Abstract
Background:
High-grade partial proximal hamstring tears and complete tears with retraction less than 2 cm are a subset of proximal hamstring injuries where, historically, treatment has been nonoperative. It is unknown how nonoperative treatment compares with operative treatment.
Hypothesis:
The clinical and functional outcomes of nonoperative and operative treatment of partial/complete proximal hamstring tears were compared. We hypothesize that operative treatment of these tears leads to better clinical and functional results.
Study Design:
Case series; Level of evidence, 4.
Methods:
A retrospective review identified patients with a high-grade partial or complete proximal hamstring rupture with retraction less than 2 cm treated either operatively or nonoperatively from 2007 to 2015. All patients had an initial period of nonoperative treatment. Surgery was offered if patients had continued pain and/or limited function refractory to nonoperative treatment with physical therapy. Outcome measures were each patient’s strength perception, ability to return to activity, Lower Extremity Functional Scale (LEFS) score, Short Form–12 (SF-12) physical and mental component outcome scores, distance traversed by a single-leg hop, and Biodex hamstring strength testing.
Results:
A total of 25 patients were enrolled in the study. The 15 patients who were treated nonoperatively sustained injuries at a mean age of 55.73 ± 14.83 years and were evaluated 35.47 ± 30.35 months after injury. The 10 patients who elected to have surgery sustained injuries at 50.40 ± 6.31 years of age (P = .23) and were evaluated 30.11 ± 19.43 months after surgery. LEFS scores were significantly greater for the operative group compared with the nonoperative group (77/80 vs 64.3/80; P = .01). SF-12 physical component scores for the operative group were also significantly greater (P = .03). Objectively, operative and nonoperative treatment modalities showed no significant difference in terms of single-leg hop distance compared with each patient’s noninjured leg (P = .26) and torque deficit at isokinetic speeds of 60 and 180 deg/s (P = .46 and .70, respectively).
Conclusion:
Patients who undergo operative and nonoperative treatment of high-grade partial and/or complete proximal hamstring tears with <2 cm retraction demonstrate good clinical and functional outcomes. In our series, 40% of patients treated nonoperatively with physical therapy went on to have surgery. For those patients with persistent pain and/or loss of function despite conservative treatment, surgical repair is a viable treatment option that is met with good results.
Keywords: proximal hamstring tears, hamstring surgical repair, high-grade partial hamstring tears, hamstring surgical outcomes
Proximal hamstring injuries are relatively uncommon.13 Multiple pathologies have been identified, from proximal tendinopathy to complete multitendon tears. Many different management strategies exist and range from nonoperative treatment to surgical repair.7
The proximal hamstring complex involves 3 separate tendons that insert on the ischial tuberosity. These 3 tendons include the long head of the biceps femoris, the semitendinosis, and the semimembranosus muscles. The complex originates on a facet that is approximately 4 cm proximolateral to the tip of the ischial tuberosity and covers an area of approximately 10 cm2.11 The semimembranosus is the most lateral of the 3 tendons, and it is not uncommon to have a separate footprint for the biceps/semitendinosus (conjoined tendon) and semimembranosus tendons.9 This becomes particularly important for intraoperative identification of the defect in the conjoined tendon.
High-grade partial tears and complete tears with retraction less than 2 cm are a subset of proximal hamstring injuries where, historically, there has not been significant focus in the literature. For this specific type of injury, anywhere from 1 to 3 tendons are torn. It is common to have tearing of the conjoined tendon complex without significant retraction, likely because of the intact or partially intact semimembranosus attachment.6 Oftentimes, in a “hidden lesion” tear, injury to the conjoined tendon is not evident because of the intact semimembranosus tendon. In such cases, incision of the semimembranosus is required to visualize the defect of the conjoined tendon.4
Nonoperative treatment has commonly been the recommendation for patients who have had high-grade partial tears with minimal retraction.5 More recent literature has demonstrated that surgical treatment of partial proximal hamstring avulsions can lead to satisfactory functional outcomes and a high rate of return to athletic activity with a low complication rate.4 To our knowledge, there has yet to be a study comparing surgical and nonsurgical outcomes for patients with high-grade partial tears with minimal retraction of the proximal hamstrings.
