Abstract
Alcoholic liver disease (ALD) is a leading cause of cirrhosis, liver cancer, and acute and chronic liver failure and as such causes significant morbidity and mortality. While alcohol consumption is slightly decreasing in several European countries, it is rising in others and remains high in many countries around the world. The pathophysiology of ALD is still incompletely understood but relates largely to the direct toxic effects of alcohol and its main intermediate, acetaldehyde. Recently, novel putative mechanisms have been identified in systematic scans covering the entire human genome and raise new hypotheses on previously unknown pathways. The latter also identify host genetic risk factors for significant liver injury, which may help design prognostic risk scores. The diagnosis of ALD is relatively easy with a panel of well-evaluated tests and only rarely requires a liver biopsy. Treatment of ALD is difficult and grounded in abstinence as the pivotal therapeutic goal; once cirrhosis is established, treatment largely resembles that of other etiologies of advanced liver damage. Liver transplantation is a sound option for carefully selected patients with cirrhosis and alcoholic hepatitis because relapse rates are low and prognosis is comparable to other etiologies. Still, many countries are restrictive in allocating donor livers for ALD patients. Overall, few therapeutic options exist for severe ALD. However, there is good evidence of benefit for only corticosteroids in severe alcoholic hepatitis, while most other efforts are of limited efficacy. Considering the immense burden of ALD worldwide, efforts of medical professionals and industry partners to develop targeted therapies in ALF has been disappointingly low.
Keywords: Hepatitis, alcoholic; Corticosteroid therapy; Carcinoma, hepatocellular; Liver transplantation; Malnutrition; PNPLA3
INTRODUCTION
Alcohol consumption accounts for approximately 3.8% of all global deaths and 4.6% of global disability-adjusted life-years.1 In Europe, this problem seems to be particularly relevant, with 6.5% of all deaths attributable to alcohol,2 and recent estimates indicate that harmful drinking, particularly when associated with alcohol dependence, is responsible for one in seven deaths in men and one in 13 deaths in women aged 15 to 64 years.3 Alcohol use disorders (AUD) are the most frequent cause of liver cirrhosis in Europe, and alcoholic liver disease (ALD) the most important cause of death due to alcohol in adults.4 Liver cirrhosis mortality over the past 30 years declined in most Western European countries, while it increased in several Eastern European countries, as well as in the United Kingdom, Ireland, and Finland.5 Of note, the all-cause mortality of middle-aged white non-Hispanic men and women in the United States between 1999 and 2013 increased significantly, largely to increasing death rates from drug and alcohol poisonings, chronic liver diseases and cirrhosis.6 A strong determinant for alcohol-related organ damage in many–but not all–patients is the alcohol dependence syndrome, a common behavioral disorder characterized by tolerance to the psychotropic effects of alcohol consumption, a preoccupation with alcohol and persistent drinking despite its harmful consequences. Chronic and episodes of binge alcohol abuse also contribute to the development of various somatic and psychiatric disorders and injuries, as well as to several diseases which are predominantly or entirely attributable to alcohol, such as alcohol-induced pancreatitis7 and the fetal alcohol syndrome.8 Furthermore, alcohol is also a contributory factor to other, diseases and injuries. Among the most important disease conditions affected by alcohol consumption are cancers of the oropharynx, esophagus, liver, colon, rectum and the female breast;9 cardiovascular diseases;10 neuropsychiatric disorders (epilepsy, depressive disorders);11 a (not necessarily complete) summary of physical and mental diseases related to alcohol consumption is given in Table 1.
Table 1.
Alcohol-Associated Somatic and Mental Diseases
| Acute intoxication (apnea, aspiration of gastric content) Alcohol use disorders Gastrointestinal tract, pancreas and liver
Cardiovascular disease
Alcoholic osteopathy Neurological and psychiatric disorders
Infections
|
EPIDEMIOLOGY AND BURDEN OF DISEASE
AUD contributes to a large proportion of deaths from liver diseases, either by causing genuine ALD or as a cofactor in patients with non-ALDs such as chronic viral hepatitis, hemochromatosis and fatty liver due to nonalcoholic causes. The Global Burden of Disease Study reported a steadily increasing mortality due to liver diseases with approximately 1 million deaths in 2010, which is roughly 2% of the global total mortality.12 With this, liver-related years of liver lost (YYL) outscore that of YYL due to cancers of the respiratory tract, esophagus, stomach, colorectum and pancreas together.13 To what proportion alcohol consumption contributes to this burden, is not entirely clear since the underlying etiologies of liver disease are not gaplessly recorded in most countries, with great variation across Europe. The most precise figures can be obtained from Finland where 87% of death cases due to liver disease seem to be alcohol-related. Taking into account the variability across Europe and figures extracted from the World Health Organization (WHO) mortality database,14 one can estimate for the European Union that 60% to 80% of liver-related mortality is due to excessive drinking.15 According to WHO, morbidity attributable to alcohol in developed countries accounts for 10.3% of disability adjusted life years and comes second only to that of tobacco (11.7%). Within this figure, liver cirrhosis is responsible for 70% to 80% of the directly recorded mortality from alcohol. In 2010, alcoholic liver cirrhosis was responsible for 493,300 deaths (47.9% of all liver cirrhosis deaths), representing 0.9% of all deaths regardless the cause (0.7% of all deaths of women and 1.2% of all deaths of men), and 80,600 deaths (14,800 deaths of women and 65,900 deaths of men) were attributable to alcohol-related liver cancer.4 Apart from mere mortality figures, harmful alcohol consumption is the second most common indication for liver transplantation, accounting for approximately 40% of all primary liver transplants in Europe and about 25% in the United States.16 Besides its remarkable health impact, this huge disease burden has an economic impact of about 125 billion Euros annually in Europe, accounting for 1.3% of the gross domestic product.17
SPECTRUM AND PATHOPHYSIOLOGY OF ALD
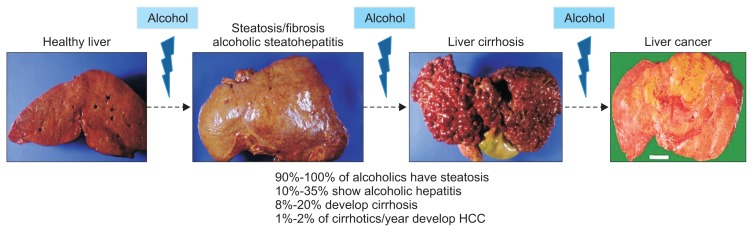
Above a certain quantity, alcoholic consumption can elicit a spectrum of liver lesions among which steatosis is present in nearly all drinkers who consume in excess of 40 g/day regularly. Beyond fatty liver, ALD comprises a continuum of partly overlapping liver abnormalities with variable degrees of inflammation and progressive fibrosis in 10% to 35% of alcoholics, and liver cirrhosis in approximately 10% to 15% of heavy drinkers (Fig. 1).18 A great concern is the rising incidence of hepatocellular carcinoma (HCC) which evolves in approximately 1% to 2% of alcoholic cirrhotics per year.19 While steatosis and inflammation are reversible upon abstinence, and probably also fibrosis below the level of cirrhotic transformation, severe alcoholic steatohepatitis (ASH), decompensating cirrhosis and HCC have a grave prognosis.
Fig. 1.
The progression for alcoholic liver injury to steatosis with scarring, inflammation and architectural distortion leading to cirrhosis. As a complication of cirrhosis, hepatocellular carcinoma may occur. However, only a minority of patients with alcoholic steatosis progress to severe liver injury.
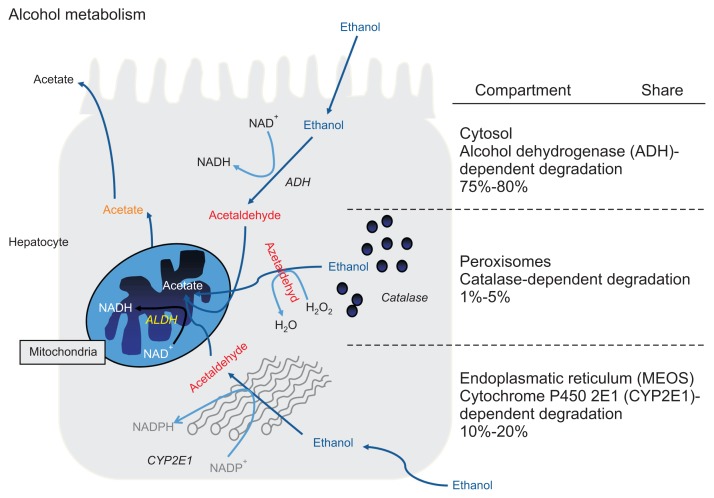
The cellular and molecular mechanisms of ALD pathogenesis are still incompletely understood but seem to be related to a complex interaction between behavioral, environmental and genetic factors. The histological hallmarks of ALD, steatosis, inflammation and fibrosis are the result of interrelated and consecutive pathophysiological events in the context of continuous alcohol exposure. A pivotal component in the evolution of ALD is the direct toxicity of the first metabolite of alcohol degradation, acetaldehyde (AA).20 Two major enzyme systems can metabolize alcohol to AA via oxidative degradation, of which alcohol-dehydrogenase is the system primarily responsible for the processing of lower amounts of alcohol. It is located in the cytosol and cannot be upregulated upon demand. In contrast, cytochrome P450 2E1 (CYP2E1) located in microsomes is inducible and can be upregulated 10- to 20-fold in heavy drinkers.21 Both enzyme systems generate AA, a highly reactive toxic and mutagenic metabolite, by which they not only degrade ethanol (and other organic substances), but also contribute to alcohol-related toxicity (Fig. 2). Apart from generating AA, CYP2E1 also contributes of oxidative damage by the formation of reactive oxygen species (ROS) such as superoxide anion and hydrogen peroxide. Hepatic CYP2E1 activity in humans may already increase following the ingestion of only 40 g of ethanol/day for 1 week.22 In rodents, the induction of CYP2E1 correlated with NAD phosphate oxidase activity, the generation of hydroxyethyl radicals, lipid peroxidation and the severity of hepatic damage, all of which could be prevented by the CYP2E1 inhibitor clome-thiazole.23,24 Importantly, AA is also a powerful carcinogen in experimental animals and in humans, and considered an important reason for the association of certain cancers with alcohol consumption.25
Fig. 2.
Hepatic metabolism of ethanol by enzymes ADH, CYP2E1 and catalase. Each enzyme generates acetaldehyde, a toxic and mutagenic metabolite of ethanol. While ADH is metabolically stable regardless of the alcohol challenge and catalase is irrelevant with respect to its role in hepatic alcohol degradation, CYP2E1 is inducible and contributes most to acetaldehyde production during heavy alcohol consumption.
