Abstract
Background/Aims
Patients with active ulcerative colitis (UC) have elevated levels of activated myeloid-derived leukocytes as a source of inflammatory cytokines. The selective depletion of these leukocytes by adsorptive granulocyte/monocyte apheresis (GMA) with an Adacolumn should alleviate inflammation, promote remission and enhance drug efficacy. However, studies have reported contrasting efficacy outcomes based on patients’ baseline demographic variables. This study was undertaken to understand the demographic features of GMA responders and nonresponders.
Methods
This was a multicenter study in China involving four institutions and 34 patients with active UC. Baseline conventional medications were continued without changing the dosage. The treatment efficacy was evaluated based on the endoscopic activity index and the Mayo score.
Results
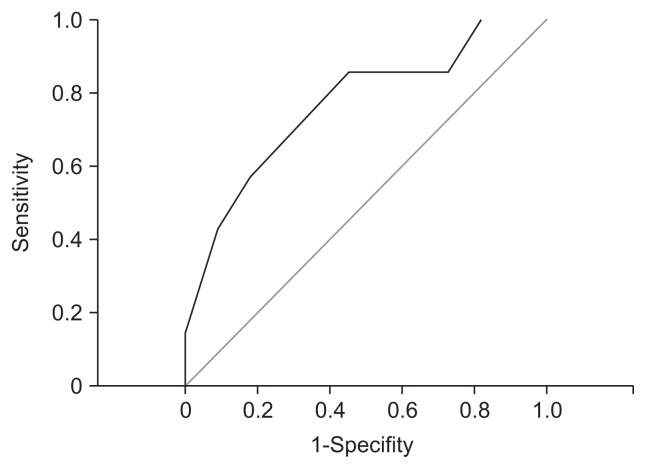
Thirty of the 34 patients completed all 10 GMA treatment sessions. The overall efficacy rate was 70.59%. The receiver operating characteristic analysis showed that the area under the curve was approximately 0.766 for a Mayo score of ≤5.5 with 0.273 specificity and 0.857 sensitivity (Youden index, 0.584) for GMA responders. No GMA-related serious adverse events were observed.
Conclusions
The overall efficacy of GMA in patients with active UC who were taking first-line medications or were corticosteroid refractory was encouraging. Additionally, GMA was well tolerated and had a good safety profile.
Keywords: Colitis, ulcerative; Mayo score; Myeloid lineage leucocytes; Adsorptive granulocyte/monocyte apheresis; Receiver operating characteristic curve
INTRODUCTION
Ulcerative colitis (UC) is a chronic relapsing-remitting inflammatory bowel disease (IBD), which afflicts millions of individuals throughout the world with symptoms that impair performance and quality of life. The etiopathogenesis of IBD is not fully understood at present, but immune-related mechanisms are responsible for the observed dysregulated immune responses against intraluminal antigens in genetically susceptible individuals.1,2 Further, the current treatment of IBD with anti-inflammatory drugs, including steroids, and immunosuppressants is inadequate for achieving a sustainable disease remission. Additionally, the chronic administration of these medications is associated with serious side effects as treatment-related morbidity factors. However, in drug refractory cases with active disease, surgical intervention is often applied to remove the affected segment of the large intestine. Therefore, an effective and safe treatment option is desirable.
In recent years, selective depletion of myeloid lineage leucocytes by adsorptive granulocyte and monocyte apheresis (GMA) with an Adacolumn (JIMRO, Takasaki, Japan) has been introduced as a nonpharmacologic treatment strategy in patients with IBD. GMA is aimed at reducing the elevated and activated leucocytes known to be sources of inflammatory cytokines.1,3–21 In most hitherto studies, the efficacy outcomes have been promising. In China, GMA with the Adacolumn for the treatment of patients with IBD was officially approved for the treatment of patients with IBD in 2013.
Will GMA become an effective and safe alternative therapeutic option to conventional medications in China, and the rest of the world? In line with this thinking, we undertook a multi-center observational study to better understand the therapeutic potential of GMA in a Chinese population of patients with active UC. An observational study protocol was compiled with a 12-month follow-up involving four independent gastroenterology units.
Further, to improve the cost effectiveness of GMA, we aimed to identify markers of clinical responses to GMA. In fact, even in Japan, it has been difficult to select the right patients for therapeutic GMA due to a lack of established biomarkers or other demographic variables to measure the clinical response to this nonpharmacologic treatment option.
MATERIALS AND METHODS
1. Study design and objectives
This retrospective multicenter study in China aimed at identifying disease background features, which potentially mark a UC patient as either a responder or nonresponder to GMA. Four independent IBD units actively participated in this study. The eligible patients had been treated with GMA between April 2012 and September 2013 at the four centers.
