Abstract
Purpose: Cancer-related fatigue (CRF) is a distressing consequence of cancer and its treatment. CRF impacts many young adult (YA) survivors of childhood cancer, compromising work, social relationships, and daily activities. No satisfactory treatment exists. This pilot study aimed to assess the feasibility, safety, and preliminary efficacy of an 8-week twice/week Iyengar yoga (IY) intervention for treating persistent fatigue in YA survivors of childhood cancer.
Methods: Using a single-arm mixed-methods design, adult childhood cancer survivors aged between 18 and 39 years were recruited from a survivorship clinic at a single institution. Quantitative: The primary outcome was fatigue as measured by the Functional Assessment of Chronic Illness Therapy-Fatigue. Secondary outcomes included vitality, social functioning, multidimensional fatigue, mood, and sleep. Weekly self-report monitoring data were collected. Qualitative: Participants also completed a post-intervention interview, major themes evaluated.
Results: Five participants enrolled into the study and four completed the intervention. Attendance was 92% and there were no adverse events. Baseline mobility was highly varied, with one YA having had a hemipelvectomy. Quantitative data revealed significantly improved fatigue, social functioning, somatization, and general and emotional manifestations of fatigue following yoga. Qualitative data cross validated, clarified, and expanded upon the quantitative findings.
Conclusions: The study suggests that a brief IY intervention is safe for YA survivors of childhood cancer, even for those with physical disabilities. Preliminary efficacy was demonstrated for the primary outcome of fatigue. Qualitative data elucidated additional improvements, such as work-related social functioning, and a sense of calm and relaxation.
Keywords: : yoga, fatigue, cancer survivors, integrative medicine
Introduction
Approximately 80% of children and adolescents diagnosed with pediatric cancers survive at least 5 years after their diagnosis.1,2 Survivors of childhood cancer are at risk for diminished health status, including fatigue. Cancer-related fatigue (CRF) has been described by patients as pervasive, debilitating, and not relieved by rest, and involving physical, mental, and emotional exhaustion.3 Such fatigue has a negative impact on work, social relationships, and daily activities and causes significant impairment in quality of life among survivors.4,5
The causes of CRF have not been determined, but may relate to the direct effects of cancer or cancer treatment, comorbid medical conditions, comorbid symptoms, and psychosocial factors.6 Despite the prevalence of CRF, few evidence-based interventions exist.7 Behavioral interventions, such as exercise, may be effective,8 as may psychosocial interventions that include stress management and relaxation.9–11 However, survivors with CRF may be unwilling or unable to participate in standard exercise programs, since fatigue is one of the primary barriers to participation in exercise programs among cancer survivors.12 Interventions that incorporate both physical activity and relaxation may offer greater benefit than either modality alone,13 particularly for fatigued patients, who require a balance of exertion and restoration. Yoga includes both physical activity and relaxation/meditation and offers a promising integrative treatment for CRF.
A growing number of yoga studies have been conducted for varied medical conditions, demonstrating beneficial effects on physical and behavioral outcomes, including fatigue. A review of yoga for cancer14 concluded that yoga interventions consistently yield modest improvement in psychological (mood, distress, stress) and somatic symptoms. Possible mechanisms of Iyengar yoga (IY) for fatigue include improving muscle strength, sleep quality, and mood, and in reducing underlying biological inflammatory processes such as inflammation-related gene expression.15
Although it has been estimated that as many as one-third of young adult (YA) survivors regularly practice yoga,16 no studies have yet examined the use of yoga specifically in a YA childhood cancer survivor population. The purpose of the current study was to pilot the use of IY, a tradition that emphasizes alignment, individualized restorative poses that can be accommodated to patients, and extensive teacher training, in YA survivors with fatigue. We used a mixed-methods approach, examining both quantitative (questionnaire) and qualitative (interview) data, to gain a comprehensive overview of the feasibility issues, safety, and preliminary efficacy of yoga in this population.