The purpose of this study was to identify those patients who sustained a high-grade partial and/or complete tear with minimal (<2 cm) retraction retrospectively. Subjective evaluation, functional outcomes, and strength testing for these patients were assessed to determine the effects of conservative treatment compared with surgical intervention.
Methods
Patients who received surgical and nonsurgical treatment for proximal hamstring tears were retrospectively identified. Subjective and objective data were subsequently collected. Each patient was contacted by telephone and gave his or her consent to participate in the study.
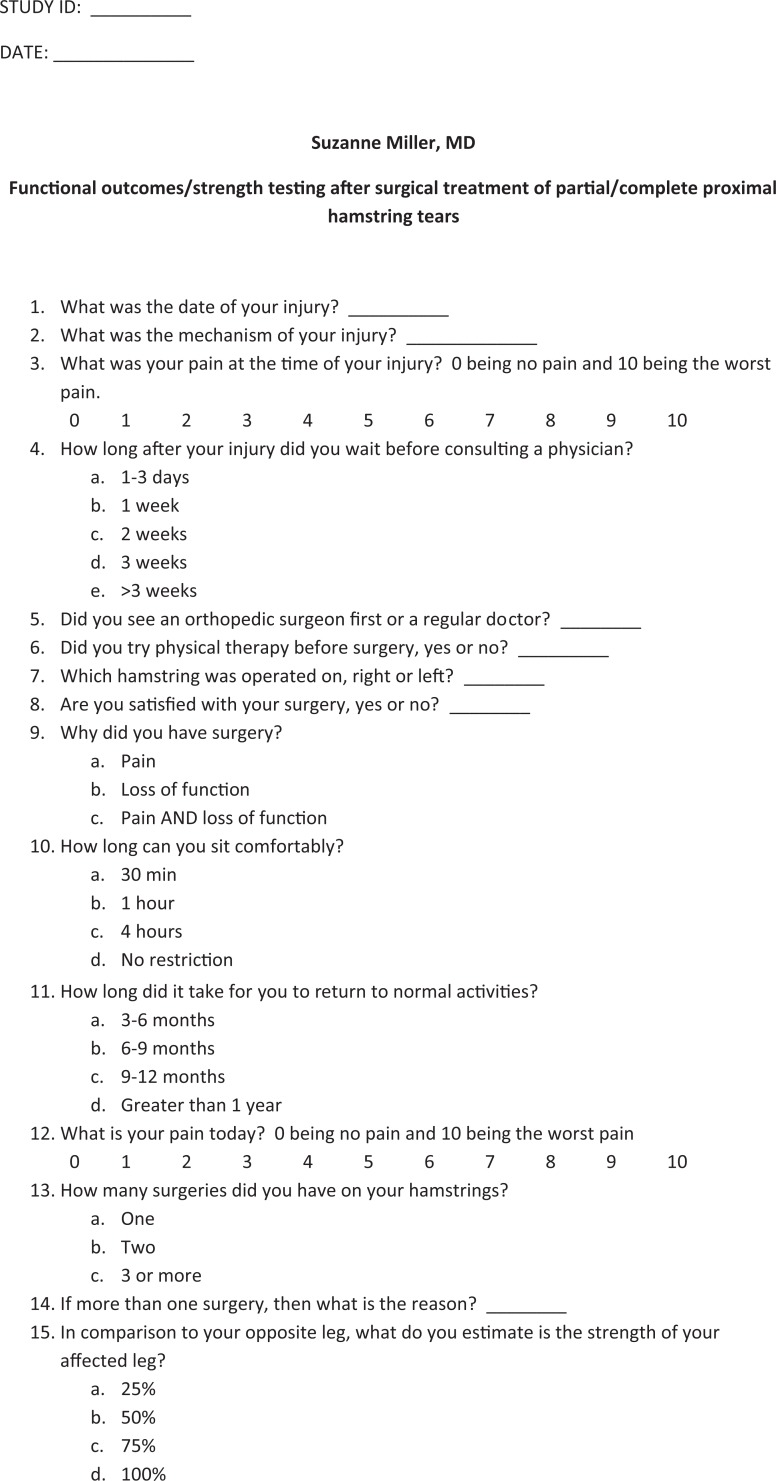
Clinical records were reviewed from 2007 through 2015. Inclusion criteria were patients who presented with high-grade partial- or full-thickness nonretracted (<2 cm) proximal hamstring tears. All diagnoses were confirmed with magnetic resonance imaging (MRI) (Figure 1). Exclusion criteria consisted of those patients with retracted tears greater than 2 cm, who were younger than 18 years of age, or who had bony avulsions.
