Abstract
Curcumin is a constituent (up to ∼5%) of the traditional medicine known as turmeric. Interest in the therapeutic use of turmeric and the relative ease of isolation of curcuminoids has led to their extensive investigation. Curcumin has recently been classified as both a PAINS (pan-assay interference compounds) and an IMPS (invalid metabolic panaceas) candidate. The likely false activity of curcumin in vitro and in vivo has resulted in >120 clinical trials of curcuminoids against several diseases. No double-blinded, placebo controlled clinical trial of curcumin has been successful. This manuscript reviews the essential medicinal chemistry of curcumin and provides evidence that curcumin is an unstable, reactive, nonbioavailable compound and, therefore, a highly improbable lead. On the basis of this in-depth evaluation, potential new directions for research on curcuminoids are discussed.
Introduction
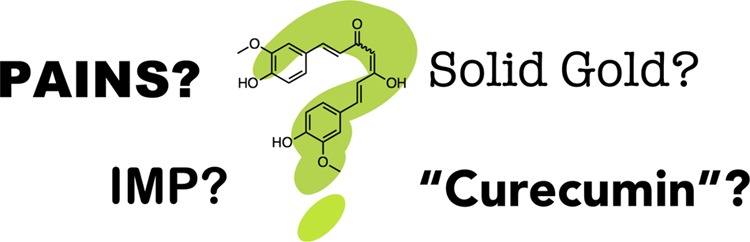
Natural products (NPs) form the basis for many widely used drugs. This utility was recently recognized on a larger stage, as the discoverer of artemisinin shared the Nobel Prize in Physiology or Medicine in 2015 with the discoverers of the anthelmintic avermectin family of NPs. Artemisinin, a NP discovered from a traditional Chinese medicine (TCM), Artemisia annua, was developed into an effective therapy for Plasmodium falciparum malaria. Some researchers viewed this award as a validation of the general utility of TCMs.1,2 In marked contradistinction to this claimed vindication of the role of certain ethnic and traditional medicines (TxMs) in medical practice are recent reports labeling curcumin, a constituent of the spice turmeric and part of the mixture of compounds referred to as curcuminoids, as both a PAINS (pan assay interference compounds)3 and an IMPS (invalid metabolic panaceas) compound.4 Additionally, many researchers have described the potential “dark side of curcumin”:5−9 the drawbacks noted for curcumin include its poor pharmacokinetic/pharmacodynamic (PK/PD) properties, low efficacy in several disease models, and toxic effects under certain testing conditions.5 These cautionary reports appear to have been swept away in the torrent of papers, reviews, patents, and Web sites touting the use of curcumin (and its primary commercial source, turmeric) as an anticancer agent,10,11 a therapeutic for Alzheimer’s disease,12 a treatment for hangovers,13,14 erectile dysfunction,15,16 baldness,17,18 hirsutism,19 a fertility-boosting,20 and contraceptive21 extract, collectively establishing the properties expected of a panacea.22,23
Scientific manuscripts are still published regularly that are based solely on the foundational premise of the reported activity and therapeutic utility of curcumin. In 2015, this plethora of data motivated the compilation of a Curcumin Resource Database (CRDB) that seeks to support the preclinical development of curcuminoids by putting over 1000 analogues and their alleged molecular target24 at the fingertips of researchers via a Web interface. The CRDB coverage of over 9000 publications and 500 patents demonstrates the magnitude of both the scientific interest and vast amount of dormant information that is awaiting a more global, medicinal chemistry interpretation. It is the goal of this manuscript to primarily review curcumin (1; Figure 1) and related curcuminoids, which are the species extracted from turmeric, and largely what is sold or tested in clinical trials.
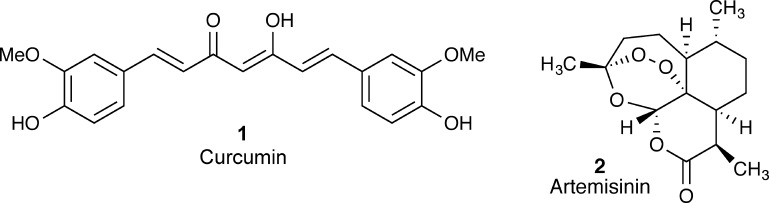
Figure 1.
Structural comparison of curcumin and artemisinin. Curcumin has been the focus of heavy research for new drug development. Artemisinin is an FDA approved antimalarial.
A simple analogy will help us set the stage for this Miniperspective. Artemisinin (2; Figure 1) has been shown to function like an effective long-range and targeted missile that homes in on heme-loving parasites and destroys them in a spectacular burst of nonselective reactivity.25 The peroxide-containing structure of artemisinin suggests that it would be unstable in a biological setting. However, its in vivo stability (T1/2 = 2.5 h; F = 30%)26 provides evidence that it is sufficiently stable, from a pharmacokinetic perspective, to be an effective therapeutic. Curcumin, on the other hand, is more like a missile that has shown excellent promise in early testing (in vitro), even though this testing may have been bedeviled by design problems that led to several misfires. The structure of 1 suggests that it might be unstable in a biological setting, and in fact, it is: both its in vitro and in vivo stabilities are abysmal (T1/2 < 5 min; F < 1%)27,28 relative to commercial drugs.
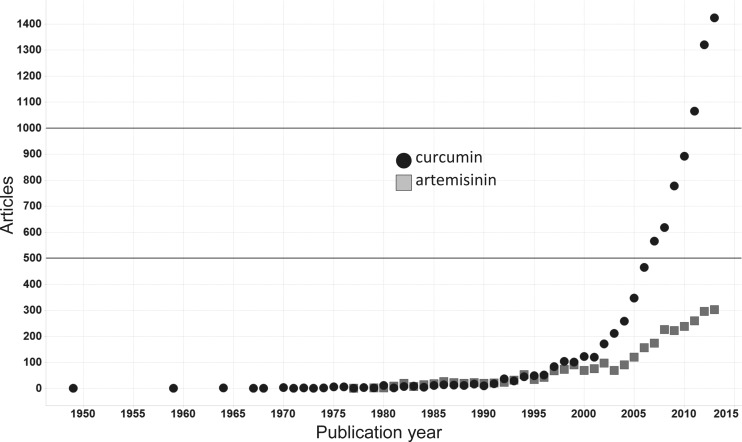
To our knowledge, compound 1 has never been shown to be conclusively effective in a randomized, placebo-controlled clinical trial for any indication.29 Curcumin is best typified, therefore, as a missile that continually blows up on the launch pad, never reaching the atmosphere or its intended target(s). These results have given curcumin the label of pharmacodynamically fierce (hits many targets) yet pharmacokinetically feeble (does not get to its targets).9 While these failures would normally end further research on its use as a therapeutic, they apparently have not deterred researchers interested in its development. Accordingly, major resources have been expended on research enterprises that involve curcumin as a key study agent. From 1995 to the present, according to the NIH RePORTER database (query of the term “curcumin” in keywords, titles, and abstracts),30 federal funds exceeding $150 million have been awarded for projects that are linked, directly or indirectly, to the biomedical exploration of curcumin. This result gives an approximate estimate of the order of magnitude of resources (not scientific significance) that are used directly or indirectly for experiments with curcumin and its analogues. Consequently, projects involving, for example, method development work where curcuminoids serve as model compounds are likely included in this estimation. However, this continued interest has resulted in the generation of manuscripts reporting biological studies of curcumin at a rate that far outpaces those published on artemisinin (Figure 2). This suggests that while artemisinin research has matured, curcumin research may have entered the steep section of the hyperbolic black hole of natural products (NPs)4 where effort rapidly exceeds utility, a common occurrence for IMPS. Furthermore, most NPs that have been successfully developed as drugs were discovered in phenotypic assays showing activity at or near a therapeutically relevant level. This allowed for the rapid development of the parent natural product or relatively straightforward analogue development to achieve a desired therapeutic effect.6 Such was the story for artemisinin, but careful analysis of the literature leads to a much different conclusion where curcumin is concerned.
Figure 2.
Comparison of publication frequency for biological studies of curcumin and artemisinin. The numbers of manuscripts per year were retrieved from SciFinder by searching for the substances curcumin (CAS no. 458-37-7) or artemisinin (CAS no. 63968-64-9) and then filtering by “biological study” and “document type” = journal. (Data accessed May 3, 2016.)
In this Miniperspective, we hope to address these questions regarding curcumin: PAINS, IMPS, or promise? Solid gold or just pyrite? Valuable lead for therapeutic development or still a tough challenge for NP and medicinal chemists? These are important questions, and they cannot be fully addressed even in this platform, as there are greater than 15 000 manuscripts published related to the biological interactions of curcumin, with ∼50 more manuscripts published each week. However, it is our goal to offer guidance and orthogonal perspectives to scientists and reviewers who may not have the time or resources to trek through the forest of curcumin literature. This is especially pertinent as articles relating to curcumin bioactivity appear in such a broad range of journals as to limit the ability of one to evaluate them all, due to both time and subscription limitations. By outlining the essential medicinal chemistry of curcumin, we aspire to improve the significance of science performed in the area of turmeric (and general NP) research and ensure that ever-precious research resources are spent most effectively. First, we will present evidence that curcumin is most probably an invalid lead compound, as can be shown by a critical evaluation of its PAINS and IMPS characteristics. Second, we will critically evaluate the physicochemical and pharmacokinetic/pharmacodynamic properties of curcumin responsible for its behavior in vitro and in vivo and tie these properties to the reported activity of curcumin against a variety of biological targets. Third, we will offer a critical look at a sampling of curcumin/curcuminoids clinical trials to put its therapeutic utility in context. The final section will compile the key points from the three discussion areas and seeks to identify new aspects that could potentially guide future research on this important traditional medicine.
Overview: Allure of the “Golden Spice”
Turmeric, the powdered rhizome of Curcuma longa, is extensively used as a spice in curries and mustards, is often responsible for their distinct color, and contributes much to their flavor due to the presence of its oleoresins and essential oil. Turmeric is a member of the ginger family (Zingiberaceae) and is prescribed abundantly for ailments in both traditional Chinese and Indian medicine.31 For example, turmeric preparations are applied to fresh wounds and bruises and as counterirritants for insect bites. Turmeric paste is used to facilitate scabbing in chicken pox and small pox. It is used in urologic diseases, hepatobiliary diseases and as an anthelminthic. Turmeric has also been described as a cancer remedy in Indian natural medical literature.
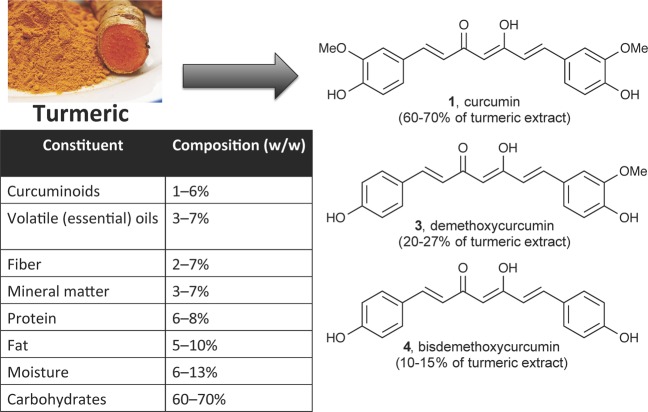
Major phytoconstituents of turmeric are diarylheptanoids, which occur in a mixture termed curcuminoids that generally make up approximately 1–6% of turmeric by dry weight.32 Most crude extracts prepared from turmeric, and even some refined “curcumin” materials, contain three major compounds (Figure 3): curcumin [1, (1E,6E)-1,7-bis(4-hydroxy-3-methoxyphenyl)-1,6-heptadiene-3,5-dione, typically 60–70% of a crude extract], demethoxycurcumin (3, 20–27%), and bisdemethoxycurcumin (4, 10–15%), along with numerous and less abundant secondary metabolites.33
Figure 3.
Major phytoconstituents of extracts of Curcuma longa. Compounds 1, 3, and 4, often grouped together as “curcuminoids”, generally make up approximately 1–6% of turmeric by weight.33 Of a curcuminoid extract, 1 makes up 60–70% by weight, while 3 (20–27%) and 4 (10–15%) are more minor components. The major constituent of a curcuminoid extract, 1, and the properties important for its consideration as a lead compound for therapeutic development are the focus of this review.
Although the multicomponent nature of “curcumin” is well documented, that fact and/or the unambiguous assignment of specific structures in a particular preparation is not always clear. Herein, the term “curcumin” will be used interchangeably with “curcuminoids” unless a more explicit description (e.g., of a single chemical structure) is deemed necessary. On the basis of our literature review, many in vitro studies use pure, synthetic 1, while most in vivo studies and clinical trials use a curcuminoid mixture. The dynamic nature of solubilized 1 makes it challenging to consider it a single compound in vitro or in vivo. However, regardless of the source material used in most studies, the structure of 1 is usually cited, perhaps by default, as designated active constituent that should be pursued for therapeutic benefit and is the compound used as a proposed “lead” structure for medicinal chemistry investigations. This Miniperspective will not attempt to address the potential therapeutic effects of even more complex turmeric extracts or preparations thereof but instead focuses on the reported utility of the chemical structure of the major constituent of these extracts: curcumin.
From a drug discovery standpoint, 1 appears to have several attractive qualities. There is a plethora of publications reporting a wide variety of biological activities for the compound(s), which is/are “generally recognized as safe” (GRAS) by the FDA as a food additive at levels up to 20 mg per serving,34 a designation that could conceivably help developers bypass some regulatory requirements for its approval as a therapeutic. This designation, along with the long historical and cultural use of turmeric as a medication, has contributed to its popularity as a dietary supplement marketed for many common ailments. Sales of curcumin supplements in the United States were reported to exceed $20 million in 2014, though a precise number is difficult to estimate.35 In concert with this boom in nutraceutical applications of curcumin, DSHEA (Dietary Supplement Health and Education Act) legislation establishing the legalities of dietary supplements in the United States (1994) and advents in in vitro testing likely contributed significantly to a sharp upturn in the publication of manuscripts regarding the use of curcumin in biological studies in the late 1990s (Figure 2). Since that time, curcumin has been reported to have activity for the following indications: anti-inflammatory, anti-HIV, antibacterial, antifungal, nematocidal, antiparasitic, antimutagenic, antidiabetic, antifibrinogenic, radioprotective, wound healing, lipid lowering, antispasmodic,36 antioxidant,37 immunomodulating, anticarcinogenic,38 and Alzheimer’s disease,39 among others. In many scientific and medicinal circles, these reported effects of curcumin have marked it as a source of future breakthrough therapeutics for complex diseases that are thought to require potent but nonselective therapeutics. In this uncritical enthusiasm for curcumin’s potential utility, its “dark side”5 is often disregarded. It is important, therefore, that any manuscript or research proposal that is based on the bioactivity (experimentally tested or computationally predicted) of curcumin or its analogues addresses additional characteristics of this natural product: its chemical instability, poor ADME properties, potential toxicological effects, and its lack of success to date in the clinic. These challenges will be addressed in further detail in subsequent sections.