The initial liver lesion in alcoholics is steatosis which occurs in literally all heavy drinkers as a result of disrupted lipid turnover.26 Above all, decreased fatty acid oxidation, increased fatty acid and triglyceride synthesis, increased fat entry into the liver by fatty acid mobilisation from peripheral fat stores and via chylomicrons from the intestine are instrumental. Furthermore, increased lipogenesis by dysregulation of steatogenic enzymes and transcription factors including sterol regulatory-binding protein 1c, peroxisome proliferator-activated receptor α, and microsomal triglyceride transport protein are involved. A more recent revelation is the potential role of protein enzymes involved in lipid processing such as PNPLA3 and TM6SF2 for which genetic variants of the coding genes were found associated with ALD (see below). Whether and how alcohol consumption affects the function of these enzymes, however, is still unclear.
Similar to non-ASH, inflammation can occur as an important feature in alcoholic steatosis resulting in ASH, and evolve as a major driving force for fibrogenesis leading to fibrosis, cirrhosis and most likely, hepatocarcinogenesis. Histologically, ASH is characterized by variable degrees of steatosis, a typical inflammatory infiltrate consisting of predominantly polymorphonuclear (PMN) cells, centrilobular hepatocyte ballooning, Mallory-Denk inclusion bodies, and a “chicken wire”-like fibrosis network.27 A key pathogenic pathway in this stage is the gut-liver axis. Thus, alcohol ingestion increases gut permeability and promotes the translocation of endotoxins from Gram negative bacteria such as lipopolysaccharides (LPS) into the portal bloodstream to reach Kupffer cells which, upon binding of LPS to the endotoxin receptor CD14 activate the MyD88-independent signaling pathway through TLR4, with consecutive production of proinflammatory cytokines such as tumor necrosis factor α that contribute to hepatocellular damage.28–30 Additional cytokines and chemokines involved in the activation/recruitment of inflammatory and mesenchymal cells contributing to inflammation and fibrotic repair processes in ALD are interleukin (IL)-1, IL-8, and IL-17, osteopontin, chemokine (CXCL)1, CXCL4, CXCL5, and CXCL6.30–32 These proinflammatory sequelae are particular prominent in patients with ASH.
The key lesion in chronic liver disease is fibrosis that, in essence, resembles the process of excessive wound healing as a result of increased fibrogenesis and decreased fibrolysis. In progressive fibrosis, liver parenchyma is replaced by excess extra-cellular matrix produced by activated hepatic stellate cells (HSC) and myofibroblasts (MFB), resulting in a distorted liver architecture and progressive functional impairment.33 Various triggers can activate liver macrophages (Kupffer cells) and other inflammatory cells which leads to the production of the profibrogenic cytokines platelet-derived growth factor and transforming growth factor-β1 which can stimulate HSC/MFB to produce collagens, noncollagenous glycoproteins, proteoglycans, and glycosaminoglycans up to 10-fold compared to normal liver tissue. Here, the fibril forming collagens type I and III make up for >80% of total liver collagen. In turn, matrix-degrading enzymes termed matrix-metalloproteinases are downregulated by their corresponding tissue inhibitors.33 In ALD, HSCs/MFBs can be stimulated by AA,34 ROS,35 leptin,36 endocannabinoids37 and lipid peroxides.38
The most worrisome complication of ALD is HCC, and the vast majority of HCCs develops on the background of alcoholic cirrhosis.39 Besides cirrhotic transformation as a precancerous condition, a number of pathophysiological aspects are specific to alcohol-associated HCC. An important trigger of tumor development is AA, which is not only a toxin, but also a highly reactive mutagen that forms stable DNA adducts, causes point mutation, sister chromatid exchanges, inhibits DNA repair, and via induced CYP2E1, activates pro-carcinogens to carcinogens.9 Other molecular mechanisms include epigenetic modifications from alcohol by altering DNA methylation. Indeed, epigenetic silencing of hypermethylated tumor suppressor genes and activation of oncogenes via hypomethylation correlate with survival in human HCC including patients with alcoholic cirrhosis.40
Recent studies have shed some light on the pathogenesis of ASH. Here, failure of the liver to regenerate the hepatocellular mass seems to play a major role. Explants from ASH patients that underwent liver transplantation revealed that nonresponders to medical therapy had reduced hepatic expression of liver regeneration-related cytokines and the lack of proliferative hepatocytes.41 This observation was further confirmed by others, which showed that presence of proliferating hepatocytes in alcoholic hepatitis (AH) is associated with a better prognosis.42 In addition, a massive expansion of liver progenitor cells (LPCs) called “ductular reaction” is often observed in AH patients, but these LPCs fail to differentiate into mature hepatocytes and correlate positively with severity of liver disease and short-term mortality in these patients.43
Experimental ALD
Studying ALD experimentally has been extremely difficult since no animal model exists that closely mirrors all relevant features of severe ALD in humans or only pivotal elements of it.44 Rodents are notoriously resistant to the hepatotoxic effects of alcohol due to species-related differences in alcohol metabolism, and rats or mice only develop significant chronic liver injury when exposed to alcohol in combination with a second toxin (e.g., carbon tetrachloride and thioacetamide) or major dietary manipulations (e.g., choline/methionine deficiency) that still do not produce a histological picture that fully models that of human ALD.45 The experimental setup that produces liver lesions most similar to those in humans is the intragastric feeding model, or Tsukamoto-French model in which continuous infusion of alcohol-containing food via a surgically-implanted gastric tube results in typical alcohol-induced liver injury including steatohepatitis, fibrosis and microscopic lesions such as ballooning, Mallory-Denk bodies and neutrophilic inflammatory infiltration.46 The lack of a suitable animal model has been a significant impediment to more deeply study ALD experimentally, and is one of the reasons for the suboptimal research on novel biomarkers retrieved from human omics studies (vide infra). Recent advances, such as the National Institute on Alcohol Abuse and Alcoholism model of ALD, that combine binge drinking patterns with chronic alcohol exposure may pave the way for more suitable models.47 This can be promising when combined with novel technologies to design genetically modified rodents such as with the CRISPR/Cas9 technique to overcome species-related differences in alcohol susceptibility.48
FACTORS MODULATING PROGRESSION OF ALD
Significant ALD with progressive fibrosis and cirrhosis develops only in a minority of heavy drinkers suggesting that apart from alcohol itself, modifying variables exist that modulate the individual susceptibility to the toxic effects of alcohol. ALD is considered a complex disease in which numerous factors interact to allow for liver disease to occur. These factors are referred to as environmental (exogenous) or host (inherent) disease modifiers which partly explain the large inter-individual variability in the likelihood to develop ALD. Much progress has been made in our understanding of how these factors are entangled as outlined below.
1. Environmental factors
The development of ALD requires heavy alcohol drinking, and consensus exists that there is a clear dose-relationship between the amount of alcohol and the likelihood of its development.49,50 According to the Dionysos Study from Italy the risk of developing alcoholic cirrhosis is highest in those with a daily consumption of above 120 g of pure alcohol per day.51 Drinking patterns were suggested as modifier of ALD, such as drinking with meals appeared to confer less risk than consuming alcohol outside separately. Regarding the type of alcoholic beverage it was suggested that wine drinking is associated with a lower risk of ALD;52 however, scientific persuasion prevails that it is rather the amount of alcohol contained in certain alcoholic beverages than the nonalcoholic contents, and that the effect of different beverages on ALD risk are rather related to lifestyle and dietary factors.53 Coffee drinking appears to protect alcohol-related liver injury with people drinking four or more cups a day having one-fifth of the risk of developing cirrhosis as non-coffee drinkers.54 In turn, cigarette smoking increases the risk of alcoholic cirrhosis with smokers of ≥1 pack daily showing a 3-fold higher risk than nonsmokers.55
Coinfection with viral hepatitis B and C is also recognized as an important promoter of ALD, although the clear distinction between viral hepatitis worsened by alcohol, or vice versa, is often difficult to make and relies mainly on the predominant histology lesion prevalent in a patient with both conditions. The most abundant data exist for the interaction between alcohol and chronic hepatitis C for which numerous population-based, cross-sectional and cohort studies have demonstrated a higher prevalence of alcohol abuse among hepatitis C virus (HCV)-infected subjects, and a higher prevalence of HCV antibodies among drinkers.56 In a large study including 800 patients with chronic HCV infection, Monto et al.57 showed that those who drink alcohol in excess of 50 g/day have a significantly higher risk of advanced fibrosis than those who drink less or not at all. Mechanistically, published data suggest that alcohol accelerates the progression of hepatitis C-related liver disease via increased oxidative stress, cytotoxicity, immune dysfunction and reduction of response to antiviral treatment. Similar mechanisms are believed to be in place regarding hepatitis B virus-infected subjects, although the data regarding the latter is less abundant.58
Overweight has been consistently associated with an increased risk of developing alcohol-related fibrosis and cirrhosis potentially reflecting a synergistic interaction between alcohol and lipotoxicity from steatosis as a consequence of obesity.59–61
2. Host genetic factors
Several observations indicate an at least partial genetic background of ALD and its progression. Persuasive evidence for a genetic background of ALD stems from a twin study undertaken in a population of 15,924 male twin pairs in which the concordance for alcohol-related cirrhosis was found three times higher in monozygotic twins than in dizygotic twins.62 Another strong genetic modifier is gender: women carry a greater risk of developing alcohol-related cirrhosis, likely attributable to hormonal effects on oxidative stress and inflammation,63 differences in expression patterns of alcohol-metabolizing enzymes,64 and a smaller distribution volume of alcohol in women and, thus, higher tissue levels of alcohol exposure.65
In the United State white Hispanic men and women reveal a higher risk for alcoholic cirrhosis compared with black and Caucasian white men and women,66 and present with alcohol-related cirrhosis up to 10 years earlier than their Caucasian counterparts.67 However, besides constitutional differences in alcohol metabolism these differences could very well be related to cultural differences, amounts and types of alcohol consumed, dietary intake, socioeconomic status, and access to health care.
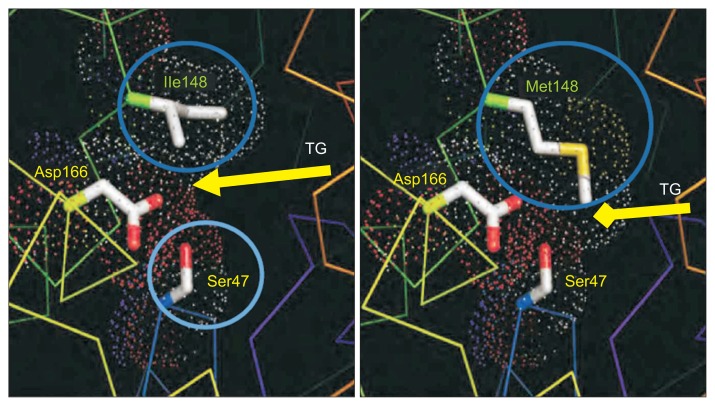
After an avalanche of relatively small candidate gene studies investigating hypothesis-based single nucleotide polymorphisms within genes considered relevant for ALD phenotypes generated data which could not be replicated, recent candidate gene studies and genome-wide scans have identified genetic risk factors which robustly associate with ALD and its complications. These data shed new light on yet unknown pathophysiological aspects of ALD, and potentially open the field for better prevention, screening and the development of novel therapies. The first and most robustly confirmed risk locus for ALD is a sequence variation within the gene coding for patatin-like phospholipase encoding 3 (PNPLA3, rs738409C>G, I148M) which was found to modulate the evolution of steatosis, necroinflammation, fibrosis and HCC in alcoholics.68,69 The genetic risk of ALD has also been studied on a genome-wide level by two recent studies in alcoholic cirrhosis70 and alcoholic hepatitis.71 Both studies confirmed PNPLA3 rs738409 as a strong genetic risk locus for both alcoholic cirrhosis and AH with genome-wide significance, and for cirrhosis, two additional, hitherto unknown loci were identified: membrane bound O-acyltransferase domain containing 7 (MBOAT7) (P=9.25×10−10) and transmembrane 6 superfamily member 2 (TM6SF2). Both PNPLA3 and TM6SF2 are implicated in hepatic lipid trapping, while MBOAT7 mediates the transfer of fatty acid between phospholipids and lysophospholipids, a potent driver of hepatic inflammation.69 However, the functional implication of the mutant PNPLA3 variant is not yet fully understood, partly due to a lack of experimental translation in animals, but a homology model of the patatin domain derived from a plant protein structure suggests that the isoleucine to methionine substitution at position 148 in rs738409 is stereotypically close to the catalytic dyad of the protein (Fig. 3).72 This substitution likely results in impaired accessibility of PNPLA3 substrates, i.e., triglycerides, to the catalytic serine moiety, a theory supported by subsequent molecular dynamic simulations.73 This would result in a reduction in hydrolytic function, “lipid trapping” and the accumulation of fat.