Figure 1.
T2-weighted coronal hip magnetic resonance image (MRI) demonstrating a high-grade partial tear of the conjoined tendon (blue arrowhead) with the semimembranosus still attached (blue arrow).
Nonoperative treatment was the initial treatment for all patients, which included a combination of activity modification, physical therapy, and nonsteroidal anti-inflammatory drugs (NSAIDs), and was individualized based on patient comfort and preference of therapeutic modality. Patients gradually returned to activities as symptoms allowed. If patients had continued pain beyond 3 months of conservative treatment and/or limited function refractory to nonoperative treatment, surgery was offered.
The senior author (S.L.M.) performed all surgeries. The surgical procedure was performed through a transverse incision along the gluteal crease. Subcutaneous dissection was carried down to the gluteal fascia. The gluteal fascia was incised horizontally. The gluteus maximus was retracted proximally, and the hamstring tendon was identified. For high-grade partial tears, these lesions were typically not visible initially. The defect was located on the undersurface; therefore, the tendon appears intact when viewed posteriorly. For partial tears, a longitudinal incision was made in the intact tendon where the tendon felt thin. The bare ischial tuberosity could then be palpated. The sciatic nerve, which lies 1.2 cm lateral to the ischial tuberosity, was identified and protected.10 The ischium was prepared by creating a bleeding surface through removal of all soft tissue using an elevator and curettes. The proximal hamstring tear was identified. Chronic, attenuated tissue was debrided if present. One to 3 suture anchors (Q-FIX; Smith & Nephew) were placed in the tuberosity. The sutures were passed in a horizontal mattress configuration, and the hamstring was reapproximated to its anatomic origin. The gluteal fascia was closed. The skin was closed using monocryl sutures and Dermabond (Ethicon) adhesive. An Aquacel (ConvaTec) dressing was placed. Postoperatively, patients were locked in hip extension in an extension brace with partial weightbearing and allowed hip flexion at 4 weeks postoperatively. Physical therapy began at 4 weeks, and patients were allowed to bear full weight at 6 weeks postoperatively, being careful to avoid end range of motion stretch. At 8 weeks, patients were allowed to begin hamstring-strengthening exercises. Patients could begin a return to activities at 12 to 16 weeks.
Patients were contacted to obtain subjective outcome data as well as objective functional outcome scores. Thirty-six patients met the inclusion criteria. Of these, 25 were able to be contacted by telephone and willing to participate in the study. Patients either completed the questionnaires over the phone or in person if they underwent functional testing. All 25 patients completed the questionnaires, and 21 completed functional testing. Four could not complete functional testing because of time constraints, no longer living in the area, or had a different significant medical condition that prevented participation.
