ABSTRACT
Meningioma is typically considered to be a benign tumor. Malignant transformation and metastasis of meningiomas are rare. Moreover, most meningiomas are intracranial, and there are few reports on intraspinal meningiomas. This report aimed to describe the clinical features and pathological findings of a case of malignant transformation and distant metastasis of intraspinal meningioma, with a review of the literature. A 44-year-old man with a bilateral lower limb paresis was diagnosed with an intradural extramedullary tumor of the thoracic spine. Primary tumor resection was performed, and the histological findings revealed atypical meningioma. The meningioma recurred 2 years after the primary surgery, and a second resection was performed, but only partial resection was possible because of decreased motor evoked potential. At age 48, the patient’s lower limb weakness returned, and a third resection was performed, and the histological finding remained atypical meningioma. At age 54, the tumor increased and stereotactic irradiation was performed. At age 60, the patient was diagnosed with metastatic tumors of the rib, lumbar vertebra, cervical spine, and sacrum. Biopsy of the rib metastatic tumor was performed, and the histological findings revealed anaplastic meningioma. This case is the first report of an intraspinal meningioma that transformed from atypical to anaplastic meningioma with distant hematogenous metastasis.
Key Words: meningioma, intraspinal, malignant transformation, metastasis, atypical
INTRODUCTION
Meningioma is typically considered to be a benign tumor. Indeed, malignant meningioma represents only 6~10% of all cases.1, 2) Malignant transformation and metastasis are rare.3-5) Although metastasis of intracranial meningioma has been reported, there are few reports on the metastasis of intraspinal meningioma.6)
This report aimed to describe the clinical features and pathological findings of the case of malignant transformation and distant metastasis of intraspinal meningioma, with a review of the literature.
CASE PRESENTATION
A 44 year-old man with a bilateral lower limb paresis was diagnosed with an intradural extramedullary tumor at the thoracic spine. A T2-4 laminectomy with tumor resection and coagulation of the dural attachment were performed, and the histological findings revealed an atypical meningioma classified as WHO grade 2 (Fig. 1). Postoperatively, the lower limb paresis completely resolved, but at age 46, deteriorated again. Tumor resection was performed a second time, but complete removal was abandoned because of a fall in motor evoked potential during the surgery. At age 48, lower limb weakness occurred again. MRI revealed a T2-4 intradural tumor surrounding the spinal cord and enhanced by gadolinium (Fig. 2). The tumor was adherent to the spinal cord making it difficult to distinguish the spinal cord from the tumor microscopically. Subtotal tumor resection, resection of the dural attachment as possible, and a T1-6 posterolateral fusion were performed as a third surgery. The histological findings of the tumor remained atypical meningioma (Fig. 3). At age 54, the tumor increased, therefore, stereotactic irradiation was performed but not effective. At age 60, the patient suffered from thoracic pain and was diagnosed with metastatic tumors of the rib, lumbar vertebra, and sacrum. Moreover, the meningioma directly invaded and surrounded the thoracic spine (Fig. 4). Whole-body CT scan could not detect the primary tumor except the thoracic meningioma. Biopsy of the rib metastatic tumor was performed, and the histological finding revealed anaplastic meningioma classified as WHO grade 3 (Fig. 4). With this, the patient was diagnosed with malignant transformation and distant metastasis of an intraspinal meningioma. The patient died at age 61.
Fig. 1.
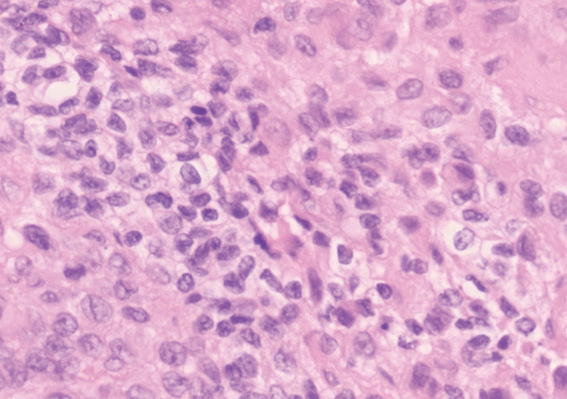
Histologic analyses. Hematoxylin-eosin, original magnification ×20.
Histological examination on the spinal cord tumor, showing sheet like growth, and cells with prominent nuclei diagnosed as Atypical meningioma (WHO grade 2).