Fig. 3.
Structural modifications at the PNPLA3 rs738409 locus (I148) affect the substrate binding groove rather than the catalytic center of the protein. Substituting methionine (Met) for isoleucine (Ile) at position 148 of the PNPLA3 protein reduces accessibility for substrates (e.g., triglycerides) and thus results in a loss of function.
CLINICAL MANAGEMENT OF ALD
1. Diagnostic evaluation
In most cases, ALD is a clinically silent disease with little or no symptoms in patients with early ALD and in patients with compensated cirrhosis. Thus, diagnosis depends highly on clinical suspicion, various laboratory tests and invasive or noninvasive techniques.74 In some patients with early ALD stigmata of alcohol abuse such as bilateral parotid gland hypertrophy, muscle wasting, malnutrition, Dupuytren’s sign, and signs of peripheral neuropathy may be present, but more often patients are entirely asymptomatic and reluctant to openly admit that their drinking behavior may be the reason of their liver abnormalities. On physical examination of cirrhotic patients, liver-typical skin signs include gynecomastia, spider angiomata, palmar erythema, and smooth tongue. Moreover, jaundice, hepatic encephalopathy, ascites and pedal edema may also be visible at first glance in patients with end-stage liver disease. The diagnosis of ALD is frequently suspected upon documentation of excess alcohol consumption (>40–50 g/day) and the presence of clinical and/or biological abnormalities suggestive of liver injury. However, on taking the medical history one needs to be aware that self-reported alcohol consumption is often under-reported and that quantification of alcohol consumption is at best semi-quantitative.75 Past complications of liver cirrhosis such as gastrointestinal bleeding, ascites, jaundice episodes, or accidents due to encephalopathy or drunkenness reported by the patient or an accompanying person are important diagnostic information.
Laboratory tests such as mean corpuscular volume of red blood cells, γ-glutamyltransferase (GGT) and aspartate amino-transferase (AST), IgA, can indicate early ALD while a decrease of albumin, increased international normalized ratio (INR), elevated bilirubin level and/or a low platelet count are signs of advanced ALD. Many heavy drinkers also reveal elevated levels of triglycerides and uric acid, the latter often associated with gout attacks.76 Alcohol-specific markers include carbohydrate deficient transferrin and ethyl-glucuronide,77 however, sensitivity of the former is limited as many drinkers remain undetected due to normal levels.78 Clinically, GGT is the most frequently used marker to detect previous alcohol consumption, however, it lacks specificity and can also rise due to other etiologies.79 In patients with ALD, the AST/alanine aminotransferase (ALT) ratio typically is >1, and may be >2 in patients with AH. However, it can also be found in patients with advanced cirrhosis regardless of the etiology.
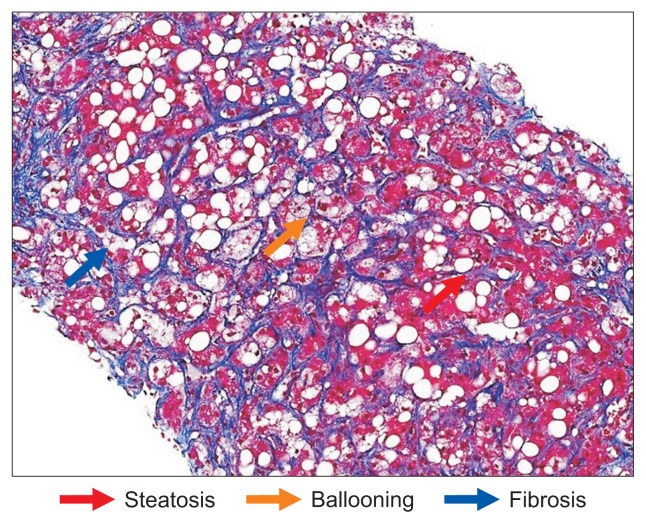
Liver biopsy is not routinely advised in patients with early or cirrhotic stages of ALD if clinical, analytical and imaging data are undisputed.74,80 However, a liver biopsy may be useful to rule out nonalcoholic etiologies or when noninvasive tools fail to obtain a clear result. Biopsies are mostly performed percutaneously, but may require a transjugular route in patients with impaired coagulation due to a low platelet count and/or a prolonged prothrombin time, or when portal pressure shall be measured in addition. Sometimes, a liver biopsy can help to convince a patient of the cause of their liver abnormalities, and to persuade patients to change their drinking behavior, although this line of reasoning is not entirely scientific.81 A clear indication exists in patients with aggressive forms of ALD such as ASH requiring specific therapies (e.g., corticosteroids and/or pentoxifylline) and in patients with other cofactors suspected of contributing to liver disease, e.g., coexisiting viral hepatitis or iron overload.74 The typical findings in patients with ALD include steatosis, hepatocellular damage (ballooning and/or Mallory-Denk bodies), inflammatory infiltrates composed of PMN cells predominating in the lobules, and a variable degree of fibrosis and lobular distortion that may progress to cirrhosis (Fig. 4).82
Fig. 4.
Typical appearance of alcoholic cirrhosis showing three prominent features of alcoholic liver disease, i.e., fibrosis (blue arrow), steatosis (red arrow) and ballooning (yellow arrow). Significant inflammation is often not seen but consists of neutrophilic and lymphocytic infiltrates when visible (chromotrope anilin-blue stain; magnification × 100).
For the assessment of liver fibrosis in patients with ALD, there are noninvasive methods including serum markers and liver stiffness measurement, however, none has been sufficiently validated in ALD. Simple tests that rely on AST levels, such as AST to platelet ratio index and AST/ALT ratio, are not particularly useful in ALD due to the higher AST values in such patients that do not necessarily correlate with severe fibrosis.83 Single variables such as hyaluronic acid are useful to confirm advanced fibrosis or cirrhosis, but are neither specific nor helpful in early diagnosis of ALD. Branded panels such as FibroTest, FibroMeter and Enhanced Liver Fibrosis score have not been sufficiently validated for ALD. Common to all these tests is that they are useful to distinguish between mild and severe fibrosis, but have limited value in intermediate stages of fibrosis.83
Transient elastography (Fibroscan®) is widely established to assess fibrosis in patients with chronic liver disease and has recently been approved by the Food and Drug Adminstration (FDA). In patients with ALD, liver stiffness correlates with the stage of fibrosis,84 but elevated values need to be interpreted with caution in patients with ALD and AST serum levels >100 U/L due to the possibility of falsely elevated liver stiffness as a result of inflammation-related liver congestion. Moreover, recent alcohol consumption can also increase liver stiffness, perhaps related to the vasodilatory effects of alcohol.85 Imaging techniques can also be used to assess the severity of ALD. Ultrasonography, magnetic resonance imaging (MRI), and computed tomography are useful to detect steatosis, advanced fibrosis/cirrhosis as well as signs of portal hypertension.86 Moreover, they are useful for the screening and assessment of complications such as ascites and portal vein thrombosis. Among those methods, ultrasound is the most widely used due to its low cost. MRI and MR spectroscopy are reliable tools for quantifying steatosis but their use is limited by high cost.87 Transient elastography (Fibroscan®) offers a software update to quantify liver fat termed Controlled Attenuation Parameter (CAP function) as a significantly cheaper alternative;88 however, comparative studies are lacking.
A distinct entity represents severe ASH as a relatively rare but serious complication of ALD characterized by new onset jaundice and/or ascites in heavy drinkers with or without underlying advanced ALD. Population based studies estimate approximately 4.5 hospitalizations for AH per 100,000 persons each year, with a slight male predominance, and wide variation across countries.89 Prospective studies assessing the incidence, risk factors and clinical features of AH are clearly needed as it is assumed that a large proportion of ASH cases remain unrecognized and therefore not appropriately treated.
Patients with ASH typically present with rapidly progressive jaundice, often accompanied by fever, abdominal discomfort, anorexia, and weight loss. In severe cases, patients present with ascites, encephalopathy, hepatorenal failure and/or variceal bleeding. Patients with severe AH frequently present with the clinical picture of a so-called systemic inflammatory syndrome characterized by tachycardia, leucocytosis, and elevated C-reactive protein and procalcitonin probably due to sterile inflammation and/or or concomitant infections.90 In some patients, ASH is the first manifestation of a previously unnoticed ALD, in others it can be a complication of cirrhosis.
Serum liver enzyme levels are often elevated 2- to 6-fold, and lower that in acute viral hepatitis, characteristically with AST elevation exceeding that of ALT related to an alcohol-induced deficiency of pyridoxal 5′-phosphate (vitamin B6).91 Most patients with AH have some degree of coagulopathy with an increased INR impaired liver function, and/or low platelet numbers due to splenomegaly from portal hypertension or direct alcohol toxicity on platelets. Particularly severe is the development of kidney failure due to hepatorenal syndrome or acute tubular necrosis which identifies the subgroup with the worst prognosis.92
Of note, patients with ALD can also show an episode of jaundice and liver decompensation due to other reasons than AH such as in sepsis, biliary obstruction, diffuse HCC, drug-induced liver injury or gastrointestinal bleeding. Infections, particularly spontaneous bacterial peritonitis, must be ruled out as they can present with similar clinical findings (abdominal pain, fever, leukocytosis), and because they are a contraindication to specific therapy with corticosteroids. This is why a correct diagnosis and detailed work-up is so important and advocates a liver biopsy as set forth in recent clinical practice guidelines.74,80,93 Due to frequent coexisting ascites and/or coagulopathy a transjugular route is often preferred which also allows for the measurement of hepatovenous pressure gradient as a surrogate marker of portal pressure. Serologic evaluation for viral hepatitis and imaging with Doppler ultrasound to exclude biliary or vascular disorders and HCC are recommended.