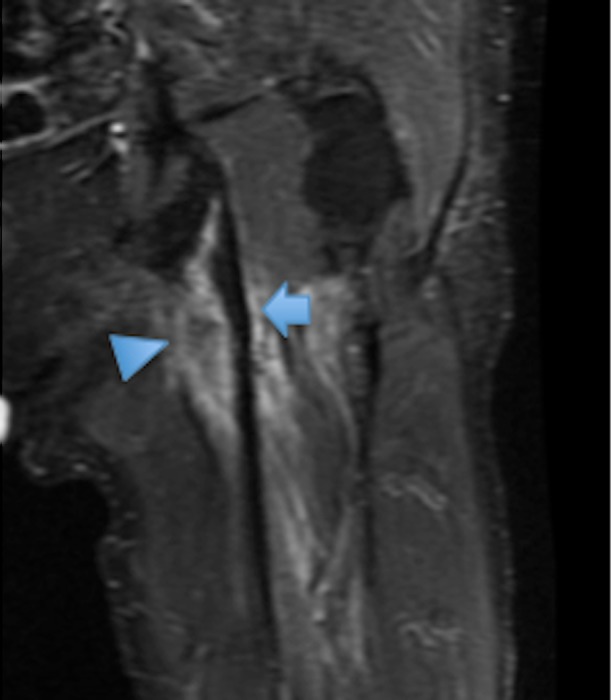
Three questionnaires were completed by each patient. The first was a nonvalidated questionnaire created by the senior author (S.L.M.) regarding the details of the patient’s injury, treatment plan, and subjective evaluation of his or her recovery (see the Appendix). The second questionnaire was the Lower Extremity Functional Scale (LEFS), a reliable and validated outcome scale evaluating one’s functional level.3 The third questionnaire was the Short Form–12 (SF-12).14
A single certified physical therapist/athletic trainer conducted functional testing. Testing included a single-leg hop test for distance comparing the injured to the uninjured leg. The hop was measured from a starting line to the maximum distance hopped. Each leg was measured 3 times and an average distance hopped was calculated. Nineteen of 21 patients were able to complete this task, while 2 refused to participate because of apprehension and persistent pain.
A Biodex System 3 machine (Biodex Medical Systems) was used to obtain peak hamstring strength measurements (Figure 2). Isokinetic testing at speeds of 60 and 180 deg/s were obtained. These values were compared with the noninjured leg to obtain a strength deficit comparison.
Figure 2.

Biodex System 3 machine (Biodex Medical Systems).
Patient data were collected and organized in a spreadsheet. Data were analyzed using the Shapiro-Wilk test to determine whether each outcome measure was normally distributed. Functional outcome and strength testing results for normally distributed data were assessed using a 2-sample t test. An exact Wilcoxon 2-sample test was utilized to assess nonnormally distributed data. Responses to the nonvalidated questionnaire were assessed for significance utilizing chi-square testing.
Results
Fifteen of the 25 patients who were treated had acceptable outcomes with nonoperative treatment. Table 1 lists patient demographics, including age at injury and the mean time from injury or surgery to survey completion. Table 2 lists the mechanism of injury.
TABLE 1.
Nonoperative and Operative Group Demographics
| Nonoperative | Operative | P Value | |
|---|---|---|---|
| Total patients | 15 | 10 | |
| Sex | .68 | ||
| Male | 7 | 3 | |
| Female | 8 | 7 | |
| Age at time of injury, y, mean ± SD | 55.73 ± 14.83 | 50.4 ± 6.31 | .23 |
| Mean time from injury/surgery to evaluation, mo, mean ± SD | 35.47 ± 30.35 | 30.11 ± 19.43 | .45 |
TABLE 2.
