Summary
Background
We performed a retrospective case-control study to assess the values of cardiac troponin I (cTnI) in a large number of patients admitted to the emergency department (ED) with different types of trauma.
Methods
The study population consisted of all patients aged 18 years or older admitted to the local ED with all types of traumas over a 1-year period. Results of cTnI were compared with those of 125 consecutive blood donors and 25 non-cardiac chest pain ED patients.
Results
The final study population consisted of 380 trauma patients, 10 with isolated abdominal trauma, 99 with isolated trauma of the limbs, 49 with isolated chest trauma, 145 with isolated head trauma and 77 with polytrauma. The concentration of cTnI did not differ among the three study populations, but the frequency of measurable values was substantially higher in patients with trauma (63%) than in blood donors and non-cardiac chest pain ED patients (both 20%). The frequency of cTnI values above the 99th percentile of the reference range was significantly higher in trauma patients (20%) than in blood donors (0%) and noncardiac chest pain ED patients (8%). Increased cTnI values were more frequent after head trauma (21%), chest trauma (27%) and polytrauma (29%) compared to patients with abdominal (0%) or limbs trauma (8%).
Conclusions
These results suggest that the measurement of cardiac troponin may be advisable to identify potential cardiac involvement in trauma patients, especially in those with polytrauma and head or chest trauma.
Keywords: trauma, polytrauma, injury, cardiac biomarkers, troponin
Kratak sadržaj
Uvod
Ovu retrospektivnu anamnestičku studiju sproveli smo u cilju određivanja vrednosti srčanog troponina I (cTnI) kod velikog broja pacijenata primljenih na odeljenje urgentne medicine sa različitim vrstama trauma.
Metode
Populacija u ovoj studiji sastojala se od pacijenata starih 18 godina ili više sa svim vrstama trauma koji su primljeni na lokalno odeljenje hitne službe tokom perioda od godinu dana. Rezultati cTnI upoređeni su sa rezultatima 125 uzastopnih davalaca krvi i 25 pacijenata sa bolom u grudima koji nije bio srčanog porekla sa odeljenja hitne službe.
Rezultati
Konačnu populaciju u ovoj studiji činilo je 380 pacijenata sa traumama, 10 sa izolovanim povredama abdomena, 99 sa izolovanim povredama udova, 49 sa izolovanim povredama grudnog koša, 145 sa izolovanim povredama glave i 77 sa politraumom. Koncentracija cTnI nije se razlikovala između tri populacije u studiji, ali je učestalost merljivih vrednosti bila značajno veća kod pacijenata sa traumom (63%) nego kod davalaca krvi i bolesnika sa odeljenja za hitnu pomoć koji su imali bol u grudima koji nije bio srčanog porekla (oba po 20%). Učestalost vrednosti cTnI iznad 99-og percentila u referentnom opsegu bila je značajno veća kod pacijenata sa traumama (20%) nego kod davalaca krvi (0%) i pacijenata sa odeljenja hitne službe sa bolom u grudima nesrčanog porekla (8%). Povišene vrednosti cTnI bile su češće posle povreda glave (21%), povreda grudnog koša (27%) i politraume (29%) u poređenju s pacijentima sa povredama abdomena (0%) ili udova (8%).
Zaključak
Ovi rezultati pokazuju da bi se merenje srčanog troponina moglo savetovati radi identifikovanja potencijalnog učešća srca kod pacijenata sa traumama, naročito kod onih sa politraumom ili povredama glave ili grudi.