Prior to the initiation of GMA therapy, from our database, we selected patients with inadequate efficacy response to 5-aminosalicylic acid (5-ASA) or patients who had active UC refractory to prednisolone and were 18 to 60 years of age, with a Mayo score 2 to 10, and endoscopy score 1 or 2 (0, inactive disease; 1, mild; 2, moderate; 3, severe). The extent of disease was limited to the left colon or total colitis.
The study patients had to have good vascular condition to receive an indwelling catheter of 18 to 20 gauge size to achieve blood access and flow during GMA. Exclusion criteria included recent (within 6 weeks) use of azathioprine, 6-mercaptopurine, or infliximab, or deep ulcers and extensive loss of the mucosal tissue at the affected sites. ‘Refractory to prednisolone’ was defined as oral corticosteroid (30 to 40 mg/day) for at least 2 to 3 weeks or intravenous corticosteroid (1 to 1.5 mg/kg bodyweight/day) for at least 7 to 10 days.
In general, “corticosteroid refractory UC” meant patients who had active disease in spite of receiving prednisolone up to 0.75 mg/kg bodyweight per day for more than 4 weeks.
Likewise, “steroid-dependent UC” meant patients who were either unable to reduce steroids below 10 mg/day equivalent prednisolone within 3 months of starting corticosteroid without experiencing recurrence, or patients who had UC flare-up within 3 months of stopping corticosteroids.
2. GMA procedures
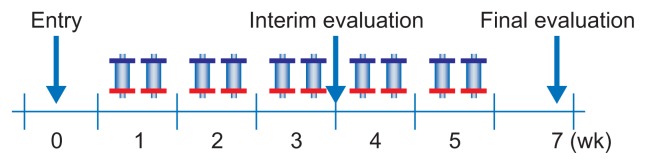
All patients received GMA therapy twice a week with the Adacolumn as previously described.12,17 The first patient evaluation was done after six GMA sessions. If patients showed no signs of improvement in their clinical symptoms, then they attended another four GMA sessions. Conventional medication was to be continued during the whole GMA treatment course, but without any change in the dosage (Fig. 1).
Fig. 1.
Study design for granulocyte/monocyte apheresis (GMA) treatment in patients with active ulcerative colitis. As shown, each patient was to receive up to 10 GMA sessions at a rate of two sessions per week. After six sessions, patients who improved received four additional GMA sessions. The final evaluation was done at week 7.
3. Evaluations of safety and efficacy
During the GMA treatment period, patients’ vital signs including heart rate, blood pressure, and the respiration rate were monitored. Long-term safety was evaluated by measuring albumin, alanine aminotransferase (ALT), aspartate aminotransferase (AST), total bilirubin (TBil), glutamate (GLU), creatinine (Cr), blood urea nitrogen (BUN), hemoglobin (Hb), red blood cell count (RBC), white blood cell count (WBC), platelets (PLT), and erythrocyte sedimentation rate (ESR) levels. For these measurements, routine blood samples were taken at entry, after GMA treatment, and at regular intervals during the observation period.
The clinical measurements included data on ALT, AST, TBil, GLU, Cr, BUN, Hb, RBC, WBC, PLT, ESR, C-reactive protein (CRP), and colonoscopy. The primary efficacy measures included endoscopic activity index (EAI) according to Naganuma et al.,22 or the Mayo score.23,24 The included patients were assessed at entry and after treatment according to the following calculation: (pretreatment score–posttreatment score)/pretreatment score×100%=efficacy level. Similar results for the two assessment methods were obtained after applying this calculation.22–24
A reduction of 90% to 100% in the EAI score or the Mayo score was defined as “remission”; 70% to 89% decrease in symptoms was defined as “significant efficacy”; 30% to 69% was defined as “effective”; and <30% was defined as “no response.” “Total efficacy” was the sum of remission, significant efficacy, and effective fractions.
On the basis of the Mayo scoring system, “clinical response” was defined as a decrease from baseline in the total Mayo score of at least 3 points (and 30%), with an accompanying decrease in the subscore for rectal bleeding of at least 1 point, or absolute subscore for rectal bleeding of 0 or 1. Further, “clinical remission” was defined as total Mayo score of 2 points or lower, with no individual subscore exceeding 1. Likewise, “mucosal healing” was defined as the absolute subscore for endoscopy (0 or 1).
4. Ethical considerations
As stated above, in China, GMA with the Adacolumn is an officially approved therapeutic option for patients with active IBD. Additionally, informed consent was obtained from all patients after explaining to them the study aim and the nature of the procedures involved. Further, adherence was made to the Principle of Good Clinical Practice and the Helsinki Declaration at all times.