Mechanism of Injury for Operative and Nonoperative Patients
| Operative Patients | Nonoperative Patients | |
|---|---|---|
| Cartwheel | 1 | |
| Handstand | 1 | |
| Nontraumatic | 1 | |
| Running | 2 | 3 |
| Trampoline | 1 | |
| Unknown | 2 | 3 |
| Waterskiing | 2 | 3 |
| Bowling | 1 | |
| Mountain biking | 1 | |
| Skiing | 1 | |
| Soccer | 1 | |
| Tripped | 1 | |
| Yoga | 1 |
LEFS scores were collected and compared to a maximum score of 80. Scores of 64.3 and 77 (exact Wilcoxon 2-sample test, P = .01) were obtained from the nonoperative and operative treatment groups, respectively. The specific difficulties that operative and nonoperative patients had were variable. Walking, taking stairs, and standing, however, appeared to give nonoperative patients more difficulty than operative patients, as none of the operative patients described moderate difficulty or worse with these activities. The mean SF-12 physical component summary (PCS) score was 48 (range, 29-58) for the nonoperative group compared with 55 (range, 50-59) for the operative group (exact Wilcoxon 2-sample test, P = .03). The mean SF-12 mental component summary (MCS) score was 55 for both groups (exact Wilcoxon 2-sample test, P = .46) (Table 3).
TABLE 3.
Subjective Outcome Scores for Nonoperative and Operative Treatment Groupsa
| Nonoperative | Operative | P Value | |
|---|---|---|---|
| Lower Extremity Functional Scale score | 64.3 | 77 | .01 |
| SF-12 PCS | 48 | 55 | .03 |
| SF-12 MCS | 55 | 55 | .46 |
aMCS, mental component score; PCS, physical component score; SF-12, Short Form–12.
Isokinetic testing was performed to gauge hamstring strength. The torque deficit was calculated at 2 different speeds for the injured extremity compared with the noninjured limb. The torque deficit between the injured and noninjured limb was 4.2% for the nonoperative group and −1.7% for the operative group at an isokinetic speed of 60 deg/s (2-sample t test, P = .46) (Table 4). The torque deficit between the injured and noninjured limb was 5.6% for the nonoperative group and 8.5% for the operative group at an isokinetic speed of 180 deg/s (2-sample t test, P = .70).
TABLE 4.
Absolute Values for Isokinetic Torque at 60 and 180 deg/s for Operative and Nonoperative Patientsa
| Nonoperative Healthy Leg | Operative Healthy Leg | P Value | Nonoperative Injured Leg | Operative Injured Leg | P Value | |
|---|---|---|---|---|---|---|
| Torque at 60 deg/s, ft-lbs | 45.7 ± 16.9 | 60.6 ± 20.6 | .08 | 43.6 ± 17.1 | 62.9 ± 26.4 | .06 |
| Torque at 180 deg/s, ft-lbs | 36.5 ± 10.5 | 48.9 ± 15.6 | .04 | 34.7 ± 12.0 | 45.0 ± 19.0 | .15 |
aValues are expressed as mean ± SD.
Patients treated nonoperatively were able to hop 108 cm on the noninjured leg and 111 cm on the injured leg. Patients who underwent surgery were able to hop 130 cm on the noninjured leg compared with 128 cm on the injured leg. The nonoperative treatment group had a hop distance improvement of 2.7% compared with the noninjured leg. The operative group had a decrease of 1.5% in hop distance compared with the noninjured leg (2-sample t test, P = .26).
From the data acquired in the nonvalidated questionnaire employed in this study, it was found that the most common mechanism of injury was either waterskiing or running (5 patients each) followed by various sports or low energy trauma. Only 6 of the 25 (24%) who were injured did so via an unknown or atraumatic mechanism. Evaluation of the 2 groups found no significant difference in either group’s subjective rating of current pain levels (chi-square test, P = .18), current strength estimate (chi-square test, P = .16), ability to sit for prolonged periods of time (chi-square test, P = .35), or ability to participate in strenuous activities (chi-square test, P = .13). Recovery from the hamstring injury adversely affected the nonoperative group more with regard to participation in recreational activities (chi-square test, P = .05) and interfering with daily activities (chi-square test, P = .02) as compared with the operative group. A majority in both treatment groups had minimal pain and subjectively reported >75% strength return as compared with the noninjured leg (P = .12).
There were minimal complications in each treatment arm. Of the surgical patients, only 1 complained of transient numbness and tingling, while 3 nonoperative patients had numbness and tingling (P = .61). Eight of 10 surgical patients were able to sit for 4 or more hours, while 10 of 15 nonoperative patients could sit for 4 or more hours (P = .35).