Introduction
Trauma injuries fulfill the typical disease classification criteria for a global pandemic, since their frequency is high and they are associated with substantial morbidity and mortality over time and across all continents. Overall, deaths from injury have been estimated at 5.1 million per year in the 1990 worldwide, and this epidemiological burden is expected to increase further to 8.4 million in the next five years, thus becoming the second cause of disability-adjusted life years (DALYs) lost (1). The most recent statistics of the US National Trauma Institute attests that trauma accounts for as many as 41 million emergency department (ED) visits and 2.3 million hospital admissions across the US each year (2). Even more importantly, trauma injuries account for up to 30% of all life years lost and pose a dramatic economic burden to the health care system, estimated at approximately $585 billions per year (including costs related to health care expenditure and lost productivity). Although the true incidence of fatal traumas can be hardly established and is reportedly heterogeneous around the globe depending on local efficiency of care, epidemiological studies indicate that fatal traumas have an approximate incidence of 10 per 100,000 inhabitants, increasing to 17 per 100,000 after the age of 55 (3). A large survey assessing prehospitalization and in-hospital trauma deaths recorded at a single level I trauma center (4) recently attested that the leading causes of traumas were motor vehicle accidents (72%), gunshots (8%), stabs (6%) and falls (4%). Overall, the vast majority of patients (i.e., 66%) had already died during the pre-hospital phase, 27% died after <48 hours in hospital, 5% died after 3–7 days in hospital, whereas 2% died after >7 days in hospital. As regards the mechanisms, traumas to central nervous system (CNS; 33%), exsanguination (33%), both CNS trauma and exsanguination (17%), and airway compromise (8%) were the more frequent reasons of death.
Irrespective of the relatively high frequency in the general population, traumas are one of the leading conditions managed in the ED, thus posing considerable clinical and organizational issues to this vital health care setting. The US Centers for Disease Control and Prevention (CDC) currently estimates that as many as 40.2 million visits per year in the ED are injury-related out of a total 136.3 million visits (i.e., ~30% of all visits) (5). In an epidemiological study carried out at an urban level I trauma center, trauma represented 1,036 of overall 4,246 ED visits (i.e., 24.4%) (6). Due to this important epidemiological evidence, a deepened understanding of the precise factors that may influence acute care and prognosis of trauma patients is clinically and economically valuable. Cardiac troponins are now regarded as the most sensitive and specific biomarkers for the diagnosis of myocardial injury, since these biomarkers are released into the circulation whenever myocardiocyte injury occurs for acute ischemia as for any other mechanism (7, 8). More importantly, there is now convincing evidence that elevation of cardiac troponin values above the upper limit of the reference range, even when the threshold is low, is a significant predictor of death and morbidity in the general population (9, 10), as well as in patients with acute conditions admitted to the ED (11) and the intensive care unit (ICU) (12), irrespective of the presence of myocardial ischemia. Therefore, in order to establish whether myocardial sufferance or injury may be present after common trauma injuries, we carried out a retrospective case-control study to assess the values of cardiac troponin I (cTnI) in a large number of patients admitted to the ED with different types of trauma.
Materials and Methods
Study populations
The population of this retrospective case-control study consisted of all patients aged 18 years or older admitted to the ED of the Academic Hospital of Parma during the year 2014. The hospital is a 1250-bed facility and a level II trauma center. All patients visiting for trauma-related problems and needing admission to hospital wards were systematically extracted from the local database. As for local practice, all patients with trauma undergo a routine clinical chemistry testing upon ED admission, which also includes the measurement of cTnI to diagnose or rule out cardiac involvement. Results of cTnI obtained on trauma patients at admission and before receiving any type of treatment were then compared with those of two other different populations. One included 125 consecutive blood donors who participated in the definition of the local reference range for the cTnI immunoassay, as described elsewhere (13). The other population (i.e., ED patients with no trauma) consisted of 25 consecutive patients admitted to the local observation unit for evaluation of chest pain at moderate-to-high probability, who had negative results of dipyridamole-atropine echocardiography, as also described elsewhere (14).
Laboratory measurements
Blood sampling was performed in all patients immediately after ED admission. Blood was collected into evacuated blood tubes containing K2EDTA (Becton Dickinson, Franklin Lakes, NJ, USA). Plasma EDTA was separated within 1 h from blood drawing by centrifugation at 1500 × g for 15 min at room temperature, and cTnI was then measured using Beckman Coulter AccuTnI on DxI 800 (Beckman Coulter Inc, Chaska, Minnesota, USA). According to the results of a previous analytical study, the detection limit of this assay is 10 ng/L, the 99th percentile upper reference limit (URL) is 40 ng/L, whereas the total imprecision is comprised between 4.0–8.8% (15).