Curcumin Is a PAINS, IMPS, and Poor Lead Compound
Curcumin Is a PAINS
PAINS, or pan-assay interference compounds, are compounds that have been observed to show activity in multiple types of assays by interfering with the assay readout rather than through specific compound/target interactions. Many compound classes have been codified and identified as PAINS or potential PAINS.40 Compound 1 exhibits all known PAINS-type behaviors: covalent labeling of proteins,41−43 metal chelation,44 redox reactivity,45 aggregation,46 membrane disruption,47 fluorescence interference,48 and structural decomposition.45,49 This suggests that any report of its activity in an assay that does not either exclude or account for these potential modes of assay interference should be treated with caution. This is a very important consideration for reviewers, for example, of U.S. federal proposals that rely on published data regarding the bioactivity of curcumin. The most recent guidelines for the review of U.S. NIH proposals require four new considerations to establish reproducibility: premise, design, variables, and authentication. Consequently, any proposal based on apparent curcumin bioactivity should ensure that the “scientific premise forming the basis of the proposed research” is sound (that is, published activity is not simply a result of assay interference) and that the “chemical resources” are “authenticated”; i.e., analytical and target engagement methods are employed to provide convincing evidence that curcumin is the causative agent of activity.
Curcumin Is an IMP
From a collective point of view, IMPS are invalid metabolic panaceas located inside the center of the black hole of natural products4 that tend to exhaust research resources. As singular elements, IMPS are prototypes of improbable metabolic panaceas that exhibit feeble performance as drug leads. The reported bioactive properties of IMPS are highly complicated by several factors that may be in addition to PAINS characteristics but often are separate from them.4 After evaluating bioactivity profiles of curcumin reported in the global literature, two broad observations raise red flags: (1) the high rate at which this compound, or mixture, is reported as being bioactive and especially (2) the relatively high ratio of positive activities seen in proportion to the total number of distinct bioactivities reported: just over 300 as assessed using the NAPRALERT database.4 NAPRALERT (www.napralert.org) is a relational database on the chemistry, biological activity, and folkloric use of natural products housed since 1975 at the Program for Collaborative Research in the Pharmaceutical Sciences at the College of Pharmacy, University of Illinois at Chicago. Founded by the late Professor Norman R. Farnsworth, NAPRALERT has since compiled data from more than 190 000 literature references, with records of over 200 000 distinct chemical compounds from more than 60 000 species of organisms. As a result, NAPRALERT covers hundreds of thousands of reports of biological activity tests (including in vitro, in vivo, and clinical results) for both natural product extracts (400 000+) and chemical isolates (300 000+).
Further IMPS considerations include the PAINS characteristics of 1, chiefly chemical aggregation,46 the presence of a reactive Michael acceptor,50 and fluorescence activity. This last attribute is particularly important as the main categories of reported activities in NAPRALERT (see also, Supporting Information Tables 1 and 2) emerge from cellular assays, which typically involve fluorescence and quenching for end point detection. A more detailed analysis of the distribution of positive activities reported in NAPRALERT shows that 28 distinct pharmacological activities, equivalent to less than 10% of all those captured, represent approximately 50% of the total reported activities for 1. In contrast, in cases of successful NP-based drug leads such as artemisinin, ivermectin, and paclitaxel, this ratio is only between 1% and 2%. This distinctive “broad bioactivity profile” associates 1 closely with the top 100 compounds with the most promiscuous bioactivity reported. Of these top 100, the ginsenosides Rb-1 and Rg-1, genistein, quercetin, apigenin, nordihydroguaiaretic acid, resveratrol, kaempferol, and fisetin are the only compounds with even more distinct reported activities than 1. While this means that these nine compounds have a wide range of positive results in bioassays, it does not automatically mean that their pharmacological effects cover such a wide range in practice. It is equally notable that, just like 1, none of these nine compounds, or any of their derivatives, have reached maturity as a drug lead to date.
One of the most plausible explanations regarding the observed polypharmacology of curcumin, besides its apparent PAINS/IMPS character, promiscuous bioassay profile, and chemical instability (vide infra), is the variable purity status and widespread lack of characterization of “curcumin” materials. This unknown mixture represents what is termed static residual complexity (static RC; see also https://go.uic.edu/residualcomplexity):51,52 the assumed bioactive material and any impurities are present and constant throughout the bioassay. The high variability of curcumin preparations and sources makes static RC an important factor of variability and can lead to unpredictable or potentially irreproducible results. In contrast, dynamic residual complexity (dynamic RC)52 is related to metabolic instability, a property that applies particularly to 1. The typical time frame for the biological experiments reported in NAPRALERT allows for significant degradation of 1 (vide infra). The degradation products will very likely have distinctly different in vitro and/or in vivo biological activities from the parent compound. In addition, biogenic metabolites are often different from the degradation products present in buffers or laboratory storage conditions, and the extended incubation times of many cellular assays make it difficult to know which degradation products are present and at what concentrations.52 For example, a recently identified degradation product of 1 is a spiroepoxide, which is highly sensitive to acids and reacts readily with thiols.53 This report indirectly emphasizes the relevance of dynamic RC by hypothesizing that the polypharmacology of 1 may in part, or even largely, be due to the sum of its degradation products.
Both the static and dynamic RC issues, as well as promiscuous reactivity, make the study of 1 a true challenge for both biologists and chemists, even when performed in close collaboration. Complex chemical characterization procedures need to be established and undertaken before starting biological experiments to control the initial material and characterize the remaining components at the end of the experiment (allowing the assessment of any degradation of the studied material). From the pharmacologist’s or biologist’s point of view, controlling chemical aggregation, target specificity (especially when using proteins), and photochemical conditions (absorbance, fluorescence, quenching, etc.) is paramount for achieving interpretable assay readouts and meaningful biological outcomes.
Curcumin Is a Poor Lead Compound
Compound 1 is completely out of balance as a lead compound when its PK and PD properties are weighed. While there are exceptions and some discrepancies about what makes a “good” lead, a prototypical lead compound for therapeutic discovery and development generally has less than 1 μM potency at its desired target(s), evidence of selectivity and tractable mechanism(s) of action, good bioavailability, chemical stability, and ADMET (absorption, distribution, metabolism, excretion, and toxicology) qualities that can be optimized in a reasonable number of synthetic cycles.54 Compound 1 has none of these features. Moreover, attempts to improve its ADMET qualities (typically the most difficult properties of a compound to optimize) and increase its specificity via chemical optimization and various formulations have thus far been unsuccessful. Optimization of the PK/PD of 1 may be impossible given the multiple structural features presumably responsible for its “desirable” activity. For example, one property often marked for optimization is indiscriminate thiol reactivity (particularly with proteins), though this is most likely a chief explanation for much of its polypharmacology. Of course, covalent reactivity can be useful in the development of therapeutics.55−62 However, this mode of action is either purposefully designed into the drug as part of the discovery process or installed after optimization of potency and ADMET properties. For example, α,β-unsaturated reactive groups are often purposefully introduced into optimized, stable compounds to increase their potency and selectivity. Optimization to improve the feeble PK of 1 will most likely lead to concomitant dulling of its PD ferocity.
Chemical (In)Stability45,49
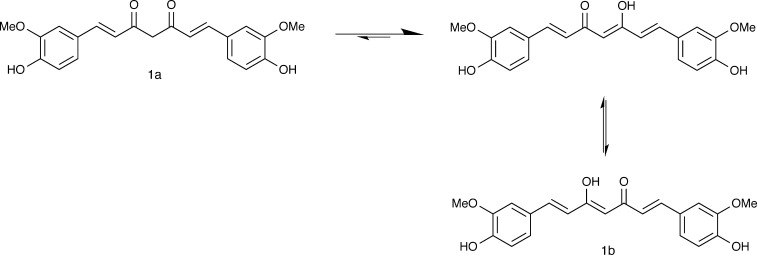
The structure of 1 contains a β-diketone moiety that readily undergoes keto–enol tautomerization (Figure 4). NMR studies using a variety of solvents at pH 3–9 have confirmed that the enol tautomer (1b), rather than the diketone (1a), is the only form of the molecule present at any detectable level in solution.63 This preference for 1b leads to a planar, intramolecularly hydrogen-bonded structure both in solution and in powder form.64 The calculated log P of 1 has been reported between 2.3 and 3.2, and it is practically insoluble in water at room temperature and neutral pH.9,65 At alkaline pH, the phenols are transformed to the phenolates, enabling the dissolution of 1 in water. A range of pKa values, 8.5–10.4 for the first and 9.5–10.7 for the second, have been reported for the phenolic protons depending on the solvent and method of measurement.48 However, at both neutral and alkaline pH, 1 degrades rapidly. Compound 1 is more structurally stable in an acidic environment, but the equilibrium shifts toward the neutral form (low/no solubility) of the molecule in parallel with decreasing pH.27,64 Therefore, studies in buffered solvents typically involve first dissolving 1 in a polar protic organic solvent, like methanol, then diluting it in an excess of the aqueous solution.
Figure 4.
Tautomerization of compound 1. NMR studies show that compound 1 is not present in solution as the diketone (1a) but only as a mixture of the equally present (due to symmetry) enol structures (1b).63
The conjugated system of 1 absorbs in the visible range (408–500 nm),48 and this property has been used to study its degradation in various buffers through spectroscopic and HPLC methods (see also Supporting Information Table 2). At neutral pH (7.5) and rt in aqueous buffer, the t1/2 for loss of 1 as the parent compound is approximately 20 min.66 When the temperature is increased to 37 °C, the reported t1/2 at pH 7.2 is less than 10 min.27 This report of rapid degradation upon heating led to a more thorough investigation of the degradation products of 1. It is known that 1 is photoreactive, as a 5% reduction in parent material is observed simply when preparing samples in clear versus amber glass.27 Compound 1 degrades by two main pathways: solvolysis and oxidative degradation. The solvolysis (nucleophilic substitution or elimination by solvent molecules) of the heptadienedione chain in aqueous alkaline buffer results in 90% compound degradation within 30 min. The major identified products are vanillin (5), ferulic acid (6), and feruloylmethane (7, Figure 5A). While the relative abundance of these degradation products differs at different incubation pH or temperature, they are also observed upon incubation of 1 in cell culture medium (RPMI 1640, Roswell Park Memorial Institute medium) and human blood.27 Recent spectroscopic analysis has revealed that solvolysis is only a minor pathway, and the major chemical degradation product is a bicyclopentadione (8) that is produced by autoxidation (Figure 5B).66 The spontaneous, free-radical-driven incorporation of O2 leads to oxygenation and double cyclization of the heptadienedione chain connecting the two methoxyphenol rings.67 Further study of the kinetics of radiolabeled compound decomposition has also identified several additional degradation products that likely appear on the pathway to compound 8 formation.45 This oxidative reaction occurs without photochemical initiation and may account, in part, for the reported antioxidant properties observed for compound 1. These degradation pathways suggest that dynamic RC (vide supra) should be considered when interpreting the outcome of bioassays involving 1.
Figure 5.
Major chemical degradation pathways of compound 1. (A) Solvolysis under alkaline pH in buffered aqueous solution rapidly leads to multiple fragmentation byproducts.27 (B) Autoxidation in buffered medium creates a bicyclopentadione (8) that is the major degradation product in aqueous conditions.66 (C) Photodegradation of 1 can occur when in crystalline form and dissolved in organic solvent.68 (D) When dissolved in certain organic solvents (like isopropanol), photodegradation can include reaction with the solvent as a substrate.69
While oxidative degradation does not require photochemical initiation, photochemical degradation of 1 does occur in both the crystalline and solubilized forms. Crystalline 1 is degraded by exposure to sunlight to give primarily 5, 6, ferulic aldehyde (9), and vanillic acid (10, Figure 5C).68 The same degradation pattern is observed for 1 in organic solvents when it is exposed to light. Several solvent-dependent products are also formed. In methanol, isopropanol, and chloroform, an internal cyclization product is formed. Isopropanol can also behave as a reactive substrate, leading to the formation of a guaiacol derivative (11, Figure 5D).69 The mechanism of photochemical degradation is caused mostly by type I and type II reactions with molecular oxygen, which has been described in detail elsewhere.9
The chemical stability of 1 can be improved by encapsulation with lipids or nanoparticles.70,71 Other attempts at improving stability have included synthetic manipulations to remove or protect the oxidation sites (phenolic and enolic hydroxyls)72 and derivatization of the β-diketone to reduce the activity of the enolate Michael acceptor.73,74 While analogues of 1 may be a more viable route to the development of a stable molecule for in vitro or in vivo evaluation, they will need to be evaluated as entirely new chemical entities and are largely outside the scope of this discussion.
The rapid degradation of 1 brings many additional requirements for its investigation in an in vitro or in vivo setting. Stability of 1 under the assay conditions should always be demonstrated. This analysis has not been reported in the vast majority of the publications reviewed here. Additionally, several publications have used computational methods to predict the activity of 1 or to explain the bioactivity observed experimentally.75,76 Because 1 is likely not present in situ, or at least its bioactivity is confounded by the presence of multiple reactive and/or bioactive degradation products, these models are less relevant to the targets of interest. Even when computational studies have accounted for the binding characteristics of the degradation products, other probable mechanisms of interference have not been considered.77
A primary requirement for most pharmaceuticals is stability under physiological conditions (a surrogate for in vivo conditions) and stability under storage conditions or in formulations. Physiological conditions here are considered an aqueous environment at pH 7.4 and 37 °C. Compound 1 has none of these characteristics and displays prominent chemical instability. Below, we highlight several other concerns regarding the physicochemical properties of 1 that could explain its promiscuous reactivity; these also need to be addressed when studying this molecule in vitro or in vivo.
Physicochemical Properties
The chemical instability of 1 is most likely the key property responsible for confounding the results of in vitro and in vivo measurements of its bioactivity and for undermining computational predictions of its potential binding and activity in biological assays. Compound 1 also displays undesirable physicochemical properties relative to known drugs. In addition to being unstable, it forms chemical aggregates (colloids) under common biochemical assay conditions.46 Adding the nonionic detergent Triton X-100 attenuates the activity of 1 versus AmpC β-lactamase (IC50 from 12 μM to >30 μM), malate dehydrogenase (IC50 from 9 μM to >30 μM), and HIV-2 protease (IC50 from 9 μM to >100 μM). This pattern is consistent with chemical aggregation and has been further confirmed by DLS (dynamic light scattering).46,78 These studies describe a critical aggregation concentration between 10 and 20 μM for compound 1. This is highly relevant because it corresponds to common compound testing concentrations in many of the investigational assays we encountered. Enzymatic inhibition by colloidal aggregates is stoichiometric, meaning that at a given compound concentration, the real concentration of enzyme is much lower. Once a chemical colloid is saturated with protein (be it enzyme or carrier protein), any unbound enzyme is free to react in the assay system.79,80 Consequently, apparent in vitro selectivity can be influenced by the relative protein concentrations in selectivity counterscreens (i.e., all proteins present: enzyme, carrier, and substrate proteins) and does not always reflect selectivity via traditional compound–ligand interactions. This also means that counterscreens with excess enzyme may appear less susceptible to aggregating compounds, helping to identify this circumstance. These phenomena deserve special consideration when designing experiments that include detergent-free assays.