Discussion
These data suggest that patients who sustain high-grade partial proximal hamstring tears with <2 cm of retraction do well with nonoperative and operative treatment. The objective findings did not indicate that one method was superior to the other. The torque deficit between the injured and noninjured leg for the nonoperative compared with the operative group was equivocal at 2 different isokinetic speeds. There was no significant difference in distance traversed by a single-leg hop when comparing the injured to noninjured leg for the 2 groups either. After a mean 30 to 35 months of follow-up, these findings suggest that strength can be recovered in the injured limb given enough time and proper rehabilitation with or without surgical repair.
Subjective outcome scores were higher for the operative group, as demonstrated by the statistically significant higher LEFS and SF-12 PCS scores. The improved subjective outcomes compared with objective outcomes indicate that patients may overestimate or underestimate their recovery based on the treatment they received, or it is possible that the objective measures tested do not truly simulate real motion with normal activities such as running. It is also quite possible that the added supervision with postoperative rehab caused the statistically significant difference in subjective outcomes. Since our cohort of patients who opted for surgical management had failed a course of nonoperative therapy, it is possible that having undergone surgery provided greater benefit. Further randomized controlled trials will be needed to fully evaluate the benefit of operative management.
Nonoperative management of proximal hamstring avulsions have been met with modest ability to return to preinjury level of sporting activity. Sallay et al12 reported that 7 of 12 patients with proximal hamstring avulsions (58%) sustained after waterskiing injuries treated nonoperatively were able to return to most sports played preinjury at a lower level, while the remaining were unable to run or perform sports requiring agility. Our nonoperative outcomes results were similar, with 15 of 25 patients (60%) responding to nonoperative treatment.
Our surgical outcomes are comparable to the few published studies in the literature that focus on surgical outcomes of partial hamstring tears. Bowman et al4 demonstrated a postoperative LEFS score of 73.3 out of 80 in a study of 17 patients who underwent surgical repair for partial-thickness tears after failing physical therapy. All patients estimated their strength recovery at 75% or greater. Aldridge et al1 followed 23 patients for 2 years after surgical repair. Visual analog pain scale scores and hamstring strength improved.1 Lempainen et al8 followed 47 patients for a mean 36 months after surgery for partial-thickness tears. Outcomes were determined to be good or excellent in 88% of the patients, and 41 of 47 patients were able to return to their preinjury level of sporting activity.8 Barnett et al2 followed 132 patients with complete and partial tears treated surgically for a mean 53.8 months. One hundred twelve of the 132 patients had good or excellent results.2
To our knowledge, this is among the first studies to compare surgical and nonoperative means to hamstring repair for avulsions less than 2 cm. It combines subjective (LEFS, SF-12, etc) with objective (Biodex, single-leg hop test) outcome measures.
There are several limitations to this study. First, this was a retrospective series, and there were no baseline data for comparison. Second, there was no standardized nonoperative treatment protocol for each patient. Patients had variable durations and quality of physical therapy, activity modification, and different NSAID usage. In addition, a variable nonoperative treatment time period existed for patients prior to undergoing surgical repair. Nonoperative patients tended to have lower peak torques in the healthy and affected leg compared with operative patients. While only the difference between torque in the healthy leg at a speed of 180 deg/s was statistically significant, it is possible that the patients who decided on surgical management were more physically fit than those managed nonoperatively.
Our sample size was adequate for this particular injury, and our patient response was good but not great. This was due largely to the fact of being unable to contact the potential study candidates. Of the 3 questionnaires, the subjective questionnaire created by the senior author has not been validated. It was created to gather responses not reported in the LEFS or SF-12 questionnaires.
