Abstract
Background:
Osteochondritis dissecans (OCD) lesions are often observed in the humeral capitellum both in young baseball players and gymnasts. It is generally believed that capitellar OCD in baseball players can be seen on an anteroposterior (AP) radiograph with the elbow in 45° of flexion. However, the mechanism of injury seems to be different in baseball players and gymnasts. Repetitive valgus overload with the elbow in flexion is believed to be the cause of capitellar OCD lesions in baseball players, whereas weightbearing with the elbow in extension may be the cause of OCD in gymnasts.
Purpose:
To determine the difference in capitellar OCD location between baseball players and gymnasts and to propose the optimal AP radiographic angle of the elbow for visualization of early-stage OCD lesions in adolescent gymnasts.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
Subjects consisted of 95 baseball players (95 elbows) and 21 gymnasts (24 elbows) with a mean age of 13.7 years (range, 11-18 years). To localize the lesion, inclination of the affected area in the humeral capitellum against the humeral axis was investigated using sagittal computed tomography images of the elbow. The inclination angle was defined as the angle between the long axis of the humerus and the line perpendicular to a line that connected the anterior and posterior margin of the lesion. The inclination angle in each group was compared and statistically analyzed.
Results:
The mean inclination angle was 57.6° ± 10.7° in baseball players and 28.0° ± 10.7° in gymnasts. Capitellar OCD lesions were located more anterior in baseball players when compared with gymnasts (P < .01).
Conclusion:
Due to differences in applied stress, capitellar OCD lesions in baseball players were located more anteriorly compared with those seen in gymnasts. Therefore, although AP radiographs with the elbow in 45° of flexion are optimal for detecting OCD lesions in baseball players, radiographs with less elbow flexion or full extension are more useful in gymnasts, especially in early-stage OCD.
Keywords: osteochondritis dissecans, capitellum, baseball players, gymnasts
Osteochondritis dissecans (OCD) is often observed in the humeral capitellum in skeletally immature athletes. Although the etiology of capitellar OCD still remains unknown, microtrauma and ischemia are believed to play a critical role.1,13 In overhead throwing athletes, the elbow is subjected to valgus overload with significant compression and shear forces applied to the radiocapitellar joint between 30° and 90° of flexion, and with repetitive overhead throwing these may cause capitellar OCD.7,9,10 It is generally believed that anteroposterior (AP) radiographs with the elbow in 45° of flexion is the best position to detect capitellar OCD in baseball players.15,16 However, several gymnasts with early-stage capitellar OCD lesions had lesions that were not detected with 45° AP radiography but rather with radiographs performed in full extension (Figure 1). Although only a limited number of articles have reported OCD lesions in young gymnasts, gymnastics requires forceful weightbearing with the elbow in full extension.3,4,6 Therefore, we hypothesized that the location of the capitellar OCD lesion may be different between baseball players and gymnasts. The purpose of this study was to investigate the difference in locations of the capitellar OCD lesions in baseball players and gymnasts and to determine optimal elbow positioning for AP radiographs used to visualize capitellar OCD in gymnasts.
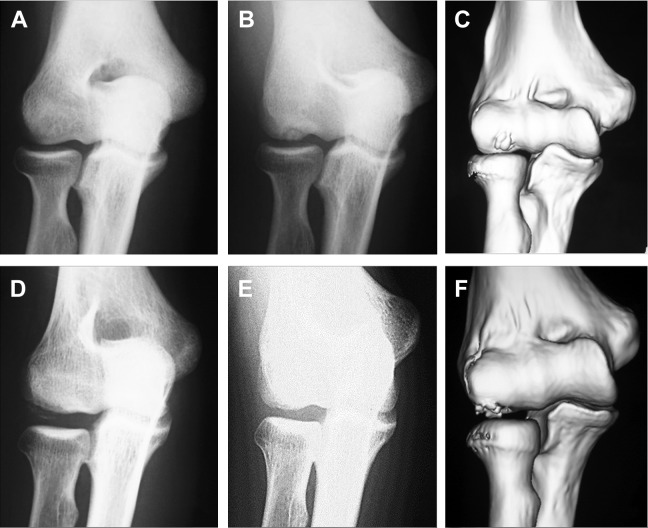
Figure 1.