Several models have been developed to help predict outcomes of patients with AH and to guide therapy (Table 2). The most widely used is the Maddrey et al.’s94 discriminant function (DF) introduced already in 1978, which is calculated as 4.6×(pro-thrombin time/patient–prothrombin time/control)+serum bilirubin. A DF value ≥32 is indicative of a high risk of short-term mortality (35% at 1 month) and selects patients for corticosteroid therapy. Additional predictive models include the Model for End-Stage Liver Disease (MELD), the Glasgow alcoholic hepatitis (GAH) score, the Age, Bilirubin, INR, Creatinine (ABIC) score.95–97 The MELD is a statistical model that is calculated using serum bilirubin, creatinine, and INR, which is able to predict 30- and 90-day mortality in patients with AH with accuracy similar to the DF.95,97 The GAH score incorporates age, serum bilirubin, blood urea nitrogen, prothrombin time, and peripheral white blood cell count, and accurately predicts short- (28 days) and midterm- (84 days) mortality. The ABIC uses age, bilirubin, INR, and creatinine to estimate a 90-day risk of mortality, and can categorize patients into low (0%), intermediate (30%), and high (75%) risk of death. The MELD has been evaluated in the U.S. cohorts, the GAH in populations from the United Kingdom, and the ABIC in Spain.98–100 An important innovation was the creation of the Lille model which assesses the patients’ prognosis as per response to corticosteroid therapy. The Lille model measures the change in serum bilirubin after one week of corticosteroid incorporating age, albumin, creatinine, and prothrombin time.101 In those not responding to corticosteroids within 7 days of treatment clinical practice guidelines recommend cessation of corticosteroids since the risks, i.e., severe infections, with continued therapy outweigh the benefits. A large multicentric study recently developed a histological scoring system, Alcoholic Hepatitis Histological score (AHHS), capable of predicting short-term survival in AH patients. AHHS computes fibrosis stage, PMN infiltration, type of bilirubinostasis and presence of megamitochondria which are independently associated with patients’ survival in a semiquantitative manner and allows for stratification of patients into low, intermediate, or high risk for death within 90 days.102
Table 2.
Scores for Assessing AH Severity
| Score | Calculator | Interpretation | Remarks | |||
|---|---|---|---|---|---|---|
| DF | DF=4.6 (patient’s PT–reference PT)+total bilirubin (mg/dL) | Poor prognosis when ≥32; defines threshold for corticosteroid therapy | Most widely used score in clinical studies | |||
| No consideration of kidney function | ||||||
| MELD | MELD=3.8×log(bilirubin [mg/dL])+11.2×log(INR)+9.6×log(creatinine [mg/dL])+6.4 | Poor prognosis when ≥18 | Designed for listing patients for liver transplant; performance comparable with DF | |||
| ABIC | (age×0.1)+(serum bilirubin×0.08)+(serum creatinine×0.3)+(INR×0.8) | Low risk ABIC ≤6.71 | Not validated outside Spain | |||
| Intermediate risk when ABIC >6.71 and ≤9.0 | Not designed to guide therapy for patients with AH | |||||
| High risk when ABIC >9.0 | ||||||
|
|
||||||
| GAH | 1 | 2 | 3 | Poor prognosis if score >8 (calculated on day 1 and 7 of hospitalization) | Requires more variables than the other scores | |
|
| ||||||
| Age | <50 | ≥50 | - | |||
| Leucocytes | <15 | ≥15 | - | |||
| Urea (mmol/L) | <5 | ≥5 | - | |||
| INR | <1.5 | 1.5–2.0 | >2.0 | |||
| Bilirubin (mg/dL) | <7.3 | 7.4–14.6 | >14.6 | |||
AH, alcoholic hepatitis; DF, discriminant function; PT, prothrombin time; MELD, Model for End-Stage Liver Disease; INR, international normalized ratio; ABIC, Age, Bilirubin, INR, Creatinine; GAH, Glasgow alcoholic hepatitis.
THERAPY OF PATIENTS WITH ALD
1. Achieving abstinence
The backbone of the treatment of patients with ALD is the achievement and maintenance of alcohol abstinence since the efficacy of medical treatments for ALD is limited in those who continue to drink. As many patients with ALD display clinical criteria of AUD, a generic term covering a wide variety of drinking behaviours and their consequences often labeled as “heavy drinking,” “harmful drinking,” “alcohol misuse/abuse,” “problem drinking” and “alcohol dependence” defined by the fourth edition of the DSM criteria (DSM-IV)103 and the 10th edition of the ICD criteria (ICD-10).104 Both systems describe drinking behavior leading to physical, psychosocial and mental disadvantages requiring therapeutic intervention. Clinical research efforts have focused on treating AUD in ALD patients and current consensus is that a combination of psychosocial interventions, pharmacological therapy and medical management seems to be the most effective management strategy for AUD patients with ALD.105 Pharmaceutical approaches to treat AUD are available, however, their safe use in patients with ALD has only been tested for a few drugs. So far, only baclofen has a published track record that confirms both efficacy and safety in several open label trials106,107 and one randomized controlled trial,108 while the FDA-approved AUD drugs disulfiram and naltrexone are contraindicated in ALD patients due to possible hepatotoxicity. Nalmefene, a μ- and δ-opioid receptor antagonist and κ-opioid receptor partial-agonist, was recently approved for the treatment of AUD by the FDA, but safety data in patients with ALD is limited since patients with advanced ALD were excluded from the registrations trial.109
Assigning the appropriate treatment for each AUD category in ALD patients requires careful assessment of patients in the context of integrated concepts in which physicians, addiction specialists and psychosocial support providers jointly treat ALD patients to achieve abstinence, or at least substantial risk reduction.
2. Nutritional support
While patients with early ALD usually are adequately nourished, those with advanced ALD, and AH in particular, reveal significant clinical signs of malnutrition. Up to 60% of alcoholics with cirrhosis and literally all hospitalized alcoholic cirrhotics reveal some degree of malnutrition which aggravates along with the severity of ALD.110 And although alcohol provides 7.1 kcal/g of energy which is more than that of carbohydrates (4.1 kcal/g), patients with ALD often present with severe primary and secondary malnutrition, and particularly, protein energy malnutrition.110 Therefore, adequate nutritional support is recommended in recent guidelines.74,80,111 The causes of primary malnutrition in ALD include: (1) low dietary intake due to imbalanced diet composition or replacement of food calories by those derived from alcohol; (2) lack of appetite related to dysgeusia, esophagitis, gastritis, poor dental status; (3) lack of palatability of diets low in sodium; (4) malabsorbtion because of diarrhea, exogenous pancreatic insufficiency; and (5) complications of liver disease, e.g., ascites, hepatic encephalopathy. Besides inadequate dietary intake, heavy alcohol consumption can also lead to profound interactions with the metabolism of numerous micronutrients. Uptake and bioavailability of a wide array of water- and fat-soluble vitamins as well as trace elements are influenced by concomitant heavy alcohol and can cause clinical syndromes unrelated to ALD per se, but which should be remembered when treating patients (Table 3).
Table 3.
Micronutrients Affected by Heavy Alcohol Consumption and Corresponding Clinical Syndromes
| Micronutrient | Clinical syndrome |
|---|---|
| Vitamin A | Night blindness, infertility |
| Thiamine | Wernicke-Korsakoff encephalopathy, cardiomyopathie (Beri-Beri) |
| Folate | Anemia, increase of cancer risk |
| Vitamin D | Osteomalacia, osteopenia |
| Vitamin E | Reduced antioxidative resistance |
| Niacine | Pellagra, neuropsychiatric symptoms |
| Pyridoxalphosphat | Anemia |
| Zink | Wound healing problems, skin problems, immunodeficiency, diarrhea |
| Magnesium | Muscle cramps, glucose intolerance |
| Selenium | Myopathy, cardiomyopathy |
While clinical trials failed to demonstrate a benefit from parenteral nutritional therapy in ALD, numerous studies provided robust evidence for a benefit from enteral nutritional support on several surrogate markers of nutritional status such as nitrogen balance, anthropometric variables and survival.110 Several studies suggested a benefit from supplementing diets with the branched-chain amino acids valine, leucine and isoleucine to maintain adequate protein intake without worsening of hepatic encephalopathy in protein-intolerant cirrhotic patients,112,113 but a recent Cochrane analysis of 37 clinical trials not restricted to ALD found only weak evidence supporting the routine use of parenteral nutrition, enteral nutrition, or oral nutritional supplements in patients with liver disease. Benefits of nutritional therapy were limited to weak endpoints such as improved bilirubin levels and a better nitrogen balance in patients actively treated with nutrition, but not on prolongation of survival.114
From a practical point of view, current guidelines recommend a dietary intake of 1.2 to 1.5 g of protein/kg and 35 to 30 kcal/kg body weight, frequent meals including a nighttime snack.74,80,111 Considering the numerous micronutrient deficiencies in advanced ALD, adequate supplementation thereof is also advised.
In patients with severe AH the prevalence of malnutrition reaches 100% and a significant correlation of malnutrition with short- and long-term survival has been demonstrated.115 While earlier randomized trials in relatively small patient numbers reported a possible benefit of vigorous nutritional support in patients with alcoholic cirrhosis and AH, including on improved survival,116 only one recent randomized controlled trial in 136 patients with biopsy-proven AH studied a combination of intensive enteral nutrition via feeding tube plus methylprednisolone against conventional nutrition plus methylprednisolone (controls).117 The primary endpoint was 6-month survival, and secondary end points comprised mortality at 1 month, rates of infection, and occurrence of hepatorenal failure at 6 months. Survival in both groups was similar (44.4% vs 52.1% in controls, p=0.406), and the feeding tube was poorly tolerated. However, patients with a calorie intake of less than 21.5 kcal/kg/day were more likely to die emphasizing the need for adequate nutrition.
3. Pharmaceutical therapy
Despite the prominent burden of ALD on liver-related morbidity and mortality, therapies that specifically target established ALD and/or fibrosis/cirrhosis are not available and very little progress has been made in this regard over the last decades in comparison to the tremendous advances in other liver diseases. For many, the therapeutic watchword has been “just stop drinking” and interest of pharmaceutical companies and clinicians in developing and testing novel drugs to treat ALD has been low. So, numerous preparations are distributed which are at best harmless, but far from truly effective.
Longest known and widely used is an extract of Silybum marianum (milk thistle) which contains silibinin as the biologically most active compound. The premier indication for silymarin treatment is Amanita phalloides (death cup fungus) intoxication in which silymarin acts as a life-saving hepatoprotectant.118 The popularity of silymarin products among patients with chronic liver disease was promoted by a clinical trial in 170 patients with cirrhosis of various etiologies which demonstrated a significant survival benefit in those treated with silymarin.119 Another multicenter trial in 200 patients with alcoholic cirrhosis treated with 450 mg silymarin daily did not confirm a benefit,120 and a Cochrane systematic review of 13 randomized controlled trials found not benefit from silymarin treatment.121
The same fate is shared by data on propylthiouracil,122 col-chicine,123 S-Adenosyl-L-methionine (SAMe),124 and polyenyl-phosphatidylcholine125 which all proved no more effective than placebo in the treatment of ALD.
