Abstract
Objective
The primary objective of this systematic review is to assess the effectiveness of telemedicine in managing chronic heart disease patients concerning improvement in varied health attributes.
Design
This review follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) standard.
Setting
We adopted a logical search process used in two main research databases, the Cumulative Index to Nursing and Allied Health Literature and PubMed (MEDLINE). Four reviewers meticulously screened 151 abstracts to determine relevancy and significance to our research objectives. The final sample in the literature review consisted of 20 articles.
Main outcome measures
We looked for improved medical outcomes as the main outcome measure.
Results
Our results indicated that telemedicine is highly associated with the reduction in hospitalisations and readmissions (9 of 20 articles, 45%). The other significant attributes most commonly encountered were improved mortality and cost-effectiveness (both 40%) and improved health outcomes (35%). Patient satisfaction occurred the least in the literature, mentioned in only 2 of 20 articles (10%). There was no significant mention of an increase in patient satisfaction because of telemedicine.
Conclusions
We concluded that telemedicine is considered to be effective in quality measures such as readmissions, moderately effective in health outcomes, only marginally effective in customer satisfaction. Telemedicine shows promise on an alternative modality of care for cardiovascular disease, but additional exploration should continue to quantify the quality measures.
Keywords: Telemedicine, telehealth, cardiovascular disease, heart failure
Introduction
Poor lifestyle behaviors and lifestyle-related risk factors are the leading causes of both death and disability in the world.1 Cardiovascular disease accounts for about 17.3 million deaths worldwide, and smoking is responsible for nearly 10% of cardiovascular disease.2,3 Appropriate inpatient and outpatient disease management is critical for patients with heart disease because about 50% of chronic heart failure patients are re-hospitalised within six months of discharge.4 Following discharge, it is the responsibility of the patient to play an active role in maintaining his/her health for effective disease management. Monitoring the outpatient care of heart failure patients from a remote or rural area, telemonitoring, has emerged as an effective method in telemedicine. Since 2007, the World Health Organization has defined telehealth as
The delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities.5
We use this definition for our review, and, also following the WHO’s example, we do not distinguish between telemedicine and telehealth.
Because the patient has an active responsibility to monitor his/her cardiovascular disease, telemedicine becomes a natural extension of the clinical walls and enables a patient-to-provider link regardless of proximity to care. Between the Internet and cellular data networks, patients with cardiovascular disease can rapidly contact a provider and remove proximity from the equation of care, which can save valuable time in the treatment of such a critical and long-reaching disease.
Our primary objective for this review is to analyse the research in the literature concerning the effectiveness of telemedicine in managing chronic heart failure patients based on the following quality measures: patient satisfaction, health outcomes, hospital readmissions, the length of hospital stay, mortality and morbidity rates, cost-effectiveness, self-management, office visits and quality of life.
Methods
Overview
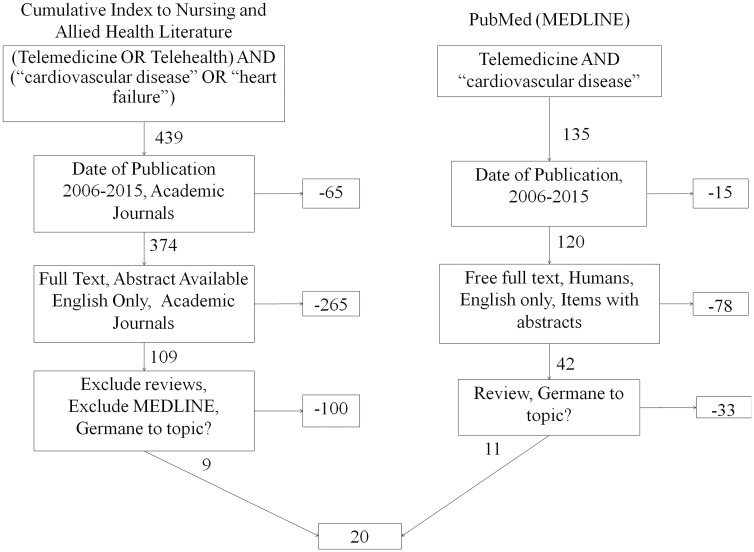
We started our research with a thorough and precise definition of terms and established research procedures and high-quality research indices (the Cumulative Index to Nursing and Allied Health Literature complete and PubMed/MEDLINE). Key terms for MEDLINE were identified through the US National Library of Medicine’s Medical Subject Headings (MeSH). Through the list of Medical Subject Headings, we were able to identify 78 subheadings that are included under the key term of Cardiovascular Disease and 11 subheadings under the key term of telemedicine; therefore, these became our key terms. Telehealth was not listed in PubMed, but when it was used as a search term, it resulted in telemedicine. Therefore, our search string for PubMed was telemedicine AND ‘cardiovascular disease’. Figure 1 illustrates the search process with inclusion and exclusion criteria.
