Abstract
Background
Fluid overload in patients on conventional hemodialysis is a frequent complication, associated with increased cardiovascular morbidity and mortality. The dialysate sodium prescription is a potential modifiable risk factor. Our primary objective was to describe associations between dialysate-to-serum sodium gradient and parameters of fluid status. A secondary objective was to evaluate the 6-month risk of hospitalization and mortality in relation to sodium gradient.
Methods
We performed a cross-sectional study of 110 prevalent conventional hemodialysis patients at a single center. The associations of sodium gradient with interdialytic weight gain index (IDWG%), ultrafiltration (UF) rate, and blood pressure (BP) were analyzed.
Results
The mean serum sodium gradient was 4.6 ± 3.6 mEq/L. There was a direct correlation between sodium gradient and IDWG% (r = 0.48, p < 0.01) as well as UF rate (r = 0.44, p < 0.01). In a logistic regression model, a 1 mEq/L higher sodium gradient was associated with increased risk of IDWG% >3% (OR 1.33, p < 0.01) and increased risk of UF rate >10 mL/kg/h (OR 1.16, p = 0.03), but there were no associations with intradialytic hypotension, intradialytic hypertension or BP. No significant differences were found with 6-month hospitalization or mortality risk in relation to sodium gradient.
Conclusion
A higher sodium gradient was associated with significant increases in IDWG and UF rates, known to be associated with poor outcomes, but was not associated with intradialytic hypotension. Individualizing the dialysate sodium prescription to minimize sodium gap may lead to less fluid overload in conventional hemodialysis patients.
Keywords: Hemodialysis, Sodium, Sodium gradient, Fluid overload, Interdialytic weight gain, Ultrafiltration
Introduction
It is estimated that up to one-third of patients on conventional hemodialysis and peritoneal dialysis are volume overloaded [1, 2]. Reasons for this are multifactorial and include limitations of physical examination and current dialysis technologies to accurately diagnose volume overload, patient indiscretion with diet, and dialysis sodium prescription [3, 4, 5, 6]. It has been demonstrated that patients who are >2.5 L volume overloaded at the start of hemodialysis have a hazard ratio (HR) of 2.1 for mortality and this is independent of blood pressure (BP) [2]. Several mechanisms have been proposed to explain how volume overload leads to increased mortality in the dialysis population, mostly linking volume overload to left ventricular hypertrophy with associated cardiovascular events and more recently, to inflammation which in turn leads to accelerated atherosclerosis [2, 7, 8, 9]. Interdialytic weight gain (IDWG) is often used as a surrogate marker for fluid overload and studies have shown that a higher IDWG% (ratio of IDWG to dry weight) predicts cardiovascular events (IDWG 3.0–3.9% and HR 1.80 [95% CI 0.95–3.41]; IDWG >4.0% and HR 1.93 [95% CI 1.02–3.64]) [10]. In addition, higher ultrafiltration (UF) rates of >10 mL/kg/h have also been shown to increase mortality [11]. Higher UF rates and IDWG may also lead to more frequent episodes of intradialytic hypotension, which can be linked to vascular access complications, and inadequate dialysis, but most importantly increased cardiovascular morbidity and mortality [12, 13].
The dialysis prescription and particularly the dialysate sodium concentration are critical to maintain a euvolemic state. While various dialysate sodium concentrations have been used throughout the history of dialysis, recent studies have shown that the potential benefits of using a higher dialysate sodium with regard to hemodynamic stability are outweighed by increased thirst, higher IDWG, and higher pre-dialysis blood pressure (pre-BP) [14, 15, 16]. Furthermore, frequently used sodium modeling algorithms which typically involve tapering a high dialysate sodium concentration during hemodialysis can lead to greater IDWG and higher pre-BP [14]. The optimal dialysate sodium concentration, however, still remains unclear. Many dialysis centers around the world use a standard dialysate sodium concentration for all patients; a recent DOPPS report showed that 57% of hemodialysis facilities use a standard dialysate sodium prescription [17, 18]. However, multiple studies have suggested that each dialysis patient may have a unique osmolar set point for plasma sodium and, therefore, dialysate sodium needs to be individualized [19, 20, 21, 22, 23]. More recently, there has been growing evidence that the sodium gradient (dialysate sodium minus predialysis serum sodium) is important to minimize in hemodialysis patients as it positively correlates with changes in BP during hemodialysis and IDWG [16, 19, 20, 21, 22, 23, 24, 25], with a sodium gradient of >3 mEq/L particularly associated with adverse outcomes [24, 25].