(A, B, D, and E) Radiographs and (C and F) 3-dimensional computed tomography (3D CT) images of the elbow in (A, B, and C) a 15-year-old baseball player and (D, E, and F) a 16-year-old gymnast with osteochondritis dissecans (OCD) of the humeral capitellum. OCD lesion of the humeral capitellum cannot be detected in the (A) anterior-posterior (AP) view with the elbow in full extension, while the OCD lesion is clearly seen in (B) the AP view with the elbow in 45° of flexion and (C) 3D CT image. On the other hand, OCD lesion is not clearly seen in (E) the AP view with the elbow in 45° of flexion. However, the OCD lesion is clearly seen in (D) the AP image with the elbow in a full extension and (F) 3D CT image.
Methods
Our diagnostic protocol for patients suspected of having capitellar OCD includes bilateral AP radiographs with the elbow in full extension and 45° of flexion and lateral views. A consecutive series of 119 elbows in 116 patients with OCD of the humeral capitellum imaged between 2004 and 2011 were included in this study. Surgical procedures included arthroscopic debridement, resection of loose bodies, and/or open osteochondral autograft transplantation. Subjects consisted of 95 male baseball players (95 elbows) with a mean age of 13.7 years (range, 11-18 years) and 21 gymnasts (24 elbows; 8 males, 16 females) with a mean age of 13.5 years (range, 11-16 years).
Preoperative sagittal computed tomography (CT) images of the elbow were retrospectively analyzed and used to determine the location of the lesions in both groups of athletes. All CT images were obtained using the same machine (Alexion; Toshiba Medical Systems).
Sagittal CT images across the center of the capitellar OCD lesion were obtained in all subjects. The sagittal images were used for the following measurements. First, a line that connected the most anterior and posterior point of the lesion was drawn (line A). Next, to determine the humeral axis, 2 transverse lines were drawn across the distal humeral shaft that connected the anterior and posterior cortices, and a line was drawn down the humeral axis, connecting the midpoints of the 2 cross-humeral lines (line B). We chose 1 sagittal CT image that demonstrated the OCD lesion most clearly and used this image for calculation. However, if we were not able to determine the location of the humeral axis using this image, another sagittal image that clearly demonstrated both anterior and posterior humeral shaft cortical bone was used to determine the humeral axis. The axis line was then transcribed to the former image with reference to landmarks of the humerus. The inclination angle was determined as the angle between the humeral axis and the line perpendicular to the line A (line C) (Figure 2).
Figure 2.

The inclination angle was measured using a slice that clearly demonstrates the osteochondritis dissecans (OCD) lesion on the sagittal computed tomography image of the elbow. (A) Line connecting the anterior and posterior margin of the OCD lesion; (B) line parallel to the axis of the humerus; (C) line perpendicular to line A; (D) inclination angle, measured as an angle between lines B and C.
Reproducibility of measurements was estimated by calculating the intraclass correlation coefficient (ICC) of 2 investigators’ measurements of 10 randomly chosen CT scans 6 times. Intra- and interobserver reproducibility were 0.998 and 0.984, respectively. The inclination angle was compared between baseball players and gymnasts and statistically analyzed using the Student t test.
Results
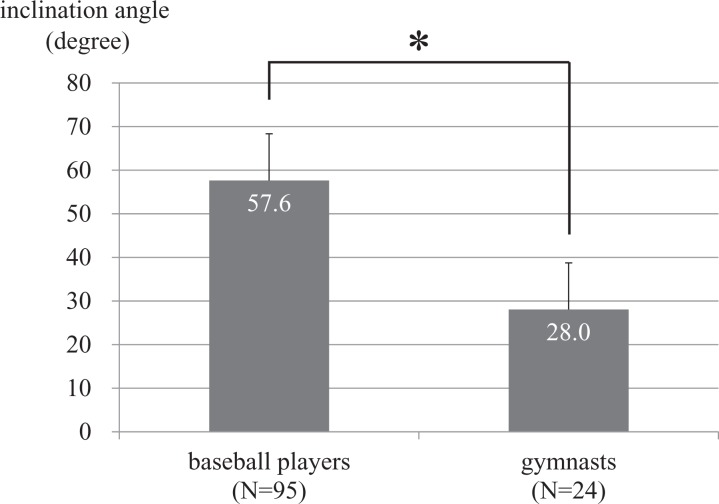
The mean inclination angle was 57.6° ± 10.7° in baseball players (Figure 3) and 28.0° ± 10.7° in true gymnasts. This difference was statistically significant (P < .01) (Figure 4).