Figure 1.
Search process with inclusion and exclusion criteria.
The identification of key terms for the Cumulative Index to Nursing and Allied Health Literature was not as simple because its catalog of search terms is not as robust as that of PubMed. We made an attempt to use inclusive search terms that comprised telemedicine OR telehealth AND cardiovascular disease OR heart failure. The search process with keywords included the use of Boolean search operators and quotation marks for exact phrases for the purpose of producing more focused and productive results. Initially, the search yielded 574 results, 439 of which were from the Cumulative Index to Nursing and Allied Health Literature and 135 were from PubMed.
Exclusion criteria
To exclude studies outside the period of study (2006–2015), we used filters. The search excluded 65 articles in the Cumulative Index to Nursing and Allied Health Literature and 15 articles in PubMed. Similar filters were used on both databases; on the Cumulative Index to Nursing and Allied Health Literature, we excluded all studies which did not include full text, abstract and those that were not published in academic journals and English. On PubMed, we excluded those studies that did not include full text, published in a language not English and studies that did not use human subjects. These filters removed 265 articles in the Cumulative Index to Nursing and Allied Health Literature and 78 articles in PubMed. To further refine the search, we excluded reviews and, in the Cumulative Index to Nursing and Allied Health Literature, those indexed in MEDLINE, which removed 100 articles.
The authors made a meticulous decision in evaluating whether the articles selected were germane to the study by manually reading all abstracts. This manual exclusion process removed 33 articles in PubMed, but none in the Cumulative Index to Nursing and Allied Health Literature. Among the articles that were excluded from the study, some were concerned only with telemedicine’s effectiveness in short-term diseases, while others mainly focused on m-health and e-health. Our evaluation criteria principally focused on research questions concerning the effectiveness of telemedicine in managing patients with heart disease based on various attributes. Articles not associated with the objectives of this literature review were eliminated. The final sample comprised 20 articles. The findings of these articles are summarised concisely in a table and trends were identified.
Results
Our research criteria enabled a meticulous evaluation of the effectiveness of telemedicine across multiple attributes: patient satisfaction, hospital readmissions, the number of physician and emergency department visits, the maximum length of hospital stay, cost-effectiveness, self-management, health outcomes, morbidity and mortality. These quality attributes became part of our search mechanism when analysing the articles (n = 20).
A final consensus was reached by four reviewers after comparing the prepared notes on articles. A terse summary of each article is delineated in Table 1. Articles are labelled by author and sorted by date of publication; the more recent articles are at the top of the table. The numbers for each article correspond to the references section.
Table 1.
Summary of results.