In the event that the observed activity is not found to be due to assay interference, the instability of compound 1 calls into question the identity of the “active” compound.45 It is important to consider the cellular location of the target protein, as 1 has been shown to perturb cell membranes. This can lead to membrane perturbation being mistaken for specific binding to membrane-associated proteins.47 This could have significant ramifications for many reported activities, including those for ion channels, transporters, and growth factors. Beyond these factors, the fluorescence properties of 1 must also be taken into account in many biological experiments. The absorbance (∼408–500 nm) and emission (∼450–600 nm) of 1 varies greatly depending on solvent, but largely falls within the range of wavelengths common for many fluorescence-based bioassays.48,81
Other physicochemical properties of 1 are important considerations when developing assays or evaluating druglike properties. Notably, 1 is nearly insoluble in water at room temperature and neutral pH, estimated at 1–10 μg/mL. This can only be viewed as an estimate, however, as the true solubility is confounded by the high propensity for aggregation.64 Both the estimated ClogP (2.3–3.2) and topological polar surface area (93.1 A2) fall in the range of known chemical aggregators.78 X-ray crystallography studies with compound 1 also confirm its rapid degradation in aqueous media. Crystallization of 1 with transthyretin revealed both the parent compound and compound 6 (a known degradation product) associated with the protein.77 When considering molecular modeling, studies based on both the diketone (1a) and enol (1b) forms have been reported but fail to recognize the complete lack of solubility of one form (1a, diketone) and the complete instability of the other (1b, enol).
Beyond the concerns of chemical and physicochemical stability, compounds taken in vivo require appropriate PK/PD properties. Next, we highlight several concerns that should be addressed when using compound 1 in vivo.
ADMET (Absorption, Distribution, Metabolism, Excretion, and Toxicology)
In addition to the poor chemical stability and multiple modes of assay interference displayed by compound 1, it is generally accepted that its pharmacokinetic properties are poor.7,82
Absorption
The absorption of any potential therapeutic is a critical consideration, especially for oral dosing. Several studies, including clinical trials, have been performed using curcumin in a variety of oral dosing formulations. An oral dose of up to 12 g/day has been given with no adverse effects.83 While this high dose was relatively well tolerated, the absorption of the compound is negligible. All clinical studies reviewed here reported that 1 could not be detected in the serum of the majority of test subjects (including those dosed at 12 g/day). This is not surprising, as the reported oral bioavailability of synthetic 1 in rats is less than 1%.28 Moreover, compound 1 has displayed poor permeability in the standard Caco-2 model system (Papp = 3.18 × 10–6 ± 1.08 × 10–6 cm/s),84 which is a widely accepted predictor of cell permeability (poorly permeable compounds have Papp < 5.0 × 10–6 cm/s).85 Several groups have attempted to improve the absorption and bioavailability of 1 through various formulations. We note that lipid dispersions and nanoparticle systems have been developed for 1, with modest improvement in the absorption and bioavailability of the compound.82
Distribution
The extent to which a compound distributes through the body has a large impact on its therapeutic utility. While the distribution of compound 1 has been extensively studied in rats, it has only been sparingly evaluated in humans. Several studies in rodent models have reported variable distribution across tissue types.9,82,86 This high degree of variability is likely due to (1) differences in the preparation of the dose used in the study, (2) differences in extraction, preparation, and detection methods of 1, and (3) lack of specificity in the detection assay. Many assays we analyzed in the literature utilized HPLC-based detection without the added specificity of confirmation of identity by MS. These methods inherently have larger amounts of error as biological impurities, and degraded or transformed compounds could have similar retention times and absorbance properties as the parent compound. In fact, a study comparing the distribution of [3H]-1 to unlabeled 1 found substantially more radioactivity in tissues compared to the amount of unlabeled 1. This result supports the observation that 1 is degraded and/or transformed before and/or after absorption.87,88 Together, these studies suggest that the parent compound does not distribute to any specific organs in appreciable levels.
Metabolism
In part due to its reactive structure, any 1 that is absorbed by the body has a high potential to be metabolized. Extensive studies have been done on 1 in human liver microsomes. Phase I metabolism primarily results in reduction of the double bonds in the heptadienedione system, mainly through the action of alcohol dehydrogenase.82 Phase II metabolic processes rapidly conjugate 1 and its reduced metabolites. The most abundant conjugates are glucuronides and sulfates at the phenolic positions. Unsurprisingly, 1 also interacts readily with glutathione in a nonenzymatic manner, presumably through a Michael-type addition.89 Some of the formulations investigated to improve the oral bioavailability of 1 also hope to slow down the observed high rate of metabolism upon absorption. Unfortunately, it appears that once 1 is released in vivo, it has a high potential for modification by both first and second phase metabolism.
Excretion
The majority of 1 ingested by oral dosing is excreted in the feces, as determined in multiple studies in rats. Very little is detected in rodent urine; however glucuronide and sulfate metabolites have been identified in rat plasma.88,90 There are conflicting reports regarding the excretion of 1 and its metabolites in human subjects. In one study, neither the parent compound nor its metabolites were detected in blood or urine of human subjects after oral dosing, but 1 was recovered from feces.91 In two other studies, 1(92) or one of its metabolites93 was detected in serum of one or three patients from each cohort of 12 or 15 patients, respectively. In a fourth study, 1 was detected in serum of only one subject, but the glucuronide and sulfate conjugates were detected in all subjects.94 Similar to the reports of absorption, some of this variability in reporting likely comes from variability in the source material and methods of dosing and sample collection, preparation, and detection. Small amounts of compound 1 may be absorbed and excreted unchanged or, if we consider other physicochemical properties (vide supra), may not be absorbed but simply pass directly to the feces. Metabolized 1 is generally excreted in urine as the glucuronide and sulfate conjugates. The remainder of any dose, whether absorbed or not, is likely degraded beyond detection by the time it is excreted.
Toxicology.7,95−98
In addition to the therapeutic targets discussed below, 1 (and its degradation products) shows broad reactivity against a number of human enzymes that are linked to compound toxicity, namely, hERG channels, cytochrome P450s, and glutathione S-transferase (see also Supporting Information Table 3). The reactivity of each of these classes has important implications for potential toxic side effects: hERG channel inhibition is related to cardiotoxicity;99−101 cytochrome P450 (CYP450) and glutathione S-transferase (GST) inhibition can lead to impaired detoxification and potential toxic drug–drug contraindications.102 Beyond specific enzyme toxicity, compound 1 has recently been shown to be an active iron chelator in vivo, inducing a state of overt iron deficiency in mice fed diets poor in iron.44 This suggests that 1 has the potential to affect systemic iron metabolism, particularly in people with a preexisting suboptimal iron status. In studies of therapeutic utility, 1 has been reported as cytotoxic against a number of important cancer cell lines. What is infrequently noted, however, is that it also shows cytotoxicity against normal human lymphocytes.31 Surprisingly, data on the cytotoxicity of 1 against normal (noncancerous) cell lines are sparse. A recent report demonstrated cytotoxicity of 1 against a murine macrophage cell line and human kidney cells at IC50 values of 31 and 15.2 μM, respectively.8 These values are at or below those reported for several therapeutic targets or cell lines (see also Supporting Information Tables 1 and 3), suggesting that 1 might be generally cytotoxic and does not show a preference for normal versus cancerous cells.
ADMET Summary
The observed ADMET properties of 1 are not surprising given its chemical structure and physicochemical properties. The numerous papers that suggest 1 has utility as a therapeutic agent have led to a large field of study focusing on the improvement of its PK properties. We would emphasize caution, however, as such improvement in PK may actually lead to exacerbation of the toxicological side effects of 1, given its cytotoxic effects.8 Fundamental medicinal chemistry principles, and available ADMET evidence, incline us to hypothesize that the observed high tolerance in humans and low rate of adverse events is likely due to its poor absorption and low bioavailability. As an alternative approach, it may be possible for compound 1 to have an effect on human health without being absorbed. Emerging research suggests that 1 could affect the gut microbiota, which has been linked to several chronic diseases.7 A recent study using a mouse model of colitis-associated colorectal cancer suggests that compound 1 may have a chemopreventive effect that is correlated to changes in the microbiota of these animals.103 This hypothesis has yet to be fully validated but may ultimately provide focus for studies on the use of 1 as a therapeutic.
Critical Analysis of Some Reported Activities of Curcumin (Real and Virtual)104,105
Compound 1 is reported to be active at multiple biological targets. What is not typically acknowledged in these focused studies is that it is nonselective for what could be considered “good” versus “bad” targets (vide supra). A comprehensive discussion of the structure–activity (and reactivity) of 1 has been published.106 In summary, every functional group in 1 probably contributes to its reactivity and its apparent activity. For example, it is not surprising that compound 1 covalently modifies a number of biological proteins given that its two α,β-unsaturated systems are potent Michael acceptors for −SH groups with low pKa values. Additionally, the two phenolic groups are susceptible to redox transformations, and the 1,3-dicarbonyl is an excellent chelator of metal ions. It is important to consider the reported activities of 1 in light of these reactive functional groups in addition to the other properties detailed above. Examples of this critical consideration are presented below as case studies (see also Supporting Information Table 1). One common theme in these reports is particularly disturbing: published bioactivity data of 1 are typically not evaluated critically before it is used to justify further research in an area. This is especially troubling when the original activity reports have been retracted.107−112
Activity Case Studies
p300
Compound 1 is reported to inhibit the histone acetyltransferase (HAT) p300 at low micromolar concentrations in vitro.11,113 In one of these original studies, counterscreens failed to show any activity versus the HAT PCAF, the histone methyltransferase G9a, or the histone deacetylase HDAC1.113 Since the original publication of this bioactivity, there have been dozens of reports that have used 1 as a tool compound to modulate HATs in cell-based and organism-based experiments across many biological systems:114 mouse neuroblastoma cells,115 parasites,116 viruses,117 and a variety of human cell lines.118−121 Several points should be made about the original data.113 First, in vitro testing was performed without detergent and often at compound concentrations above the threshold for colloid formation (vide supra). It is reasonable that aggregates of 1 could have contributed to the in vitro assay readouts and perhaps the apparent selectivity (e.g., enzymatic modulation by chemical aggregation can be mitigated by increased levels of proteins). Second, 1 was allowed to preincubate with the targets in most of the assays.113 Given its reported instability in aqueous solutions, it is difficult to draw conclusions about the nature of compound–target interactions without additional stability data under these specific testing conditions. Third, another report showed that radiolabeled 1 binds covalently to p300 in a manner consistent with Michael addition, yet failed to inhibit the HATs PCAF or Gcn5 in vitro.11 The apparent selectivity of 1 for p300 reported nearly a decade ago may be a function of the intrinsic susceptibility of each HAT to thiol-reactive compounds. Selectivity in such a case would be a function of the thiol solvent accessibility, the number of thiols in the target protein (also the overall assay), and the protein conformational changes induced by any thiol modification. As an example, during an investigation of thiol-reactive PAINS, the highly thiol-reactive probe CPM consistently showed less potent inhibition of yeast GCN5 compared to yeast Rtt109 and human p300.122 Fourth, several kinetic experiments were performed that suggest 1 does not bind to the p300 active site.113 These experiments appear to be performed without ruling out reversibility or time dependence, and it is possible these kinetic results may be confounded by chemical reactivity as well as compound stability and chemical aggregation. Without question, compound 1 can inhibit p300 HAT activity in vitro based on the published data. Whether or not this inhibition is therapeutically useful, especially in a cellular context, is considerably more controversial. When phenotypes or changes in histone acetylation are observed in cells or whole organisms, these downstream effects are often attributed carte blanche to the inhibition of p300 while downplaying or outright disregarding other potential mediators of cellular histone acetylation such as HDACs or other HATs. This logic is overly simplistic and often flawed when used as supporting evidence for studying specific pathways.
HDAC8
In one report primarily driven by molecular modeling studies, compound 1 was reported to inhibit HDAC8 at midmicromolar compound concentrations (IC50 = 115 μM).123 On the basis of the title (“potent histone deacetylase inhibitors”), one may be led into thinking 1 could serve as a tool compound for epigenetic studies. As in the p300 example, the relevant in vitro assays omit detergent to mitigate chemical aggregate formation, a potential confounder that is highly likely in this system given the relatively high compound concentrations tested. In addition, the enzyme source from which the IC50 value was derived, HeLa nuclear extracts, should contain multiple HDACs, making it impossible to confidently gauge HDAC8-specific inhibition. No controls were performed to account for readout interference, such as fluorescence quenching or autofluorescence. Orthogonal counterscreens are absent, and there is no evidence presented for direct target engagement (e.g., ITC, X-ray crystallography, or SPR). The heavy reliance on molecular modeling is problematic, including the reporting of theoretical binding constants. Despite these liabilities, subsequent reports cite curcumin for its ability to specifically modulate HDACs.124−126
GSK-3β
Compound 1 is reported to be a potent inhibitor of GSK-3β (IC50 = 66 nM).127 However, detailed analysis of the in vitro testing conditions may help rationalize this level of potency. First, the reported concentration of GSK-3β protein present in the assay was in the femtomolar range, meaning several orders of magnitude stoichiometric excess of compound 1 are still needed to appreciably inhibit GSK-3β activity. Second, the biochemical assay was performed in the absence of thiol-scavenging agents like DTT, meaning 1, or any potential degradation products, could still react with the assay target or substrate. Third, as with previous examples, the assays were performed with incubation times sufficient for compound degradation (30–90 min),127 without meaningful counterscreens for selectivity and without mechanistic studies to demonstrate therapeutically useful target engagement. In retrospect, the heavy reliance on molecular modeling is problematic without confirmation of compound stability in the assay conditions. Nevertheless, curcumin is still the subject of numerous studies involving GSK-3β.128−131
Tau and Amyloid Fibril Formation
Compound 1 was tested as an inhibitor of tau fibril formation as part of the NIH MLPCN (Molecular Libraries Probe Centers Network) campaign. The tested substance showed promising activity in the primary thioflavin T (ThT) fluorescence-based qHTS (IC50 = 3.5 μM). However, it was inactive in a fluorescence polarization (FP) based secondary screen. Compound 1 was still active in a counterscreen for total fluorescence (IC50 = 13 μM), suggesting its activity was due in large part to compound-mediated fluorescence interference. For these reasons, it was not selected for additional follow-up based on these data. This example demonstrates the utility of a well-designed screening tree, complete with secondary assays and assay-specific counterscreens.132
Additionally, 1 has been reported as an inhibitor of amyloid-β (Aβ) fibril formation and mediator of Aβ cytotoxicity, also using the ThT assay as a primary readout (IC50 = 1–64 μM).7,133 Subsequent publications have shown that 1 is highly absorptive in the same spectral range as ThT.134 Most recently, transmission electron microscopy has shown that compound 1 does not affect the aggregation of Aβ in vitro.135 This report attempts to explain the observed cellular protective effects by showing that the oligomers formed by Aβ in the presence of 1 are nontoxic; i.e., the polyclonal antibody A11, which is reported to specifically detect toxic Aβ oligomers, does not detect these oligomers.136 However, the extremely long incubation times reported here would require follow-up to exclude the likely possibility of aggregation or degradation in the assay conditions.137
CFTR (Cystic Fibrosis Transmembrane Conductance Regulator)
In 2004, compound 1 was reported as a calcium-adenosine triphosphatase pump inhibitor for the treatment of cystic fibrosis (CF).138 The compound was tested in a mouse model based on previously reported in vitro activity (5–15 μM) in a related SERCA (sarcoplasmic/endoplasmic reticulum calcium) pump assay. The assay readout required the release of ΔF508-CFTR protein from the endoplasmic reticulum, which would increase calcium ion flux, a process that is known to be deficient in CF patients. These studies were followed by an investigation using a mouse model that expresses mutant CFTR, which showed that a dose of 45 mg kg–1 day–1 oral administration of 1 ameliorated phenotypic deficits in these mice. However, no orthogonal assay was used to confirm target engagement, and there was no confirmation of 1 in the blood of these animals. The improvement of ion channel conductance in these studies could be largely due to the disruption of cellular membranes by 1 (vide supra), thereby increasing ion release. Follow-up studies by an independent lab were unable to reproduce these in vitro and in vivo results.139 The measured concentration of 1 in vivo peaked at 60 nM, 30 min after oral dosing at 100 mg/kg, but was not detectable below this dosing level. While publications continue to point to compound 1 as a CFTR modulator as a potential CF treatment,140 no confirmation of CFTR activity has been published.