Statistical analysis
Data were checked for normality using Kolmogorov-Smirnov distributional test and values were finally displayed as median and interquartile range (IQR). The significance of differences among groups was assessed by Mann-Whitney U test (for continuous variables) and chi-square test (for categorical variables), respectively. The statistical analysis was performed using Analyse-it (Analyse-it Software Ltd, Leeds, UK). The odds ratio (OR) and its 95% confidence interval (95% CI) was calculated using MedCalc version 12.3.0 (MedCalc Software, Mariakerke, Belgium). This retrospective study was carried out in accordance with the Declaration of Helsinki, under the terms of all relevant local legislation, and was cleared by the Institutional Review Board.
Results
A total number of 456 trauma cases could be extracted from the hospital database according to the criteria formerly described. Seventy-six patients had to be further excluded due to incorrect or inappropriate recording in the database. Therefore, the final study population consisted of 380 trauma patients, 10 with isolated abdominal trauma, 99 with isolated trauma of the limbs, 49 with isolated chest trauma, 145 with isolated head trauma and 77 with polytrauma. No significant difference was observed in the age distribution of trauma patients compared to the populations of blood donors and ED patients without trauma. Compared to trauma patients, a larger prevalence of women was present in the population of blood donors but not in that of non-cardiac chest pain ED patients (Table I.)
Table I.
Demographic characteristics and cardiac troponin I (cTnI) values of the study populations. Results are shown as median and interquartile range or percentage.
| Trauma patients | Blood donors | p vs trauma patients | ED patients with no trauma | p vs trauma patients | |
|---|---|---|---|---|---|
| n | 380 | 125 | 25 | ||
| Age (years) | 72 (52–83) | 72 (57–81) | 0.450 | 71 (60–77) | 0.452 |
| Sex (F/M) | 165/215 | 77/48 | <0.001 | 9/16 | 0.234 |
| cTnI | |||||
| Values (ng/L) | 10 (0–20) | 0 (0–0) | 0.092 | 0 (0–10) | 0.288 |
| No. of cases >10 ng/L |
238 (63%) | 16 (20%) | <0.001 | 5 (20%) | <0.001 |
| No. of cases >40 ng/L |
77 (20%) | 0 (0%) | <0.001 | 2 (8%) | 0.067 |
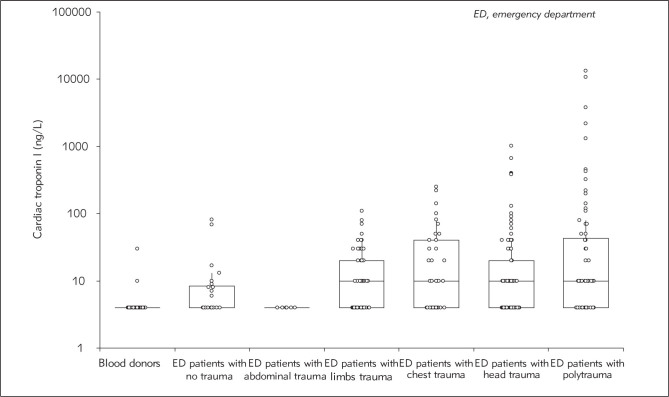
Although the median concentration of cTnI did not differ between the three study populations, the frequency of measurable values (i.e., >10 ng/L) was substantially higher in patients with trauma (63%) than in blood donors and non-cardiac chest pain ED patients (both 20%) (Table I; Figure 1). The frequency of patients with values above the 99th percentile URL (i.e., >40 ng/L) was also significantly higher in trauma patients (20%) than in blood donors (0%) and non-cardiac chest pain ED patients (8%), although in the latter case such difference did not reach statistical significance. Accordingly, the risk of having measurable cTnI in patients with trauma was nearly 11-fold higher (OR, 11.4; 95% CI, 6.5–20.1) compared to blood donors, and approximately 7-fold higher (OR, 6.7; 95% CI, 2.5–18.3) compared to ED patients with no trauma. The risk of having cTnI values above the 99th URL in trauma patients was also 64-fold higher (OR, 64.1; 95% CI: 3.9–1042.0) compared to blood donors and 2.9-fold higher (OR, 2.9; 95% CI, 0.7–12.7) compared to non-cardiac chest pain ED patients.
Figure 1.
Value of cardiac troponin I (cTnI) in the different study populations. Results are shown as median and interquartile range.