| Title | Findings |
|---|---|
| Siebert et al.4 | • ‘Telemedicine led to a reduction in physician and emergency department visits and significant improvement in control of chronic heart failure facilitating self-management for chronic heart failure patients’ |
| Straub et al.6 | • Increased quality of life • Substantial reduction in the frequency of repeated hospitalisations • Better self-management of disease by patients • Significant reduction in hospital costs • Reduction in length of hospital stays |
| Biermann et al.7 | • ‘Recent studies have shown clear clinical and economic benefits of Telemedicine solutions that focus on the patient and integrated care’ • To fulfill the growth promises further, attention is needed in areas of telemetric, medical information, and IT telematics infrastructure |
| van Montfort et al.8 | • Use of Telemedicine technology in managing heart failure promotes a healthier lifestyle and enhances quality of life |
| Cleland et al.9 | • ‘Duration of admissions was found to be significantly shorter with Telemedicine technology’ • Decrease in number of office visits • Cost-effective • Significant reduction in hospitalisations and mortality rates when compared with usual care |
| Bashshur et al.10 | • ‘Reduced length and number of hospital stays and readmissions, optimised medical therapy and better quality of life’ • Improved health outcomes • Significant reduction in mortality • Substantial savings in travel costs • Significantly lower outpatient and emergency visits • Fewer episodes of health worsening |
| Conway et al.11 | • ‘Non-invasive remote monitoring of heart failure with the use of Telemedicine technology was found to be effective in reducing the risk of all-cause mortality and heart failure-related hospitalisations and in improving health outcomes’ |
| Wootton et al.12 | • ‘Majority of studies conducted have reported positive effects concerning outcomes. However, the evidence base for the value of Telemedicine in managing chronic diseases was reported to be weak and contradictory’ |
| Seto et al.13 | • The results show an ‘evidence of improved quality of life through improved self-care and clinical management of disease with the aid of mobile phone-based telemonitoring system. However, no differences were found between intervention group and control group in terms of hospitalisations, mortality, and emergency department visits’ |
| Kotb et al.14 | • ‘Telemedicine interventions that involved the use of electrocardiographic data transmission were significantly effective in reducing mortality rates and hospitalisations related to heart failure when compared with usual care’ |
| Koehler et al.15 | • Several studies on impact of Telemedical care in chronic heart failure patients have reported reduction in ○ Healthcare costs ○ Hospitalisations ○ Mortality • Also, improvements in quality of life have been reported. |
| Backman et al.16 | • Electrocardiographic recordings via telephonic transmission of Telemedicine technology resulted in reduced hospitalisations, re-admission rates, time, and costs |
| Brignell et al.17 | • Results showed considerable levels of patient satisfaction when measured using remote Telemedicine technology |
| Domingo et al.18 | • Results showed that with ‘frequent monitoring and patient management using a Telemedicine system, hospitalisations, length of hospital stay, and emergency department visits were reduced’ |
| Klersy et al.19 | • A meta-analysis by the authors demonstrated that Telehealth programs resulted in substantial decrease in mortality, hospitalisation, and chronic heart failure-related length stay |
| Kenealy et al.20 | • Results unveiled improvement in health outcomes, quality of life, decreased anxiety and depression levels, decreased mortality, and improved self-management |
| Salisbury et al.21 | • ‘Improved health, access to care, self-management, patient experience, and cost-effective care were the intended outcomes that were achieved through TElehealth in CHronic disease conceptual model’ • Secondary outcomes were health-related quality of life, measures of access, and patient satisfaction |
| Seto et al.22 | • The study reported that Telemedicine technology which included monitoring from a remote area resulted in improved self-care by the patients |
| Koehler et al.23 | • Few meta-analyses suggest a significant reduction in morbidity and mortality in patients with heart failure. However, the effectiveness of Telemedicine has not been clearly established and requires an adequate research |
| Black et al.24 | • The study unveils that ‘completion of Better Effectiveness After Transition-Heart Failure is meant to serve an important research source in understanding the use of Telehealth in improving health outcomes and hospital readmissions in heart failure patients’ |
In order to identify the frequency of occurrence of attributes in the literature, we also created an affinity matrix that is illustrated in Table 2. Quality attributes are sorted by frequency of occurrence in the literature. The percentages correspond to the number of occurrence of that one attribute compared to the sum of all occurrences, which was 58.
Table 2.
Affinity matrix showing frequency of occurrence in the literature.
| Attributes | Occurrences | Instances of the attributes (%) |
|---|---|---|
| Hospitalisations and re-admissions | 4,8–10,13–15, 18,19 | 9 (15.5) |
| Mortality | 8,10,13,14,19,20,23,24 | 8 (13.8) |
| Cost-effectiveness | 4,6,8,9,14,15,21 | 7 (12.0) |
| Health outcomes | 7,9-12,20,21 | 7 (12.0) |
| Quality of life | 4,7,9,14,20,22 | 6 (10.3) |
| Self-management | 4,12,16,20–22 | 6 (10.3) |
| Length of hospital stay | 4,8,9,18,19 | 5 (8.6) |
| Number of physician and emergency department visits | 8,9,16,18 | 4 (6.9) |
| Morbidity | 6,9,16,23 | 4 (6.9) |
| Patient satisfaction | 17,21 | 2 (3.3) |
We identified 10 attributes of quality for this review, and we found these attributes throughout our sample (n = 20) Among all the attributes mentioned in the literature, 13 articles addressed hospitalisations and ED visits (13 of 20, 65%).
