GEC-ESTRO Working Group (I): concepts and terms in 3D image based 3D treatment planning in cervix cancer brachytherapy with emphasis on MRI assessment of GTV and CTV. Radiother Oncol. 2005;74:235–245. doi: 10.1016/j.radonc.2004.12.015. [DOI] [PubMed] [Google Scholar]
- 8.Pötter R, Haie-Meder C, Van Limbergen E, et al. GEC ESTRO Working Group. Recommendations from gynecological (GYN) GEC ESTRO working group (II): concepts and terms in 3D image-based treatment planning in cervix cancer brachytherapy-3D dose volume parameters and aspects of 3D image-based anatomy, radiation physics, radiobiology. Radiother Oncol. 2006;78:67–77. doi: 10.1016/j.radonc.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 9.Dimopoulos J, Petrow P, Tanderup K, et al. Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group (IV): Basis principles and parameters for MR imaging within the frame of image based adaptive cervix cancer brachytherapy. Radiother Oncol. 2012;103:113–122. doi: 10.1016/j.radonc.2011.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hellebust TP, Kirisits C, Berger D, et al. Gynaecological (GYN) GEC-ESTRO Working Group. Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group: considerations and pitfalls in commissioning and applicator reconstruction in 3D image-based treatment planning of cervix cancer brachytherapy. Radiother Oncol. 2010;96:153–160. doi: 10.1016/j.radonc.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 11.Kiristis C, Lang S, Dimopoulus J, et al. The Vienna applicator for combined intracavitary and interstitial brachytherapy of cervical cancer: design, application, treatment planning and dosimetric results. Int J Radiat Oncol Biol Phys. 2006;65:624–630. doi: 10.1016/j.ijrobp.2006.01.036. [DOI] [PubMed] [Google Scholar]
- 12.Nomden CN, de Leeuw AA, Moerland MA, et al. Clinical use of the Utrecht applicator for combined intracavitary/interstitial brachytherapy treatment in locally advanced cervical cancer. Int J Radiat Oncol Biol Phys. 2012;82:1424–1430. doi: 10.1016/j.ijrobp.2011.04.044. [DOI] [PubMed] [Google Scholar]
- 13.Nag S, Erickson B, Thomadsen B, et al. The American Brachytherapy society recommendations for high dose rate brachytherapy for carcinoma of the cervix. Int J Radiat Oncol Biol Phys. 2000;48:201–211. doi: 10.1016/s0360-3016(00)00497-1. [DOI] [PubMed] [Google Scholar]
- 14.Viswanathan A, Erickson B, Rownd J. Image guided approaches to interstitial brachytherapy. In: Viswanathan A, Kiristis C, Erickson B, Potter R, editors. Gynecologic radiation therapy: novel approaches to image-guidance and management. Berlin-Heidelberg: Springer; 2011. pp. 247–259. [Google Scholar]
- 15.Martinez A, Cox RS, Edmundson GK. A multiple-site perineal applicator (MUPIT) for treatment of prostatic, anorectal and gynecologic malignancies. Int J Radiat Oncol Biol Phys. 1984;10:297–305. doi: 10.1016/0360-3016(84)90016-6. [DOI] [PubMed] [Google Scholar]
- 16.Syed A, Puthawala AA, Neblett D, et al. Transperineal interstitial intracavitary “Syed-Neblett” applicator in the treatment of carcinoma of the uterine cervix. Endocuriether Hypertherm. 1986;2:1–13. [Google Scholar]
- 17.Rodríguez Villalba S, Richart Sancho J, Otal Palacin A, et al. A new template for MRI-based intracavitary/interstitial gynecologic brachytherapy: design and clinical implementation. J Contemp Brachytherapy. 2015;7:265–272. doi: 10.5114/jcb.2015.54051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Richart J, Otal A, Rodriguez S, et al. A practical MRI-based reconstruction method for a new endocavitary and interstitial gynaecological template. J Contemp Brachytherapy. 2015;5:407–414. doi: 10.5114/jcb.2015.55340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Perez-Calatayud J, Kuipers F, Ballester F, et al. Exclusive MRI- based tandem and colpostats reconstruction in gynaecological brachytherapy treatment planning. Radiother Oncol. 2009;91:181–186. doi: 10.1016/j.radonc.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 20.Perez-Calatayud J, Carmona V, Lliso F, et al. Utrecht applicator reconstruction in MRI-based cervix gynaecological brachytherapy. Radiother Oncol. 2011;99:S268. [Abstract] [Google Scholar]