CB1
In 2009, compound 1 was reported as a potent, selective inhibitor of human and mouse cannabinoid receptor 1 (CB1).141 The initial report should raise some concern as the assay had a 90 min incubation time of 1 with the receptor at room temperature, conditions known to result in rapid compound degradation (vide supra). These results are, therefore, confounded minimally by the formation of degradation products. In addition, there is no orthogonal evidence presented of direct target engagement. Approximately six months after the publication of these results, the manuscript was retracted.142 According to the letter of retraction, both the authors and three external labs were unable to reproduce the original results. In repeated experiments, compound 1 was a low micromolar inhibitor of both CB1 and CB2 and showed no selectivity. The original authors hypothesized that their results were due to sample contamination by their CB1 control compound. Unfortunately, articles are still published that cite the originally reported activity and selectivity of 1 for CB1, without acknowledgment of the subsequent retraction.143
Overview of Literature Reports of Curcumin Activity
A critical review of the literature reveals several major themes whenever novel bioactivity has been attributed to 1: (1) bioactivity was often observed at low micromolar to midmicromolar compound concentrations, typically above the critical aggregation concentration threshold for 1; (2) appropriate counterscreens for assay interference were frequently not performed, and target engagement was not confirmed nor was target selectivity; (3) nearly all the manuscripts reviewed failed to consider the stability of the compound; (4) finally, weak yet desired phenotypes, often observed at relatively high compound concentrations, were taken to “validate” specific target engagement but without sufficient evidence to rule out off-target effects. Such critical review of any reported activity requires a thorough understanding of the medicinal chemistry properties of 1 (vide supra).
Critical Evaluation of Clinical Trials
Most researchers currently consider compound 1 as a dietary supplement, and the FDA does not support claims regarding its therapeutic utility. For it to achieve a level of documented therapeutic utility in the United States, researchers will need to show that it is safe and effective for its intended use. While the essential oils and oleoresins of turmeric are recognized as GRAS substances,1441 is not on any readily accessible FDA GRAS list. When one company requested GRAS designation for a proprietary preparation of a mixture of curcuminoids, the FDA responded that it “has no questions at this time regarding (the company’s) conclusion that curcuminoids is [sic] GRAS under the intended conditions” (inclusion in baked goods; soups; snack foods; imitation dairy products; and seasoning and flavors at use levels up to 20 mg curcumin/serving) but that the agency “has not, however, made its own determination regarding the GRAS status of the subject use of curcuminoids”.34
Adverse events are rarely observed when curcuminoid preparations are dosed orally in humans, though some adverse reactions have occurred when large doses (8–12 g/day) necessary to provide “adequate systemic exposure” were administered orally. For example, a phase I dose-escalation study was carried out where three subjects in each of eight cohorts were treated with a single dose of a commercial milled curcumin mixture (95% curcuminoids with 70–80% 1, 15–25% 3, and 2.5–6.5% 4),145 over a range escalating from 500 mg to 12 g. Compound 1 was only detected in the serum of 2/6 subjects taking the single doses of 10 or 12 g.83 A peak serum level of 57.6 ng/mL (156 nmol/L) was measured at 2 h in the one individual who received the single 12 g dose. (For comparison, the Cmax for a 10 mg dose of atorvastatin is 2.81 ng/mL.)146 Adverse events in this study were diarrhea, rash, or headache. These events occurred in 30% of the trial participants, but did not appear to be dose related. In a longitudinal Phase I study of curcumin dosing, 15 patients with advanced colorectal cancer were administered 0.45 to 3.6 g daily of the same commercial mixture of curcuminoids described above for up to four months.147 In this case, 1 was found in the blood of 3/6 of the patients receiving the highest dose (11.1 ± 0.22 ng/mL, converted from the reported 0.6 nmol/L, at the 1 h time point on days 1, 2, 8, and 29), but not in the other nine subjects who received lower doses. Sulfate (8.9 ± 0.7 nmol/L) and glucuronide (15.8 ± 0.9 nmol/L) conjugates were found in all six of the subjects taking the 3.6 g daily dose, though there was no obvious difference in metabolite levels between those high-dose subjects in which 1 was found and in those in which it was not present. Notably “decreases in tumor markers or serum cholesterol were not observed as a result of treatment in any of the patients”, and “three significant changes in quality of life scores were reported: one patient noticed a significant improvement after one month of treatment, and two patients deteriorated after two months of treatment, both of whom were found to have radiologic progressive disease.” Mild diarrhea was the only sign of toxicity observed. In the present discussion, the significance of these phase I studies is two-fold. First, large amounts of 1 appear to be fairly well tolerated, suggesting that the use of curcuminoids or turmeric as an herbal supplement at lower doses is probably benign. Second, even at what might be considered the maximum-tolerated dose from the standpoint of pill consumption,148 we note that 1 has a variable and extremely low systemic bioavailability when dosed orally.
Beyond these primarily PK in vivo studies, 1 has a long history of being the subject of human PD clinical trials. The first article to report its use as a human therapeutic was in 1937.149−152 None of these studies have yet led to the approval of 1, curcuminoids, or turmeric as a therapeutic for any disease. According to the United States NIH,153 currently (from 2001 to the present) there are 135 registered clinical trials that have evaluated or will evaluate the toxicity and efficacy of curcuminoids in the treatment of a broad spectrum of diseases. Of the 135 trials, eight have reported study results. Forty-nine studies are listed as “recruiting” or “not yet recruiting”. It is beyond the scope of this work to compile, categorize, or analyze the results of all of these trials. We will, however, review the results of four archetypical clinical trials that illustrate the lack of significant success in this area. These trials were selected because data were reported on clinicaltrials.gov, and the therapeutic utility of 1 for these diseases is often referenced in manuscripts as validating its continued study.
Radiation Dermatitis
A recent example (2011–2014, NCT01246973) advanced to phase II/III and evaluated the administration of oral curcuminoids for the treatment of radiation-induced dermatitis in 686 women undergoing radiotherapy for the treatment of breast cancer. The objective “was to study the efficacy of curcumin in preventing and/or reducing the severity of dermatitis in radiation treatment site in breast cancer patients”. The treatment group took four commercially produced 500 mg curcuminoid mixture capsules (2.0 g) orally three times daily (6.0 g/day) throughout the course of radiation treatment plus one adjuvant week, while a placebo group received placebo capsules. To summarize, the study results appear inconclusive. The radiation dermatitis score (RDS, 0–4 with higher numbers indicating worse outcome) was used as a measure of the severity of the dermatitis. The RDS for the 283 patients who completed the curcumin arm of the study was 2.02 ± 0.05, while that of the placebo group was 1.99 ± 0.06. This result is perhaps not surprising, given the low oral bioavailability of compound 1. To our knowledge these data have not yet been published.
Colon Cancer
A phase IIa study evaluated the efficacy of curcumin in preventing colon cancer in smokers with aberrant crypt foci (NCT00365209). In stage 1 of this trial, 23 enrolled patients (21 completed the trial) received 2 g/day of a curcumin preparation. In stage 2, 21 additional subjects (19 completed) received 4 g/day of the curcumin preparation. In both cases the trial was continued for 30 days in the absence of unacceptable toxicity or disease progression. One important outcome measure was post-treatment concentration of compound 1 in rectal mucosa. In the stage 1 cohort, 5/21 subjects had detectable levels of 1 (8.2 ± 2.9 μg/g of protein), and in the stage 2 group, 3/18 subjects had detectable levels of 1 (3.8 ± 0.6 μg/g of protein). Additionally, compound 1 was observed in 2/19 subjects in stage 2 (3.8 ± 1.3 μg/mL). One key outcome measure was the change in total aberrant crypt foci number. The median change in stage 1 was 0.0 (range, −18 to 15) and was 6.0 in stage 2 (range, −1 to 14). While no statistical analysis was reported, there was no overall change in the stage 1 group (0.0) and very modest change in the stage 2 group (6.0). For clinical context, a change of 6.0 may move a patient from “normal” to “precancerous” or from “precancerous” to “cancerous”, but this will often result in no change in patient designation.3,154 To our knowledge, these data have not yet been published.
Alzheimer’s Disease (AD)
The results of a phase II 24-week, randomized, double-blinded clinical trial (2004–2008) studying the tolerability and efficacy of oral curcumin were reported in 2012.145 This trial was based on extensive preclinical experiments demonstrating that 1 reduced Aβ-induced toxicity in vitro and reduced markers of central nervous system oxidative stress in Tg2576 APPsw mice. In this study, human subjects (average age 74 years) received placebo, 2 g, or 4 g of a commercial curcuminoid mixture in two daily oral doses. PK sampling was performed using HPLC (lower limit of detection (LLOD), 200 ng/mL of 1) at baseline and 0.5, 1, 2, 3, and 4 h postdose at 24 weeks and by LC/MS/MS (LLOD 1 ng/mL compound 1; 3 ng/mL, tetrahydrocurcumin) at baseline and 3 h postdose at 24 weeks. As might be expected based on our previous ADMET discussion, 1 was not found by HPLC analysis in any patient plasma sample, save one sample taken 4 h after a 4 g dose (6 ng/mL, below the assay LLOD). With more sensitive LC/MS/MS methods, the mean baseline level of 1 at 24 weeks was 2.67 ± 1.69 ng/mL, while that of tetrahydrocurcumin was 6.86 ± 1.69 ng/mL. Three hours post-treatment, the mean plasma levels were as follows: compound 1 (7.76 ± 3.23 ng/mL), tetrahydrocurcumin (3.73 ± 2.0 ng/mL), glucuronidated 1 (96.05 ± 26 ng/mL), and glucuronidated tetrahydrocurcumin (298.2 ± 140.0 ng/mL). After 24 weeks of treatment, there was no observed difference in mental status between the placebo and treated groups based on several measurements of cognitive status such as ADAS-Cog or mini-mental state examination (MMSE) scores. While no serious adverse events were reported, almost all (>90%) of the control and experimental subjects reported adverse events such as diarrhea, joint pain, and complaints attributed to endocrine system effects. The plasma glucose levels in the treated subjects were statistically higher than those of the placebo subjects, though not outside a normal range. The potential of compound 1 as a neurotherapeutic has been extensively reviewed, and it was concluded (our notes italicized):
“It seems debatable to further pursue the supplementation of high concentrations of curcumin in humans. Instead, in line with the concepts of promising alternative mechanisms such as neurohormesis (Note: a mechanism by which the therapeutic effects of low doses of substances are amplified by stimulation of endogenous, beneficial biochemical pathways155) and the gut microbiota as primary targets of curcumin to mediate neuroprotection, low doses of curcumin should be considered in future in clinical trial design.”7
Another more recent review156 stated that there is insufficient evidence to recommend the use of curcumin in dementia patients and that its low bioavailability and poor study design could explain the apparent discrepancies between in vitro and human clinical trial results.
The results of an epidemiological study comparing the low incidence of AD in Ballabgarh, a rural community in northern India, to a cohort of subjects in the rural mid-Monongahela Valley of Pennsylvania is often cited as evidence that a diet containing turmeric (of which 1 is a minor component) is beneficial.157 However, even the authors of the oft-cited study cautioned against overinterpretation of their results given the relatively short duration of the study, the small number of incident cases, and the wide confidence intervals. Diet was not considered as part of the study, and the frequency of the APOE4 allele, a risk factor for AD, was noted as being lower in the Ballabgarh group (0.073) as compared to the Monongahela Valley group (0.11). Another frequently cited study158 used to support the impact of curcumin on AD measured the cognitive function of 1010 nondemented, elderly subjects (Singapore National Mental Health Survey) compared to their self-reported ingestion of curry (containing turmeric spice; 1–6% curcuminoids).159 Various ethnic versions of the MMSE were used to compare the cognitive status of those who consumed curry “never or rarely”, “occasionally”, or “often” (Table 1).
Table 1. Data Relating Cognitive Function of Nondemented Elderly Subjects and Their Self-Reported Curry Consumption158,a.
| unadjusted
(MMSE)b |
adjusted
(MMSE)c |
||||
|---|---|---|---|---|---|
| curry consumption | no. subjects | mean | 95% CI | mean | 95% CI |
| never or rarely | 163 | 24.9 | 24.2, 25.7 | 23.3 | 21.2, 25.4 |
| occasionally | 411 | 26.2 | 25.8, 26.6 | 24.8 | 22.9, 26.7 |
| often | 436 | 25.0 | 25.6, 26.4 | 24.8 | 22.9, 26.6 |
| ANOVA | p = 0.004 | p = 0.023 | |||
Cognitive function was evaluated using various ethnic versions of the MMSE scores for each group.
Unweighted sample estimates.
Weighted least-squares regression estimates adjusted for age, education, gender, ethnicity, etc. (20 variables total).
According to the study authors, “although the results are suggestive of a biological therapeutic effect, we emphasize that they do not establish a clear and direct causal effect of curry consumption on improving cognitive function.” The difference in MMSE between those who rarely use turmeric and those that often use it is not significant.160
Pancreatic Cancer
A phase II study of the use of curcuminoids in patients with advanced pancreatic cancer was reported in 2008.148 This study used encapsulated curcuminoids in a form that contained 90% compound 1, 8% of 3, and 2% of 4. Patients started at a dose of 8 g/day and took oral curcuminoids daily for at least 8 weeks. The dosing regimen was then continued if their disease had stabilized. Twenty-one of the 25 subjects initially enrolled were evaluable for response at the end of the study. At the time of publication, one patient had remained stable for more than 18 months and another single patient had a brief but marked 73% reduction in tumor size that lasted one month. One other patient remained enrolled in the study for approximately eight months with “stable weight and a feeling of well-being, albeit with progression in non-target lesions”. Only low levels of 1 were detectable in plasma (∼22–41 ng/mL at steady state on day 3). No treatment-related toxic effects were reported.
Clinical Trials Review Summary
The aforementioned clinical trials were discussed because they are representative of many other studies for which outcome data are not (yet) available. Given its low systemic bioavailability, we remain highly skeptical that an oral dose of 1 can ever be effective in human clinical trials that are translated from reports of in vitro activity. Disagreements regarding the importance of alternative therapeutic mechanisms like neurohormesis notwithstanding, it is hard to formulate reasonable justification for studying lower oral doses of curcuminoids given that even at high doses compound 1 is not found in the serum of test subjects. The transformation of 1 to potentially active metabolites in the gut and the related influence on the gut microbiota (vide supra)103 seems to be reasonable areas of study as no absorption of the parent compound is necessary. Still, the lack of any observed efficacy of oral curcuminoids in clinical trials where it was given in high doses does not bode well for these alternative hypotheses of therapeutic efficacy.