Fig. 2.
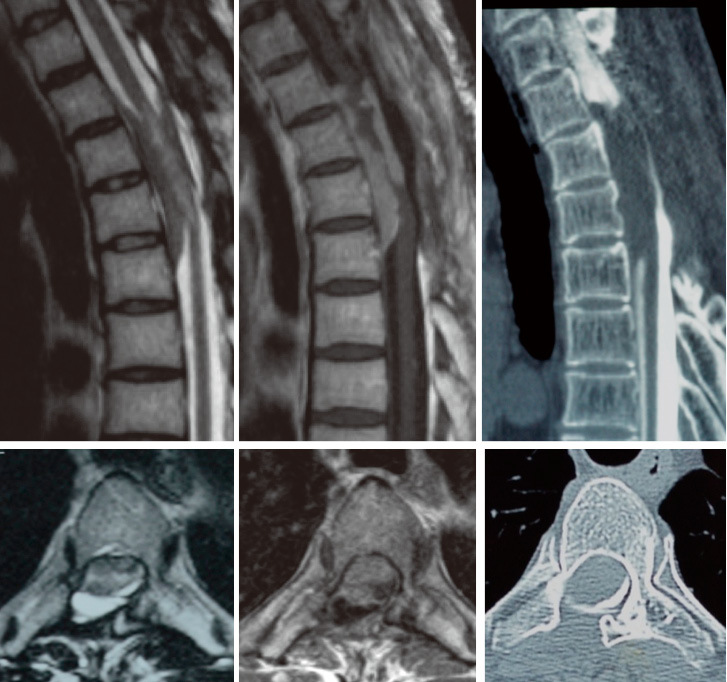
T2-weighted, T1-weighted gadolinium enhanced MRI, and CT myelogram.
Intradural-extramedullary tumor surrounded the spinal cord enhanced by gadolinium with no calcification and no invasion.
Fig. 3.
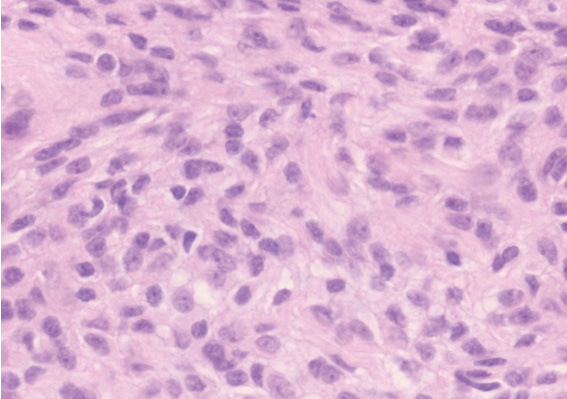
Histologic analyses. Hematoxylin-eosin, original magnification ×20.
Histological examination on the spinal cord tumor diagnosed as Atypical meningioma (WHO grade 2).
Fig. 4.
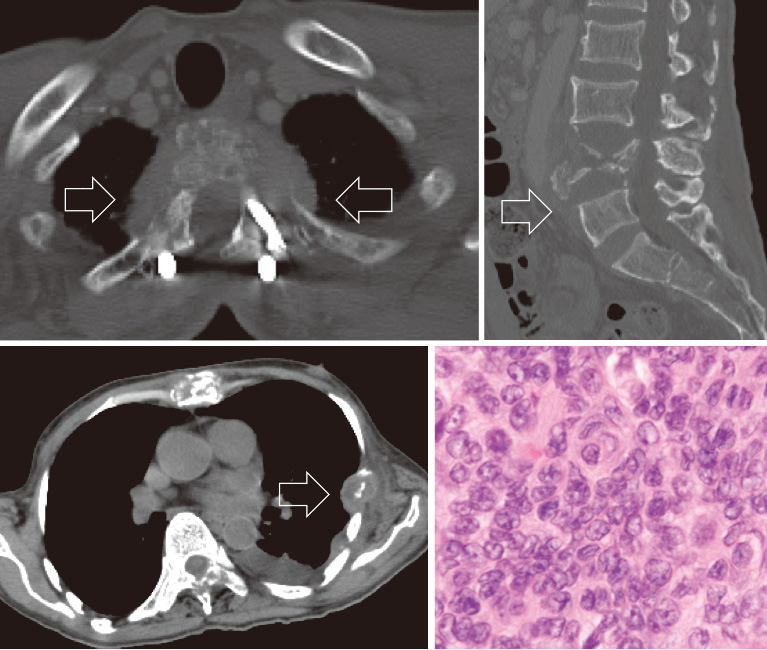
Tumor invaded and surrounded the thoracic spine and metastasized to the rib and the lumbar spine. Histological examination on the metastatic rib tumor, showing round cells with eccentric nuclei, eosinophilic cytoplasm, and focal necrosis diagnosed as anaplastic meningioma (WHO grade 3).