1) Alcoholic steatohepatitis
A somewhat different situation is that of severe ASH in which therapeutic challenges reside in the restoration of liver synthetic function as well as reducing hepatic and systemic inflammation. The linchpin of AH treatment are abstinence, corticosteroids and intensive care addressing the complications of ASH such as renal failure and sepsis.
Corticosteroids have been used in the treatment of ASH for more than 40 years.126 A meta-analysis from individual data from studies considered of high quality showed improved survival in patients with a high DF when treated with corticoste-roids.127 The most studied formulation is prednisolone 40 mg daily for 4 weeks, with or without a taper after that period. The response to prednisolone can be assessed based on the change in bilirubin after one week of therapy and quantified using the Lille score, as outlined above.101 For those with a poor response as indicated by a Lille score ≥0.45, stopping therapy can be considered, as these patients are not likely to benefit from continued corticosteroids and rather incur side-effects. Based on these data, expert practice guidelines recommend the use of corticosteroids in AH patients with a DF >32, and the European guideline advises cessation thereof should response after 7 days of treatment should be insufficient according to the Lille model.74,80
Numerous reports suggested a benefit of pentoxifylline (PTX), an orally absorbed nonselective phosphodiesterase inhibitor approved for the treatment of intermittent claudication, in reducing the development of the hepatorenal syndrome in patients with ASH.128 However, recent data from the Steroid or Pentoxifylline for Alcoholic Hepatitis (STOPAH) trial, a large randomized-controlled trial of treatment of patients with severe AH with prednisolone or PTX, or their combination has raised doubts over the benefit of PTX in AH patients.129 Prednisolone alone reduced the risk of 28-day mortality, but no additional benefit derived from PTX. But the trial was underpowered to analyze the subgroup of patients with hepatorenal failure which may have resulted in a failure to detect a benefit in a specific group where PTX could have been of value. Similar results came from a similar trial, which however was again underpowered for the subgroup of patients with hepatorenal syndrome.130
N-acetylcysteine (NAC) is well-established in the treatment of fulminant hepatic failure due to paracetamol overdose,131 and improves transplant-free survival in early stage nonparacetamol acute liver failure.132 A recent randomized trial showed that the combination of NAC with prednisolone reduced 1-month mortality (8% vs 24%) and the incidence of hepatorenal syndrome and infection.133 The favorable safety profile of NAC makes it a potential option, in combination with corticosteroids, for patients with severe disease.
4. Liver transplantation
ALD is among the most frequent indications for orthotopic liver transplantation (OLT) worldwide.16 In general, mortality and morbidity after LT in ALD patients is similar to patients with other etiologies, but the causes of death after transplantation for ALD differ from those in non-ALD recipients.134 In particular, cardiovascular causes and de novo malignancies are more frequent in the patients transplanted for ALD both of which are associated with decreased survival.16,135 The combination of cardiovascular deaths and of new onset cancers of the aerodigestive tract in patients after OLT for ALD strongly suggest a causal linkage with cigarette smoking, which is common among ALD transplanted patients. These data highlight a serious health risk for ALD patients after OLT and demonstrate the need for stringent clinical monitoring and intervention for tobacco use in the pre- and post-transplant periods.
OLT listing should be considered for patients who develop liver dysfunction corresponding to a Child-Pugh score ≥7 or MELD score ≥10, or clinical decompensation (ascites, variceal bleeding, or hepatic encephalopathy).93
Most transplant programs require a 6-month period of abstinence before consideration for LT, mainly for two reasons: (1) to allow for recovery of liver function which may improve to the point that OLT is no longer necessary and (2) to reduce the risk of posttransplant recidivism, although its value for predicting abstinence after OLT is poor.136,137 According the “6-month rule,” patients with AH are ineligible for OLT and die if they do not respond to corticosteroids. However, posttransplant outcomes including that of abstinence seem to be good for highly selected patients with severe AH unresponsive to medical therapy, as demonstrated by a recent French multicenter study in nonresponders to prior corticosteroid therapy.138 Mathurin et al.138 selected 26 patients with severe AH with a median Lille score of 0.88 indicating a high risk of short-term death for OLT after careful pretransplant assessment. The cumulative 6-month survival rate was 77%, a figure comparable to those for other indications. Recurrence to harmful drinking was extremely rare, likely due to the stringent selection criteria (first AH episode, support from family background, exclusion of psychiatric illnesses, other substance abuse, consensus among OLT team members, absence of violence). This indication of liver transplantation is increasingly accepted in many transplant centers including in the United State.139
After OLT, ALD patients require lifelong follow-up for prevention and management of complications, just as all other OLT patients, too. As mentioned above, cardiovascular disease, chronic kidney disease, and cancer must be kept in mind. Calcineurin inhibitor-based immunosuppression (particularly cyclosporine A) increase the risk of metabolic complications such as hypertension, diabetes, and dyslipidemia, which may contribute to the high incidence of cardiovascular disease and kidney disease in ALD patients. However, ALD is a good indication of OLT as demonstrated by data from the European Liver Transplant Registry, showing survival at 84%, 78%, 73%, and 58% after 1, 3, 5, and 10 years, respectively, which is better than that with viral hepatitis and cryptogenic cirrhosis.16
Patients transplanted due to ALD often present with multisystemic effects of long-term ethanol abuse.140 These comorbidities include malnutrition, muscle wasting due to alcoholic myopathy, vitamin deficiencies, peripheral and central neural system abnormalities, and others. Therefore, the care of patients transplanted for ALD ideally calls for a multidisciplinary approach.
CONCLUSIONS
Although much insight has been gained in the epidemiology, pathophysiology and clinical diagnosis of ALD, the armoury of therapies is still disappointing. This lack of therapeutic options to treat AUD, ALD and related complications will only improve if more scientific, medical and societal attention is paid to this prevalent and deadly disease. A coalition among political, scientific, and industry-based stakeholders is required to make a step forward. So far, these peers devoted the topic “ALD” only the role of a fringe group when drafting their health policies, research efforts and conference programs. In essence, this attitude is a good example of a prepossession that made ALD an orphan disease in its own right. But ALD is a fully preventable disease, and more efforts should be made to use this fact as an advantage.
ACKNOWLEDGEMENTS
The present work was supported by grants from the Swiss National Funds and the Swiss Foundation for Alcohol Research (SSA) to Felix Stickel.
Footnotes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373:2223–2233. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. European status report on alcohol and health 2010. Copenhagen: WHO Regional Office for Europe; 2010. [Google Scholar]
- 3.Rehm J, Shield KD, Gmel G, Rehm MX, Frick U. Modeling the impact of alcohol dependence on mortality burden and the effect of available treatment interventions in the European Union. Eur Neuropsychopharmacol. 2013;23:89–97. doi: 10.1016/j.euroneuro.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 4.Rehm J, Samokhvalov AV, Shield KD. Global burden of alcoholic liver diseases. J Hepatol. 2013;59:160–168. doi: 10.1016/j.jhep.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 5.Leon DA, McCambridge J. Liver cirrhosis mortality rates in Britain from 1950 to 2002: an analysis of routine data. Lancet. 2006;367:52–56. doi: 10.1016/S0140-6736(06)67924-5. [DOI] [PubMed] [Google Scholar]
- 6.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A. 2015;112:15078–15083. doi: 10.1073/pnas.1518393112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yadav D, Lowenfels AB. The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology. 2013;144:1252–1261. doi: 10.1053/j.gastro.2013.01.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Popova S, Lange S, Shield K, et al. Comorbidity of fetal alcohol spectrum disorder: a systematic review and meta-analysis. Lancet. 2016;387:978–987. doi: 10.1016/S0140-6736(15)01345-8. [DOI] [PubMed] [Google Scholar]
- 9.Seitz HK, Stickel F. Molecular mechanisms of alcohol-mediated carcinogenesis. Nat Rev Cancer. 2007;7:599–612. doi: 10.1038/nrc2191. [DOI] [PubMed] [Google Scholar]
- 10.Fernández-Solà J. Cardiovascular risks and benefits of moderate and heavy alcohol consumption. Nat Rev Cardiol. 2015;12:576–587. doi: 10.1038/nrcardio.2015.91. [DOI] [PubMed] [Google Scholar]
- 11.Foulds JA, Adamson SJ, Boden JM, Williman JA, Mulder RT. Depression in patients with alcohol use disorders: systematic review and meta-analysis of outcomes for independent and substance-induced disorders. J Affect Disord. 2015;185:47–59. doi: 10.1016/j.jad.2015.06.024. [DOI] [PubMed] [Google Scholar]
- 12.Mokdad AA, Lopez AD, Shahraz S, et al. Liver cirrhosis mortality in 187 countries between 1980 and 2010: a systematic analysis. BMC Med. 2014;12:145. doi: 10.1186/s12916-014-0145-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization. Global health estimates (GEHE) 2014: YLL by age, sex and cause. Geneva: World Health Organization; 2012. [Google Scholar]