Conclusions: Future Curcumin Research
The vast number of manuscripts published on the biological activity of curcumin makes it all but impossible for researchers to keep up with the state-of-the-art in the field. Herein, an attempt has been made to present an overview of the medicinal chemistry research that will be helpful for researchers and reviewers to consider in their respective roles. At first, curcumin appeared to offer great potential for the development of a therapeutic from a NP (turmeric) that is classified as a GRAS material.144 Unfortunately, no form of curcumin, or its closely related analogues, appears to possess the properties required for a good drug candidate (chemical stability, high water solubility, potent and selective target activity, high bioavailability, broad tissue distribution, stable metabolism, and low toxicity). The in vitro interference properties of curcumin do, however, offer many traps that can trick unprepared researchers into misinterpreting the results of their investigations.
The observations of this Miniperspective offer several key points that can help identify potentially problematic research approaches and/or interpretation of outcomes in publications or preliminary data involving curcumin bioactivity. Notably, many of these strategies have been articulated previously:122,161
-
1.
Look for evidence of compound stability in assay buffer/media, including when molecular models are invoked as supporting evidence of target engagement.
-
2.
Look for the presence of detergent and thiol-scavenging reagents in biochemical assays to mitigate the impact of chemical aggregation and nonspecific thiol reactivity. Are/were any additional counterscreens performed to rule out these phenomena?
-
3.
Examine the selectivity data. What are the magnitudes of any observed selectivity? Are these significant? Can any selectivity be explained by differential target susceptibilities to nonspecific interference modalities like thiol reactivity? Can any apparent selectivity be explained by the assay conditions, such as target or total protein concentration?
-
4.
Examine the potency of the compound. At those concentrations, would there be any expected aggregation or off-target effects? And if so, can one make meaningful conclusions about specific pathways and target engagement? Does the stoichiometry make sense?
-
5.
Evaluate the methods to confirm target engagement. Look for biophysical orthogonal methods for support of target engagement (e.g., SPR, ITC, CETSA), not solely phenotypic assays.
-
6.
Carefully examine the detection method for determining the concentration of 1 present in an assay. What biophysical method is/was used for detection? Can likely degradation products or metabolites have a similar response and/or explain the data/hypothesis?
With respect to curcumin/curcuminoids and in vivo studies and clinical trials, we believe there is rather “much ado about nothing”. Certainly, the low systemic exposure levels reported in clinical trials do not support its further investigation as a therapeutic. Circumventing the requirement for systemic circulation, curcumin might provide benefit by acting on gut microbiota. Thus far, there is limited evidence to support this hypothesis, which will also limit the utility of this delivery method. Delivery systems such as lipid vesicles, nanoparticles, and nanofibers might be able to boost the bioavailability of 1, but this could also conceivably narrow its therapeutic window and lead to off-target toxicity by aforementioned processes. Available evidence demonstrates curcumin will ultimately degrade upon release into physiologic media, no matter the delivery mechanism. Analogues of 1 might address some of the delivery challenges but would be new chemical entities and would have to proceed through expensive preclinical work to be approved for clinical trials. In our opinion, analogues of curcumin are based on a fairly weak foundation.
Of course, we do not rule out the possibility that an extract of crude turmeric might have beneficial effects on human health. The large RC of NP extracts, and even of refined NP preparations, makes the identification of the active constituent(s) and evaluation of their efficacy in humans very difficult.51,162 Considering the overwhelming evidence showing the weakness of isolated curcumin (almost always a mixture of curcuminoids) as a viable therapeutic, consideration of holistic approaches that take into account the chemical and PD/PK complexity of turmeric and its broad TxM/nutritional foundation appears to be superior directions for future research in the turmeric domain. While the concepts of static and dynamic RC apply equally to synthetically prepared compounds, the development of leads sourced from metabolomic (natural) sources is intrinsically more prone to the impact of purity (and unknown impurities). In some ways, the oversimplification of this complexity has led to complicatedness that makes it difficult to interpret results of curcumin-based studies.142,143 In addition, there is increasing evidence that TxM agents cannot be adequately described with reductionist pharmacology models but require consideration of polypharmacology and synergy.163 The recent recognition of IMPS4 adds to the uniqueness of natural products by identifying panacea-type substances that establish a new dimension of biological signatures generated by bioactive molecules. Curcumin is not the only potential IMP that has received much attention by the scientific community as a drug lead. Development projects with numerous other prominent plant natural products (e.g., polyphenolics) have experienced similar drawbacks despite major efforts. As shown here for curcumin, the essential medicinal chemistry of natural products that were developed into drugs successfully, and as almost unaltered structures (e.g., artemisinin, camptothecin, taxol, ivermectin, etc.), differs significantly from those of potential IMPS. This orthogonal perspective on the druggability of NPs is further supported by the metabolic feedback hypothesis,164 which states that bioactivity, especially of many food-borne phytochemicals, can act via weak negative biological feedback mechanisms, escaping in vitro detection and blurring our understanding of mechanisms of action. Collectively, recognition of these factors may remove complicatedness from ongoing research while inspiring the development of out-of-the-box approaches to unraveling the complexity and potential health benefits of turmeric and other NPs.
Acknowledgments
J.L.D., J.B., J.G., and G.F.P. acknowledge Dr. Brian Shoichet for helpful discussions. J.B. and G.F.P. acknowledge funding from NCCIH and ODS/NIH through Grant U41AT008706. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The opinions or assertions contained herein belong to the authors and are not necessarily the official views of the funders.
Glossary
Abbreviations Used
- AD
Alzheimer’s disease
- ADMET
absorption, distribution, metabolism, excretion, and toxicology
- AID
assay identifier
- CETSA
cellular thermal shift assay
- CPM
N-[4-(7-diethylamino-4-methylcoumarin-3-yl)phenyl]maleimide
- DLS
dynamic light scattering
- DTT
dithiolthreitol
- FDA
Federal Drug Administration
- FP
fluorescence polarization
- GRAS
generally recognized as safe
- HAT
histone acetyltransferase
- HDAC
histone deacetylase
- HPLC
high-performance liquid chromatography
- HTS
high-throughput screening
- IC50
half-maximal inhibitory concentration
- IMPS
invalid (or improbable) metabolic panaceas
- ITC
isothermal titration calorimetry
- LLOD
lower limit of detection
- ClogP
calculated partition coefficient
- MLPCN
Molecular Libraries Probe Centers Network
- MMSE
mini-mental state examination
- NAPRALERT
natural products alert
- NP
natural product
- PAINS
pan assay interference compounds
- NMR
nuclear magnetic resonance
- PD
pharmacodynamics
- PK
pharmacokinetics
- RDS
radiation dermatitis score
- RPMI 1640
Roswell Park Memorial Institute 1640 medium
- RC
residual complexity
- SPR
surface plasmon resonance
- ThT
thioflavin T
Biographies
Kathryn M. Nelson is a Research Associate at the Institute for Therapeutics Discovery and Development at the University of Minnesota (UMN) in Minneapolis, MN. She graduated from the UMN College of Pharmacy in 2013, where she received her Ph.D. in Medicinal Chemistry. Her doctoral thesis work focused on the development of novel antitubercular agents and chemical tools for biological target identification. Her current research interests include development of new Alzheimer’s therapeutics, assay development and triage, and the development of new chemical tools for target interrogation.
Jayme L. Dahlin is a Resident Physician in Clinical Pathology at Brigham and Women’s Hospital in Boston, MA. He graduated from the Mayo Clinic Medical Scientist Training Program in 2016, where he received his Ph.D. in Molecular Pharmacology and Experimental Therapeutics from Mayo Graduate School and his M.D. from Mayo Medical School. His doctoral thesis work focused on chemical mechanisms of assay interference in high-throughput screening (HTS) and early drug discovery. His current research interests include HTS and triage, bioassay promiscuity, and assay development.
Jonathan Bisson obtained an M.S. degree in Structural Biochemistry and started his phytochemistry journey under the mentorship of Dr. Vincent Dumontet at the Institut de Chimie des Substances Naturelles, Gif-sur-Yvette, France. He then obtained a Ph.D. in Science, Technology and Health from the University of Bordeaux, France under the mentorship of Dr. Pierre Waffo-Téguo, specializing in methodology at the chemistry–biology interface. In 2013, he joined the University of Illinois at Chicago, where he is currently a Postdoctoral Research Associate, developing new methods and tools for natural products research in interdisciplinary programs, mainly through data analysis, NMR, and chromatographic approaches related to promiscuous natural products (IMPS). Recently, he has been involved in the redesign of the NAPRALERT database.
James Graham received a B.S. in Chemistry in 1994 from the University of Pittsburgh, followed by a Ph.D. in Pharmacognosy in 2001, as a protégé of Norman R. Farnsworth at the University of Illinois at Chicago College of Pharmacy (UIC-COP). Following an NIH postdoctoral fellowship in Miami and a stint as Technical Officer at the World Health Organization in Geneva, he returned to UIC-COP in 2007, where he is currently editor of the NAPRALERT database and Research Associate Professor in the Department of Medicinal Chemistry and Pharmacognosy.
Guido F. Pauli is a pharmacist with a doctoral degree in Natural Products Chemistry and Pharmacognosy. As Professor and University Scholar at UIC, Chicago (IL), he is PI and collaborator in various interdisciplinary natural-product-centered research projects and Director of the Center for Natural Product Technologies. His research involves metabolome analysis of complex natural products, analytical methodology for bioactive principles, herbal dietary supplements, anti-TB drug discovery, and dental applications of natural agents. His scholarly activities involve the education of the next generation of pharmacognosist, service on pharmacopoeial expert and federal agency panels, and guest professorships. His dissemination portfolio comprises 170+ peer-reviewed journal articles as well as journal coeditorial and board functions.
Michael A. Walters is a Research Associate Professor of Medicinal Chemistry at the University of Minnesota (UMN). He began his academic career in the Department of Chemistry at Dartmouth College and then worked at Parke-Davis and Pfizer. He is currently the Director of the Lead and Probe Discovery Group in the Institute for Therapeutics Discovery and Development at the UMN. This institute serves as a minibiotech for the development of the ideas of biomedical researchers at the UMN and Mayo Clinic. His research interests currently focus on the investigation of compound reactivity as it applies to assay interference mechanisms, the development of Alzheimer’s disease therapeutics, and new compounds to treat heart valve calcification.
Supporting Information Available
The Supporting Information is available free of charge on the ACS Publications website at DOI: 10.1021/acs.jmedchem.6b00975.
Supplemental Tables 1, 2, and 3 of assays, half-lives, and activities, along with a discussion of covalent protein modification by 1 (PDF)
Author Contributions
K.M.N., M.A.W., J.L.D., J.B., J.G., and G.F.P. wrote the manuscript. K.M.N., M.A.W., J.L.D., G.F.P., J.G., and J.B. contributed to revisions.
The authors declare no competing financial interest.
Supplementary Material
References
- Yuan D.; Yang X.; Guo J. C. A great honor and a huge challenge for China: You-you tu getting the nobel prize in physiology or medicine. J. Zhejiang Univ., Sci., B 2016, 17, 405–408. 10.1631/jzus.B1600094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson M. Is the 2015 Nobel Prize a turning point for traditional Chinese medicine? https://theconversation.com/is-the-2015-nobel-prize-a-turning-point-for-traditional-chinese-medicine-48643 (accessed June 6, 2016).
- Baell J.; Walters M. A. Chemistry: Chemical con artists foil drug discovery. Nature (London, U. K.) 2014, 513, 481–483. 10.1038/513481a. [DOI] [PubMed] [Google Scholar]
- Bisson J.; McAlpine J. B.; Friesen J. B.; Chen S.-N.; Graham J.; Pauli G. F. Can invalid bioactives undermine natural product-based drug discovery?. J. Med. Chem. 2016, 59, 1671–1690. 10.1021/acs.jmedchem.5b01009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgos-Moron E.; Calderon-Montano J. M.; Salvador J.; Robles A.; Lopez-Lazaro M. The dark side of curcumin. Int. J. Cancer 2010, 126, 1771–1775. 10.1002/ijc.24967. [DOI] [PubMed] [Google Scholar]
- Baell J. B. Feeling nature’s PAINS: Natural products, natural product drugs, and pan assay interference compounds (PAINS). J. Nat. Prod. 2016, 79, 616–628. 10.1021/acs.jnatprod.5b00947. [DOI] [PubMed] [Google Scholar]
- Chin D.; Huebbe P.; Pallauf K.; Rimbach G. Neuroprotective properties of curcumin in Alzheimer’s disease - merits and limitations. Curr. Med. Chem. 2013, 20, 3955–3985. 10.2174/09298673113209990210. [DOI] [PubMed] [Google Scholar]
- Glaser J.; Holzgrabe U. Focus on PAINS: False friends in the quest for selective anti-protozoal lead structures from nature?. MedChemComm 2016, 7, 214–223. 10.1039/C5MD00481K. [DOI] [Google Scholar]
- Heger M.; van Golen R. F.; Broekgaarden M.; Michel M. C. The molecular basis for the pharmacokinetics and pharmacodynamics of curcumin and its metabolites in relation to cancers. Pharmacol. Rev. 2014, 66, 222–307. 10.1124/pr.110.004044. [DOI] [PubMed] [Google Scholar]
- Elias G.; Jacob P. J.; Hareeshbabu E.; Mathew V. B.; Krishnan B.; Krishnakumar K. Curcumin: Transforming the spice to a wonder drug. Int. J. Pharm. Sci. Res. 2015, 6, 2671–2680. 10.13040/IJPSR.0975-8232.6(7).2671-80. [DOI] [Google Scholar]
- Neckers L.; Trepel J.; Lee S.; Chung E.-J.; Lee M.-J.; Jung Y.-J.; Marcu M. G. Curcumin is an inhibitor of p300 histone acetyltransferase. Med. Chem. (Sharjah, United Arab Emirates) 2006, 2, 169–174. 10.2174/157340606776056133. [DOI] [PubMed] [Google Scholar]
- Rainey-Smith S. R.; Brown B. M.; Sohrabi H. R.; Shah T.; Goozee K. G.; Gupta V. B.; Martins R. N. Curcumin and cognition: A randomised, placebo-controlled, double-blind study of community-dwelling older adults. Br. J. Nutr. 2016, 115, 2106–2113. 10.1017/S0007114516001203. [DOI] [PubMed] [Google Scholar]
- Okamura T.; Kubo K.. Turmeric pigment-containing chocolate with excellent flavor, texture, and hangover prevention/treatment properties. JP2009183206A, 2009.
- Kwon H. N.Functional noodles for relieving hangover and its manufacturing method. KR1314917B1, 2013.
- Rezq E.-S. A. M.; Mansour M. T. A.-A.; Kumosani T. A.. Long acting conserved natural functional groups curcumin. WO2010057503A2, 2010.
- Wang A.; An X.; Zhou Y.. Application of curcumin to medicinal preparations for treating erectile dysfunction. CN101822656A, 2010.
- Isaacs E.; Cobbledick T.. Complete supplement formulae for maintenance of hair growth and condition. GB2484812A, 2012.
- Huh S.; Lee J.; Jung E.; Kim S.-C.; Kang J.-I.; Lee J.; Kim Y.-W.; Sung Y. K.; Kang H.-K.; Park D. A cell-based system for screening hair growth-promoting agents. Arch. Dermatol. Res. 2009, 301, 381–385. 10.1007/s00403-009-0931-0. [DOI] [PubMed] [Google Scholar]
- Ahluwalia G. S.; Shander D.; Styczynski P.. Inhibition of hair growth with protein kinase C inhibitors. WO9609806A2, 1996.