A total of 9 out of 20 articles (45%) reported a significant reduction in hospitalisations and readmissions as a result of using telemedicine. This attribute was mentioned 9 of 58 occurrences (15.5%).4,8–10,13–15,18,19 The mortality attribute was mentioned 8 times (13.8%).8,10,13,14,19,20,23,24 Two attributes were mentioned seven times: cost-effectiveness4,6,8,9,14,15,21 and improved health outcomes,7,9–12,21,22 which each represent 12.0% of total occurrences of attributes in the literature.
Two attributes were addressed in 6 of 20 articles (30% of all occurrences): greater quality of life compared to traditional modalities of care4,7,9,14,21,23 and an increase in self-management when using the modality of telemedicine.4,12,16,20–22 Also, five out of 20 articles (25%) reported a decrease in the length of hospital stay due to longer follow-up periods, and this accounted for 8% of all occurrences of attributes.4,8,9,18,19
Two attributes occurred in 4 of 20 articles which together represent 13.8% of total occurrences: decrease in the number of physician and emergency room visits8,9,16,18 and a reduction in morbidity.6,9,16,23 Notably, only 2 in 20 articles (10%) reported better rates of patient satisfaction, which accounted for only 3% of total attribute occurrences.17,21
Discussion
The authors of this systematic review made an attempt to comprehend the effectiveness of telemedicine which has many positive effects among heart failure patients. Apart from identifying the effectiveness of telemedicine in the improvement of attributes, the authors also identified the elements that need to be further investigated. Though this systematic review evaluates the similar inclusive aspects of the effectiveness of telemedicine from other articles,25–27 our findings report the effectiveness of telemedicine from a global perspective using quality lexicon to identify attributes of effectiveness. None of the studies we analysed revealed the frequency of occurrence of each attribute with statistical significance. Our study identifies positive effects across 20 articles globally, which include the United States, the United Kingdom, Canada, the Netherlands, Germany, Australia and smaller countries in Europe. The motive of our systematic review was not to replicate the work of other researchers.
The introduction of telemedicine into the care process of cardiovascular disease patients has revolutionised healthcare in terms of modality, and it has improved many quality attributes associated with it. The authors of this review found many attributes which reflect the effectiveness of telemedicine in cardiovascular disease patients. The main attributes with increased number of instances were reduced hospitalisation and readmissions,4,8–10,13–15,18,19 improved mortality rates,8,10,13,14,19,20,23,24 increased cost-effectiveness,4,6,8,9,14,15,21 and improved health outcomes,7,9–12,20,21 improved quality of life4,7,9,14,20,22 and an increase in self-management of cardiovascular disease.4,12,16,20–22 These attributes comprised up to 75% of all occurrences of attributes found in the literature.
Significant reduction in hospitalisation and increased self-management by patients epitomises the economic perceptive of telemedicine, since it has helped reduce the monetary side of re-admittance of patients. Telemedicine has made remote monitoring a possibility, which has helped physicians in monitoring and administering post-operative care that the patient or his immediate family can easily manage, expanding the capabilities of the existing health work force without increasing the size of the health work force. Reduction in hospital stay, cost-effectiveness and improved outcomes are three attributes that are consistent with other reviews that looked at telemedicine to help manage heart failure.25–27
This literature review summarises the positive outcomes as reported by studies on telemedicine. However, there are inconsistencies in the literature as well as illustrated; ‘the evidence base for the efficacy of telemedicine technology in managing chronic heart failure in terms of outcomes was reported to be weak and contradictory’.12 There are certain doubts in the industry and positive areas for exploitation that are worth studying. Additionally, the external validity of some articles was weak due to the small sample size. In some studies, the patient’s condition or the kind of care was not same or varied in complexity. In addition, telemedicine requires high-speed internet to transmit the data to and from remote areas in order for timely information to be relevant, but it is the rural areas that often lack high-speed connectivity. Furthermore, not all patients and doctors accept telemedicine. The evidence for cost reduction has not been strong enough to prove that telemedicine was the sole reason for the reduction since there could be many other factors. Hence, there is still room for a wide range of studies to prove quantitatively that telemedicine is a definitive reason for increased quality attributes.