The primary objective of our study was to describe associations between dialysate-to-serum sodium gradient and various hemodialysis parameters of fluid status including BP, IDWG, and UF rates. A secondary analysis was performed to evaluate the 6-month risk of all-cause hospitalization and mortality in relation to the sodium gradient.
Methods
We performed a cross-sectional study of all prevalent hemodialysis patients at the McGill University Health Centre including the Royal Victoria Hospital and Montreal General Hospital units with an index study date of January 26 or 27, 2015. We included all patients aged >18 years undergoing conventional hemodialysis treatments 3 times per week for >6 months with residual urine output <150 ml/day. Exclusion criteria were as follows: patients with dialysis treatment time <3.5 h, missed dialysis treatment in the last 2 weeks prior to index study date, inadequate dialysis with spKt/V <1.2, change in target weight in the last 2 prior weeks, severe hyperglycemia (plasma glucose >15 mmol/L), liver cirrhosis, active infection or inflammatory disease, and hospitalization of any cause in the 4 weeks prior to the index study date.
For the predialysis serum sodium, the average of the last 3 monthly values prior to the index date was used. The sodium gradient was calculated using the prescribed dialysate sodium minus the average predialysis sodium. For the pre- and post-BP, IDWG, IDWG% (IDWG/prescribed dry weight) and UF rates, the average of the last 6 hemodialysis treatments prior to the index date was used. A sodium gradient cutoff of 3 mEq/L (<3 vs. ≥3 mEq/L) was used to categorize patients. The presence of intradialytic hypotension was defined as follows: in patients with a presystolic BP (pre-sBP) <159 mm Hg, reaching a nadir of sBP <90 mm Hg, and in patients with a pre-sBP >160 mm Hg, reaching a nadir of sBP <100 mm Hg in at least 30% of treatments. This definition was used as it has been shown to be associated with cardiovascular outcomes [11]. Intradialytic hypertension was defined as post-sBP – pre-sBP >0 [26].
Statistical Analysis
Baseline demographics and clinical characteristics are presented as means or medians and proportions, as appropriate, based on a sodium gradient >3 or ≤3 mEq/L. Comparisons were tested using the χ2 or Fisher exact test for categorical variables, and the Student t test for parametric variables. Correlations were assessed with the Pearson product-moment coefficient. The associations between sodium gradient and IDWG, UF rates, intradialytic hypotension and intradialytic hypertension were also examined using a logistic regression analysis. p values of <0.05 were considered statistically significant. All analyses were performed using SPSS version 20.0 (IBM Corp., USA).
Results
A total of 194 patients were screened for inclusion. After excluding the following patients (dialysis treatment <3.5 h [n = 16], missed dialysis treatment [n = 8], inadequate dialysis [n = 1], recent change in target weight [n = 2], severe hyperglycemia [n = 11], liver cirrhosis [n = 3], active infection or inflammatory disease [n = 9], and hospitalization in the 4 weeks prior to index date [n = 34]), 110 patients were included in the analysis.
Baseline Characteristics
The overall mean serum sodium gradient was 4.6 ± 3.6 mEq/L with a mean predialysis sodium of 137.4 ± 2.5 mEq/L and a mean dialysate sodium of 142.0 ± 3.0 mEq/L. Baseline patient characteristics are presented in Table 1. There was a higher proportion of males in patients with a sodium gradient ≤3 mEq/L compared to patients with a gradient >3 mEq/L (71.1 vs. 50.8%, p = 0.05). The mean predialysis serum sodium (139 vs. 137 mEq/L, p < 0.01) and the mean dialysate sodium (140 vs. 144 mEq/L, p < 0.01) were also significantly different among patients with a sodium gradient ≤3 mEq/L compared to those with a gradient >3 mEq/L. Furthermore, there were no patients with a predialysis serum sodium <135 mEq/L among patients with a gradient ≤3 mEq/L, whereas they represented 23% of the patients with a gradient >3 mEq/L. All other baseline characteristics were similar.