- 14.World Health Organization. WHO mortality database: raw data files. Geneva: World Health Organization; 2015. [Google Scholar]
- 15.Sheron N. Alcohol and liver disease in Europe: simple measures have the potential to prevent tens of thousands of premature deaths. J Hepatol. 2016;64:957–967. doi: 10.1016/j.jhep.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 16.Burra P, Senzolo M, Adam R, et al. Liver transplantation for alcoholic liver disease in Europe: a study from the ELTR (European Liver Transplant Registry) Am J Transplant. 2010;10:138–148. doi: 10.1111/j.1600-6143.2009.02869.x. [DOI] [PubMed] [Google Scholar]
- 17.Sheron N, Hawkey C, Gilmore I. Projections of alcohol deaths: a wake-up call. Lancet. 2011;377:1297–1299. doi: 10.1016/S0140-6736(11)60022-6. [DOI] [PubMed] [Google Scholar]
- 18.Teli MR, Day CP, Burt AD, Bennett MK, James OF. Determinants of progression to cirrhosis or fibrosis in pure alcoholic fatty liver. Lancet. 1995;346:987–990. doi: 10.1016/S0140-6736(95)91685-7. [DOI] [PubMed] [Google Scholar]
- 19.Stickel F. Alcoholic cirrhosis and hepatocellular carcinoma. Adv Exp Med Biol. 2015;815:113–130. doi: 10.1007/978-3-319-09614-8_7. [DOI] [PubMed] [Google Scholar]
- 20.Konishi M, Ishii H. Role of microsomal enzymes in development of alcoholic liver diseases. J Gastroenterol Hepatol. 2007;22(Suppl 1):S7–S10. doi: 10.1111/j.1440-1746.2006.04638.x. [DOI] [PubMed] [Google Scholar]
- 21.Oneta CM, Lieber CS, Li J, et al. Dynamics of cytochrome P4502E1 activity in man: induction by ethanol and disappearance during withdrawal phase. J Hepatol. 2002;36:47–52. doi: 10.1016/S0168-8278(01)00223-9. [DOI] [PubMed] [Google Scholar]
- 22.Neuman MG, Malnick S, Maor Y, et al. Alcoholic liver disease: clinical and translational research. Exp Mol Pathol. 2015;99:596–610. doi: 10.1016/j.yexmp.2015.09.001. [DOI] [PubMed] [Google Scholar]
- 23.Gouillon Z, Lucas D, Li J, et al. Inhibition of ethanol-induced liver disease in the intragastric feeding rat model by chlormethiazole. Proc Soc Exp Biol Med. 2000;224:302–308. doi: 10.1046/j.1525-1373.2000.22435.x. [DOI] [PubMed] [Google Scholar]
- 24.Bradford BU, Kono H, Isayama F, et al. Cytochrome P450 CYP2E1, but not nicotinamide adenine dinucleotide phosphate oxidase, is required for ethanol-induced oxidative DNA damage in rodent liver. Hepatology. 2005;41:336–344. doi: 10.1002/hep.20532. [DOI] [PubMed] [Google Scholar]
- 25.Scoccianti C, Cecchini M, Anderson AS, et al. European Code against Cancer 4th Edition: alcohol drinking and cancer. Cancer Epidemiol. 2015;39(Suppl 1):S67–S74. doi: 10.1016/j.canep.2015.01.007. [DOI] [PubMed] [Google Scholar]
- 26.Gao B, Bataller R. Alcoholic liver disease: pathogenesis and new therapeutic targets. Gastroenterology. 2011;141:1572–1585. doi: 10.1053/j.gastro.2011.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brunt EM, Neuschwander-Tetri BA, Burt AD. Fatty liver disease: alcoholic and non-alcoholic. In: Burt A, Portmann B, Ferrell L, editors. MacSween’s pathology of the liver. 6th ed. Edinburgh: Churchill Livingstone; 2012. pp. 293–360. [DOI] [Google Scholar]
- 28.Roh YS, Zhang B, Loomba R, Seki E. TLR2 and TLR9 contribute to alcohol-mediated liver injury through induction of CXCL1 and neutrophil infiltration. Am J Physiol Gastrointest Liver Physiol. 2015;309:G30–G41. doi: 10.1152/ajpgi.00031.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.An L, Wang X, Cederbaum AI. Cytokines in alcoholic liver disease. Arch Toxicol. 2012;86:1337–1348. doi: 10.1007/s00204-012-0814-6. [DOI] [PubMed] [Google Scholar]
- 30.Petrasek J, Csak T, Szabo G. Toll-like receptors in liver disease. Adv Clin Chem. 2013;59:155–201. doi: 10.1016/B978-0-12-405211-6.00006-1. [DOI] [PubMed] [Google Scholar]
- 31.Lemmers A, Moreno C, Gustot T, et al. The interleukin-17 pathway is involved in human alcoholic liver disease. Hepatology. 2009;49:646–657. doi: 10.1002/hep.22680. [DOI] [PubMed] [Google Scholar]
- 32.Szabo G, Petrasek J. Inflammasome activation and function in liver disease. Nat Rev Gastroenterol Hepatol. 2015;12:387–400. doi: 10.1038/nrgastro.2015.94. [DOI] [PubMed] [Google Scholar]
- 33.Schuppan D. Liver fibrosis: common mechanisms and antifibrotic therapies. Clin Res Hepatol Gastroenterol. 2015;39(Suppl 1):S51–S59. doi: 10.1016/j.clinre.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 34.Svegliati-Baroni G, Inagaki Y, Rincon-Sanchez AR, et al. Early response of alpha2(I) collagen to acetaldehyde in human hepatic stellate cells is TGF-beta independent. Hepatology. 2005;42:343–352. doi: 10.1002/hep.20798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bataller R, Schwabe RF, Choi YH, et al. NADPH oxidase signal transduces angiotensin II in hepatic stellate cells and is critical in hepatic fibrosis. J Clin Invest. 2003;112:1383–1394. doi: 10.1172/JCI18212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Elinav E, Ali M, Bruck R, et al. Competitive inhibition of leptin signaling results in amelioration of liver fibrosis through modulation of stellate cell function. Hepatology. 2009;49:278–286. doi: 10.1002/hep.22584. [DOI] [PubMed] [Google Scholar]
- 37.Patsenker E, Stoll M, Millonig G, et al. Cannabinoid receptor type I modulates alcohol-induced liver fibrosis. Mol Med. 2011;17:1285–1294. doi: 10.2119/molmed.2011.00149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zamara E, Novo E, Marra F, et al. 4-Hydroxynonenal as a selective profibrogenic stimulus for activated human hepatic stellate cells. J Hepatol. 2004;40:60–68. doi: 10.1016/S0168-8278(03)00480-X. [DOI] [PubMed] [Google Scholar]
- 39.Fattovich G, Stroffolini T, Zagni I, Donato F. Hepatocellular carcinoma in cirrhosis: incidence and risk factors. Gastroenterology. 2004;127(5 Suppl 1):S35–S50. doi: 10.1053/j.gastro.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 40.Villanueva A, Portela A, Sayols S, et al. DNA methylation-based prognosis and epidrivers in hepatocellular carcinoma. Hepatology. 2015;61:1945–1956. doi: 10.1002/hep.27732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dubuquoy L, Louvet A, Lassailly G, et al. Progenitor cell expansion and impaired hepatocyte regeneration in explanted livers from alcoholic hepatitis. Gut. 2015;64:1949–1960. doi: 10.1136/gutjnl-2014-308410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lanthier N, Rubbia-Brandt L, Lin-Marq N, et al. Hepatic cell proliferation plays a pivotal role in the prognosis of alcoholic hepatitis. J Hepatol. 2015;63:609–621. doi: 10.1016/j.jhep.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 43.Sancho-Bru P, Altamirano J, Rodrigo-Torres D, et al. Liver progenitor cell markers correlate with liver damage and predict short-term mortality in patients with alcoholic hepatitis. Hepatology. 2012;55:1931–1941. doi: 10.1002/hep.25614. [DOI] [PubMed] [Google Scholar]
- 44.Mathews S, Xu M, Wang H, Bertola A, Gao B. Animals models of gastrointestinal and liver diseases. Animal models of alcohol-induced liver disease: pathophysiology, translational relevance, and challenges. Am J Physiol Gastrointest Liver Physiol. 2014;306:G819–G823. doi: 10.1152/ajpgi.00041.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mandrekar P, Bataller R, Tsukamoto H, Gao B. Alcoholic hepatitis: translational approaches to develop targeted therapies. Hepatology. 2016;64:1343–1355. doi: 10.1002/hep.28530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.de la M Hall P, Lieber CS, DeCarli LM, et al. Models of alcoholic liver disease in rodents: a critical evaluation. Alcohol Clin Exp Res. 2001;25(5 Suppl ISBRA):254S–261S. doi: 10.1111/j.1530-0277.2001.tb02405.x. [DOI] [PubMed] [Google Scholar]
- 47.Bertola A, Mathews S, Ki SH, Wang H, Gao B. Mouse model of chronic and binge ethanol feeding (the NIAAA model) Nat Protoc. 2013;8:627–637. doi: 10.1038/nprot.2013.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shalem O, Sanjana NE, Zhang F. High-throughput functional genomics using CRISPR-Cas9. Nat Rev Genet. 2015;16:299–311. doi: 10.1038/nrg3899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sørensen TI, Orholm M, Bentsen KD, Høybye G, Eghøje K, Christ-offersen P. Prospective evaluation of alcohol abuse and alcoholic liver injury in men as predictors of development of cirrhosis. Lancet. 1984;2:241–244. doi: 10.1016/S0140-6736(84)90295-2. [DOI] [PubMed] [Google Scholar]
- 50.Kamper-Jørgensen M, Grønbaek M, Tolstrup J, Becker U. Alcohol and cirrhosis: dose. Response or threshold effect? J Hepatol. 2004;41:25–30. doi: 10.1016/j.jhep.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 51.Bellentani S, Saccoccio G, Costa G, et al. Drinking habits as cofactors of risk for alcohol induced liver damage: the Dionysos Study Group. Gut. 1997;41:845–850. doi: 10.1136/gut.41.6.845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Becker U, Grønbaek M, Johansen D, Sørensen TI. Lower risk for alcohol-induced cirrhosis in wine drinkers. Hepatology. 2002;35:868–875. doi: 10.1053/jhep.2002.32101. [DOI] [PubMed] [Google Scholar]
- 53.Johansen D, Friis K, Skovenborg E, Grønbaek M. Food buying habits of people who buy wine or beer: cross sectional study. BMJ. 2006;332:519–522. doi: 10.1136/bmj.38694.568981.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kennedy OJ, Roderick P, Buchanan R, Fallowfield JA, Hayes PC, Parkes J. Systematic review with meta-analysis: coffee consumption and the risk of cirrhosis. Aliment Pharmacol Ther. 2016;43:562–574. doi: 10.1111/apt.13523. [DOI] [PubMed] [Google Scholar]
- 55.Dam MK, Flensborg-Madsen T, Eliasen M, Becker U, Tolstrup JS. Smoking and risk of liver cirrhosis: a population-based cohort study. Scand J Gastroenterol. 2013;48:585–591. doi: 10.3109/00365521.2013.777469. [DOI] [PubMed] [Google Scholar]