5. Statistics
When appropriate, numerical data are presented as mean±standard deviation values. Comparison of demographic variables between the remission and the nonremission groups was done by using either the Mann-Whitney U-test or Fisher exact test. Multiple logistic regressions were applied to determine markers of response to GMA (Dr SSAPII for Windows).
To determine predictive factors that were closely associated with the response to GMA, we used receiver operating characteristic (ROC) curves with area under the curve (AUC). The ROC curves for the predictive factors were plotted by using SPSS for Windows statistical software version PASW Statistics 24 (SPSS Inc., Chicago, IL, USA). The AUC was calculated, and the point with the largest AUC was defined as the point having the greatest association with the response to GMA.
The best cutoff values for the predictive factors had to have a minimum distance from the upper-left corner to the point on the ROC curve, and were distinguishable between the remission and the non-remission groups. A p-value <0.05 was considered statistically significant. When appropriate, we applied the paired t-test for ALT, AST, TBil, GLU, Cr, BUN, Hb, RBC, WBC, and PLT.
RESULTS
1. Baseline demographic variables
Thirty-four patients with active UC received 10 consecutive GMA treatment sessions (two sessions per week) as shown in Fig. 1. The patients’ main demographic variables are presented in Table 1. Among the 34 patients, 19 were male and 15 were female, and the average age was 41.42±13.03 years, all with a definitive diagnosis of UC. One patient’s Mayo score was 2, however, that patient fulfilled the relevant clinical features of UC according to the other diagnosis (including endoscopic activity) so he was not excluded from this study. The 34 patients’ conditions and treatment methods reflected various clinical features (Table 1).
Table 1.
Baseline Demographic Variables of the 34 Patients with Ulcerative Colitis Who Were Included in This Study
| Demographic | Value |
|---|---|
| Age, yr | 41.42±13.03 |
| Male:female | 19:15 |
| Height, cm | 167.00±7.99 |
| Body weight, kg | 36.50±9.87 |
| Duration of UC, mo | 51.45±40.28 |
| Endoscopic activity index | 7.97±2.71 |
| Mayo score | 6.74±2.09 |
| Location of lesions | |
| Entire colon | 16 |
| Rectum and sigmoid colon | 5 |
| Left colon | 13 |
| Clinical course | |
| First onset | 3 |
| Chronic | 31 |
| UC severity level | |
| Mild | 5 |
| Moderate | 21 |
| Severe | 8 |
| Medications | |
| First episode | 3 |
| Oral 5-ASA or sulphasalazine | 11 |
| Corticosteroid, oral or intravenous | 3 |
| Oral 5-ASA or sulphasalazine+oral or intravenous steroid | 7 |
| Oral 5-ASA or sulphasalazine oral or intravenous steroid+topical 5-ASA | 2 |
| Oral 5-ASA or sulphasalazine+enema and oral or intravenous steroid | 1 |
| Oral 5-ASA or sulphasalazine+5-ASA enema | 5 |
| Enema and oral or intravenous steroid | 1 |
| Other | 1 |
Data are presented as mean±SD or number. UC, ulcerative colitis; 5-ASA, 5-aminosalicylic acid.
2. Clinical efficacy outcomes after 10 GMA sessions
Among the 34 patients included in this study, four were excluded because of ineligibility so they did not complete the procedure as stated in the safety section. The remaining 30 patients completed all 10 GMA treatment sessions according to the study’s intention. The clinical efficacy was evaluated based on the EAI and Mayo scores. According to the EAI score, there were four cases in remission, nine significant efficacy cases, 11 effective cases, and six no-response cases (Table 2).
Table 2.
Assessment of Efficacy Based on the Endoscopic Activity Index Score after 10 Monocyte Apheresis Sessions
| Definition | No. of patients (%) |
|---|---|
| Remission | 4 (11.76) |
| Significant efficacy | 9 (26.47) |
| Effective | 11 (32.35) |
| No response | 6 (17.65) |
| Withdrew | 4 (11.76) |
| Total | 34 (100.00) |
The total efficacy rate by EAI was 70.59%. Likewise, according to the Mayo score, 16 patients had mucosal healing, 15 patients were in clinical remission, 24 were clinical response cases, and six were nonresponders (Table 3). The clinical response (according to the Mayo score) was 70.59% in this study.
Table 3.
Assessment of Efficacy Based on the Mayo Ulcerative Colitis Scores
| Definition | No. of patients (%) |
|---|---|
| Mucosal healing | 16 (47.06) |
| Clinical remission | 15 (44.12) |
| Clinical response | 24 (70.59) |
| No response | 6 (17.65) |
| Withdrew | 4 (11.76) |
The efficacy of granulocyte/monocyte apheresis (GMA) was based on changes in the endoscopic activity index and the Mayo score as evaluated at entry and after 10 GMA sessions.