DISCUSSION
To the best of our knowledge, this is the first report of a case of intraspinal meningioma with malignant transformation and distant metastasis. The meningioma transformed from atypical to anaplastic meningioma over a span of 14 years. In this case, the thoracic intraspinal meningioma transformed into a malignancy and invaded directly around the thoracic spine. Finally, the direct invasion brought a hematogenous metastasis.
Distant metastases of meningioma
There have been several reports on distant metastases of intracranial meningioma.3, 7) Surov et al. thoroughly reviewed distant metastases of intracranial meningioma, including 115 cases with 165 metastatic lesions in their analysis.3) They found that the primary tumor of metastasized meningioma was, 33.9% for WHO grade 1, 20.9% for WHO grade 2, and 40% for WHO grade 3. The metastatic lesions included 37.2% in the lung, 16.5% in the bones, 15.2% intraspinal, and 9.2% in the liver.
In contrast, there has only been a single case report of distant metastases of intraspinal meningioma, and that case was originally graded as WHO grade 3, which was different from our case originally graded as WHO grade 2.6)
Malignant transformation of meningioma
Malignant transfomation of intracranial meningioma are rare, occurring in only 0.16–2.0% of cases, and the time to malignant transformation ranging from 8 months to 26 years.8-12) Factors that induce malignant transformation in intracranial meningioma include high-dose radiation,13) surgical stress,14) viral infection,15) growth factors such as VEGF,16) and numerous progression-associated alternations of chromosomes 1p, 6q, 9q, 10q, 14q, 17q, and 22q.9, 17) In our case, three times surgery and stereotactic irradiation was performed. However, it cannot conclude that these factors change the atypical intraspinal meningioma into malignant transformation.
Treatment to avoid recurrence of meningioma
To avoid recurrence, a macroscopically complete removal of tumor, with excision of its dural attachment or a macroscopically complete removal, with coagulation of its dural attachment are recommended.18) Reports have shown that the recurrence rate of subtotal resection is significantly higher than that of total resection.19-22) However, when evaluating recurrence, these reports have intermixed the tumor WHO grade.
The recurrence rate for intracranial atypical meningioma is eightfold higher than it is for WHO grade 1 meningioma.2) The mean recurrence-free survivals time was 66 months, and the recurrence-free rate was 92% at one year and 53% at five years. When meningioma involves and adheres to the spinal cord, as in our case, it is extremely difficult to achieve total gross resection of the meningioma without damage to the spinal cord. However, based on the aforementioned studies and the course of our case, total resection is recommended to avoid recurrence of atypical meningioma.
This report is the extremely rare case of intraspinal meningioma that transformed from WHO grade 2 to 3 with distant hematogenous metastasis. To avoid recurrence and malignant transformation of meningioma, gross total resection is likely required.