Table 1.
Baseline characteristics
| Na gradient ≤3 mEq/L (n = 45) | Na gradient >3 mEq/L (n = 65) | p value | |
|---|---|---|---|
| Mean age, years | 67 | 69 | 0.44 |
| Male sex, n (%) | 32 (71.1) | 33 (50.8) | 0.05 |
| Primary renal disease, n (%) | |||
| Diabetes | 16 (35.6) | 25 (38.5) | 0.46 |
| Hypertension | 11 (24.4) | 13 (20.0) | |
| Glomerulonephritis | 6 (13.3) | 10 (15.4) | |
| Polycystic kidney disease | 2 (4.4) | 2 (3.1) | |
| Other | 10 (22.2) | 15 (23.1) | |
| Access type, n (%) | |||
| CVC | 22 (48.9) | 35 (53.8) | 0.64 |
| AVF | 20 (44.4) | 28 (43.1) | |
| AVG | 3 (6.7) | 2 (3.1) | |
| Mean dialysis vintage, years | 6.5 | 5.1 | 0.16 |
| Mean dialysis time, h | 3.8 | 3.9 | 0.53 |
| Mean dialysate sodium, mEq/L | 140 | 144 | <0.01 |
| Mean serum sodium, mEq/L | 139 | 137 | <0.01 |
| Serum sodium subgroups, n (%) | |||
| <135 mEq/L | 0 (0) | 15 (23.1) | <0.01 |
| 135–139.9 mEq/L | 34 (75.6) | 44 (67.7) | |
| ≥140 mEq/L | 11 (24.4) | 6 (9.2) |
AVF, arteriovenous fistula; AVG, arteriovenous graft; CVC, central venous catheter. p values in bold are significant.
Hemodialysis Characteristics
When hemodialysis characteristics were compared (Table 2), the mean IDWG% was significantly lower in patients with a gradient ≤3 mEq/L compared with >3 mEq/L (2.4 vs. 3.5%, p < 0.01). Similarly, the mean UF rate was also significantly lower in patients with a gradient ≤3 mEq/L (7.2 vs. 9.6 mL/kg/h, p < 0.01). However, there was no difference in terms of pre- or post-BP, number of BP medication, episodes of intradialytic hypotension or presence of intradialytic hypertension between patients with a gradient ≤3 and >3 mEq/L.
Table 2.
Hemodialysis characteristics
| Na gradient ≤3 mEq/L (n = 45) | Na gradient >3 mEq/L (n = 65) | p value | |
|---|---|---|---|
| Mean pre-HD sBP, mm Hg | 136 | 139 | 0.40 |
| Mean pre-HD dBP, mm Hg | 64 | 62 | 0.44 |
| Mean post-HD sBP, mm Hg | 131 | 134 | 0.34 |
| Mean post-HD dBP, mm Hg | 64 | 64 | 0.94 |
| Mean IDWG% – IDWG/TW | 2.4 | 3.5 | <0.01 |
| Mean UF rate, mL/kg/h | 7.2 | 9.6 | <0.01 |
| Intradialytic hypotension, n (%) | 8 (17.8) | 12 (18.5) | 0.93 |
| Intradialytic hypertension, n (%) | 12 (26.7) | 28 (43.1) | 0.08 |
| Mean number of BP medications | 1.5 | 1.4 | 0.47 |
BP, blood pressure; dBP, diastolic blood pressure; HD, hemodialysis; IDWG, interdialytic weight gain; sBP, systolic blood pressure; UF, ultrafiltration; TW, target weight. p values in bold are significant.
Sodium Gradient and IDWG
The mean sodium gradient was significantly lower in patients with an IDWG% of ≤3% compared with >3% (3.2 vs. 6.3 mEq/L, p < 0.01). The sodium gradient positively correlated with increasing IDWG% (r = 0.48, p < 0.01, Fig. 1). In a logistic regression analysis, a 1 mEq/L higher sodium gradient had an OR of 1.33 (95% CI 1.17–1.52, p < 0.01, Table 3) of >3% IDWG%.
Fig. 1.
Sodium gradient and interdialytic weight gain. An increasing sodium gradient positively correlates with increased interdialytic weight gain (expressed as ratio of interdialytic weight gain to dry weight in percent). IDWG, interdialytic weight gain.