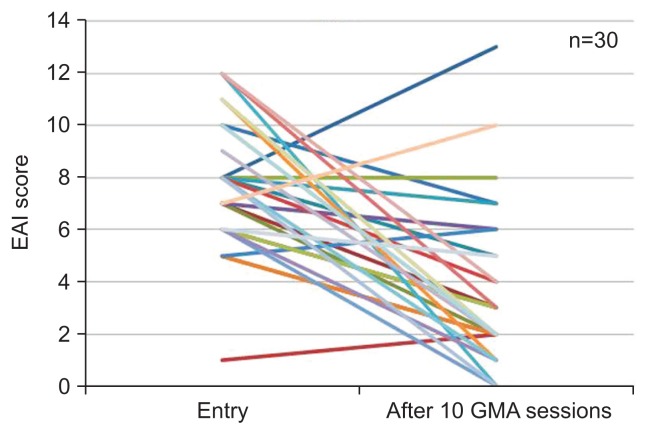
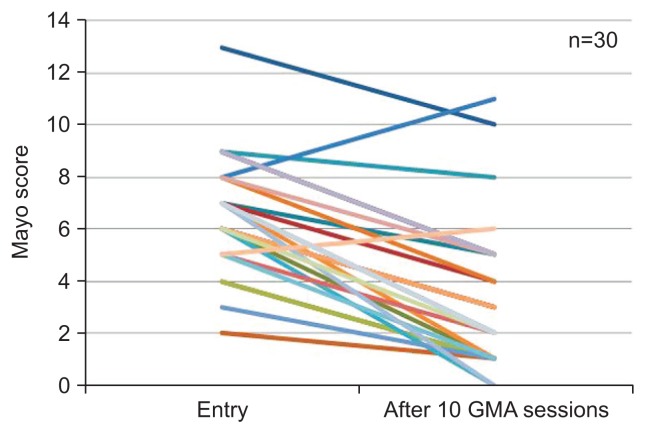
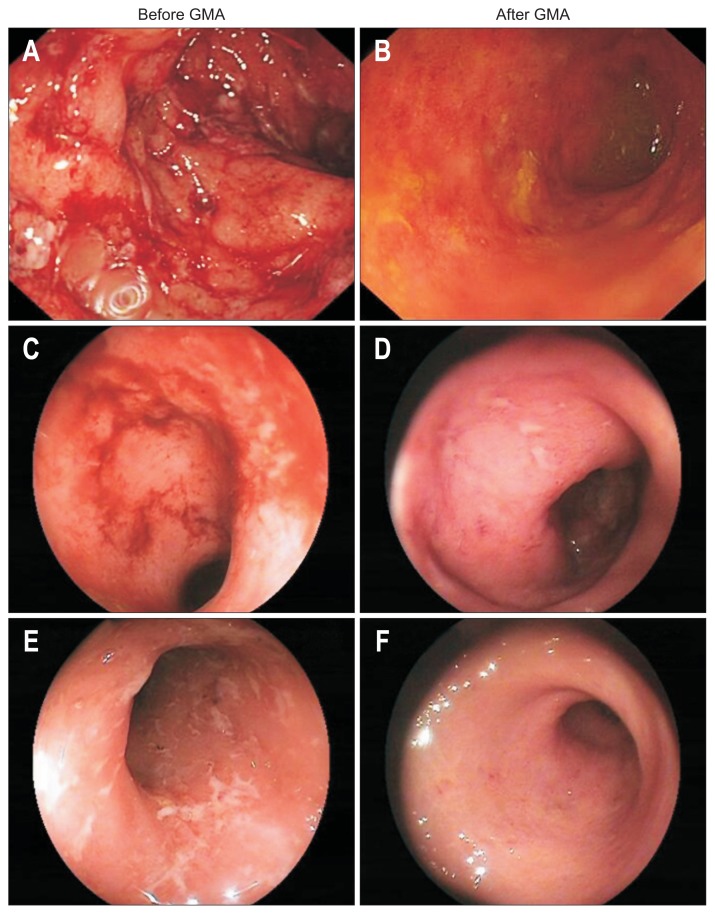
Figs 2 and 3 show the clinical efficacy outcomes (via line charts) based on Mayo scores before and after treatment. Both these figures show a decline in UC scores after treatment. Fig. 4 shows representative endoscopy findings before and after treatment. Additionally, Table 4 shows the EAI and the Mayo score subindex by paired t-test before and after GMA. Each subindex shows a statistically significant difference after treatment (p<0.05).
Fig. 2.
The endoscopic activity index (EAI) score of the patients before and after granulocyte/monocyte apheresis (GMA) therapy. The 30 colored lines represent the 30 patients who did not withdraw from the study, and the two endings on every line represent the EAI score before and after GMA therapy, respectively.