Compared to blood donors, the concentration of cTnI was found to be significantly higher in all trauma patients except in the limited number of those with abdominal trauma (Table II). Compared to non-cardiac chest pain ED patients, only patients with chest trauma had significantly increased values of cTnI (Table II.) Interestingly, the frequency of measurable cTnI as well as that of values above the 99th percentile URL were significantly higher in all types of trauma except abdominal trauma when compared to blood donors, and this may also be due to the limited number of patients included in the abdominal trauma subgroup. The frequency of measurable cTnI values was also significantly higher in all types of trauma except abdominal trauma when compared to noncardiac chest pain ED patients, whereas the frequency of cTnI values above the 99th percentile URL was significantly higher only in chest trauma and polytrauma (Table II). Multiple comparison of the frequency of values above the 99th percentile URL in the different types of trauma patients is shown in Table III. Patients with polytrauma and head or chest trauma had a significantly higher frequency of cTnI values above the 99th percentile URL compared to those with limbs and abdominal trauma, whereas no significant difference was found among patients with polytrauma and head or chest trauma, nor between patients with abdominal and limbs trauma.
Table II.
Demographic characteristics and cardiac troponin I (cTnI) values of the study populations. Results are shown as median and interquartile range or percentage.
| Blood donors | ED patients with no trauma | Abdominal | Limbs | Chest | Head | Polytrauma | |
|---|---|---|---|---|---|---|---|
| n | 125 | 25 | 10 | 99 | 49 | 145 | 77 |
| Age (years) | 72 (57–81) | 71 (60–77) | 45 (31–50)†,‡ | 73 (63–86)† | 71 (55–83) | 76 (60–84) | 60 (41–30)†,‡ |
| Sex (F/M) | 77/48 | 9/16 | 3/7† | 58/41‡ | 17/32† | 65/80† | 22/55† |
| cTnI | |||||||
| Values (ng/L) | 0 (0–0) | 0 (0–10) | 0 (0–0) | 10 (0–20)† | 10 (0–40)†,‡ | 10 (0–20)‡ | 10 (0–40)‡ |
| No. of cases >10 ng/L | 16 (20%) | 5 (20%) | 0 (0%) | 57 (58%)†,‡ | 29 (59%)†,‡ | 99 (68%)†,‡ | 53 (69%)†,‡ |
| No. of cases >40 ng/L | 0 (0%) | 2 (8%) | 0 (0%) | 11 (11%)† | 13 (27%)†,‡ | 31 (21%)† | 22 (29%)†,‡ |
p<0.05 versus blood donors;
p<0.05 versus ED patients with no trauma
Table III.
Comparison of the frequency of cardiac troponin I (cTnI) values >0.04 μg/L by chi square test.
| Limbs | Head | Polytrauma | Chest | |
|---|---|---|---|---|
| Abdominal | 0 vs 11% (p=0.123) |
0 vs 21% (p=0.049) |
0 vs 29% (p=0.025) |
0 vs 27% (p=0.032) |
| Limbs | – |
11 vs 21% (p=0.018) |
11 vs 29% (p=0.002) |
11 vs 27% (p=0.008) |
| Head | – | – | 21 vs 29% (p=0.116) |
21 vs 27% (p=0.228) |
| Polytrauma | – | – | – | 29 vs 27% (p=0.402) |
Significant differences in bold.
Discussion
Traumatic injuries generate many clinical and organizational problems for health care systems and the EDs, in that patients with acute and severe traumas need to be urgently managed and are at a greater risk of adverse outcome. Therefore, the identification of patients more vulnerable to complications is crucial for appropriate management, especially in increasingly overcrowded short stay units. Injury mortality is typically described by a trimodal distribution, entailing immediate death as a direct consequence of the trauma, early mortality due to massive hemorrhage, and late death mainly attributable to (multi) organ failure (16). Cardiac involvement, with or without cardiopulmonary instability, can be reliably mirrored by the release of cardiac biomarkers, and is now recognized as a negative prognostic factor in trauma patients (17). Due to the fact that cardiac troponin elevation is associated with a worse prognosis in many clinical settings (18), the identification of a certain degree of cardiac sufferance or overt injury may represent a cornerstone for acute patient management, whatever the pathogenetic mechanism and irrespective of the site and type of injury. Taken together, the results of our retrospective case-control study which first measured cardiac troponin in a vast array of trauma injuries attest that measurable cTnI values may be detected in approximately two-third of trauma patients, and are especially common in those with limbs, head or chest trauma, as well as in those with polytrauma. Even more importantly, cTnI values above the 99th percentile URL were also found to be frequent after trauma injuries, being present in 21–29% of patients with polytrauma and with head or chest trauma.