Table 3.
Logistic regression per 1 mEq/L increase in sodium gradient
| Odds ratio | 95% CI | p value | |
|---|---|---|---|
| UF rate >10 mL/kg/h | 1.16 | 1.02–1.33 | 0.03 |
| IDWG >3% | 1.33 | 1.17–1.52 | <0.01 |
| Intradialytic hypertension | 1.08 | 0.96–1.20 | 0.19 |
| Intradialytic hypotension | 0.99 | 0.87–1.14 | 0.98 |
IDWG, interdialytic weight gain; UF, ultrafiltration.
Sodium Gradient and UF Rates
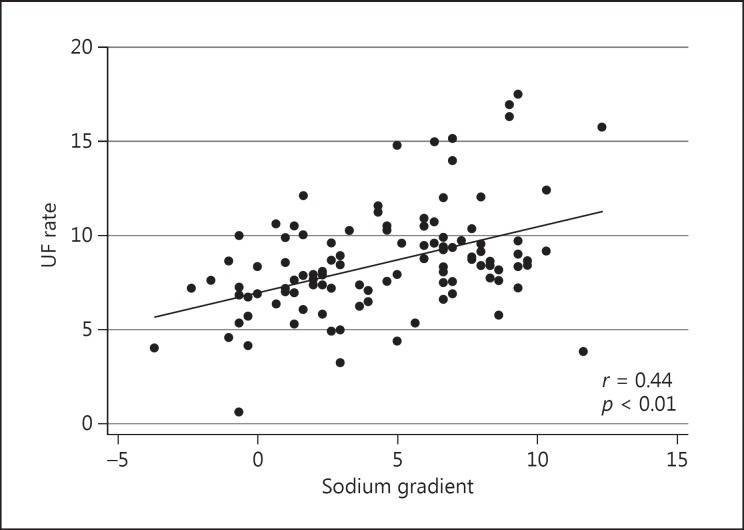
The mean sodium gradient was significantly lower in patients with UF rates ≤10 mL/kg/h compared with >10 mL/kg/h (4.2 vs. 6.0 mEq/L, p = 0.03) and the sodium gradient positively correlated with increasing UF rates (r = 0.44, p < 0.01, Fig. 2). In a logistic regression analysis, a 1 mEq/L increase in sodium gradient carried an OR of 1.16 (95% CI 1.02–1.33, p = 0.03, Table 3) for UF rates >10 mL/kg/h.
Fig. 2.
Sodium gradient and ultrafiltration rates. An increasing sodium gradient positively correlates with increased ultrafiltration rates (expressed in mL/kg/h). UF, ultrafiltration.
Sodium Gradient and BP
The mean sodium gradient was similar in patients with or without episodes of intradialytic hypotension. Moreover, the sodium gradient did not correlate with pre- or postdialysis BP values. A further logistic regression showed that the sodium gradient was not associated with increased risk of intradialytic hypertension or intradialytic hypotension (Table 3).
Patients with Predialysis Serum Sodium <135 mEq/L
When we excluded patients with a serum sodium <135 mEq/L, a positive correlation between the sodium gradient and IDWG% (r = 0.49, p < 0.01) or UF rates (0.45, p < 0.01) was still present.
Risk of Death and Hospitalization
With regard to the 6-month risk of hospitalization of all-cause mortality, there were proportionately more hospitalizations (30.8 vs. 17.8%, p = 0.12) and death (4.6 vs. 2.2%, p = 0.51) in patients with a sodium gradient >3 mEq/L, but these results did not reach statistical significance.
Discussion
Our study showed that a higher sodium gradient is associated with significant increases in IDWG and UF rates without an associated difference in intradialytic hypotensive episodes. We found no significant association between the sodium gradient and BP or number of antihypertensive medications. Thus, it appears that minimizing the sodium gradient is important given its association with these hemodialysis markers of fluid overload, which, in turn, are associated with increased cardiovascular morbidity and mortality. Our study suggests that a sodium gradient ≤3 mEq/L seems to be associated with favorable IDWG and UF rates. However, for the subset of patients with lower serum sodium levels (<135 mEq/L), the optimal sodium gradient cannot be concluded based on our study as all these patients had a gradient >3 mEq/L. This would particularly be important to investigate further, especially since lower serum sodium is associated with higher adjusted risk of death and a recent DOPPS study observed an interesting lower mortality risk in patients with serum sodium <137 mEq/L dialyzed against a dialysate sodium >140 mEq/L [18].