- Jana S.; Paul S.; Swarnakar S. Curcumin as anti-endometriotic agent: Implication of MMP-3 and intrinsic apoptotic pathway. Biochem. Pharmacol. (Amsterdam, Neth.) 2012, 83, 797–804. 10.1016/j.bcp.2011.12.030. [DOI] [PubMed] [Google Scholar]
- Naz R. K.; Lough M. L. Curcumin as a potential non-steroidal contraceptive with spermicidal and microbicidal properties. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014, 176, 142–148. 10.1016/j.ejogrb.2014.01.024. [DOI] [PubMed] [Google Scholar]
- Data pertaining to these claims are easily accessible by any Internet search engine, e.g., https://www.google.com/#q=curcumin+AND+health+benefits
- Goel A.; Kunnumakkara A. B.; Aggarwal B. B. Curcumin as "curecumin": From kitchen to clinic. Biochem. Pharmacol. (Amsterdam, Neth.) 2008, 75, 787–809. 10.1016/j.bcp.2007.08.016. [DOI] [PubMed] [Google Scholar]
- Kumar A.; Chetia H.; Sharma S.; Kabiraj D.; Talukdar N. C.; Bora U. Curcumin resource database. Database 2015, 2015, bav070. 10.1093/database/bav070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J.; Zhang C.-J.; Chia W. N.; Loh C. C. Y.; Li Z.; Lee Y. M.; He Y.; Yuan L.-X.; Lim T. K.; Liu M.; Liew C. X.; Lee Y. Q.; Zhang J.; Lu N.; Lim C. T.; Hua Z.-C.; Liu B.; Shen H.-M.; Tan K. S. W.; Lin Q. Haem-activated promiscuous targeting of artemisinin in Plasmodium falciparum. Nat. Commun. 2015, 6, 10111. 10.1038/ncomms10111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medhi B.; Patyar S.; Rao R. S.; Byrav D. S. P.; Prakash A. Pharmacokinetic and toxicological profile of artemisinin compounds: An update. Pharmacology 2009, 84, 323–332. 10.1159/000252658. [DOI] [PubMed] [Google Scholar]
- Wang Y.-J.; Pan M.-H.; Cheng A.-L.; Lin L.-I.; Ho Y.-S.; Hsieh C.-Y.; Lin J.-K. Stability of curcumin in buffer solutions and characterization of its degradation products. J. Pharm. Biomed. Anal. 1997, 15, 1867–1876. 10.1016/S0731-7085(96)02024-9. [DOI] [PubMed] [Google Scholar]
- Yang K. Y.; Lin L. C.; Tseng T. Y.; Wang S. C.; Tsai T. H. Oral bioavailability of curcumin in rat and the herbal analysis from Curcuma longa by LC-MS/MS. J. Chromatogr. B: Anal. Technol. Biomed. Life Sci. 2007, 853, 183–189. 10.1016/j.jchromb.2007.03.010. [DOI] [PubMed] [Google Scholar]
- Chow S.-C.; Chiu S.-T. A note on design and analysis of clinical trials. Drug Des.: Open Access 2013, 2, 102. 10.4172/2169-0138.1000102. [DOI] [Google Scholar]
- National Institutes of Health. NIH RePORTER. Research portfolio online reporting tools. Reports, data, and analysis of NIH research activities. http://projectreporter.nih.gov/reporter.cfm (accessed October 6, 2016).
- Kuttan R.; Bhanumathy P.; Nirmala K.; George M. C. Potential anticancer activity of turmeric (Curcuma longa). Cancer Lett. (N. Y., NY, U. S.) 1985, 29, 197–202. 10.1016/0304-3835(85)90159-4. [DOI] [PubMed] [Google Scholar]
- Niranjan A.; Singh S.; Dhiman M.; Tewari S. K. Biochemical composition of Curcuma longa l. Accessions. Anal. Lett. 2013, 46, 1069–1083. 10.1080/00032719.2012.751541. [DOI] [Google Scholar]
- Priyadarsini K. I. The chemistry of curcumin: From extraction to therapeutic agent. Molecules 2014, 19, 20091–20112. 10.3390/molecules191220091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Food and Drug Administration Office of Food Additive Safety. Agency Response Letter GRAS Notice No. Grn 000460. U.S. Food and Drug Administration, 2013. [Google Scholar]
- Majeed S.The state of the curcumin market. Natural Products Insider; Informa Exhibitions, 2015; http://www.naturalproductsinsider.com/articles/2015/12/the-state-of-the-curcumin-market.aspx. [Google Scholar]
- Niranjan A.; Prakash D. Chemical constituents and biological activities of turmeric (Curcuma longa l.) - a review. J. Food Sci. Technol. (New Delhi, India) 2008, 45, 109–116. [Google Scholar]
- Panahi Y.; Hosseini M. S.; Khalili N.; Naimi E.; Majeed M.; Sahebkar A. Antioxidant and anti-inflammatory effects of curcuminoid-piperine combination in subjects with metabolic syndrome: A randomized controlled trial and an updated meta-analysis. Clin. Nutr. 2015, 34, 1101–1108. 10.1016/j.clnu.2014.12.019. [DOI] [PubMed] [Google Scholar]
- Yue G. G.; Chan B. C.; Hon P. M.; Lee M. Y.; Fung K. P.; Leung P. C.; Lau C. B. Evaluation of in vitro anti-proliferative and immunomodulatory activities of compounds isolated from Curcuma longa. Food Chem. Toxicol. 2010, 48, 2011–2020. 10.1016/j.fct.2010.04.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu S.; Maiti P.; Ma Q.; Zuo X.; Jones M. R.; Cole G. M.; Frautschy S. A. Clinical development of curcumin in neurodegenerative disease. Expert Rev. Neurother. 2015, 15, 629–637. 10.1586/14737175.2015.1044981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baell J. B.; Holloway G. A. New substructure filters for removal of pan assay interference compounds (PAINS) from screening libraries and for their exclusion in bioassays. J. Med. Chem. 2010, 53, 2719–2740. 10.1021/jm901137j. [DOI] [PubMed] [Google Scholar]
- Fang J.; Lu J.; Holmgren A. Thioredoxin reductase is irreversibly modified by curcumin: A novel molecular mechanism for its anticancer activity. J. Biol. Chem. 2005, 280, 25284–25290. 10.1074/jbc.M414645200. [DOI] [PubMed] [Google Scholar]
- Jurrmann N.; Birgelius-Flohe R.; Boel G.-F. Curcumin blocks interleukin-1 (IL-1) signaling by inhibiting the recruitment of the IL-1 receptor-associated kinase IRAK in murine thymoma EL-4 cells. J. Nutr. 2005, 135, 1859–1864. [DOI] [PubMed] [Google Scholar]
- Jung Y.; Xu W.; Kim H.; Ha N.; Neckers L. Curcumin-induced degradation of ErbB2: A role for the E3 ubiquitin ligase CHIP and the Michael reaction acceptor activity of curcumin. Biochim. Biophys. Acta, Mol. Cell Res. 2007, 1773, 383–390. 10.1016/j.bbamcr.2006.11.004. [DOI] [PubMed] [Google Scholar]
- Chin D.; Huebbe P.; Frank J.; Rimbach G.; Pallauf K. Curcumin may impair iron status when fed to mice for six months. Redox Biol. 2014, 2, 563–569. 10.1016/j.redox.2014.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider C.; Gordon O. N.; Edwards R. L.; Luis P. B. Degradation of curcumin: From mechanism to biological implications. J. Agric. Food Chem. 2015, 63, 7606–7614. 10.1021/acs.jafc.5b00244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan D.; Doak A. K.; Nedyalkova L.; Shoichet B. K. Colloidal aggregation and the in vitro activity of traditional Chinese medicines. ACS Chem. Biol. 2015, 10, 978–988. 10.1021/cb5009487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingolfsson H. I.; Thakur P.; Herold K. F.; Hobart E. A.; Ramsey N. B.; Periole X.; de Jong D. H.; Zwama M.; Yilmaz D.; Hall K.; Maretzky T.; Hemmings H. C. Jr.; Blobel C.; Marrink S. J.; Kocer A.; Sack J. T.; Andersen O. S. Phytochemicals perturb membranes and promiscuously alter protein function. ACS Chem. Biol. 2014, 9, 1788–1798. 10.1021/cb500086e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Priyadarsini K. I. Photophysics, photochemistry and photobiology of curcumin: Studies from organic solutions, bio-mimetics and living cells. J. Photochem. Photobiol., C 2009, 10, 81–95. 10.1016/j.jphotochemrev.2009.05.001. [DOI] [Google Scholar]
- Esatbeyoglu T.; Ulbrich K.; Rehberg C.; Rohn S.; Rimbach G. Thermal stability, antioxidant, and anti-inflammatory activity of curcumin and its degradation product 4-vinyl guaiacol. Food Funct. 2015, 6, 887–893. 10.1039/C4FO00790E. [DOI] [PubMed] [Google Scholar]
- Avonto C.; Taglialatela-Scafati O.; Pollastro F.; Minassi A.; Di Marzo V.; De Petrocellis L.; Appendino G. An NMR spectroscopic method to identify and classify thiol-trapping agents: Revival of Michael acceptors for drug discovery?. Angew. Chem., Int. Ed. 2011, 50, 467–471. 10.1002/anie.201005959. [DOI] [PubMed] [Google Scholar]
- Pauli G. F.; Chen S. N.; Friesen J. B.; McAlpine J. B.; Jaki B. U. Analysis and purification of bioactive natural products: The AnaPurNa study. J. Nat. Prod. 2012, 75, 1243–1255. 10.1021/np300066q. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmler C.; Hajirahimkhan A.; Lankin D. C.; Bolton J. L.; Jones T.; Soejarto D. D.; Chen S. N.; Pauli G. F. Dynamic residual complexity of the isoliquiritigenin-liquiritigenin interconversion during bioassay. J. Agric. Food Chem. 2013, 61, 2146–2157. 10.1021/jf304445p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon O. N.; Luis P. B.; Sintim H. O.; Schneider C. Unraveling curcumin degradation: Autoxidation proceeds through spiroepoxide and vinylether intermediates en route to the main bicyclopentadione. J. Biol. Chem. 2015, 290, 4817–4828. 10.1074/jbc.M114.618785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Workman P.; Collins I. Probing the probes: Fitness factors for small molecule tools. Chem. Biol. (Oxford, U. K.) 2010, 17, 561–577. 10.1016/j.chembiol.2010.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh J.; Petter R. C.; Baillie T. A.; Whitty A. The resurgence of covalent drugs. Nat. Rev. Drug Discovery 2011, 10, 307–317. 10.1038/nrd3410. [DOI] [PubMed] [Google Scholar]
- Kalgutkar A. S.; Dalvie D. K. Drug discovery for a new generation of covalent drugs. Expert Opin. Drug Discovery 2012, 7, 561–581. 10.1517/17460441.2012.688744. [DOI] [PubMed] [Google Scholar]
- Schröder J.; Klinger A.; Oellien F.; Marhoefer R. J.; Duszenko M.; Selzer P. M. Docking-based virtual screening of covalently binding ligands: An orthogonal lead discovery approach. J. Med. Chem. 2013, 56, 1478–1490. 10.1021/jm3013932. [DOI] [PubMed] [Google Scholar]
- Davids M. S.; Brown J. R. Ibrutinib: A first in class covalent inhibitor of Bruton’s tyrosine kinase. Future Oncol. 2014, 10, 957–967. 10.2217/fon.14.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flanagan M. E.; Abramite J. A.; Anderson D. P.; Aulabaugh A.; Dahal U. P.; Gilbert A. M.; Li C.; Montgomery J.; Oppenheimer S. R.; Ryder T.; Schuff B. P.; Uccello D. P.; Walker G. S.; Wu Y.; Brown M. F.; Chen J. M.; Hayward M. M.; Noe M. C.; Obach R. S.; Philippe L.; Shanmugasundaram V.; Shapiro M. J.; Starr J.; Stroh J.; Che Y. Chemical and computational methods for the characterization of covalent reactive groups for the prospective design of irreversible inhibitors. J. Med. Chem. 2014, 57, 10072–10079. 10.1021/jm501412a. [DOI] [PubMed] [Google Scholar]
- Jost C.; Nitsche C.; Scholz T.; Roux L.; Klein C. D. Promiscuity and selectivity in covalent enzyme inhibition: A systematic study of electrophilic fragments. J. Med. Chem. 2014, 57, 7590–7599. 10.1021/jm5006918. [DOI] [PubMed] [Google Scholar]
- Mah R.; Thomas J. R.; Shafer C. M. Drug discovery considerations in the development of covalent inhibitors. Bioorg. Med. Chem. Lett. 2014, 24, 33–39. 10.1016/j.bmcl.2013.10.003. [DOI] [PubMed] [Google Scholar]
- Moghaddam M. F.; Tang Y.; O’Brien Z.; Richardson S. J.; Bacolod M.; Chaturedi P.; Apuy J.; Kulkarni A. A proposed screening paradigm for discovery of covalent inhibitor drugs. Drug Metab. Lett. 2014, 8, 19–30. 10.2174/1872312808666140317151735. [DOI] [PubMed] [Google Scholar]
- Payton F.; Sandusky P.; Alworth W. L. NMR study of the solution structure of curcumin. J. Nat. Prod. 2007, 70, 143–146. 10.1021/np060263s. [DOI] [PubMed] [Google Scholar]
- Jagannathan R.; Abraham P. M.; Poddar P. Temperature-dependent spectroscopic evidences of curcumin in aqueous medium: A mechanistic study of its solubility and stability. J. Phys. Chem. B 2012, 116, 14533–14540. 10.1021/jp3050516. [DOI] [PubMed] [Google Scholar]
- Takagi T.; Ramachandran C.; Bermejo M.; Yamashita S.; Yu L. X.; Amidon G. L. A provisional biopharmaceutical classification of the top 200 oral drug products in the United States, Great Britain, Spain, and Japan. Mol. Pharmaceutics 2006, 3, 631–643. 10.1021/mp0600182. [DOI] [PubMed] [Google Scholar]
- Griesser M.; Pistis V.; Suzuki T.; Tejera N.; Pratt D. A.; Schneider C. Autoxidative and cyclooxygenase-2 catalyzed transformation of the dietary chemopreventive agent curcumin. J. Biol. Chem. 2011, 286, 1114–1124. 10.1074/jbc.M110.178806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon O. N.; Schneider C. Vanillin and ferulic acid: Not the major degradation products of curcumin. Trends Mol. Med. 2012, 18, 361–363. (author reply, pp 363–364) 10.1016/j.molmed.2012.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khurana A.; Ho C. T. High-performance liquid-chromatographic analysis of curcuminoids and their photo-oxidative decomposition compounds in Curcuma longa l. J. Liq. Chromatogr. 1988, 11, 2295–2304. 10.1080/01483918808067200. [DOI] [Google Scholar]
- Tønnesen H. H.; Karlsen J.; van Henegouwen G. B. Studies on curcumin and curcuminoids. VIII. Photochemical stability of curcumin. Z. Lebensm.-Unters. Forsch. 1986, 183, 116–122. 10.1007/BF01041928. [DOI] [PubMed] [Google Scholar]