The significance of cardiac troponin elevations after traumatic injury has been previously demonstrated by Martin et al. (19), who reviewed the hospital records of 1081 patients admitted to the ICU with severe trauma. Specifically, cTnI elevations were observed in 29% of patients, a percentage similar to that observed in our investigation (i.e., 20%). The frequency of cTnI elevation was 17% in patients with head injury and 22% in those with chest trauma, respectively. Edouard et al. also showed that the incidence of cTnI release was 12% in a large series of 728 patients admitted to a surgical intensive care unit without preexisting coronary artery disease (20). In another case-control study based on a children population, Bennett et al. showed the frequency of serum cTnI values above the reference range was nearly 2-fold higher in patients with non-accidental trauma than in similarly aged uninjured children (21). In accord with these findings, Lindner et al. (22) recently reported that trauma injuries were responsible for as many as 15% of total elevation of cardiac troponin observed in an ED.
The observation that cTnI values were consistently increased in patients with head injury (21% of our patients had values above the 99th URL) is not really surprising, wherein Salim et al. (23) also showed that elevated cTnI is frequently observed after severe traumatic brain injury (i.e., in 30% of patients), that the levels are related to the severity of the injury and are also independent predictors of adverse outcomes. In a more recent investigation, Prathep et al. reviewed clinical data of 139 patients with isolated traumatic brain injury, and observed that elevated values of cardiac biomarkers were also present in 30% of patients (24).
Interestingly, evidence about the clinical usefulness of cardiac troponins for identifying cardiac involvement after chest trauma is limited. Ferjani et al. measured cardiac troponin T (cTnT) in 128 patients who suffered chest trauma, and found that elevated values of this biomarker were present in 31% of cases (25). Bertinchant et al. (26) also studied 94 patients with acute chest trauma and reported that the frequency of elevated cTnI and cTnT values was 23% and 12%, respectively. Overall, these two studies are in accord with our findings that cTnI values above the 99th percentile URL can be observed in 27% of patients admitted to the ED for chest trauma.
As regards polytrauma, our results demonstrate that this type of injury is associated with the highest frequency of both measurable cTnI values (i.e., 69%) and cTnI values above the 99th URL (i.e., 29%), thus essentially confirming that polytrauma patients may be those with the worst prognosis overall. Interestingly, no other reports could be found in the scientific literature about the association between increased cardiac biomarkers and polytrauma, nor could we find other studies which compared cardiac troponin values in trauma patients with those of both ostensibly healthy subjects and different ED populations.
There is now emerging evidence that the poor prognosis of acutely ill patients can be predicted by the measurement of cardiac biomarkers, especially cardiac troponins (12, 27). Therefore, the results of our retrospective case-control study support the concept that measurement of cardiac troponin may be advisable in trauma patients, especially in those with polytrauma and head or chest trauma, in order to diagnose or rule out a potential cardiac involvement and adopt the most appropriate therapeutic management. Regardless of the fact that a cardiac troponin elevation may mirror mechanical chest trauma, the severity of the overall injury, or even a physiologic stress in these patients, the identification of abnormal troponin values upon ED admission may then require a more focalized intervention for supporting cardiovascular health and a more strict monitoring of heart function.
The major strength of this study is that cTnI values could be consistently compared among different populations of trauma patients, thus allowing to identify specific categories with increased cardiovascular involvement. Moreover, the relative increments of troponin values were not only compared with those of a healthy population (i.e., blood donors) but also with those of non-cardiac chest pain ED patients, despite the fact that the sample size of this last population was indeed limited. Some limitations should also be disclosed. First, the precise cardiac mechanism leading to cTnI elevation could not be established in the vast majority of cases, wherein the presence of measurable or moderately elevated values (i.e., 40–100 ng/L) is not systemically investigated by diagnostic imaging in our local facility. No information is also available on potential co-morbidities that may have contributed to increase the frequency of measurable cTnI values in our trauma patients. However, to overcome this limitation, cTnI values of trauma patients were compared to those of non-cardiac chest pain ED patients matched for sex and age. Indeed, the use of the newer high-sensitivity cardiac troponin immunoassays is expected to generate additional information and further studies would hence be needed to confirm our findings (28). Unfortunately, no data on short-term mortality were available for these patients, and this may be regarded as another potential limitation of the study.