In summary, patients who sustain high-grade partial proximal hamstring tears with <2 cm of retraction can recover well with either nonoperative and operative treatment; 40% of our study participants went on to have surgical repair and did well. Patients with this injury can expect that after failing a trial of nonoperative treatment, surgical repair remains a viable treatment option with good results. Regardless of treatment method, it can take several months or longer to recover from this injury. Long-term follow-up of 2.5 to 3 years suggests that a majority of patients recover more than 75% hamstring strength, have minimal pain, and the injury has little effect with regard to interfering with daily activities. While the objective findings do not demonstrate a difference between the 2 treatment strategies, subjective results are better for the surgical repair group when compared with the nonoperative group.
Appendix
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: S.L.M. has partial ownership of Parcus Medical.
Ethical approval for this study was obtained from New England Baptist Hospital (IRB #559155).
References
- 1. Aldridge SE, Heilpern GN, Carmichael JR, Sprowson AP, Wood DG. Incomplete avulsion of the proximal insertion of the hamstring: outcome two years following surgical repair. J Bone Joint Surg Br. 2012;94:660–662. [DOI] [PubMed] [Google Scholar]
- 2. Barnett AJ, Negus JJ, Barton T, Wood DG. Reattachment of the proximal hamstring origin: outcome in patients with partial and complete tears. Knee Surg Sports Traumatol Arthrosc. 2015;23:2130–2135. [DOI] [PubMed] [Google Scholar]
- 3. Binkley JM, Stratford PW, Lott SA, Riddle DL. The Lower Extremity Functional Scale (LEFS): scale development, measurement properties, and clinical application. North American Orthopaedic Rehabilitation Research Network. Phys Ther. 1999;79:371–383. [PubMed] [Google Scholar]
- 4. Bowman KF, Jr, Cohen SB, Bradley JP. Operative management of partial-thickness tears of the proximal hamstring muscle in athletes. Am J Sports Med. 2013;41:1363–1371. [DOI] [PubMed] [Google Scholar]
- 5. Cohen S, Bradley J. Acute proximal hamstring rupture. J Am Acad Orthop Surg. 2007;15:350–355. [DOI] [PubMed] [Google Scholar]
- 6. De Smet AA, Best TM. MR imaging of the distribution and location of acute hamstring injuries in athletes. AJR Am J Roentgenol. 2000;174:393–399. [DOI] [PubMed] [Google Scholar]
- 7. Harris JD, Griesser MJ, Best TM, Ellis TJ. Treatment of proximal hamstring ruptures—a systematic review. Int J Sports Med. 2011;32:490–495. [DOI] [PubMed] [Google Scholar]
- 8. Lempainen L, Sarimo J, Heikkilä J, Mattila K, Orava S. Surgical treatment of partial tears of the proximal origin of the hamstring muscles. Br J Sports Med. 2006;40:688–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Miller SL, Gill J, Webb GR. The proximal origin of the hamstrings and surrounding anatomy encountered during repair. A cadaveric study. J Bone Joint Surg Am. 2007;89:44–48. [DOI] [PubMed] [Google Scholar]
- 10. Miller SL, Webb GR. The proximal origin of the hamstrings and surrounding anatomy during repair. Surgical technique. J Bone Joint Surg Am. 2008;90(suppl 2, pt 1):108–116. [DOI] [PubMed] [Google Scholar]
- 11. Neuschwander TB, Benke MT, Gerhardt MB. Anatomic description of the origin of the proximal hamstring. Arthroscopy. 2015;31:1518–1521. [DOI] [PubMed] [Google Scholar]
- 12. Sallay PI, Friedman RL, Coogan PG, Garrett WE. Hamstring muscle injuries among water skiers. Functional outcome and prevention. Am J Sports Med. 1996;24:130–136. [DOI] [PubMed] [Google Scholar]
- 13. Sherry MA, Johnston TS, Heiderscheit BC. Rehabilitation of acute hamstring strain injuries. Clin Sports Med. 2015;34:263–284. [DOI] [PubMed] [Google Scholar]
- 14. Ware J, Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. [DOI] [PubMed] [Google Scholar]