CONFLICTS OF INTEREST
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
REFERENCES
- 1).Goyal LK, Suh JH, Mohan DS, Prayson RA, Lee J, Barnett GH. Local control and overall survival in atypical meningioma: a retrospective study. Int J Radiat Oncol Biol Phys, 2000; 46: 57–61. [DOI] [PubMed]
- 2).Mawrin C, Perry A. Pathological classification and molecular genetics of meningiomas. J Neurooncol, 2010; 99: 379–391. [DOI] [PubMed]
- 3).Surov A, Gottschling S, Bolz J, Kornhuber M, Alfieri A, Holzhausen HJ, et al. Distant metastases in meningioma: an underestimated problem. J Neurooncol, 2013; 112: 323–327. [DOI] [PubMed]
- 4).Miller DC, Ojemann RG, Proppe KH, McGinnis BD, Grillo HC. Benign metastasizing meningioma. Case report. J Neurosurg, 1985; 62: 763–766. [DOI] [PubMed]
- 5).LeMay DR, Bucci MN, Farhat SM. Malignant transformation of recurrent meningioma with pulmonary metastases. Surg Neurol, 1989; 31: 365–368. [DOI] [PubMed]
- 6).Wang Z, Kong M, Li J, Xiao W, Zheng S. Intraspinal rhabdoid meningioma metastasis to the liver. J Clin Neurosci, 2011; 18: 714–716. [DOI] [PubMed]
- 7).Cachia D, Alderson L, Smith T, Yunus S. Widely metastatic meningioma. Arch Neurol, 2012; 69: 1372–1373. [DOI] [PubMed]
- 8).Jellinger K, Slowik F. Histological subtypes and prognostic problems in meningiomas. J Neurol, 1975; 208: 279–298. [DOI] [PubMed]
- 9).Lamszus K, Kluwe L, Matschke J, Meissner H, Laas R, Westphal M. Allelic losses at 1p, 9q, 10q, 14q, and 22q in the progression of aggressive meningiomas and undifferentiated meningeal sarcomas. Cancer Genet Cytogenet, 1999; 110: 103–110. [DOI] [PubMed]
- 10).Matsuno A, Fujimaki T, Sasaki T, Nagashima T, Ide T, Asai A, et al. Clinical and histopathological analysis of proliferative potentials of recurrent and non-recurrent meningiomas. Acta Neuropathol, 1996; 91: 504–510. [DOI] [PubMed]
- 11).Yamazaki Y, Kawano N, Suwa T, Ito H, Yada K, Kuwao S. [Recurrent meningioma with malignant transformation: a case which changed from meningothelial type to papillary type]. No Shinkei Geka, 1994; 22: 285–289. [PubMed]
- 12).Younis GA, Sawaya R, DeMonte F, Hess KR, Albrecht S, Bruner JM. Aggressive meningeal tumors: review of a series. J Neurosurg, 1995; 82: 17–27. [DOI] [PubMed]
- 13).Salvati M, Cervoni L, Puzzilli F, Bristot R, Delfini R, Gagliardi FM. High-dose radiation-induced meningiomas. Surg Neurol, 1997; 47: 435–441; discussion 441–432. [DOI] [PubMed]
- 14).Mesfin A, Ahn NU, Carrino JA, Sponseller PD. Ten-year clinical and imaging follow-up of dural ectasia in adults with Marfan syndrome. Spine J, 2013; 13: 62–67. [DOI] [PubMed]
- 15).Knirsch W, Kurtz C, Haffner N, Binz G, Heim P, Winkler P, et al. Dural ectasia in children with Marfan syndrome: a prospective, multicenter, patient-control study. Am J Med Genet A, 2006; 140: 775–781. [DOI] [PubMed]
- 16).Shono T, Inamura T, Torisu M, Suzuki SO, Fukui M. Vascular endothelial growth factor and malignant transformation of a meningioma: case report. Neurol Res, 2000; 22: 189–193. [DOI] [PubMed]
- 17).Arai H, Beppu T, Wada T, Yoshida Y, Kubo Y, Suzuki M, et al. Pathological analyses of early recurrence and malignant transformation in meningiomas. Brain Tumor Pathol, 1998; 15: 37–40. [DOI] [PubMed]
- 18).Simpson D. The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry, 1957; 20: 22–39. [DOI] [PMC free article] [PubMed]
- 19).Klekamp J, Samii M. Surgical results for spinal meningiomas. Surg Neurol, 1999; 52: 552–562. [DOI] [PubMed]
- 20).Roux FX, Nataf F, Pinaudeau M, Borne G, Devaux B, Meder JF. Intraspinal meningiomas: review of 54 cases with discussion of poor prognosis factors and modern therapeutic management. Surg Neurol, 1996; 46: 458–463; discussion 463–454. [DOI] [PubMed]
- 21).Solero CL, Fornari M, Giombini S, Lasio G, Oliveri G, Cimino C, et al. Spinal meningiomas: review of 174 operated cases. Neurosurgery, 1989; 25: 153–160. [PubMed]
- 22).Nakamura M, Tsuji O, Fujiyoshi K, Hosogane N, Watanabe K, Tsuji T, et al. Long-term surgical outcomes of spinal meningiomas. Spine (Phila Pa 1976), 2012; 37: E617–623. [DOI] [PubMed]