Methods
We employed a mixed-methods single-arm design to examine an 8-week twice/week IY intervention for YA survivors of childhood cancer. Inclusion criteria included YAs aged between 18 and 39 years diagnosed with cancer (leukemia, brain tumor, Hodgkin lymphoma, non-Hodgkin lymphoma, Wilms' tumor, neuroblastoma, soft tissue sarcoma, or bone tumors) before the age of 21 experiencing persistent fatigue, and no longer receiving treatment or therapy for cancer for at least 1 year. Inclusion criteria also included approval from their oncologist to participate in the study; participants without an oncologist were asked to obtain permission from their primary care provider. Full approval for this study was received from the Institutional Review Board of the University of California, Los Angeles.
Participants were recruited by sending ∼40 invitation letters to the Young Adult Survivorship clinic (a program of the UCLA-LIVESTRONG Survivorship Center of Excellence). We also contacted online cancer community support groups to post about the study during 2011 and 2012. Preliminary screening for cancer-related and medical criteria (e.g., age, time of cancer diagnosis and treatment) was conducted through an initial telephone screening. The current fatigue level was evaluated using the vitality subscale of the Short Form (SF)-36. Participants who scored at or below 50 were eligible for participation. Previous research examining yoga for fatigued cancer survivors has used a score of 50 or below on the vitality subscale of the SF-36,17 as the score seems to denote behavioral, immune, and neuroendocrine alterations associated with clinically important levels of fatigue.4 A trained research assistant scheduled a preliminary assessment involving questionnaires ∼2 weeks before the intervention. Participants returned for their post-intervention assessments, which included questionnaires and an interview, within 2 weeks of completing yoga (range = 2–7 days).
A total of eight individuals expressed interest in the study. One did not meet fatigue criteria, another cited scheduling conflicts, and another fatigue and distance barriers. A further participant dropped out of the study after the first week. The remaining four participants completed the yoga intervention. Diagnoses include one participant with Hodgkin lymphoma, one with neuroblastoma and breast cancer, one with non-Hodgkin lymphoma, and one with osteosarcoma. The mean number of yoga sessions attended was 14.75 classes (92% adherence). The demographic characteristics of participants, including length of time since cancer treatment, are shown in Table 1.
Table 1.
Participant Characteristics
| Characteristic | Total sample (n = 4) |
|---|---|
| Female, n (%) | 3 (75) |
| Male, n (%) | 1 (25) |
| Age, years, mean (SD) | 26.5 (8.9) |
| Years since diagnosis | 12.8a (14.5) |
| Ethnicity, n (%) | |
| Hispanic | 1 (25) |
| Non-Hispanic | 3 (75) |
| Race, n (%) | |
| Caucasian | 3 (75) |
| Multiracial | 1 (25) |
| Education, n (%) | |
| Some college | 2 (50) |
| Bachelor's degree | 1 (25) |
| Master's degree | 1 (25) |
One participant was diagnosed with neuroblastoma at age 4 and was later diagnosed with breast cancer at age 37.
Yoga intervention
We used IY, a tradition suited to meeting the rehabilitation needs of people with medical conditions.18 Postures and breathing techniques believed to be effective for reducing fatigue were used, with a focus on passive inversions (i.e., supported upside-down postures in which the head is lower than the heart) and passive backbends (i.e., supported spinal extensions). In supportive postures, the shape of the pose is supported by props (e.g., blocks, bolsters, blankets, wall ropes, belts), rather than held by the strength of the body, so that participants can perform and maintain the postures without stress and tension.
Poses were carefully selected by an experienced IY teacher (B.S), who is also a qualified teacher of mindfulness based stress reduction and mindful self-compassion (MSC; which incorporates mindfulness and practices around developing compassion and kindness toward oneself and others), with more than 15 years of experience teaching yoga and meditation to patient populations at UCLA, including breast cancer survivors with persistent fatigue. A typical sequence of IY postures at midintervention is as follows (not accounting for pose setup and explanation time): 1) Supta Baddhakonasana (10 minutes), 2) Setubandha Sarvangasana on bolsters (5 minutes); Bolster twist, Sukhanasana forward bend with head support; janu sirsasana forward bend with head support, 3) Adhomukha Svanasana (5 minutes), 4) Salamba Sirsasana (5 minutes); salamba purvottanasana, 5) Viparita Dandasana (5 minutes), 6) Setubandha Sarvangasana on a wooden bench (5 minutes), 7) Viparita Karani (10 minutes), and 8) Supported Savasana (10 minutes). The 10-minute savasana included a meditation focused on loving kindness practices. The intervention was administered twice a week for 1.5 hours of duration per session for 8 weeks, and one make up class was available. Daily home practice was encouraged but not prescribed. Participants were given a selection of props (blankets and bolsters) and an audio link to an MSC exercise to use at home. At the end of the 8 weeks, interested participants were provided with a list of referrals to IY studios/teachers in the community.