- 56.Shoreibah M, Anand BS, Singal AK. Alcoholic hepatitis and concomitant hepatitis C virus infection. World J Gastroenterol. 2014;20:11929–11934. doi: 10.3748/wjg.v20.i34.11929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Monto A, Patel K, Bostrom A, et al. Risks of a range of alcohol intake on hepatitis C-related fibrosis. Hepatology. 2004;39:826–834. doi: 10.1002/hep.20127. [DOI] [PubMed] [Google Scholar]
- 58.Gitto S, Micco L, Conti F, Andreone P, Bernardi M. Alcohol and viral hepatitis: a mini-review. Dig Liver Dis. 2009;41:67–70. doi: 10.1016/j.dld.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 59.Naveau S, Giraud V, Borotto E, Aubert A, Capron F, Chaput JC. Excess weight risk factor for alcoholic liver disease. Hepatology. 1997;25:108–111. doi: 10.1002/hep.510250120. [DOI] [PubMed] [Google Scholar]
- 60.Raynard B, Balian A, Fallik D, et al. Risk factors of fibrosis in alcohol-induced liver disease. Hepatology. 2002;35:635–638. doi: 10.1053/jhep.2002.31782. [DOI] [PubMed] [Google Scholar]
- 61.Hart CL, Morrison DS, Batty GD, Mitchell RJ, Davey Smith G. Effect of body mass index and alcohol consumption on liver disease: analysis of data from two prospective cohort studies. BMJ. 2010;340:c1240. doi: 10.1136/bmj.c1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Reed T, Page WF, Viken RJ, Christian JC. Genetic predisposition to organ-specific endpoints of alcoholism. Alcohol Clin Exp Res. 1996;20:1528–1533. doi: 10.1111/j.1530-0277.1996.tb01695.x. [DOI] [PubMed] [Google Scholar]
- 63.Eagon PK. Alcoholic liver injury: influence of gender and hormones. World J Gastroenterol. 2010;16:1377–1384. doi: 10.3748/wjg.v16.i11.1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Baraona E, Abittan CS, Dohmen K, et al. Gender differences in pharmacokinetics of alcohol. Alcohol Clin Exp Res. 2001;25:502–507. doi: 10.1111/j.1530-0277.2001.tb02242.x. [DOI] [PubMed] [Google Scholar]
- 65.Marshall AW, Kingstone D, Boss M, Morgan MY. Ethanol elimination in males and females: relationship to menstrual cycle and body composition. Hepatology. 1983;3:701–706. doi: 10.1002/hep.1840030513. [DOI] [PubMed] [Google Scholar]
- 66.Stinson FS, Grant BF, Dufour MC. The critical dimension of ethnicity in liver cirrhosis mortality statistics. Alcohol Clin Exp Res. 2001;25:1181–1187. doi: 10.1111/j.1530-0277.2001.tb02333.x. [DOI] [PubMed] [Google Scholar]
- 67.Levy RE, Catana AM, Durbin-Johnson B, Halsted CH, Medici V. Ethnic differences in presentation and severity of alcoholic liver disease. Alcohol Clin Exp Res. 2015;39:566–574. doi: 10.1111/acer.12660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Anstee QM, Daly AK, Day CP. Genetics of alcoholic liver disease. Semin Liver Dis. 2015;35:361–374. doi: 10.1055/s-0035-1567832. [DOI] [PubMed] [Google Scholar]
- 69.Stickel F, Moreno C, Hampe J, Morgan MY. The genetics of alcohol dependence and alcohol-related liver disease. J Hepatol. 2017;66:195–211. doi: 10.1016/j.jhep.2016.08.011. [DOI] [PubMed] [Google Scholar]
- 70.Buch S, Stickel F, Trépo E, et al. A genome-wide association study confirms PNPLA3 and identifies TM6SF2 and MBOAT7 as risk loci for alcohol-related cirrhosis. Nat Genet. 2015;47:1443–1448. doi: 10.1038/ng.3417. [DOI] [PubMed] [Google Scholar]
- 71.Atkinson S, Way M, McQuillin A, Morgan M, Thursz M. A genome-wide association study identifies PNPLA3 and SLC38A4 as risk loci for alcoholic hepatitis. J Hepatol. 2016;64(2 Suppl):S134. doi: 10.1016/S0168-8278(16)01634-2. [DOI] [Google Scholar]
- 72.He S, McPhaul C, Li JZ, et al. A sequence variation (I148M) in PNPLA3 associated with nonalcoholic fatty liver disease disrupts triglyceride hydrolysis. J Biol Chem. 2010;285:6706–6715. doi: 10.1074/jbc.M109.064501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Xin YN, Zhao Y, Lin ZH, Jiang X, Xuan SY, Huang J. Molecular dynamics simulation of PNPLA3 I148M polymorphism reveals reduced substrate access to the catalytic cavity. Proteins. 2013;81:406–414. doi: 10.1002/prot.24199. [DOI] [PubMed] [Google Scholar]
- 74.European Association for the Study of Liver. EASL clinical practical guidelines: management of alcoholic liver disease. J Hepatol. 2012;57:399–420. doi: 10.1016/j.jhep.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 75.Stockwell T, Zhao J, Greenfield T, Li J, Livingston M, Meng Y. Estimating under- and over-reporting of drinking in national surveys of alcohol consumption: identification of consistent biases across four English-speaking countries. Addiction. 2016;111:1203–1213. doi: 10.1111/add.13373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tu HP, Tung YC, Tsai WC, Lin GT, Ko YC, Lee SS. Alcohol-related diseases and alcohol dependence syndrome is associated with increased gout risk: a nationwide population-based cohort study. Joint Bone Spine. doi: 10.1016/j.jbspin.2016.02.024. Epub 2016 May 26. https://doi.org/10.1016/j.jbspin.2016.02.024. [DOI] [PubMed] [Google Scholar]
- 77.Lowe JM, McDonell MG, Leickly E, et al. Determining ethyl glucuronide cutoffs when detecting self-reported alcohol use in addiction treatment patients. Alcohol Clin Exp Res. 2015;39:905–910. doi: 10.1111/acer.12699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hock B, Schwarz M, Domke I, et al. Validity of carbohydrate-deficient transferrin (%CDT), gamma-glutamyltransferase (gamma-GT) and mean corpuscular erythrocyte volume (MCV) as biomarkers for chronic alcohol abuse: a study in patients with alcohol dependence and liver disorders of non-alcoholic and alcoholic origin. Addiction. 2005;100:1477–1486. doi: 10.1111/j.1360-0443.2005.01216.x. [DOI] [PubMed] [Google Scholar]
- 79.Alatalo P, Koivisto H, Puukka K, et al. Biomarkers of liver status in heavy drinkers, moderate drinkers and abstainers. Alcohol Alcohol. 2009;44:199–203. doi: 10.1093/alcalc/agn099. [DOI] [PubMed] [Google Scholar]
- 80.O’Shea RS, Dasarathy S, McCullough AJ Practice Guideline Committee of the American Association for the Study of Liver Diseases; Practice Parameters Committee of the American College of Gastroenterology. Alcoholic liver disease. Hepatology. 2010;51:307–328. doi: 10.1002/hep.23258. [DOI] [PubMed] [Google Scholar]
- 81.Trabut JB, Plat A, Thepot V, et al. Influence of liver biopsy on abstinence in alcohol-dependent patients. Alcohol Alcohol. 2008;43:559–563. doi: 10.1093/alcalc/agn046. [DOI] [PubMed] [Google Scholar]
- 82.Tannapfel A, Denk H, Dienes HP, et al. Histopathological diagnosis of non-alcoholic and alcoholic fatty liver disease. Virchows Arch. 2011;458:511–523. doi: 10.1007/s00428-011-1066-1. [DOI] [PubMed] [Google Scholar]
- 83.Lombardi R, Buzzetti E, Roccarina D, Tsochatzis EA. Non-invasive assessment of liver fibrosis in patients with alcoholic liver disease. World J Gastroenterol. 2015;21:11044–11052. doi: 10.3748/wjg.v21.i39.11044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mueller S, Millonig G, Sarovska L, et al. Increased liver stiffness in alcoholic liver disease: differentiating fibrosis from steatohepatitis. World J Gastroenterol. 2010;16:966–972. doi: 10.3748/wjg.v16.i8.966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gelsi E, Dainese R, Truchi R, et al. Effect of detoxification on liver stiffness assessed by Fibroscan® in alcoholic patients. Alcohol Clin Exp Res. 2011;35:566–570. doi: 10.1111/j.1530-0277.2010.01374.x. [DOI] [PubMed] [Google Scholar]
- 86.Penny SM. Alcoholic liver disease. Radiol Technol. 2013;84:577–592. [PubMed] [Google Scholar]
- 87.d’Assignies G, Fontés G, Kauffmann C, et al. Early detection of liver steatosis by magnetic resonance imaging in rats infused with glucose and intralipid solutions and correlation to insulin levels. Metabolism. 2013;62:1850–1857. doi: 10.1016/j.metabol.2013.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.de Lédinghen V, Vergniol J, Capdepont M, et al. Controlled attenuation parameter (CAP) for the diagnosis of steatosis: a prospective study of 5323 examinations. J Hepatol. 2014;60:1026–1031. doi: 10.1016/j.jhep.2013.12.018. [DOI] [PubMed] [Google Scholar]
- 89.Sandahl TD, Jepsen P, Thomsen KL, Vilstrup H. Incidence and mortality of alcoholic hepatitis in Denmark 1999–2008: a nationwide population based cohort study. J Hepatol. 2011;54:760–764. doi: 10.1016/j.jhep.2010.07.016. [DOI] [PubMed] [Google Scholar]
- 90.Cervoni JP, Thévenot T, Weil D, et al. C-reactive protein predicts short-term mortality in patients with cirrhosis. J Hepatol. 2012;56:1299–1304. doi: 10.1016/j.jhep.2011.12.030. [DOI] [PubMed] [Google Scholar]
- 91.Diehl AM, Potter J, Boitnott J, Van Duyn MA, Herlong HF, Mezey E. Relationship between pyridoxal 5′-phosphate deficiency and aminotransferase levels in alcoholic hepatitis. Gastroenterology. 1984;86:632–636. [PubMed] [Google Scholar]
- 92.Martín-Llahí M, Guevara M, Torre A, et al. Prognostic importance of the cause of renal failure in patients with cirrhosis. Gastroenterology. 2011;140:488–496. doi: 10.1053/j.gastro.2010.07.043. [DOI] [PubMed] [Google Scholar]
- 93.Murray KF, Carithers RL, Jr AASLD. AASLD practice guidelines: evaluation of the patient for liver transplantation. Hepatology. 2005;41:1407–1432. doi: 10.1002/hep.20704. [DOI] [PubMed] [Google Scholar]
- 94.Maddrey WC, Boitnott JK, Bedine MS, Weber FL, Jr, Mezey E, White RI., Jr Corticosteroid therapy of alcoholic hepatitis. Gastroenterology. 1978;75:193–199. [PubMed] [Google Scholar]
- 95.Dunn W, Jamil LH, Brown LS, et al. MELD accurately predicts mortality in patients with alcoholic hepatitis. Hepatology. 2005;41:353–358. doi: 10.1002/hep.20503. [DOI] [PubMed] [Google Scholar]
- 96.Forrest EH, Morris AJ, Stewart S, et al. The Glasgow alcoholic hepatitis score identifies patients who may benefit from corticosteroids. Gut. 2007;56:1743–1746. doi: 10.1136/gut.2006.099226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Dominguez M, Rincón D, Abraldes JG, et al. A new scoring system for prognostic stratification of patients with alcoholic hepatitis. Am J Gastroenterol. 2008;103:2747–2756. doi: 10.1111/j.1572-0241.2008.02104.x. [DOI] [PubMed] [Google Scholar]
- 98.Srikureja W, Kyulo NL, Runyon BA, Hu KQ. MELD score is a better prognostic model than Child-Turcotte-Pugh score or discriminant function score in patients with alcoholic hepatitis. J Hepatol. 2005;42:700–706. doi: 10.1016/j.jhep.2004.12.022. [DOI] [PubMed] [Google Scholar]