Figure 3.
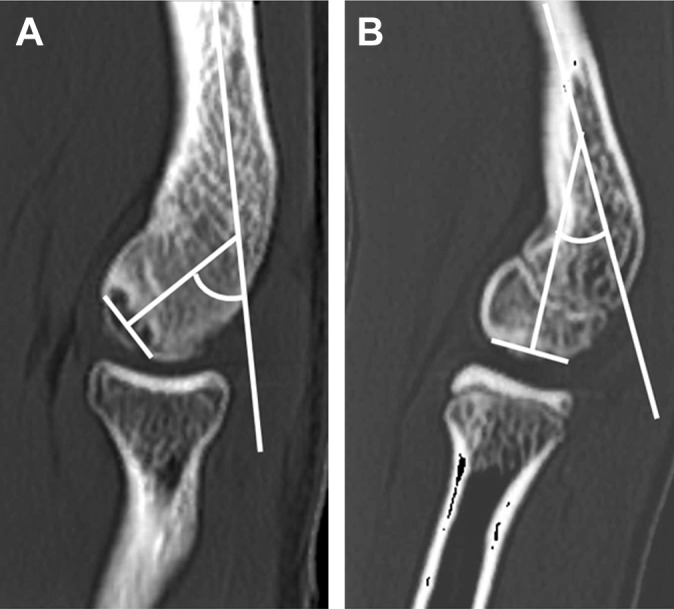
Representative cases. (A) Osteochondritis dissecans (OCD) lesion seen in a 13-year-old baseball player. The inclination angle measures 57°. (B) OCD lesion seen in an 11-year-old gymnast. The inclination angle measures 28°.
Figure 4.
Inclination angle of baseball players and gymnasts. The mean inclination angle was significantly greater in baseball players when compared with gymnasts (*P < .01).
Discussion
Radiography of the elbow is commonly performed as the first diagnostic study for OCD of the humeral capitellum, and some modifications have been reported to improve the sensitivity of radiographs.13,16 Because typical capitellar OCD lesions in baseball players are located in the anterior aspect of the capitellum, the AP view with the elbow in 45° of flexion is recommended.16 In the present study, the sagittal inclination angle in baseball players was 57.6°. In contrast, OCD lesions in gymnasts were more distal in the capitellum, and the inclination angle was 28.0°. Consequently, radiographs with the elbow in 45° of flexion are the most useful when evaluating OCD lesions in baseball players, while those in full extension are most useful in gymnasts.
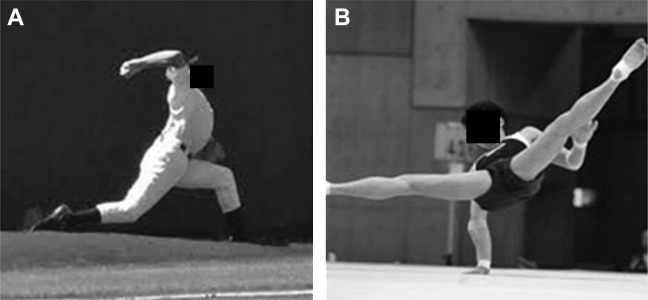
Many hypotheses regarding the etiology of OCD have been proposed, including microtrauma, ischemia, disordered ossification, and genetic predisposition.1 There are some reports about familial cases of OCD,5,8 and these reports stated a genetic predisposition for OCD lesions. On the other hand, repetitive microtrauma to the capitellum of the elbow is thought to be one of the primary causes of OCD.1 In baseball players, the pathogenesis of capitellar OCD may be high compression and shear forces on the radiocapitellar joint that occur during the late cocking and early acceleration phases of throwing, when the elbow is flexed from 30° to 90° (Figure 5A).7,9,10 In a CT osteoabsorptiometry study in baseball players, Momma et al11 reported the stress distribution to the anterior part of the capitellum, which supports the hypothesis that high compression and shear have an important role in the development of elbow OCD in baseball players. However, gymnasts load the radiocapitellar joint with their elbows fully extended, and that force seems to cause capitellar OCD (Figure 5B).3,4,6 In our study, the difference in the sagittal location of the lesions between baseball players and gymnasts was identified, and the OCD lesions of the gymnasts occurred more distally in the capitellum than those of the baseball players. The difference in elbow flexion angle at which the highest compression force occurred between the capitellum and radial head may greatly contribute to the difference in location of the lesions. This suggests that repetitive microtrauma to the capitellum might be one of the most important factors in pathogenesis of OCD in adolescent athletes.