Measures
Primary outcome
The Functional Assessment of Chronic Illness Therapy-Fatigue Subscale 19 measures fatigue in a cancer setting and includes 13 items that assess physical and functional consequences of fatigue. Higher scores indicate less fatigue.
Secondary outcomes
The Vitality subscale of the SF-36 (SF-36)20 was used to assess energy/fatigue. Higher scores denote better functioning.
The Fatigue Symptom Inventory was used to assess fatigue interference with daily social functioning.21
The Multidimensional Fatigue Symptom Inventory-SF assesses general, physical, emotional, and mental manifestations of fatigue. This measure was developed specifically for use with cancer populations.22,23
Mood was evaluated using the Brief Symptom Inventory 18,24 which assesses anxiety, somatization, and depressive symptoms within the past 7 days.24
Pittsburgh Sleep Quality Index25 assesses subjective sleep quality over the past month. We used the overall sleep quality component. Higher scores indicate better functioning.
A weekly monitoring form was administered via email to participants at the beginning of each week. The form asked about weekly fatigue, functioning, mood, pain, improvement, and yoga home practice. The form was administered 7 days preceding the intervention to ascertain baseline functioning, once/week during the intervention period (it was sent out to participants the day following yoga classes, and the majority of participants completed it within 36 hours of the preceding class), and at a 2-month follow-up.
Data analysis
For the questionnaire data, we used paired-sample t-tests to examine differences in postintervention versus preintervention scores. T-tests represent a reasonable approach to analyzing data from very small sample sets.26 Significance tests were set at 0.05, although trends at 0.10 were also noted. Effect sizes (using Cohen's d comparing mean changes from baseline to postintervention) were calculated to show magnitude and direction of the effect of the yoga intervention. Values of Cohen's d of 0.20, 0.50, and 0.80 represent small, medium, and large effect sizes, respectively.27 For the weekly monitoring form data, means for each variable were calculated and plotted.
Qualitative responses were analyzed with ethnographic content analysis. This technique involves the creation of a codebook based on variables designated by the researcher as relevant to the research questions and goals. Texts are read, and codes are assigned to relevant portions of the text and entered. The process is iterative and code categories are revised, expanded, and created as research progresses. After the interviews had been read in detail twice by two different researchers who discussed and resolved any discrepancies in coding, main themes were identified and coded according to variables that were consistent with the quantitative data. Corresponding quotes were entered into Microsoft Excel to create tables identifying the main themes. Quantitative and qualitative measures were used to cross validate the qualitative and quantitative data (triangulation), clarify the data from one method with the data of another (complementarity), and broaden the depth of the data (expansion).
Results
Quantitative data
As shown in Table 2, participants reported significant improvement in the primary outcome of fatigue and significant improvements in general and emotional manifestations of fatigue, social relationships, and somatization following yoga. Trends were observed for improved vitality and physical manifestations of fatigue. Effect sizes were generally large.
Table 2.