Fig. 3.
Mayo scores of the patients before and after granulocyte/monocyte apheresis (GMA) therapy. The 30 colored lines represent the 30 patients who did not withdraw from the study, and the two endings on every line represent the Mayo score before and after GMA therapy, respectively.
Fig. 4.
(A–F) Representative colonoscopic findings before and after 10 granulocyte/monocyte apheresis (GMA) sessions.
Table 4.
The Endoscopic Activity Index Scores and the Mayo Subscores before versus after Monocyte Apheresis Were Assessed Using Paired t-Tests
| Before entry | After entry | Before-after | p-value* | ||||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| Mean | SD | Mean | SD | Mean | SD | ||
| EAI score | |||||||
| Size of ulcers | 1.59 | 0.78 | 0.57 | 0.50 | 0.97 | 0.93 | 0.000 |
| Bleeding | 1.00 | 0.65 | 0.53 | 0.73 | 0.50 | 0.97 | 0.009 |
| Depth of ulcers | 1.15 | 0.50 | 0.50 | 0.73 | 0.70 | 0.79 | 0.000 |
| Mucosal oedema | 2.00 | 0.70 | 0.90 | 0.92 | 1.10 | 1.13 | 0.000 |
| Redness | 1.59 | 0.50 | 0.97 | 0.61 | 0.63 | 0.77 | 0.000 |
| Mucous exudate | 0.85 | 0.78 | 0.13 | 0.43 | 0.67 | 0.92 | 0.000 |
| Average EAI | 7.97 | 2.71 | 3.60 | 3.06 | 4.33 | 4.11 | 0.000 |
| Mayo UC score | |||||||
| Stool frequency | 2.38 | 1.30 | 1.23 | 1.10 | 0.97 | 0.81 | 0.000 |
| Endoscopic findings | 2.59 | 0.70 | 1.70 | 1.06 | 0.80 | 0.96 | 0.000 |
| Rectal bleeding | 1.62 | 0.89 | 0.90 | 0.88 | 0.73 | 0.74 | 0.000 |
| Physician’s global assessment | 1.79 | 1.04 | 0.80 | 1.03 | 0.83 | 0.75 | 0.000 |
| Average Mayo score | 6.74 | 2.09 | 3.30 | 2.74 | 3.33 | 2.02 | 0.000 |
EAI, endoscopic activity index; UC, ulcerative colitis.
p<0.05 indicates a statistically significant difference.
3. Predictive factors for response to GMA
Hitherto publications12,17 have reported that some patients show good response, while a minority subgroup do not respond well to GMA. To identify the relevant factors, we analyzed the difference between the “effective” and “poorly effective” (Table 5) subgroups. The patients in remission (or with significant efficacy and effectiveness) were included in the effective group; the patients with no-response were included in the poorly effective group. The poorly effective group contained six no-response patients and the other 24 patients were in the effective group.
Table 5.
Comparison (Univariate Analysis) of Patient Demographic Variables in the “Effective” and “Poorly Effective” (No Response) Subgroups
| Variable | Poorly effective group (n=6) | Effective group (n=24) | p-value |
|---|---|---|---|
| Age, yr | 36.72±15.33 | 43.36±12.56 | 0.26 |
| BMI, kg/m2 | 19.92±2.65 | 20.97±3.06 | 0.42 |
| HR, bpm | 87.57±10.10 | 79.59±9.20 | 0.06 |
| Course, mo | 45.34±43.49 | 54.72±39.80 | 0.60 |
| Combined daily dosage of steroid | 17.57±22.15 | 7.18±12.72 | 0.13 |
| Entry WBC, ×1000/μL | 8.52±2.92 | 7.10±2.52 | 0.22 |
| Entry Hb, g/L | 109.14±29.40 | 122.10±21.77 | 0.22 |
| Entry ALB, g/L | 36.50±5.07 | 40.02±9.77 | 0.50 |
| Entry ESR | 27.86±28.39 | 17.95±13.34 | 0.40 |
| Entry CRP, mg/L | 33.08±43.82 | 4.93±10.94 | 0.18 |
| Entry EAI | 7.29±1.11 | 8.05±2.87 | 0.32 |
| Entry Mayo score | 8.29±2.50 | 6.14±1.78 | 0.02* |
Data are presented as mean±SD.
bpm, beats per minute; BMI, body mass index; HR, heart rate; WBC, white blood cells; Hb, hemoglobin; ALB, albumin; ESR, erythrocyte sedimentation rate; CRP, C-reactive protein; EAI, endoscopic activity index.
p<0.05.