Our findings are consistent with the current literature demonstrating a positive correlation between the sodium gradient and parameters of fluid overload in hemodialysis patients [15, 16, 19–21, 23, 27, 28]. These associations of a high sodium gradient with fluid overload are likely explained by a high dialysate sodium concentration leading to an elevated postdialysis serum sodium level with the consequence of increased thirst and fluid intake [29]. Our results are in keeping with Munoz Mendoza et al. [16] who also found a direct correlation between IDWG and sodium gradient with no associations with the frequency of intradialytic hypotension episodes. Other studies have equally shown that a sodium gradient of >3 mEq/L is associated with fluid overload and adverse outcomes [24, 25]. Similarly, by decreasing dialysate sodium concentrations, Munoz Mendoza et al. [15] also demonstrated a significant decrease in IDWG without associated adverse events in patients undergoing in-center nocturnal hemodialysis. However, while Movilli et al. [26] showed an independent association between intradialytic hypertension and the dialysis sodium gradient, our results did not show a similar association, which could perhaps be related to our smaller sample size.
There are several strengths of this study. Firstly, at the time of this study, there were 2 different dialysate sodium strategies used at the 2 dialysis units which allowed for a range of sodium gaps to be studied. Although we did not collect data on the patients' cardiovascular status or echocardiogram results (if done), we limited our inclusion criteria to a stable cohort of prevalent hemodialysis patients. Our study does have some limitations given its single-institution nature and small sample size. Moreover, the finding of 23% of patients with serum sodium <135 mEq/L only in the high sodium gradient group suggests possible confounding by indication which could have contributed to some of the results, especially the lack of differences in intradialytic hypotension. Patients with lower predialysis sodium may have been treated with higher dialysate sodium to potentially prevent this occurrence. The actual dialysate sodium was also not measured and others have demonstrated a large difference in the actual measured versus prescribed dialysate sodium with differences ranging from −13 to +6 mEq/L [30]. We used standard hemodialysis BP monitoring rather than home ambulatory BP, the latter of which is more accurate in the hemodialysis population [31, 32]. Finally, an objective measurement of fluid status such as bioimpedance was not available.
Optimal fluid status is crucial in our dialysis population as it has an impact on quality of life, cardiovascular events, and mortality. Achieving euvolemia in our dialysis patients is therefore a high priority. Individualizing the dialysate sodium prescription to minimize the sodium gap may lead to less fluid overload in hemodialysis patients.
Statement of Ethics
This study was approved by the appropriate ethics committee and did not require informed consent.
Disclosure Statement
The authors declare no conflicts of interest. The results presented in this paper have not been published previously, in whole or part, except in abstract format.