Pre- and Postintervention Score Differences with Effect Sizes
| Measure | Pre-yoga mean (SD) | Post-yoga mean (SD) | % Difference | T-test (df = 3) | Effect size (Cohen's d) |
|---|---|---|---|---|---|
| FACIT-Fatigue | 26.75 (5.32) | 39.25 (5.80) | 46.73 | −3.81a | −1.91 |
| Vitality SF-36 | 31.25 (4.79) | 47.50 (11.90) | 52.0 | −2.93b | −1.73 |
| FSI impaired social functioning | 5.25 (2.63) | 1.0 (0.82) | −80.95 | 4.12a | 3.71 |
| MFSI general | 15.75 (0.96) | 8.75 (2.63) | −44.44 | 3.93a | 2.0 |
| Physical | 8.25 (6.13) | 6.25 (6.24) | −24.24 | 2.45b | 1.32 |
| Emotional | 10.25 (4.03) | 5.0 (2.94) | −51.22 | 10.67a | 1.61 |
| Mental | 10.75 (0.96) | 9.25 (4.27) | −13.95 | 0.67 | 0.38 |
| BSI-18 anxiety | 6.0 (4.08) | 3.3 (2.62) | −45.0 | 1.18 | 0.60 |
| Depression | 4.25 (4.57) | 2.5 (1.73) | −41.18 | 1.21 | 3.93 |
| Somatization | 6.25 (1.26) | 2.5 (1.91) | −60.0 | 5.96a | 3.42 |
| PSQI sleep quality | 1.5 (1.0) | 1.75 (0.96) | 16.67 | −1.0 | −0.50 |
p < 0.05.
p < 0.10.
BSI, Brief Symptom Inventory; FACIT, Functional Assessment of Chronic Illness Therapy; MFSI, Multidimensional Fatigue Symptom Inventory; PSQI, Pittsburgh Sleep Quality Index; SF, Short Form.
Weekly monitoring
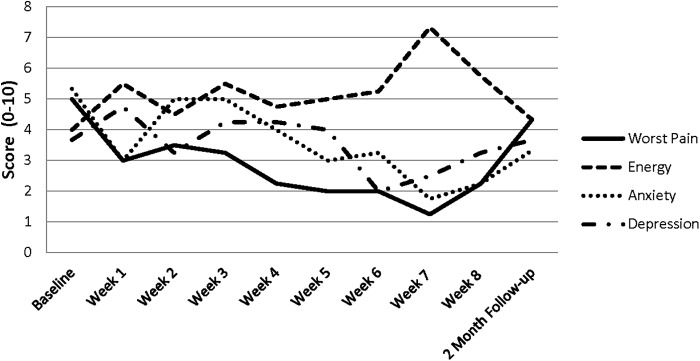
Data from the weekly monitoring form are shown in Figure 1, demonstrating weekly ratings of pain, energy anxiety, and depression across baseline, throughout the intervention, and at 2-month follow-up. Because of the small sample size, statistical tests were not performed on the multiple time points. The plots demonstrate a possible reduction in anxiety toward the end of the intervention, with scores returning to baseline levels at the 2-month follow-up. Data also indicated that none of the participants had continued with yoga at follow-up. No serious adverse events were reported during class or home practice.
FIG. 1.
Baseline, weekly, and 2-month follow-up pain, anxiety, depression, and energy scores across the intervention.
Qualitative data
Postintervention interview data were analyzed for the four study completers. Themes related to triangulation, complementarity, and expansion of the quantitative measures. Triangulation, or cross validation of the qualitative and quantitative data, was evident in a number of domains, including improvement in social functioning following yoga:
“I'm not reluctant to go out any more because I was reluctant in the past to just be active because I didn't want to be tired all the time afterward. And I'm not so reluctant about that anymore.”
Another participant noted improved relationships in her family, as well as more energy to perform in the work domain, which improved her social relationships: “I think that it (yoga) helps also in managing work stress too because I'm able to kind of better handle it.”
A further area that interviews cross validated the quantitative findings was in improved somatization. Participants felt that their general aches and pain had improved, and they were less focused on judging or worrying about their health:
“I think that, so what I used to do is have, ruminations and the spinning thoughts of what's wrong with my body or am I going to get sick again—just really a lot of anxiety like that. And I noticed that's really calmed down. That's a lot quieter, and that I don't have as much nervousness and anxiety about getting sick or things being wrong with my body.”
Information shared by participants in the interviews provides complementarity, or clarification of the data from one method with the data of another, with clues as to why we did not find significant quantitative differences in some outcomes, such as sleep. For at least one participant, the benefits of yoga for sleep were contingent upon her home practice near bedtime.
“I think I know how to be a better sleeper now. Just because, I would do yoga in the afternoon, near night-time, and it would just put me in a relaxed state of mind before sleep. And so I found it really easy to go to sleep.”