- 99.Sandahl TD, Jepsen P, Ott P, Vilstrup H. Validation of prognostic scores for clinical use in patients with alcoholic hepatitis. Scand J Gastroenterol. 2011;46:1127–1132. doi: 10.3109/00365521.2011.587200. [DOI] [PubMed] [Google Scholar]
- 100.Papastergiou V, Tsochatzis EA, Pieri G, et al. Nine scoring models for short-term mortality in alcoholic hepatitis: cross-validation in a biopsy-proven cohort. Aliment Pharmacol Ther. 2014;39:721–732. doi: 10.1111/apt.12654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Louvet A, Naveau S, Abdelnour M, et al. The Lille model: a new tool for therapeutic strategy in patients with severe alcoholic hepatitis treated with steroids. Hepatology. 2007;45:1348–1354. doi: 10.1002/hep.21607. [DOI] [PubMed] [Google Scholar]
- 102.Altamirano J, Miquel R, Katoonizadeh A, et al. A histologic scoring system for prognosis of patients with alcoholic hepatitis. Gastroenterology. 2014;146:1231–1239. doi: 10.1053/j.gastro.2014.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 104.World Health Organization. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1992. [Google Scholar]
- 105.Addolorato G, Mirijello A, Barrio P, Gual A. Treatment of alcohol use disorders in patients with alcoholic liver disease. J Hepatol. 2016;65:618–630. doi: 10.1016/j.jhep.2016.04.029. [DOI] [PubMed] [Google Scholar]
- 106.Leggio L, Ferrulli A, Zambon A, et al. Baclofen promotes alcohol abstinence in alcohol dependent cirrhotic patients with hepatitis C virus (HCV) infection. Addict Behav. 2012;37:561–564. doi: 10.1016/j.addbeh.2011.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Barrault C, Lison H, Roudot-Thoraval F, et al. One year effectiveness of Baclofen treatment in 100 alcohol-dependent patients. J Hepatol. 2015;62(Suppl 2):S758–S759. doi: 10.1016/S0168-8278(15)31288-5. [DOI] [Google Scholar]
- 108.Owens L, Rose A, Thompson A, Pirmohamed M, Gilmore I, Richardson P. Baclofen: maintenance of abstinence in alcohol dependent patients attending liver clinic. J Hepatol. 2015;62(Suppl 2):S767. doi: 10.1016/S0168-8278(15)31309-X. [DOI] [PubMed] [Google Scholar]
- 109.Palpacuer C, Laviolle B, Boussageon R, Reymann JM, Bellissant E, Naudet F. Risks and benefits of nalmefene in the treatment of adult alcohol dependence: a systematic literature review and meta-analysis of published and unpublished double-blind randomized controlled trials. PLoS Med. 2015;12:e1001924. doi: 10.1371/journal.pmed.1001924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Stickel F, Hoehn B, Schuppan D, Seitz HK. Review article: nutritional therapy in alcoholic liver disease. Aliment Pharmacol Ther. 2003;18:357–373. doi: 10.1046/j.1365-2036.2003.01660.x. [DOI] [PubMed] [Google Scholar]
- 111.Plauth M, Cabré E, Riggio O, et al. ESPEN guidelines on enteral nutrition: liver disease. Clin Nutr. 2006;25:285–294. doi: 10.1016/j.clnu.2006.01.018. [DOI] [PubMed] [Google Scholar]
- 112.Marchesini G, Dioguardi FS, Bianchi GP, et al. Long-term oral branched-chain amino acid treatment in chronic hepatic encephalopathy: a randomized double-blind casein-controlled trial. The Italian Multicenter Study Group. J Hepatol. 1990;11:92–101. doi: 10.1016/0168-8278(90)90278-Y. [DOI] [PubMed] [Google Scholar]
- 113.Muto Y, Sato S, Watanabe A, et al. Effects of oral branched-chain amino acid granules on event-free survival in patients with liver cirrhosis. Clin Gastroenterol Hepatol. 2005;3:705–713. doi: 10.1016/S1542-3565(05)00017-0. [DOI] [PubMed] [Google Scholar]
- 114.Koretz RL, Avenell A, Lipman TO. Nutritional support for liver disease. Cochrane Database Syst Rev. 2012;(5):CD008344. doi: 10.1002/14651858.CD008344.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Mendenhall C, Roselle GA, Gartside P, Moritz T. Relationship of protein calorie malnutrition to alcoholic liver disease: a reexamination of data from two Veterans Administration Cooperative Studies. Alcohol Clin Exp Res. 1995;19:635–641. doi: 10.1111/j.1530-0277.1995.tb01560.x. [DOI] [PubMed] [Google Scholar]
- 116.Fialla AD, Israelsen M, Hamberg O, Krag A, Gluud LL. Nutritional therapy in cirrhosis or alcoholic hepatitis: a systematic review and meta-analysis. Liver Int. 2015;35:2072–2078. doi: 10.1111/liv.12798. [DOI] [PubMed] [Google Scholar]
- 117.Moreno C, Deltenre P, Senterre C, et al. Intensive enteral nutrition is ineffective for patients with severe alcoholic hepatitis treated with corticosteroids. Gastroenterology. 2016;150:903–910. doi: 10.1053/j.gastro.2015.12.038. [DOI] [PubMed] [Google Scholar]
- 118.Floersheim GL. Treatment of human amatoxin mushroom poisoning: myths and advances in therapy. Med Toxicol. 1987;2:1–9. doi: 10.1007/BF03259857. [DOI] [PubMed] [Google Scholar]
- 119.Ferenci P, Dragosics B, Dittrich H, et al. Randomized controlled trial of silymarin treatment in patients with cirrhosis of the liver. J Hepatol. 1989;9:105–113. doi: 10.1016/0168-8278(89)90083-4. [DOI] [PubMed] [Google Scholar]
- 120.Parés A, Planas R, Torres M, et al. Effects of silymarin in alcoholic patients with cirrhosis of the liver: results of a controlled, double-blind, randomized and multicenter trial. J Hepatol. 1998;28:615–621. doi: 10.1016/S0168-8278(98)80285-7. [DOI] [PubMed] [Google Scholar]
- 121.Rambaldi A, Jacobs BP, Iaquinto G, Gluud C. Milk thistle for alcoholic and/or hepatitis B or C liver diseases: a systematic cochrane hepatobiliary group review with meta-analyses of randomized clinical trials. Am J Gastroenterol. 2005;100:2583–2591. doi: 10.1111/j.1572-0241.2005.00262.x. [DOI] [PubMed] [Google Scholar]
- 122.Rambaldi A, Gluud C. Propylthiouracil for alcoholic liver disease. Cochrane Database Syst Rev. 2002;(2):CD002800. doi: 10.1002/14651858.CD002800. [DOI] [PubMed] [Google Scholar]
- 123.Rambaldi A, Gluud C. Colchicine for alcoholic and non-alcoholic liver fibrosis and cirrhosis. Cochrane Database Syst Rev. 2005;(2):CD002148. doi: 10.1002/14651858.CD002148.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Rambaldi A, Gluud C. S-adenosyl-L-methionine for alcoholic liver diseases. Cochrane Database Syst Rev. 2006;(2):CD002235. doi: 10.1002/14651858.CD002235.pub2. [DOI] [PubMed] [Google Scholar]
- 125.Lieber CS, Weiss DG, Groszmann R, Paronetto F, Schenker S Veterans Affairs Cooperative Study 391 Group. II. Veterans Affairs Cooperative Study of polyenylphosphatidylcholine in alcoholic liver disease. Alcohol Clin Exp Res. 2003;27:1765–1772. doi: 10.1097/01.ALC.0000093743.03049.80. [DOI] [PubMed] [Google Scholar]
- 126.Stickel F, Seitz HK. Update on the management of alcoholic steatohepatitis. J Gastrointestin Liver Dis. 2013;22:189–197. [PubMed] [Google Scholar]
- 127.Mathurin P, O’Grady J, Carithers RL, et al. Corticosteroids improve short-term survival in patients with severe alcoholic hepatitis: meta-analysis of individual patient data. Gut. 2011;60:255–260. doi: 10.1136/gut.2010.224097. [DOI] [PubMed] [Google Scholar]
- 128.Parker R, Armstrong MJ, Corbett C, Rowe IA, Houlihan DD. Systematic review: pentoxifylline for the treatment of severe alcoholic hepatitis. Aliment Pharmacol Ther. 2013;37:845–854. doi: 10.1111/apt.12279. [DOI] [PubMed] [Google Scholar]
- 129.Thursz MR, Richardson P, Allison M, et al. Prednisolone or pentoxifylline for alcoholic hepatitis. N Engl J Med. 2015;372:1619–1628. doi: 10.1056/NEJMoa1412278. [DOI] [PubMed] [Google Scholar]
- 130.Mathurin P, Louvet A, Duhamel A, et al. Prednisolone with vs without pentoxifylline and survival of patients with severe alcoholic hepatitis: a randomized clinical trial. JAMA. 2013;310:1033–1041. doi: 10.1001/jama.2013.276300. [DOI] [PubMed] [Google Scholar]
- 131.Harrison PM, Wendon JA, Gimson AE, Alexander GJ, Williams R. Improvement by acetylcysteine of hemodynamics and oxygen transport in fulminant hepatic failure. N Engl J Med. 1991;324:1852–1857. doi: 10.1056/NEJM199106273242604. [DOI] [PubMed] [Google Scholar]
- 132.Lee WM, Hynan LS, Rossaro L, et al. Intravenous N-acetylcysteine improves transplant-free survival in early stage non-acetaminophen acute liver failure. Gastroenterology. 2009;137:856–864.e1. doi: 10.1053/j.gastro.2009.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Nguyen-Khac E, Thevenot T, Piquet MA, et al. Glucocorticoids plus N-acetylcysteine in severe alcoholic hepatitis. N Engl J Med. 2011;365:1781–1789. doi: 10.1056/NEJMoa1101214. [DOI] [PubMed] [Google Scholar]
- 134.Singal AK, Guturu P, Hmoud B, Kuo YF, Salameh H, Wiesner RH. Evolving frequency and outcomes of liver transplantation based on etiology of liver disease. Transplantation. 2013;95:755–760. doi: 10.1097/TP.0b013e31827afb3a. [DOI] [PubMed] [Google Scholar]
- 135.Singal AK, Hmoud BS, Guturu P, Kuo YF. Outcome after liver transplantation for cirrhosis due to alcohol and hepatitis C: comparison to alcoholic cirrhosis and hepatitis C cirrhosis. J Clin Gastroenterol. 2013;47:727–733. doi: 10.1097/MCG.0b013e318294148d. [DOI] [PubMed] [Google Scholar]
- 136.DiMartini A, Day N, Dew MA, et al. Alcohol consumption patterns and predictors of use following liver transplantation for alcoholic liver disease. Liver Transpl. 2006;12:813–820. doi: 10.1002/lt.20688. [DOI] [PubMed] [Google Scholar]
- 137.Neuberger J. Public and professional attitudes to transplanting alcoholic patients. Liver Transpl. 2007;13(11 Suppl 2):S65–S68. doi: 10.1002/lt.21337. [DOI] [PubMed] [Google Scholar]
- 138.Mathurin P, Moreno C, Samuel D, et al. Early liver transplantation for severe alcoholic hepatitis. N Engl J Med. 2011;365:1790–1800. doi: 10.1056/NEJMoa1105703. [DOI] [PubMed] [Google Scholar]
- 139.Im GY, Kim-Schluger L, Shenoy A, et al. Early liver transplantation for severe alcoholic hepatitis in the United States: a single-center experience. Am J Transplant. 2016;16:841–849. doi: 10.1111/ajt.13586. [DOI] [PubMed] [Google Scholar]
- 140.Lucey MR. Liver transplantation for alcoholic liver disease. Nat Rev Gastroenterol Hepatol. 2014;11:300–307. doi: 10.1038/nrgastro.2013.247. [DOI] [PubMed] [Google Scholar]