Limitations
This review is subject to much of the same bias that other studies experience. Publication bias can impose influence because we did not have immediate access to studies that were not published. Another bias is selection bias. Our selection criteria could have screened out factors that would change our conclusions. We attempted to control the selection bias through our initial definition of terms and multiple consensus meetings.
Our systematic review evaluated only those articles that were published during the specified period from 2006 to 2015 and did not review the articles from other years. The main reason for the selection of this specified period is that we felt 10 years was a sufficient amount of time to gather material germane to our objectives. Another factor that weighed into the selection of time was America’s passage of the Affordable Care Act which created mechanisms of reimbursement for telemedicine. We felt that several years prior and after its emergence would be a sufficient amount of time to examine the telemedicine landscape across multiple countries.
Conclusion
Overall, telemedicine has been found to be effective in managing cardiovascular disease; however, an in-depth evaluation of its effectiveness, in certain aspects, such as patient satisfaction and cost-effectiveness is imperative. The authors suggest that further improvements in the provision of healthcare services by telemedicine through appropriate training of the providers and patient education would most likely result in increased patient satisfaction and better health outcomes.
Declarations
Competing Interests
None declared.
Funding
None declared.
Ethical approval
Not applicable.
Guarantor
CSK
Contributorship
MS designed the study and conducted the searches in indices (20%). NTN composed the introduction and methods as well as part of the discussion sections (20%). DP composed the results and parts of the discussion (20%). MS and NTN served as master editor, compiled the search results into a table for evaluation, and composed the abstract, conclusions and references (20%). MB and CSK provided critical analysis and revising of all portions of the manuscript and authorised the final version for publication (20%). CSK is responsible for all revisions and maintains contact with the rest of the review team with status reports.
Acknowledgements
None.
Provenance
Not commissioned; peer-reviewed by Grace Carolan-Rees.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics – 2016 update. Circulation 2015; 133. [DOI] [PubMed]
- 2.World Health Organization. Causes of death 2008 summary tables. WHO subregions by country. Geneva: WHO, 2011.
- 3.Mendis S, Puska P and Norrving B (eds). Global atlas on cardiovascular disease prevention and control. Geneva: World Health Organization, 2011.
- 4.Seibert PS, Whitmore TA, Patterson C, Parker PD, Otto C, Basom J, et al. Telemedicine facilitates CHF home health care for those with systolic dysfunction. Int J Telemed Appl 2008; 2008:3. [DOI] [PMC free article] [PubMed]
- 5.World Health Organization. Telemedicine: opportunities and developments in Member States: report on the second global survey on eHealth. Geneva: World Health Organization, 2010.
- 6.Straub C, Haas AK, Mex J. Telemedicine in heart disease: role of remote patient management in guideline-based heart failure care. Dis Manage Health Outcomes 2006; 14: 15–18. [Google Scholar]
- 7.Biermann CW, Schumacher N, Luhmann B, Habetha J, Pelc N. Future of Telemedicine in Heart Disease. Dis Manage Health Outcomes 2006; 14(Suppl): 43–47. [Google Scholar]
- 8.van Montfort AP, van der Helm MH. Telemonitoring of patients with chronic heart failure. Dis Manage Health Outcomes 2006; 14(Suppl): 33–35. [Google Scholar]
- 9.Cleland JG. The Trans-European Network – Home-Care Management System (TEN–HMS) Study: an investigation of the effect of telemedicine on outcomes in Europe. Dis Manage Health Outcomes 2006; 14(Suppl): 23–28. [Google Scholar]