Two other participants noted that following the weekly evening yoga classes, they slept well. Another area the interview data provided clarification to the quantitative data was in assessing mood. We failed to find significant improvements on the anxiety and depression questionnaire items. However, interviews revealed that participants felt a growing sense of calm. Key phrases used by participants included ‘less stressed’ and “more relaxed.” One participant noted: “In general I can be a lot calmer. I can just calm myself down. The yoga study has helped with my body and my mind. It's helped me be more positive.” All participants noted that yoga helped with stress, but perhaps these global improvements in mood were not reflected in their responses to the questionnaire items.
With respect to expansion of the quantitative data, a number of responses highlighted the complexities of fatigue. Yoga did not entirely remove fatigue, but the intervention did provide relief from symptoms and enabled participants to carry on despite lingering fatigue. One participant described yoga as helping to “combat fatigue,” another noted she now experienced “tired waves as opposed to being tired all the time,” and a third expressed that although her fatigue was still present “It's really important to me that I have kind of a medicine for it now.” The following participant, however, felt it was hard to quantify whether her fatigue had reduced: “Maybe it's the kind of thing where if you look from a bird's eye view, maybe I am less fatigued and I don't even know because I'm in it.”
Interviews also revealed that yoga impacted general physical activity. Participants noted that they developed increased stamina to engage in other forms of exercise as a result of participating in yoga, without “feeling exhausted afterward.” Although we did not formally assess changes in weight or BMI, one participant lost a substantial amount of weight over the course of the intervention, which she attributed to yoga:
“I've definitely been doing more physical activity than before. I lost 10 pounds. That's a huge, big deal. My doctors are super happy. That's been a huge benefit. I've been more mindful of my eating. Now I'm conscious of what I'm going to eat that's going to make me feel good and that's helping.”
Yoga also brought a sense of confidence and self efficacy: “And we also did a lot of things with our bodies that I didn't think possible—like hanging upside down and the different ways we stretched. And for confidence, it was great to see.” Perhaps this confidence in their yoga capabilities generalized outside class and equipped participants with the confidence to engage in life tasks, including the social experiences and physical activity they noted in interviews.
Discussion
This study examined the feasibility, safety, and preliminary efficacy of an 8-week twice/week yoga intervention for fatigue in YA survivors of childhood cancer. Our efforts yielded a small number of interested participants, which may reflect low interest of survivors in such an intervention, or difficulty reaching this group. Participants who completed the intervention demonstrated excellent adherence, attending 92% of classes. The intervention was safe, with no serious adverse events reported. We also found significant improvements in the primary outcome of self-reported fatigue and significant improvements in general and emotional manifestations of fatigue, social relationships, and somatization following yoga. For all significant findings, effect sizes were large (above 1.0) and in a direction indicating improved functioning following yoga. We noted statistical trends for physical manifestations of fatigue and vitality (as assessed by the SF-36). Although mean SF-36 vitality scores remained below 50, reflecting fatigue levels that were higher than the general population, there was a large standard deviation for post-yoga scores, indicating that some participants' scores reached normative levels.
The qualitative data cross validated, clarified, and expanded data sources. Interviews revealed strong validation of statistically improved somatization and social functioning, which included social functioning in personal and work relationships. Patients spoke of increased energy for social outings, including dating and effort into work relationships. For a YA population, such tasks are developmentally critical, since young adulthood is concerned with forming relationships, creation of family, and career establishment. Of interest, somatization and social functioning saw the largest statistical improvements, demonstrating cross validation between data sources. Interviews also clarified statistical data; for example, no statistical improvements were found for self-reported sleep quality. However, at least one participant reported that the benefits of yoga for sleep were contingent upon her home practice near bedtime. Participants also indicated that they felt a general uplift in their mood, improved ability to relax, and sense of calm, findings that may not have been captured by specific items on the anxiety and depression questionnaires we used. Expansion of the data sets was evident in the area of fatigue. Although we found statistically significant improvement in fatigue, interviews provided greater detail about the complexity of this outcome. Participants expressed that fatigue was still present, but episodes were less frequent and less debilitating.