- Ghosh M.; Singh A. T.; Xu W.; Sulchek T.; Gordon L. I.; Ryan R. O. Curcumin nanodisks: Formulation and characterization. Nanomedicine 2011, 7, 162–167. 10.1016/j.nano.2010.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun M.; Su X.; Ding B.; He X.; Liu X.; Yu A.; Lou H.; Zhai G. Advances in nantoechnology-based delivery systems for curcumin. Nanomedicine (London, U. K.) 2012, 7, 1085–1100. 10.2217/nnm.12.80. [DOI] [PubMed] [Google Scholar]
- Tamvakopoulos C.; Dimas K.; Sofianos Z. D.; Hatziantoniou S.; Han Z.; Liu Z. L.; Wyche J. H.; Pantazis P. Metabolism and anticancer activity of the curcumin analogue, dimethoxycurcumin. Clin. Cancer Res. 2007, 13, 1269–1277. 10.1158/1078-0432.CCR-06-1839. [DOI] [PubMed] [Google Scholar]
- Robinson T. P.; Hubbard R. B. t.; Ehlers T. J.; Arbiser J. L.; Goldsmith D. J.; Bowen J. P. Synthesis and biological evaluation of aromatic enones related to curcumin. Bioorg. Med. Chem. 2005, 13, 4007–4013. 10.1016/j.bmc.2005.03.054. [DOI] [PubMed] [Google Scholar]
- Liang G.; Shao L.; Wang Y.; Zhao C.; Chu Y.; Xiao J.; Zhao Y.; Li X.; Yang S. Exploration and synthesis of curcumin analogues with improved structural stability both in vitro and in vivo as cytotoxic agents. Bioorg. Med. Chem. 2009, 17, 2623–2631. 10.1016/j.bmc.2008.10.044. [DOI] [PubMed] [Google Scholar]
- Lim T.-G.; Lee S.-Y.; Huang Z.; Lim D. Y.; Chen H.; Jung S. K.; Bode A. M.; Lee K. W.; Dong Z. Curcumin suppresses proliferation of colon cancer cells by targeting CDK2. Cancer Prev. Res. 2014, 7, 466–474. 10.1158/1940-6207.CAPR-13-0387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balasubramanian K. Molecular orbital basis for yellow curry spice curcumin’s prevention of Alzheimer’s disease. J. Agric. Food Chem. 2006, 54, 3512–3520. 10.1021/jf0603533. [DOI] [PubMed] [Google Scholar]
- Ciccone L.; Tepshi L.; Nencetti S.; Stura E. A. Transthyretin complexes with curcumin and bromo-estradiol: Evaluation of solubilizing multicomponent mixtures. New Biotechnol. 2015, 32, 54–64. 10.1016/j.nbt.2014.09.002. [DOI] [PubMed] [Google Scholar]
- Irwin J. J.; Duan D.; Torosyan H.; Doak A. K.; Ziebart K. T.; Sterling T.; Tumanian G.; Shoichet B. K. An aggregation advisor for ligand discovery. J. Med. Chem. 2015, 58, 7076–7087. 10.1021/acs.jmedchem.5b01105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coan K. E.; Shoichet B. K. Stoichiometry and physical chemistry of promiscuous aggregate-based inhibitors. J. Am. Chem. Soc. 2008, 130, 9606–9612. 10.1021/ja802977h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coan K. E. D.; Maltby D. A.; Burlingame A. L.; Shoichet B. K. Promiscuous aggregate-based inhibitors promote enzyme unfolding. J. Med. Chem. 2009, 52, 2067–2075. 10.1021/jm801605r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winter S.; Tortik N.; Kubin A.; Krammer B.; Plaetzer K. Back to the roots: Photodynamic inactivation of bacteria based on water-soluble curcumin bound to polyvinylpyrrolidone as a photosensitizer. Photochem. Photobiol. Sci. 2013, 12, 1795–1802. 10.1039/c3pp50095k. [DOI] [PubMed] [Google Scholar]
- Siviero A.; Gallo E.; Maggini V.; Gori L.; Mugelli A.; Firenzuoli F.; Vannacci A. Curcumin, a golden spice with a low bioavailability. Journal of Herbal Medicine 2015, 5, 57–70. 10.1016/j.hermed.2015.03.001. [DOI] [Google Scholar]
- Lao C. D.; Ruffin M. T. I. V.; Normolle D.; Heath D. D.; Murray S. I.; Bailey J. M.; Boggs M. E.; Crowell J.; Rock C. L.; Brenner D. E. Dose escalation of a curcuminoid formulation. BMC Complementary Altern. Med. 2006, 6, 10. 10.1186/1472-6882-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahlang B.; Pawar Y. B.; Bansal A. K. Identification of permeability-related hurdles in oral delivery of curcumin using the Caco-2 cell model. Eur. J. Pharm. Biopharm. 2011, 77, 275–282. 10.1016/j.ejpb.2010.12.006. [DOI] [PubMed] [Google Scholar]
- Volpe D. A.; Faustino P. J.; Ciavarella A. B.; Asafu-Adjaye E. B.; Ellison C. D.; Yu L. X.; Hussain A. S. Classification of drug permeability with a Caco-2 cell monolayer assay. Clin. Res. Regul. Aff. 2007, 24, 39–47. 10.1080/10601330701273669. [DOI] [Google Scholar]
- Suresh D.; Srinivasan K. Tissue distribution & elimination of capsaicin, piperine & curcumin following oral intake in rats. Indian J. Med. Res. 2010, 131, 682–691. [PubMed] [Google Scholar]
- Ravindranath V.; Chandrasekhara N. Absorption and tissue distribution of curcumin in rats. Toxicology 1980, 16, 259–265. 10.1016/0300-483X(80)90122-5. [DOI] [PubMed] [Google Scholar]
- Ravindranath V.; Chandrasekhara N. Metabolism of curcumin - studies with [3H]curcumin. Toxicology 1982, 22, 337–344. 10.1016/0300-483X(81)90027-5. [DOI] [PubMed] [Google Scholar]
- Mathews S.; Rao M. N. A. Interaction of curcumin with glutathione. Int. J. Pharm. (Amsterdam, Neth.) 1991, 76, 257–259. 10.1016/0378-5173(91)90278-V. [DOI] [Google Scholar]
- Asai A.; Miyazawa T. Occurrence of orally administered curcuminoid as glucuronide and glucuronide/sulfate conjugates in rat plasma. Life Sci. 2000, 67, 2785–2793. 10.1016/S0024-3205(00)00868-7. [DOI] [PubMed] [Google Scholar]
- Sharma R. A.; McLelland H. R.; Hill K. A.; Ireson C. R.; Euden S. A.; Manson M. M.; Pirmohamed M.; Marnett L. J.; Gescher A. J.; Steward W. P. Pharmacodynamic and pharmacokinetic study of oral Curcuma extract in patients with colorectal cancer. Clin. Cancer Res. 2001, 7, 1894–1900. [PubMed] [Google Scholar]
- Garcea G.; Berry D. P.; Jones D. J. L.; Singh R.; Dennison A. R.; Farmer P. B.; Sharma R. A.; Steward W. P.; Gescher A. J. Consumption of the putative chemopreventative agent curcumin by cancer patients: Assessment of curcumin levels in the colorectum and their pharmacodynamic consequences. Cancer Epidemiol., Biomarkers Prev. 2005, 14, 120–125. [PubMed] [Google Scholar]
- Johnson J. J.; Mukhtar H. Curcumin for chemoprevention of colon cancer. Cancer Lett. (N. Y., NY, U. S.) 2007, 255, 170–181. 10.1016/j.canlet.2007.03.005. [DOI] [PubMed] [Google Scholar]
- Vareed S. K.; Kakarala M.; Ruffin M. T.; Crowell J. A.; Normolle D. P.; Djuric Z.; Brenner D. E. Pharmacokinetics of curcumin conjugate metabolites in healthy human subjects. Cancer Epidemiol., Biomarkers Prev. 2008, 17, 1411–1417. 10.1158/1055-9965.EPI-07-2693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan E.; Tan M.; Xin J.; Sudarsanam S.; Johnson D. E. Interactions between traditional Chinese medicines and western therapeutics. Curr. Opin. Drug Discovery Dev. 2010, 13, 50–65. [PubMed] [Google Scholar]
- Hong D. H.; Son Y. K.; Choi I.-W.; Park W. S. The inhibitory effect of curcumin on voltage-dependent K+ channels in rabbit coronary arterial smooth muscle cells. Biochem. Biophys. Res. Commun. 2013, 430, 307–312. 10.1016/j.bbrc.2012.10.132. [DOI] [PubMed] [Google Scholar]
- Bamba Y.; Yun Y. S.; Kunugi A.; Inoue H. Compounds isolated from Curcuma aromatica Salisb. inhibit human P450 enzymes. J. Nat. Med. 2011, 65, 583–587. 10.1007/s11418-011-0507-0. [DOI] [PubMed] [Google Scholar]
- Gupta S. C.; Kismali G.; Aggarwal B. B. Curcumin, a component of turmeric: From farm to pharmacy. BioFactors 2013, 39, 2–13. 10.1002/biof.1079. [DOI] [PubMed] [Google Scholar]
- Schramm A.; Jahne E. A.; Baburin I.; Hering S.; Hamburger M. Natural products as potential human ether-a-go-go-related gene channel inhibitors - outcomes from a screening of widely used herbal medicines and edible plants. Planta Med. 2014, 80, 1045–1050. 10.1055/s-0034-1382907. [DOI] [PubMed] [Google Scholar]
- Xia M.; Shahane S. A.; Huang R.; Titus S. A.; Shum E.; Zhao Y.; Southall N.; Zheng W.; Witt K. L.; Tice R. R.; Austin C. P. Identification of quaternary ammonium compounds as potent inhibitors of hERG potassium channels. Toxicol. Appl. Pharmacol. 2011, 252, 250–258. 10.1016/j.taap.2011.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu C.-W.; Sheng Y.; Zhang Q.; Liu H.-B.; Xie X.; Ma W.-C.; Huo R.; Dong D.-L. Curcumin inhibits hERG potassium channels in vitro. Toxicol. Lett. 2012, 208, 192–196. 10.1016/j.toxlet.2011.11.005. [DOI] [PubMed] [Google Scholar]
- Zhang G.; Nitteranon V.; Chan L. Y.; Parkin K. L. Glutathione conjugation attenuates biological activities of 6-dehydroshogaol from ginger. Food Chem. 2013, 140, 1–8. 10.1016/j.foodchem.2013.02.073. [DOI] [PubMed] [Google Scholar]
- McFadden R.-M. T.; Larmonier C. B.; Shehab K. W.; Midura-Kiela M.; Ramalingam R.; Harrison C. A.; Besselsen D. G.; Chase J. H.; Caporaso J. G.; Jobin C.; Ghishan F. K.; Kiela P. R. The role of curcumin in modulating colonic microbiota during colitis and colon cancer prevention. Inflamm Bowel Dis. 2015, 21, 2483–2494. 10.1097/MIB.0000000000000522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta S. C.; Prasad S.; Kim J. H.; Patchva S.; Webb L. J.; Priyadarsini I. K.; Aggarwal B. B. Multitargeting by curcumin as revealed by molecular interaction studies. Nat. Prod. Rep. 2011, 28, 1937–1955. 10.1039/c1np00051a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghosh S.; Banerjee S.; Sil P. C. The beneficial role of curcumin on inflammation, diabetes and neurodegenerative disease: A recent update. Food Chem. Toxicol. 2015, 83, 111–124. 10.1016/j.fct.2015.05.022. [DOI] [PubMed] [Google Scholar]
- Oliveira A. S.; Sousa E.; Vasconcelos M. H.; Pinto M. Curcumin: A natural lead for potential new drug candidates. Curr. Med. Chem. 2015, 22, 4196–4232. 10.2174/0929867322666151029104611. [DOI] [PubMed] [Google Scholar]
- Kundu P.; Mohanty C.; Sahoo S. K. Antiglioma activity of curcumin-loaded lipid nanoparticles and its enhanced bioavailability in brain tissue for effective glioblastoma therapy. Acta Biomater. 2012, 8, 2670–2687. 10.1016/j.actbio.2012.03.048. [DOI] [PubMed] [Google Scholar]
- Dilnawaz F.; Singh A.; Sahoo S. K. Transferrin-conjugated curcumin-loaded superparamagnetic iron oxide nanoparticles induce augmented cellular uptake and apoptosis in K562 cells. Acta Biomater. 2012, 8, 704–719. 10.1016/j.actbio.2011.10.022. [DOI] [PubMed] [Google Scholar]
- Ni Z.; Xing F.; Wang P.; Cao G. Retracted: Synthesis, characterization and release of curcumin-intercalated Mg–Al-layered double hydroxides. Appl. Clay Sci. 2008, 40, 72–80. 10.1016/j.clay.2007.07.008. [DOI] [Google Scholar]
- Tomita M.; Kawakami H.; Uchihara J. N.; Okudaira T.; Masuda M.; Takasu N.; Matsuda T.; Ohta T.; Tanaka Y.; Mori N. Curcumin suppresses constitutive activation of AP-1 by downregulation of Jund protein in HTLV-1-infected T-cell lines. Leuk. Res. 2006, 30, 313–321. 10.1016/j.leukres.2005.08.004. [DOI] [PubMed] [Google Scholar]
- Mishra A.; Kumar R.; Tyagi A.; Kohaar I.; Hedau S.; Bharti A. C.; Sarker S.; Dey D.; Saluja D.; Das B. Curcumin modulates cellular AP-1, NF-kB, and HPV16 E6 proteins in oral cancer. ecancer 2015, 9, 525. 10.3332/ecancer.2015.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomita M.; et al. Retraction: Curcumin targets Akt cell survival signaling pathway in HTLV-I-infected T-cell lines. Cancer Sci. 2011, 102, 499. 10.1111/j.1349-7006.2010.01831.x. [DOI] [PubMed] [Google Scholar]
- Balasubramanyam K.; Varier R. A.; Altaf M.; Swaminathan V.; Siddappa N. B.; Ranga U.; Kundu T. K. Curcumin, a novel p300/CREB-binding protein-specific inhibitor of acetyltransferase, represses the acetylation of histone/nonhistone proteins and histone acetyltransferase-dependent chromatin transcription. J. Biol. Chem. 2004, 279, 51163–51171. 10.1074/jbc.M409024200. [DOI] [PubMed] [Google Scholar]
- Simon R. P.; Robaa D.; Alhalabi Z.; Sippl W.; Jung M. Katching-up on small molecule modulators of lysine acetyltransferases. J. Med. Chem. 2016, 59, 1249–1270. 10.1021/acs.jmedchem.5b01502. [DOI] [PubMed] [Google Scholar]
- Lu X.; Deng Y.; Yu D.; Cao H.; Wang L.; Liu L.; Yu C.; Zhang Y.; Guo X.; Yu G. Histone acetyltransferase p300 mediates histone acetylation of PS1 and BACE1 in a cellular model of Alzheimer’s disease. PLoS One 2014, 9, e103067. 10.1371/journal.pone.0103067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui L.; Miao J.; Cui L. Cytotoxic effect of curcumin on malaria parasite Plasmodium falciparum: Inhibition of histone acetylation and generation of reactive oxygen species. Antimicrob. Agents Chemother. 2007, 51, 488–494. 10.1128/AAC.01238-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kutluay S. B.; Doroghazi J.; Roemer M. E.; Triezenberg S. J. Curcumin inhibits herpes simplex virus immediate-early gene expression by a mechanism independent of p300/CBP histone acetyltransferase activity. Virology 2008, 373, 239–247. 10.1016/j.virol.2007.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang S.-K.; Cha S.-H.; Jeon H.-G. Curcumin-induced histone hypoacetylation enhances caspase-3-dependent glioma cell death and neurogenesis of neural progenitor cells. Stem Cells Dev. 2006, 15, 165–174. 10.1089/scd.2006.15.165. [DOI] [PubMed] [Google Scholar]