The results shown in Table 5 indicate that before the treatments there was no significant difference (between the two subgroups) in age, duration of UC, combined daily dosage of steroids, WBC, or CRP. Only the Mayo score revealed that there was a statistically significant difference between the two groups: the Mayo score in the effective group was significantly lower than that in the poorly effective group. Table 5 shows a comparison of patients’ demographic variables in the subgroups by univariate analysis.
To understand the significance of the Mayo score for response to GMA treatment, we applied the ROC approach (Fig. 5), and found that the area under the curve was approximately 0.766 (p=0.037; 95% CI, 0.553 to 0.979). We tried to find the best cutoff value, which could help us to better understand patient features, which potentially might identify GMA responders. One such value was found to be 6.5, with a specificity of 0.545, and sensitivity of 0.857 (Youden index 0.312). Using another measure it was found to be 5.5, with specificity above 0.273, and a sensitivity of 0.857 (Youden index 0.584).
Fig. 5.
Receiver operating characteristic curves for assessing the Mayo score before the first granulocyte/monocyte apheresis session in patients with active ulcerative colitis.
4. Safety
All adverse events in the 34 patients of this study were recorded. The most common side effects were transient migraine-like headache in three of 34 patients (8.82%). Only one patient withdrew due to unbearable treatment-related migraine-like headache; his headache remitted upon discontinuation of GMA treatment. In the remaining two patients, their headaches were very mild and both patients completed their 10 GMA sessions. One patient withdrew because her UC was very severe before entry and she received emergency colectomy. Another patient failed to attend after one GMA session. In addition there was one patient who developed spasmodic pain during treatment, which disappeared after cessation of treatment. Subsequently, he was diagnosed as having ischaemic bowel disease and he withdrew after one GMA session. However none of the GMA-related adverse events were considered serious.
There was no other serious adverse event or opportunistic infection during our observation period, even in patients who were on prednisolone during the course of GMA therapy. Among the 34 patients, there were three cases with poor vascular conditions. In these three cases we had to keep a deep venous catheter in position for GMA. They had no deep venous catheter-related complication such as infection or thrombosis. Likewise, liver and kidney function tests showed no significant change after GMA therapy.
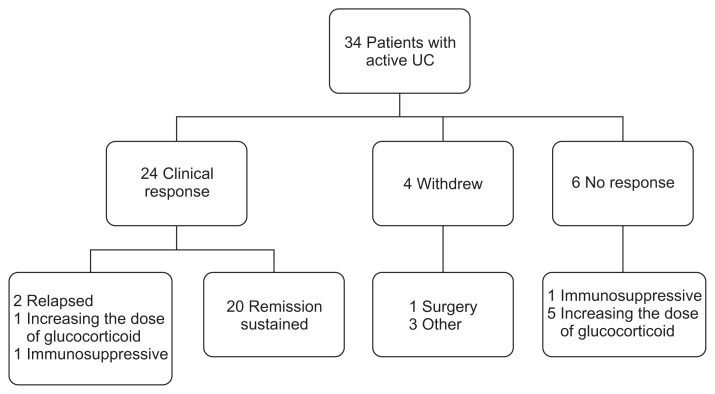
5. Follow-up
All patients were followed up for 8.87±1.42 months or longer after the final GMA session (Fig. 6). Up to 20 patients (60%) maintained the remission during the follow-up time. Figs 5 and 6 show the treatment of patients and summary of the clinical outcomes in this study.
Fig. 6.
Summary of treatments and the overall clinical outcomes.
UC, ulcerative colitis.
DISCUSSION
Historically, UC has been a relatively rare disease in China,25 but in recent years the incidence of this immune disorder has increased dramatically so it might reach the same level as countries in the European Union or in the United States.26
For patients who do not respond well to first-line salicylates or whose disease becomes refractory to corticosteroids, UC can be very debilitating. However, even those who respond to corticosteroids may develop adverse side effects, which add complexity to the disease symptoms. Further, the chronic nature of the disease means that patients need lifelong medications and this may lead to refractoriness and an increase in the risk of drug-related adverse events. Accordingly, drug therapy by its very nature has serious limitations. For many years, colectomy has been considered as an option in drug refractory patients with active UC, but the vast majority of patients in China (and perhaps other parts of the world) are reluctant to undergo colectomy or surgical resection of the UC lesions. Therefore, an effective new treatment is very much desired if we are to have good efficacy margins and low colectomy rates. GMA, if effective, should be an ideal alternative to pharmacological treatments because of its good safety profile as well as for being a nonpharmacologic treatment option.