Data from the weekly monitoring forms suggest that there may be gradual improvement in anxiety toward the end of the intervention, with a return to baseline functioning at the 2-month follow-up. No participants were practicing yoga at the follow-up. These findings indicate that the benefits of yoga may only be present while engaging in the practice, much like other physical exercise treatments. To see sustained effects, patients likely need to continue with long-term yoga training or develop a home practice. The lack of engagement in yoga at follow-up is consistent with previous studies28,29 and likely reflects the need for continued support of the practice.
This study is limited in various ways. A key weakness of the study is the difficulty drawing conclusions from the data, given the very small sample size and the lack of control/comparison group. Without an active control group, we are not able to account for the nonspecific effects of yoga practice, including patient expectations, group membership, and teacher attention. Although conclusions are limited, the present study marks the beginning of our understanding of yoga as a suitable adjunct treatment in the clinical care of YA survivors with fatigue. We were unable to attract large numbers of participants to the study, perhaps reflecting notions that exercise interventions are difficult for YA survivors with persistent fatigue. As a result of the small sample size, it is possible that the few survivors who did participate are not representative of the young survivor population as a whole. For those who did participate, we were able to demonstrate that yoga can be successfully adapted to individual patient needs, regardless of level of functioning. In fact, one of the participants had a single lower extremity following a hemipelvectomy as treatment for Ewing's sarcoma. Yet, she was able to successfully practice and complete the intervention and her experiences were among the most positive of our participants.
CRF is a heavily disabling condition that impacts many YA survivors, yet few interventions exist to manage this distressing condition.7 Yoga may offer a cost-effective, effective, and accessible tool for YA survivors with persistent fatigue, by accessing both physical and mental health benefits, offering a balance between exertion and relaxation, and providing modifications to all patients regardless of functioning. The present study indicates the promise of yoga interventions for YA with CRF and supports the need for further large-scale trials.
We conclude by offering a word of caution when recommending yoga classes to treat fatigue. Not all yoga classes are comparable in terms of safety and efficacy, since many classes may not have a demonstrable teacher training system or teachers may not have experience with medical populations. We recommend that patients, particularly those with demonstrable physical limitations, undertake yoga under the supervision of an experienced and sufficiently qualified yoga professional.
Acknowledgments
This study was funded by NCCAM grant K01AT005093 (S.E.), UCLA Jonsson Comprehensive Cancer Center H. Brown Award (L.Z.), UCLA Clinical and Translational Science Institute Grant UL1TR000124 (J.T.), and by the UCLA Children's Discovery and Innovation Institute (S.E.).
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Mariotto AB, et al. Long-term survivors of childhood cancers in the United States. Cancer Epidemiol Biomarkers Prev. 2009;18(4):1033–40 [DOI] [PubMed] [Google Scholar]
- 2.Howlader N, Noone AM, Krapcho M, Miller D, Bishop K, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA. (Eds). SEER Cancer Statistics Review, 1975-2013, National Cancer Institute; Bethesda, MD: Accessed April2016 from: http://seer.cancer.gov/csr/1975_2013/ [Google Scholar]
- 3.Hofman M, et al. Cancer-related fatigue: the scale of the problem. Oncologist. 2007;12(Suppl 1):4–10 [DOI] [PubMed] [Google Scholar]
- 4.Bower JE, et al. Fatigue in breast cancer survivors: occurrence, correlates, and impact on quality of life. J Clin Oncol. 2000;18(4):743–53 [DOI] [PubMed] [Google Scholar]