- 10.Bashshur RL, Shannon GW, Smith BR, Alverson DC, Antoniotti N, Barsan WG, et al. The empirical foundations of telemedicine interventions for chronic disease management. Telemed e-Health 2014; 20: 769–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Conway A, Inglis SC, Clark RA. Effective technologies for noninvasive remote monitoring in heart failure. Telemed e-Health 2014; 20: 531–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wootton R. Twenty years of telemedicine in chronic disease management – an evidence synthesis. J Telemed Telecare 2012; 18: 211–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seto E, Leonard KJ, Cafazzo JA, Barnsley J, Masino C, Ross HJ. Mobile phone-based telemonitoring for heart failure management: a randomized controlled trial. J Med Internet Res 2012; 14: e31–e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kotb A, Cameron C, Hsieh S, Wells G. Comparative effectiveness of different forms of telemedicine for individuals with heart failure (HF): a systematic review and network meta-analysis. PloS One 2015; 10: e0118681–e0118681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koehler F, Winkler S, Schieber M, Sechtem U, Stangl K, Böhm M, et al. Telemedical interventional monitoring in heart failure (TIM-HF), a randomized, controlled intervention trial investigating the impact of telemedicine on mortality in ambulatory patients with heart failure: study design. Eur J Heart Fail 2010; 12: 1354–1362. [DOI] [PubMed] [Google Scholar]
- 16.Backman W, Bendel D, Rakhit R. The telecardiology revolution: improving the management of cardiac disease in primary care. J R Soc Med 2010; 103: 442–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brignell M, Wootton R, Gray L. The application of telemedicine to geriatric medicine. Age Ageing 2007; 36: 369–374. [DOI] [PubMed] [Google Scholar]
- 18.Domingo M, Lupón J, González B, Crespo E, López R, Ramos A, et al. Noninvasive remote telemonitoring for ambulatory patients with heart failure: effect on number of hospitalizations, days in hospital, and quality of life. CARME (CAtalan Remote Management Evaluation) study. Revista Española de Cardiología (English Edition) 2011; 64: 277–285. [DOI] [PubMed] [Google Scholar]
- 19.Klersy C, De Silvestri A, Gabutti G, Regoli F, Auricchio A. A meta-analysis of remote monitoring of heart failure patients. J Am Coll Cardiol 2009; 54: 1683–1694. [DOI] [PubMed] [Google Scholar]
- 20.Kenealy TW, Parsons MJ, Rouse AP, Doughty RN, Sheridan NF, Hindmarsh JK, et al. Telecare for diabetes, CHF or COPD: effect on quality of life, hospital use and costs. A randomised controlled trial and qualitative evaluation. PloS One 2015; 10: e0116188–e0116188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Salisbury C, Thomas C, O'Cathain A, Rogers A, Pope C, Yardley L, et al. TElehealth in CHronic disease: mixed-methods study to develop the TECH conceptual model for intervention design and evaluation. BMJ Open 2015; 5: e006448–e006448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Seto E, Leonard KJ, Cafazzo JA, Barnsley J, Masino C, Ross HJ. Perceptions and experiences of heart failure patients and clinicians on the use of mobile phone-based telemonitoring. J Med Internet Res 2012; 14: e25–e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Koehler F, Winkler S, Schieber M, Sechtem U, Stangl K, Böhm M, et al. Impact of remote telemedical management on mortality and hospitalizations in ambulatory patients with chronic heart failure the telemedical interventional monitoring in heart failure study. Circulation 2011; 123: 1873–1880. [DOI] [PubMed] [Google Scholar]
- 24.Black JT, Romano PS, Sadeghi B, Auerbach AD, Ganiats TG, Greenfield S, et al. A remote monitoring and telephone nurse coaching intervention to reduce readmissions among patients with heart failure: study protocol for the Better Effectiveness After Transition-Heart Failure (BEAT-HF) randomized controlled trial. Trials 2014; 15: 124–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Canadian Agency for Drugs and Technologies in Health. Telehealth for patients with heart failure: a review of the clinical effectiveness, cost-effectiveness and guidelines, www.ncbi.nlm.nih.gov/pubmedhealth/PMH0084276/ (2015, accessed 22 December 2016). [PubMed]
- 26.Inglis SC, Clark RA, McAlister FA, Stewart S, Cleland JG. Which components of heart failure programmes are effective? A systematic review and meta-analysis of the outcomes of structured telephone support or telemonitoring as the primary component of chronic heart failure management in 8323 patients: abridged Cochrane Review. Eur J Heart Fail 2011; 13: 1028–1040. [DOI] [PubMed] [Google Scholar]
- 27.Hameed AS, Sauermann S, Schreier G. The impact of adherence on costs and effectiveness of telemedical patient management in heart failure: a systematic review. Appl Clin Inform 2014; 5: 612–612. [DOI] [PMC free article] [PubMed] [Google Scholar]