Figure 5.
Typical arm positions of baseball players and gymnasts that provide maximum stress to the proximal radiocapitellar joint. (A) In baseball players, a late cocking to acceleration phase during throwing causes maximum valgus overload to the elbow. (B) In gymnasts, on the other hand, weightbearing with the elbow in extension causes maximum stress.
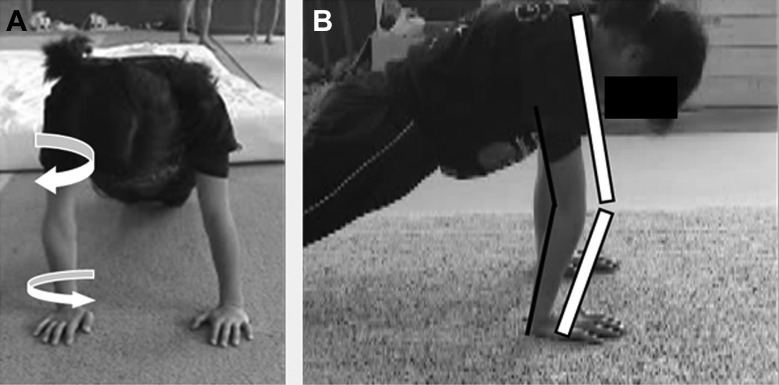
To analyze the stress to the radiocapitellar joint in different sports, it is important to consider the elbow kinetics in each sport. In throwing athletes, movement of the entire body including hip, trunk, and scapular function is extremely important to achieve optimal throwing mechanics and reduce valgus extension stress overload.14 Suboptimal throwing mechanics may adversely influence the open kinetic chain of the pitching motion, which may lead to elbow pathology.2 In adolescent baseball players, throwing mechanics are often poor, resulting in valgus stress to the elbow. This may be the main cause of elbow problems in young throwers. On the other hand, mechanical stress to the elbow during upper extremity weightbearing may contribute to development of the capitellar OCD in gymnasts. Gymnasts who develop capitellar OCD tend to demonstrate scapular dyskinesis similar to baseball players. Morrey et al12 reported that radiocapitellar force transmission was consistently greater in magnitude when the forearm was in pronation than in supination. Since scapular dyskinesis restricts internal rotation of the humerus, it forces the forearm in a pronated position during weightbearing, causing excessive stress to the radiocapitellar joint of the elbow (Figure 6). In addition, hyperextension of the elbow during weightbearing, which seems to be similar to the “bony locking position” of the knee joint in recurvatum, may also cause excessive stress to the radiocapitellar joint (Figure 6). Weakness of the triceps brachii muscle, limitation of upward rotation of the scapula, and tightness of internal rotation of the glenohumeral joint might also contribute to this condition. However, the relationship between the weightbearing position of the elbow in gymnasts and OCD of the capitellum is still unclear, and further studies are needed to clarify etiology.
Figure 6.
Possible pathomechanism of the capitellar osteochondritis dissecans (OCD) in gymnasts. (A) Weightbearing position with the humerus in external rotation due to scapular dyskinesis. The forearm needs to be in a pronated position during weightbearing (the cubital fossa needs to face front). (B) Weightbearing position with the elbow in hyperextension due to weakness of the triceps muscle.
There were some limitations in this study. First, the present study was a retrospective case series and did not include assessment of range of motion or outcomes scores. Determining the difference in outcomes of OCD of the humeral capitellum between athletes in baseball, gymnastics, and sports would be important. Second, all subjects were treated surgically so they had an advanced stage of OCD. We used CT images of the advanced OCD lesions in the center of the capitellum to determine the inclination angle. However, the early stage of OCD lesions was not evaluated. Additional radiation exposure caused by CT scanning was unwarranted for patients who were likely to be treated with conservative therapy. Takahara et al15 reported that ultrasonography was effective in detecting early-stage capitellar OCD, and we believe that another study with ultrasonography could potentially determine the sagittal location of the humeral capitellum in the initial stage of OCD in athletes participating in different sports.