Our study is the first that has investigated the efficacy and safety of GMA therapy in patients with UC in a Chinese IBD population setting. The 34 included patients had been treated with GMA and were reviewed in a retrospective setting. With regard to the efficacy outcomes, an overall efficacy rate of 70.59%—in patients who had failed to respond well to first-line medications or who had active UC refractory to corticosteroids—was very encouraging. This is like saying GMA was an opportunity for our patients to be spared from additional pharmacological treatments, which have potential safety concerns. Further, most patients included in this study were young adults. This means significant improvement in the quality-of-life and a decrease in the risk of side effects if these young patients had opted for an alternative drug-based therapy.16 Likewise, this nonpharmacologic treatment strategy should be promising for specific populations such as pediatric and adolescent patients with IBD,5,16 pregnant cases, fertility treatment patients,14 and patients with cytomegalovirus27 or hepatitis B virus infections.28
Regarding the safety of GMA, our findings showed that the most common side effect was transient migraine-like headache. The rate (8.82%) is much lower than the incidence seen in most patients on corticosteroids.3 Additionally, we found that common biochemical markers, including liver and kidney functions, were not affected by GMA. During follow-up, we found that GMA nonresponder patients could continue to opt for conventional medications including immunosuppressive therapy. Therefore, our experience suggested that GMA therapy can be a safe choice for patients with active UC who wish to avoid pharmacological treatments.
In this study, we were also interested in finding patient demographic variables, which potentially could identify responders and nonresponders to GMA. In the 2010 Japanese active UC treatment guidelines, specific recommendations include prednisone at 30 to 40 mg/day or higher doses in patients with severe UC. The combined use of GMA can add safety and potentially be more effective for maintaining or reducing the amount of corticosteroids, which is the recommendation level A (Ib).
For the initial treatment of moderate-to-severe UC patients, GMA and corticosteroids should be equally effective (recommendation level B [IIa]). However, GMA is often applied to treat patients with drug refractory UC or those who show inadequate response to conventional medications (recommendation level I [V]). We found that the Mayo score ≤5.5 may be an easier approach to select potential responder patients for GMA. However, this conclusion warrants further investigation in a larger cohort of patients with active UC, together with a longer follow-up observation time.
Our study also found specific limitations with GMA therapy: it being relatively expensive (currently not covered by health insurance in China), requiring good vascular conditions for blood access, and needing time to show efficacy. Tominaga et al.3 undertook a comprehensive assessment of cost, efficacy, and safety for GMA vs prednisolone, a commonly used corticosteroid. They found that the average medical cost per patient was €12,739.4 for GMA and €8,751.3 for prednisolone (p<0.05). However, GMA had an overwhelmingly better safety profile (p<0.001). The authors stated that this negative (higher cost for GMA) is reduced by its good safety profile as a nonpharmacologic intervention.
As already stated, we were interested in better understanding the predictive factors of the clinical response to GMA in patients with UC. With this in mind, we looked at the clinical response and patients’ demographic variables, although our analysis was limited by the small sample size (30 patients) in this study. Thus in the future we hope to continue our investigations in a larger cohort of patients in China. In clinical settings, knowing the baseline demographic variables (which potentially identifies a patient as a responder, or otherwise as a nonresponder to GMA) should help to avoid futile use of medical resources and to reduce morbidity in many patients.
The best responders to GMA appear to be first-episode cases29,30 followed by steroid-naïve patients.17,31 Recently, Yokoyama et al.12 looked for predictive factors of clinical response to GMA.12,32 In their first investigation, the authors reported that patients with a lesser duration of UC (and a low cumulative corticosteroid dose in the past) responded well to GMA. However, the best responders in that study were patients who received GMA immediately after a clinical relapse.12 Additionally, GMA was effective in patients with low WBCs at the first treatment session.32
In their second study, Yokoyama et al.32 found a significant fall in myeloid leucocytes and PLT in responders versus nonresponders to GMA. Further, baseline clinical activity index was lower in the remission group versus nonremission. After 12 months, 52 of 134 patients had maintained remission.32 Disease duration was longer in the relapsed group versus the maintained remission group.32
This study also reported that first UC episode and corticosteroid responder features, together with drug-naïvity, were significant factors for a favorable response to GMA, whereas corticosteroid-dependent UC was associated with early relapse in those who had achieved remission.32
Patients in whom colonoscopy reveals deep ulcers and extensive loss of the mucosal tissue, together with those who have a long history of exposure to multiple pharmacologics to which the disease has become refractory, may not benefit from GMA.33–35 However, it is very important and clinically relevant to indicate here that with pharmacologic treatment, in particular, corticosteroids given to patients when they first develop IBD can lead to a complicated disease course in the long term. In line with these assertions, Yamamoto et al.36 found that patients who received Adacolumn GMA in the early days of their active UC had a more favorable long-term clinical course by avoiding corticosteroids and other pharmacological treatments at an early stage of their IBD.