- 5.Vogelzang NJ, et al. Patient, caregiver, and oncologist perceptions of cancer-related fatigue: results of a tripart assessment survey. The Fatigue Coalition. Semin Hematol. 1997;34(3 Suppl 2):4–12 [PubMed] [Google Scholar]
- 6.Wagner LI, Cella D. Fatigue and cancer: causes, prevalence and treatment approaches. Br J Cancer. 2004;91:822–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mock V. Evidence-based treatment for cancer-related fatigue. J Natl Cancer Inst Monogr. 2004;2004(32):112–8 [DOI] [PubMed] [Google Scholar]
- 8.Mock V, et al. Fatigue and quality of life outcomes of exercise during cancer treatment. Cancer Pract. 2001;9(3):119–27 [DOI] [PubMed] [Google Scholar]
- 9.Jacobsen PB, et al. Efficacy and costs of two forms of stress management training for cancer patients undergoing chemotherapy. J Clin Oncol. 2002;20(12):2851–62 [DOI] [PubMed] [Google Scholar]
- 10.Fawzy FI, et al. A structured psychiatric intervention for cancer patients. II. Changes over time in immunological measures. Arch Gen Psychiatry. 1990;47(8):729–35 [DOI] [PubMed] [Google Scholar]
- 11.Spiegel D, Bloom JR, Yalom I. Group support for patients with metastatic cancer. A randomized outcome study. Arch Gen Psychiatry. 1981;38(5):527–33 [DOI] [PubMed] [Google Scholar]
- 12.Courneya KS, et al. Three independent factors predicted adherence in a randomized controlled trial of resistance exercise training among prostate cancer survivors. J Clin Epidemiol. 2004;57(6):571–9 [DOI] [PubMed] [Google Scholar]
- 13.Rabin C, Pinto B, Fava J. Randomized trial of a physical activity and meditation intervention for young adult cancer survivors. J Adolesc Young Adult Oncol. 2016;5(1):41–7 [DOI] [PubMed] [Google Scholar]
- 14.Bower JE, et al. Yoga for cancer patients and survivors. Cancer Control. 2005;12(3):165–71 [DOI] [PubMed] [Google Scholar]
- 15.Bower JE, et al. Yoga reduces inflammatory signaling in fatigued breast cancer survivors: a randomized controlled trial. Psychoneuroendocrinology. 2014;43:20–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Park CL, Cho D, Wortmann JH. The impact of Yoga upon young adult cancer survivors. Complement Ther Clin Pract. 2013;19(2):77–82 [DOI] [PubMed] [Google Scholar]
- 17.Bower JE, et al. Yoga for persistent fatigue in breast cancer survivors: a randomized controlled trial. Cancer. 2012;118(15):3766–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Evans S, Tsao JC, Zeltzer LK. Iyengar yoga for pediatric chronic pain. Pediatric Pain Lett. 2009;11(2):12–6 [Google Scholar]
- 19.Yellen SB, Cella DF, Webster K, et al. Measuring fatigue and other anemia-related symptoms with the Functional Assessment of Cancer Therapy (FACT) measurement system. J Pain Symptom Manage. 1997;13(2):63–74 [DOI] [PubMed] [Google Scholar]
- 20.Ware JE, Kosinski M, Dewey JE. How to score version two of the SF-36 health survey. Lincoln, RI: QualityMetric; 2000 [Google Scholar]
- 21.Jacobsen PB. Assessment of fatigue in cancer patients. J Natl Cancer Inst Monogr. 2004;(32):93–7 [DOI] [PubMed] [Google Scholar]
- 22.Stein KD, et al. A multidimensional measure of fatigue for use with cancer patients. Cancer Pract. 1998;6(3):143–52 [DOI] [PubMed] [Google Scholar]
- 23.Hann DM, et al. Measurement of fatigue in cancer patients: development and validation of the Fatigue Symptom Inventory. Qual Life Res. 1998;7(4):301–10 [DOI] [PubMed] [Google Scholar]
- 24.Derogatis LR. BSI 18, brief symptom inventory 18: administration, scoring and procedures manual. Minneapolis: NCS Pearson, Inc.; 2001 [Google Scholar]
- 25.Buysse DJ, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213 [DOI] [PubMed] [Google Scholar]
- 26.de Winter J. Using the Student's t-test with extremely small sample sizes. Pract Assess Res Eval. 2013;18(10):1 [Google Scholar]
- 27.Cohen J. Statistical power analysis for the behavioral sciences, 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Assoc; 1988 [Google Scholar]
- 28.Evans S, et al. Iyengar yoga for adolescents and young adults with irritable bowel syndrome. J Pediatr Gastroenterol Nutr. 2014;59(2):244–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Evans S, et al. Impact of Iyengar yoga on quality of life in young women with rheumatoid arthritis. Clin J Pain. 2013;29(11):988–97 [DOI] [PMC free article] [PubMed] [Google Scholar]