Conflict of interest statement
The authors stated that they have no conflicts of
References
- 1.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease Study. Lancet. 1997;349:1498–504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 2.US National Trauma Institute. Trauma Statistics. http://www.nationaltraumainstitute.org/home/trauma_statistics.html Available at: Last access: January 5, 2015.
- 3.Søreide K, Krüger AJ, Vårdal AL, Ellingsen CL, Søreide E, Lossius HM. Epidemiology and contemporary patterns of trauma deaths: changing place, similar pace, older face. World J Surg. 2007;31:2092–103. doi: 10.1007/s00268-007-9226-9. [DOI] [PubMed] [Google Scholar]
- 4.Evans JA, van Wessem KJ, McDougall D, Lee KA, Lyons T, Balogh ZJ. Epidemiology of traumatic deaths: comprehensive population-based assessment. World J Surg. 2010;34:158–63. doi: 10.1007/s00268-009-0266-1. [DOI] [PubMed] [Google Scholar]
- 5.US Centers for Disease Control and Prevention. Emergency Department Visits. http://www.cdc.gov/nchs/fastats/emergency-department.htm Available at: Last access: January 5, 2015.
- 6.Prekker ME, Miner JR, Rockswold EG, Biros MH. The prevalence of injury of any type in an urban emergency department population. J Trauma. 2009;66:1688–95. doi: 10.1097/TA.0b013e31817db0f1. [DOI] [PubMed] [Google Scholar]
- 7.Mahajan VS, Jarolim P. How to interpret elevated cardiac troponin levels. Circulation. 2011;124:2350–4. doi: 10.1161/CIRCULATIONAHA.111.023697. [DOI] [PubMed] [Google Scholar]
- 8.Cervellin G, Lippi G. Of MIs and men – a historical perspective on the diagnostics of acute myocardial infarction. Semin Thromb Hemost. 2014;40:535–43. doi: 10.1055/s-0034-1383544. [DOI] [PubMed] [Google Scholar]
- 9.Hamm CW, Giannitsis E, Katus HA. Cardiac troponin elevations in patients without acute coronary syndrome. Circulation. 2002;106:2871–2. doi: 10.1161/01.cir.0000044342.50593.63. [DOI] [PubMed] [Google Scholar]
- 10.Lippi G, Cervellin G. The latest generation of troponin immunoassays: the »cholesterol« of the third millennium? J Am Coll Cardiol. 2014;63:2883–4. doi: 10.1016/j.jacc.2014.02.609. [DOI] [PubMed] [Google Scholar]
- 11.Wilcox G, Archer PD, Bailey M, Dziukas L, Lim CF, Schneider HG. Measurement of cardiac troponin I levels in the emergency department: predictive value for cardiac and all-cause mortality. Med J Aust. 2001;174:170–3. doi: 10.5694/j.1326-5377.2001.tb143209.x. [DOI] [PubMed] [Google Scholar]
- 12.Reynolds T, Cecconi M, Collinson P, Rhodes A, Grounds RM, Hamilton MA. Raised serum cardiac troponin I concentrations predict hospital mortality in intensive care unit patients. Br J Anaesth. 2012;109:219–24. doi: 10.1093/bja/aes141. [DOI] [PubMed] [Google Scholar]
- 13.Lippi G, Dipalo M, Avanzini P, Formentini A, Aloe R. Analytical assessment of the Beckman Coulter Unicel DxI AccuTnI+3 immunoassay. Diagnosis. 2014;1:195–7. doi: 10.1515/dx-2013-0039. [DOI] [PubMed] [Google Scholar]
- 14.Cervellin G, Robuschi F, Scioscioli F, Ruffini L, Dipalo M, Salvagno GL. et al. Dipyridamole Stress Echocardiography Does Not Trigger Release of Highly-Sensitive Troponin I and T. J Med Biochem. 2014;33:376–83. [Google Scholar]
- 15.Uettwiller-Geiger D, Wu AH, Apple FS, Jevans AW, Venge P, Olson MD. et al. Multicenter evaluation of an automated assay for troponin I. Clin Chem. 2002;48:869–76. [PubMed] [Google Scholar]