- Chen W.; Bacanamwo M.; Harrison D. G. Activation of p300 histone acetyltransferase activity is an early endothelial response to laminar shear stress and is essential for stimulation of endothelial nitric-oxide synthase mRNA transcription. J. Biol. Chem. 2008, 283, 16293–16298. 10.1074/jbc.M801803200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu J.; Khan Z. A.; Farhangkhoee H.; Chakrabarti S. Curcumin prevents diabetes-associated abnormalities in the kidneys by inhibiting p300 and nuclear factor-kappaB. Nutrition 2009, 25, 964–972. 10.1016/j.nut.2008.12.007. [DOI] [PubMed] [Google Scholar]
- Collins H. M.; Abdelghany M. K.; Messmer M.; Yue B.; Deeves S. E.; Kindle K. B.; Mantelingu K.; Aslam A.; Winkler G. S.; Kundu T. K.; Heery D. M. Differential effects of garcinol and curcumin on histone and p53 modifications in tumour cells. BMC Cancer 2013, 13, 37. 10.1186/1471-2407-13-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahlin J. L.; Nissink J. W. M.; Strasser J. M.; Francis S.; Higgins L.; Zhou H.; Zhang Z.; Walters M. A. PAINS in the assay: Chemical mechanisms of assay interference and promiscuous enzymatic inhibition observed during a sulfhydryl-scavenging HTS. J. Med. Chem. 2015, 58, 2091–2113. 10.1021/jm5019093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bora-Tatar G.; Dayangac-Erden D.; Demir A. S.; Dalkara S.; Yelekci K.; Erdem-Yurter H. Molecular modifications on carboxylic acid derivatives as potent histone deacetylase inhibitors: Activity and docking studies. Bioorg. Med. Chem. 2009, 17, 5219–5228. 10.1016/j.bmc.2009.05.042. [DOI] [PubMed] [Google Scholar]
- Wang S.-H.; Lin P.-Y.; Chiu Y.-C.; Huang J.-S.; Kuo Y.-T.; Wu J.-C.; Chen C.-C. Curcumin-mediated HDAC inhibition suppresses the DNA damage response and contributes to increased DNA damage sensitivity. PLoS One 2015, 10, e0134110/0134111–e0134110/0134119. 10.1371/journal.pone.0134110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link A.; Balaguer F.; Goel A. Cancer chemoprevention by dietary polyphenols: Promising role for epigenetics. Biochem. Pharmacol. (Amsterdam, Neth.) 2010, 80, 1771–1792. 10.1016/j.bcp.2010.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajendran P.; Ho E.; Williams D. E.; Dashwood R. H. Dietary phytochemicals, HDAC inhibition, and DNA damage/repair defects in cancer cells. Clin. Epigenet. 2011, 3, 4. 10.1186/1868-7083-3-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bustanji Y.; Taha M. O.; Almasri I. M.; Al-Ghussein M. A. S.; Mohammad M. K.; Alkhatib H. S. Inhibition of glycogen synthase kinase by curcumin: Investigation by simulated molecular docking and subsequent in vitro/in vivo evaluation. J. Enzyme Inhib. Med. Chem. 2009, 24, 771–778. 10.1080/14756360802364377. [DOI] [PubMed] [Google Scholar]
- Di Martino R. M.; De Simone A.; Andrisano V.; Bisignano P.; Bisi A.; Gobbi S.; Rampa A.; Fato R.; Bergamini C.; Perez D. I.; Martinez A.; Bottegoni G.; Cavalli A.; Belluti F. Versatility of the curcumin scaffold: Discovery of potent and balanced dual BACE-1 and GSK-3beta inhibitors. J. Med. Chem. 2016, 59, 531–544. 10.1021/acs.jmedchem.5b00894. [DOI] [PubMed] [Google Scholar]
- Zhang X.; Yin W. K.; Shi X. D.; Li Y. Curcumin activates Wnt/beta-catenin signaling pathway through inhibiting the activity of GSK-3beta in APPswe transfected SY5Y cells. Eur. J. Pharm. Sci. 2011, 42, 540–546. 10.1016/j.ejps.2011.02.009. [DOI] [PubMed] [Google Scholar]
- Yun J. H.; Park Y. G.; Lee K. M.; Kim J.; Nho C. W. Curcumin induces apoptotic cell death via Oct4 inhibition and GSK-3beta activation in NCCIT cells. Mol. Nutr. Food Res. 2015, 59, 1053–1062. 10.1002/mnfr.201400739. [DOI] [PubMed] [Google Scholar]
- Xiong Z.; Hongmei Z.; Lu S.; Yu L. Curcumin mediates presenilin-1 activity to reduce β-amyloid production in a model of Alzheimer’s disease. Pharmacol. Rep. 2011, 63, 1101–1108. 10.1016/S1734-1140(11)70629-6. [DOI] [PubMed] [Google Scholar]
- Dahlin J. L.; Inglese J.; Walters M. A. Mitigating risk in academic preclinical drug discovery. Nat. Rev. Drug Discovery 2015, 14, 279–294. 10.1038/nrd4578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang F.; Lim G. P.; Begum A. N.; Ubeda O. J.; Simmons M. R.; Ambegaokar S. S.; Chen P. P.; Kayed R.; Glabe C. G.; Frautschy S. A.; Cole G. M. Curcumin inhibits formation of amyloid beta oligomers and fibrils, binds plaques, and reduces amyloid in vivo. J. Biol. Chem. 2005, 280, 5892–5901. 10.1074/jbc.M404751200. [DOI] [PubMed] [Google Scholar]
- Hudson S. A.; Ecroyd H.; Kee T. W.; Carver J. A. The thioflavin T fluorescence assay for amyloid fibril detection can be biased by the presence of exogenous compounds. FEBS J. 2009, 276, 5960–5972. 10.1111/j.1742-4658.2009.07307.x. [DOI] [PubMed] [Google Scholar]
- Thapa A.; Jett S. D.; Chi E. Y. Curcumin attenuates amyloid-β aggregate toxicity and modulates amyloid-β aggregation pathway. ACS Chem. Neurosci. 2016, 7, 56–68. 10.1021/acschemneuro.5b00214. [DOI] [PubMed] [Google Scholar]
- Kayed R.; Head E.; Thompson J. L.; McIntire T. M.; Milton S. C.; Cotman C. W.; Glabe C. G. Common structure of soluble amyloid oligomers implies common mechanism of pathogenesis. Science (Washington, DC, U. S.) 2003, 300, 486–489. 10.1126/science.1079469. [DOI] [PubMed] [Google Scholar]
- Feng B. Y.; Shoichet B. K. A detergent-based assay for the detection of promiscuous inhibitors. Nat. Protoc. 2006, 1, 550–553. 10.1038/nprot.2006.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egan M. E.; Pearson M.; Weiner S. A.; Rajendran V.; Rubin D.; Gloeckner-Pagel J.; Canny S.; Du K.; Lukacs G. L.; Caplan M. J. Curcumin, a major constituent of turmeric, corrects cystic fibrosis defects. Science (Washington, DC, U. S.) 2004, 304, 600–602. 10.1126/science.1093941. [DOI] [PubMed] [Google Scholar]
- Song Y.; Sonawane N. D.; Salinas D.; Qian L.; Pedemonte N.; Galietta L. J. V.; Verkman A. S. Evidence against the rescue of defective ΔF508-CFTR cellular processing by curcumin in cell culture and mouse models. J. Biol. Chem. 2004, 279, 40629–40633. 10.1074/jbc.M407308200. [DOI] [PubMed] [Google Scholar]
- Dey I.; Shah K.; Bradbury N. A. Natural compounds as therapeutic agents in the treatment cystic fibrosis. J. Genet. Syndr. Gene Ther. 2016, 7, 284. 10.4172/2157-7412.1000284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seely K. A.; Levi M. S.; Prather P. L. The dietary polyphenols trans-resveratrol and curcumin selectively bind human CB1 cannabinoid receptors with nanomolar affinities and function as antagonists/inverse agonists. J. Pharmacol. Exp. Ther. 2009, 330, 31–39. 10.1124/jpet.109.151654. [DOI] [PubMed] [Google Scholar]
- Prather P. L.; Seely K. A.; Levi M. S. Notice of retraction. J. Pharmacol. Exp. Ther. 2009, 331, 1147. [PubMed] [Google Scholar]
- Sharma C.; Sadek B.; Goyal S. N.; Sinha S.; Kamal M. A.; Ojha S. Small molecules from nature targeting G-protein coupled cannabinoid receptors: Potential leads for drug discovery and development. Evidence-Based Complementary Altern. Med. 2015, 2015, 238482. 10.1155/2015/238482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Code of Federal Regulations Title 21. Part 182: Substances Generally Recognized as Safe. Section 182.20 Essential oils, oleoresins (solvent-free), and natural extractives (including distillates). U.S. Food and Drug Administration, 2016. [Google Scholar]
- Ringman J. M.; Bardens J.; Apostolova L. G.; Frautschy S. A.; Teng E.; Cole G. M.; Begum A. N.; Beigi M.; Gylys K. H.; Badmaev V.; Heath D. D.; Porter V.; Vanek Z.; Marshall G. A.; Hellemann G.; Sugar C.; Masterman D. L.; Montine T. J.; Cummings J. L. Oral curcumin for Alzheimer’s disease: Tolerability and efficacy in a 24-week randomized, double blind, placebo-controlled study. Alzheimer's Res. Ther. 2012, 4, 43. 10.1186/alzrt146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfizer . Bioequivalence study comparing a new 10 mg atorvastatin tablet to a 10 mg atorvastatin commercial tablet. https://clinicaltrials.gov/ct2/show/NCT00917579, 2009
- Sharma R. A.; Euden S. A.; Platton S. L.; Cooke D. N.; Shafayat A.; Hewitt H. R.; Marczylo T. H.; Morgan B.; Hemingway D.; Plummer S. M.; Pirmohamed M.; Gescher A. J.; Steward W. P. Phase I clinical trial of oral curcumin: Biomarkers of systemic activity and compliance. Clin. Cancer Res. 2004, 10, 6847–6854. 10.1158/1078-0432.CCR-04-0744. [DOI] [PubMed] [Google Scholar]
- Dhillon N.; Aggarwal B. B.; Newman R. A.; Wolff R. A.; Kunnumakkara A. B.; Abbruzzese J. L.; Ng C. S.; Badmaev V.; Kurzrock R. Phase II trial of curcumin in patients with advanced pancreatic cancer. Clin. Cancer Res. 2008, 14, 4491–4499. 10.1158/1078-0432.CCR-08-0024. [DOI] [PubMed] [Google Scholar]
- Asher G. N.; Spelman K. Clinical utility of curcumin extract. Altern. Ther. Health Med. 2013, 19, 20–22. [PubMed] [Google Scholar]
- Gupta S. C.; Patchva S.; Aggarwal B. B. Therapeutic roles of curcumin: Lessons learned from clinical trials. AAPS J. 2013, 15, 195–218. 10.1208/s12248-012-9432-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu C.-H.; Cheng A.-L. Clinical studies with curcumin. Adv. Exp. Med. Biol. 2007, 595, 471–480. 10.1007/978-0-387-46401-5_21. [DOI] [PubMed] [Google Scholar]
- Oppenheimer A. Turmeric (curcumin) in biliary diseases. Lancet 1937, 229, 619–621. 10.1016/S0140-6736(00)98193-5. [DOI] [Google Scholar]
- National Institutes of Health. "ClinicalTrials.gov." Registry and results database of clinical studies of human participants. http://clinicaltrials.gov (accessed October 6, 2016).
- Hurlstone D. P.; Karajeh M.; Sanders D. S.; Drew S. K.; Cross S. S. Rectal aberrant crypt foci identified using high-magnification-chromoscopic colonoscopy: Biomarkers for flat and depressed neoplasia. Am. J. Gastroenterol. 2005, 100, 1283–1289. 10.1111/j.1572-0241.2005.40891.x. [DOI] [PubMed] [Google Scholar]
- Mattson M. P.; Cheng A. Neurohormetic phytochemicals: Low-dose toxins that induce adaptive neuronal stress responses. Trends Neurosci. 2006, 29, 632–639. 10.1016/j.tins.2006.09.001. [DOI] [PubMed] [Google Scholar]
- Brondino N.; Re S.; Boldrini A.; Cuccomarino A.; Lanati N.; Barale F.; Politi P. Curcumin as a therapeutic agent in dementia: A mini systematic review of human studies. Sci. World J. 2014, 2014, 174282. 10.1155/2014/174282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandra V.; Pandav R.; Dodge H. H.; Johnston J. M.; Belle S. H.; DeKosky S. T.; Ganguli M. Incidence of Alzheimer’s disease in a rural community in India: The Indo-US study. Neurology 2001, 57, 985–989. 10.1212/WNL.57.6.985. [DOI] [PubMed] [Google Scholar]
- Ng T.-P.; Chiam P.-C.; Lee T.; Chua H.-C.; Lim L.; Kua E.-H. Curry consumption and cognitive function in the elderly. Am. J. Epidemiol. 2006, 164, 898–906. 10.1093/aje/kwj267. [DOI] [PubMed] [Google Scholar]
- Li S.; Yuan W.; Deng G.; Wang P.; Yang P.; Aggarwal B. B. Chemical composition and product quality control of turmeric (Curcuma longa l.). Pharm. Crops 2011, 2, 28–54. 10.2174/2210290601102010028. [DOI] [Google Scholar]
- Clark C. M.; Sheppard L.; Fillinbaum G. G.; Galasko D.; Morris J. C.; Koss E.; Mohs R.; Heyman A. Variability in annual mini-mental state examination score in patients with probable Alzheimer’s disease. Arch. Neurol. (Chicago) 1999, 56, 857–862. 10.1001/archneur.56.7.857. [DOI] [PubMed] [Google Scholar]
- Dahlin J. L.; Walters M. A. The essential roles of chemistry in high-throughput screening triage. Future Med. Chem. 2014, 6, 1265–1290. 10.4155/fmc.14.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atanasov A. G.; Waltenberger B.; Pferschy-Wenzig E. M.; Linder T.; Wawrosch C.; Uhrin P.; Temml V.; Wang L.; Schwaiger S.; Heiss E. H.; Rollinger J. M.; Schuster D.; Breuss J. M.; Bochkov V.; Mihovilovic M. D.; Kopp B.; Bauer R.; Dirsch V. M.; Stuppner H. Discovery and resupply of pharmacologically active plant-derived natural products: A review. Biotechnol. Adv. 2015, 33, 1582–1614. 10.1016/j.biotechadv.2015.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner H. Synergy research: Approaching a new generation of phytopharmaceuticals. Fitoterapia 2011, 82, 34–37. 10.1016/j.fitote.2010.11.016. [DOI] [PubMed] [Google Scholar]
- Gertsch J. The metabolic plant feedback hypothesis: How plant secondary metabolites nonspecifically impact human health. Planta Med. 2016, 82, 920–929. 10.1055/s-0042-108340. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.