Footnotes
The authors declared that they have no potential conflicts of interest in the authorship and publication of this contribution.
Ethical approval for this study was obtained from the Institutional Review Board/Ethical Review Committee of Funabashi Orthopaedic Hospital.
References
- 1. Baker CL, III, Romeo AA, Baker CL., Jr Osteochondritis dissecans of the capitellum. Am J Sports Med. 2010;38:1917–1928. [DOI] [PubMed] [Google Scholar]
- 2. Ben Kibler W, Sciascia A. Kinetic chain contributions to elbow function and dysfunction in sports. Clin Sports Med. 2004;23:545–552. [DOI] [PubMed] [Google Scholar]
- 3. Bojanić I, Ivković A, Borić I. Arthroscopy and microfracture technique in the treatment of osteochondritis dissecans of the humeral capitellum: report of three adolescent gymnasts. Knee Surg Sports Traumatol Arthrosc. 2006;14:491–496. [DOI] [PubMed] [Google Scholar]
- 4. Chan D, Aldridge MJ, Maffulli N, Davies AM. Chronic stress injuries of the elbow in young gymnasts. Br J Radiol. 1991;64:1113–1118. [DOI] [PubMed] [Google Scholar]
- 5. Gardiner TB. Osteochondritis dissecans in three members of one family. J Bone Joint Surg Br. 1955;37-B:139–141. [DOI] [PubMed] [Google Scholar]
- 6. Jackson DW, Silvino N, Reiman P. Osteochondritis in the female gymnast’s elbow. Arthroscopy. 1989;5:129–136. [DOI] [PubMed] [Google Scholar]
- 7. Jobe FW, Nuber G. Throwing injuries of the elbow. Clin Sports Med. 1986;5:621–636. [PubMed] [Google Scholar]
- 8. Kenniston JA, Beredjiklian PK, Bozentka DJ. Osteochondritis dissecans of the capitellum in fraternal twins: case report. J Hand Surg Am. 2008;33:1380–1383. [DOI] [PubMed] [Google Scholar]
- 9. Klingele KE, Kocher MS. Little League elbow: valgus overload injury in the paediatric athlete. Sports Med. 2002;32:1005–1015. [DOI] [PubMed] [Google Scholar]
- 10. Kobayashi K, Burton KJ, Rodner C, Smith B, Caputo AE. Lateral compression injuries in the pediatric elbow: Panner’s disease and osteochondritis dissecans of the capitellum. J Am Acad Orthop Surg. 2004;12:246–254. [DOI] [PubMed] [Google Scholar]
- 11. Momma D, Iwasaki N, Oizumi N, et al. Long-term stress distribution patterns across the elbow joint in baseball players assessed by computed tomography osteoabsorptiometry. Am J Sports Med. 2011;39:336–341. [DOI] [PubMed] [Google Scholar]
- 12. Morrey BF, An KN, Stormont TJ. Force transmission through the radial head. J Bone Joint Surg Am. 1988;70:250–256. [PubMed] [Google Scholar]
- 13. Ruchelsman DE, Hall MP, Youm T. Osteochondritis dissecans of the capitellum: current concepts. J Am Acad Orthop Surg. 2010;18:557–567. [DOI] [PubMed] [Google Scholar]
- 14. Seroyer ST, Nho SJ, Bach BR, Bush-Joseph CA, Nicholson GP, Romeo AA. The kinetic chain in overhand pitching: its potential role for performance enhancement and injury prevention. Sports Health. 2010;2:135–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Takahara M, Ogino T, Tsuchida H, Takagi M, Kashiwa H, Nambu T. Sonographic assessment of osteochondritis dissecans of the humeral capitellum. AJR Am J Roentgenol. 2000;174:411–415. [DOI] [PubMed] [Google Scholar]
- 16. Takahara M, Shundo M, Kondo M, Suzuki K, Nambu T, Ogino T. Early detection of osteochondritis dissecans of the capitellum in young baseball players. Report of three cases. J Bone Joint Surg Am. 1998;80:892–897. [DOI] [PubMed] [Google Scholar]