- 16.Gunst M, Ghaemmaghami V, Gruszecki A, Urban J, Frankel H, Shafi S. Changing epidemiology of trauma deaths leads to a bimodal distribution. Proc (Bayl Univ Med Cent) 2010;23:349–54. doi: 10.1080/08998280.2010.11928649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kam C, Lai CH, Lam S, So F, Lau C, Cheung KH. What are the ten new commandments in severe polytrauma management? World J Emerg Med. 2010;1:85–92. [PMC free article] [PubMed] [Google Scholar]
- 18.De Palma R, Meier P. Troponin: a risk marker beyond heart disease. Open Heart. 2014;1:e000009. doi: 10.1136/openhrt-2013-000009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martin M, Mullenix P, Rhee P, Belzberg H, Demetriades D, Salim A. Troponin increases in the critically injured patient: mechanical trauma or physiologic stress? J Trauma. 2005;59:1086–91. doi: 10.1097/01.ta.0000190249.19668.37. [DOI] [PubMed] [Google Scholar]
- 20.Edouard AR, Felten ML, Hebert JL, Cosson C, Martin L, Benhamou D. Incidence and significance of cardiac troponin I release in severe trauma patients. Anesthesiology. 2004;101:1262–8. doi: 10.1097/00000542-200412000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Bennett BL, Steele P, Dixon CA, Mahabee-Gittens EM, Peebles J, Hart KW. et al. Serum Cardiac Troponin I in the Evaluation of Nonaccidental Trauma. J Pediatr. 2015;167:669–73.e1. doi: 10.1016/j.jpeds.2015.05.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lindner G, Pfortmueller CA, Braun CT, Exadaktylos AK. Non-acute myocardial infarction-related causes of elevated high-sensitive troponin T in the emergency room: a cross-sectional analysis. Intern Emerg Med. 2014;9:335–9. doi: 10.1007/s11739-013-1030-y. [DOI] [PubMed] [Google Scholar]
- 23.Salim A, Hadjizacharia P, Brown C, Inaba K, Teixeira PG, Chan L. et al. Significance of troponin elevation after severe traumatic brain injury. J Trauma. 2008;64:46–52. doi: 10.1097/TA.0b013e31815eb15a. [DOI] [PubMed] [Google Scholar]
- 24.Prathep S, Sharma D, Hallman M, Joffe A, Krishnamoorthy V, Mackensen GB. et al. Preliminary report on cardiac dysfunction after isolated traumatic brain injury. Crit Care Med. 2014;42:142–7. doi: 10.1097/CCM.0b013e318298a890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ferjani M, Droc G, Dreux S, Arthaud M, Goarin JP, Riou B. et al. Circulating cardiac troponin T in myocardial contusion. Chest. 1997;111:427–33. doi: 10.1378/chest.111.2.427. [DOI] [PubMed] [Google Scholar]
- 26.Bertinchant JP, Polge A, Mohty D, Nguyen-Ngoc-Lam R, Estorc J, Cohendy R. et al. Evaluation of incidence, clinical significance, and prognostic value of circulating cardiac troponin I and T elevation in hemodynamically stable patients with suspected myocardial contusion after blunt chest trauma. J Trauma. 2000;48:924–31. doi: 10.1097/00005373-200005000-00018. [DOI] [PubMed] [Google Scholar]
- 27.Courtney D, Conway R, Kavanagh J, O'Riordan D, Silke B. High-sensitivity troponin as an outcome predictor in acute medical admissions. Postgrad Med J. 2014;90:311–6. doi: 10.1136/postgradmedj-2013-132325. [DOI] [PubMed] [Google Scholar]
- 28.Lippi G. Biomarkers: Novel troponin immunoassay for early ACS rule-out. Nat Rev Cardiol. 2016;13:9–10. doi: 10.1038/nrcardio.2015.174. [DOI] [PubMed] [Google Scholar]