References
- 1.Hur E, Gungor O, Musayev O, Usta M, Toz H, Asci G, Ozkahya M, Duman S, Ok E. Bioimpedance spectroscopy for the detection of hypervolemia in peritoneal dialysis patients. Adv Perit Dial. 2011;27:65–70. [PubMed] [Google Scholar]
- 2.Wizemann V, Wabel P, Chamney P, Zaluska W, Moissl U, Rode C, Malecka-Masalska T, Marcelli D. The mortality risk of overhydration in haemodialysis patients. Nephrol Dial Transplant. 2009;24:1574–1579. doi: 10.1093/ndt/gfn707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Agarwal R, Alborzi P, Satyan S, Light RP. Dry-weight reduction in hypertensive hemodialysis patients (DRIP): a randomized, controlled trial. Hypertension. 2009;53:500–507. doi: 10.1161/HYPERTENSIONAHA.108.125674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agarwal R, Andersen MJ, Pratt JH. On the importance of pedal edema in hemodialysis patients. Clin J Am Soc Nephrol. 2008;3:153–158. doi: 10.2215/CJN.03650807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dou Y, Zhu F, Kotanko P. Assessment of extracellular fluid volume and fluid status in hemodialysis patients: current status and technical advances. Semin Dial. 2012;25:377–387. doi: 10.1111/j.1525-139X.2012.01095.x. [DOI] [PubMed] [Google Scholar]
- 6.Reddan DN, Szczech LA, Hasselblad V, Lowrie EG, Lindsay RM, Himmelfarb J, Toto RD, Stivelman J, Winchester JF, Zillman LA, Califf RM, Owen WF., Jr Intradialytic blood volume monitoring in ambulatory hemodialysis patients: a randomized trial. J Am Soc Nephrol. 2005;16:2162–2169. doi: 10.1681/ASN.2004121053. [DOI] [PubMed] [Google Scholar]
- 7.Kalantar-Zadeh K, Regidor DL, Kovesdy CP, Van Wyck D, Bunnapradist S, Horwich TB, Fonarow GC. Fluid retention is associated with cardiovascular mortality in patients undergoing long-term hemodialysis. Circulation. 2009;119:671–679. doi: 10.1161/CIRCULATIONAHA.108.807362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Velasco N, Chamney P, Wabel P, Moissl U, Imtiaz T, Spalding E, McGregor M, Innes A, MacKay I, Patel R, Jardine A. Optimal fluid control can normalize cardiovascular risk markers and limit left ventricular hypertrophy in thrice weekly dialysis patients. Hemodial Int. 2012;16:465–472. doi: 10.1111/j.1542-4758.2012.00689.x. [DOI] [PubMed] [Google Scholar]
- 9.Hung SC, Kuo KL, Peng CH, Wu CH, Lien YC, Wang YC, Tarng DC. Volume overload correlates with cardiovascular risk factors in patients with chronic kidney disease. Kidney Int. 2014;85:703–709. doi: 10.1038/ki.2013.336. [DOI] [PubMed] [Google Scholar]
- 10.Lee MJ, Doh FM, Kim CH, Koo HM, Oh HJ, Park JT, Han SH, Yoo TH, Kim YL, Kim YS, Yang CW, Kim NH, Kang SW. Interdialytic weight gain and cardiovascular outcome in incident hemodialysis patients. Am J Nephrol. 2014;39:427–435. doi: 10.1159/000362743. [DOI] [PubMed] [Google Scholar]
- 11.Flythe JE, Kimmel SE, Brunelli SM. Rapid fluid removal during dialysis is associated with cardiovascular morbidity and mortality. Kidney Int. 2011;79:250–257. doi: 10.1038/ki.2010.383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Flythe JE, Xue H, Lynch KE, Curhan GC, Brunelli SM. Association of mortality risk with various definitions of intradialytic hypotension. J Am Soc Nephrol. 2015;26:724–734. doi: 10.1681/ASN.2014020222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stefansson BV, Brunelli SM, Cabrera C, Rosenbaum D, Anum E, Ramakrishnan K, Jensen DE, Stalhammar NO. Intradialytic hypotension and risk of cardiovascular disease. Clin J Am Soc Nephrol. 2014;9:2124–2132. doi: 10.2215/CJN.02680314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mc Causland FR, Waikar SS. Optimal dialysate sodium: what is the evidence? Semin Dial. 2014;27:128–134. doi: 10.1111/sdi.12182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Munoz Mendoza J, Bayes LY, Sun S, Doss S, Schiller B. Effect of lowering dialysate sodium concentration on interdialytic weight gain and blood pressure in patients undergoing thrice-weekly in-center nocturnal hemodialysis: a quality improvement study. Am J Kidney Dis. 2011;58:956–963. doi: 10.1053/j.ajkd.2011.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Munoz Mendoza J, Sun S, Chertow GM, Moran J, Doss S, Schiller B. Dialysate sodium and sodium gradient in maintenance hemodialysis: a neglected sodium restriction approach? Nephrol Dial Transplant. 2011;26:1281–1287. doi: 10.1093/ndt/gfq807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Basile C, Lomonte C. It is time to individualize the dialysate sodium prescription. Semin Dial. 2016;29:24–27. doi: 10.1111/sdi.12425. [DOI] [PubMed] [Google Scholar]
- 18.Hecking M, Karaboyas A, Saran R, Sen A, Horl WH, Pisoni RL, Robinson BM, Sunder-Plassmann G, Port FK. Predialysis serum sodium level, dialysate sodium, and mortality in maintenance hemodialysis patients: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Am J Kidney Dis. 2012;59:238–248. doi: 10.1053/j.ajkd.2011.07.013. [DOI] [PubMed] [Google Scholar]
- 19.Flanigan MJ. Role of sodium in hemodialysis. Kidney Int Suppl. 2000;76:S72–S78. doi: 10.1046/j.1523-1755.2000.07609.x. [DOI] [PubMed] [Google Scholar]
- 20.Flanigan MJ. How should dialysis fluid be individualized for the chronic hemodialysis patient? Sodium. Semin Dial. 2008;21:226–229. doi: 10.1111/j.1525-139X.2008.00428.x. [DOI] [PubMed] [Google Scholar]
- 21.Lomonte C, Basile C. Do not forget to individualize dialysate sodium prescription. Nephrol Dial Transplant. 2011;26:1126–1128. doi: 10.1093/ndt/gfr073. [DOI] [PubMed] [Google Scholar]
- 22.Peixoto AJ, Gowda N, Parikh CR, Santos SF. Long-term stability of serum sodium in hemodialysis patients. Blood Purif. 2010;29:264–267. doi: 10.1159/000274460. [DOI] [PubMed] [Google Scholar]
- 23.Santos SF, Peixoto AJ. Sodium balance in maintenance hemodialysis. Semin Dial. 2010;23:549–555. doi: 10.1111/j.1525-139X.2010.00794.x. [DOI] [PubMed] [Google Scholar]
- 24.Jin H, Lee SY, Lee SN, Song JH, Kim MJ, Lee SW. Effect of dialysate sodium concentration on sodium gradient and hemodialysis parameters. Electrolyte Blood Press. 2014;12:66–73. doi: 10.5049/EBP.2014.12.2.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Penne EL, Sergeyeva O. Sodium gradient: a tool to individualize dialysate sodium prescription in chronic hemodialysis patients? Blood Purif. 2011;31:86–91. doi: 10.1159/000321851. [DOI] [PubMed] [Google Scholar]
- 26.Movilli E, Camerini C, Gaggia P, Zubani R, Feller P, Poiatti P, Pola A, Carli O, Valzorio B, Cancarini G. Role of dialysis sodium gradient on intradialytic hypertension: an observational study. Am J Nephrol. 2013;38:413–419. doi: 10.1159/000355974. [DOI] [PubMed] [Google Scholar]
- 27.Davenport A. Negative dialysate to sodium gradient does not lead to intracellular volume expansion post hemodialysis. Int J Artif Organs. 2010;33:700–705. [PubMed] [Google Scholar]
- 28.Kumar S, Khosravi M, Massart A, Potluri M, Davenport A. Are serum to dialysate sodium gradient and segmental bioimpedance volumes associated with the fall in blood pressure with hemodialysis? Int J Artif Organs. 2014;37:21–28. doi: 10.5301/ijao.5000290. [DOI] [PubMed] [Google Scholar]
- 29.Munoz Mendoza J, Arramreddy R, Schiller B. Dialysate sodium: choosing the optimal hemodialysis bath. Am J Kidney Dis. 2015;66:710–720. doi: 10.1053/j.ajkd.2015.03.034. [DOI] [PubMed] [Google Scholar]
- 30.Gul A, Miskulin DC, Paine SS, Narsipur SS, Arbeit LA, Harford AM, Weiner DE, Schrader R, Horowitz BL, Zager PG. Comparison of prescribed and measured dialysate sodium: a quality improvement project. Am J Kidney Dis. 2016;67:439–445. doi: 10.1053/j.ajkd.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 31.Agarwal R, Andersen MJ, Bishu K, Saha C. Home blood pressure monitoring improves the diagnosis of hypertension in hemodialysis patients. Kidney Int. 2006;69:900–906. doi: 10.1038/sj.ki.5000145. [DOI] [PubMed] [Google Scholar]
- 32.Alborzi P, Patel N, Agarwal R. Home blood pressures are of greater prognostic value than hemodialysis unit recordings. Clin J Am Soc Nephrol. 2007;2:1228–1234. doi: 10.2215/CJN.02250507. [DOI] [PubMed] [Google Scholar]