Currently, GMA’s long-term efficacy is unknown. For how long the responder patients will maintain in clinical remission requires a longer follow-up time. Likewise, the exact mechanism for the clinical efficacy of GMA has been reviewed by Inoue et al.10 but additional work can strengthen the current knowledge on the mode of actions of GMA in patients with UC. It is unlikely that removal of a fraction of myeloid lineage leucocytes per se can account for the observed clinical efficacy. The column outflow blood which returns to patients is where one could look for substance with potential therapeutic effect.29
In conclusion, this retrospective investigation showed an overall efficacy rate of 70.59% for GMA in patients with active UC and on first-line medications or active UC refractory to corticosteroids. Additionally, GMA was well-tolerated, and with a good patient compliance and safety profile. The entry Mayo score should identify patients who are likely to respond well to GMA, and the mean Mayo score in the poorly effective group was higher than those in the effective group in this study.
We thought that UC patients with relatively lower Mayo score at entry were more likely to respond well to GMA compared with patients with a higher Mayo score. After the multiple logistic regression analysis, we found the best cutoff value which might indicate “good GMA responder.” According to the clinical setting, we thought that a Mayo score value of ≤5.5 might indicate a good GMA responder.
Future studies should focus on the long-term efficacy of GMA and its impact on the dysregulated immune profile in patients with IBD. It is unlikely that removal of a fraction of myeloid lineage leucocytes per se can account for the observed clinical efficacy. The column outflow blood which returns to patients is where one could look for substance with potential therapeutic effect.
ACKNOWLEDGEMENTS
This study was supported in part by JIMRO (Takasaki, Japan).
Footnotes
See editorial on page 171.
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Conrad K, Roggenbuck D, Laass MW. Diagnosis and classification of ulcerative colitis. Autoimmun Rev. 2014;13:463–466. doi: 10.1016/j.autrev.2014.01.028. [DOI] [PubMed] [Google Scholar]
- 2.Podolsky DK. Inflammatory bowel disease. N Engl J Med. 2002;347:417–429. doi: 10.1056/NEJMra020831. [DOI] [PubMed] [Google Scholar]
- 3.Tominaga K, Nakano M, Hoshino M, Kanke K, Hiraishi H. Efficacy, safety and cost analyses in ulcerative colitis patients undergoing granulocyte and monocyte adsorption or receiving prednisolone. BMC Gastroenterol. 2013;13:41. doi: 10.1186/1471-230X-13-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fukunaga K, Yokoyama Y, Kamokozuru K, et al. Adsorptive granulocyte/monocyte apheresis for the maintenance of remission in patients with ulcerative colitis: a prospective randomized, double blind, sham-controlled clinical trial. Gut Liver. 2012;6:427–433. doi: 10.5009/gnl.2012.6.4.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tomomasa T, Tajiri H, Kagimoto S, et al. Leukocytapheresis in pediatric patients with ulcerative colitis. J Pediatr Gastroenterol Nutr. 2011;53:34–39. doi: 10.1097/MPG.0b013e31821058bc. [DOI] [PubMed] [Google Scholar]
- 6.Yamamoto T, Umegae S, Matsumoto K. Daily granulocyte and monocyte adsorptive apheresis in patients with active ulcerative colitis: a prospective safety and feasibility study. J Gastroenterol. 2011;46:1003–1009. doi: 10.1007/s00535-011-0428-4. [DOI] [PubMed] [Google Scholar]
- 7.Sakuraba A, Sato T, Morohoshi Y, et al. Intermittent granulocyte and monocyte apheresis versus mercaptopurine for maintaining remission of ulcerative colitis: a pilot study. Ther Apher Dial. 2012;16:213–218. doi: 10.1111/j.1744-9987.2012.01064.x. [DOI] [PubMed] [Google Scholar]
- 8.Okuyama Y, Andoh A, Nishishita M, et al. Multicenter prospective study for clinical and endoscopic efficacies of leukocytapheresis therapy in patients with ulcerative colitis. Scand J Gastroenterol. 2013;48:412–418. doi: 10.3109/00365521.2012.763175. [DOI] [PubMed] [Google Scholar]
- 9.Saniabadi AR, Hanai H, Suzuki Y, et al. Adacolumn for selective leukocytapheresis as a non-pharmacological treatment for patients with disorders of the immune system: an adjunct or an alternative to drug therapy? J Clin Apher. 2005;20:171–184. doi: 10.1002/jca.20046. [DOI] [PubMed] [Google Scholar]
- 10.Inoue T, Murano M, Narabayashi K, et al. The efficacy of oral tacrolimus in patients with moderate/severe ulcerative colitis not receiving concomitant corticosteroid therapy. Intern Med. 2013;52:15–20. doi: 10.2169/internalmedicine.52.8555. [DOI] [PubMed] [Google Scholar]
- 11.Sakata Y, Iwakiri R, Amemori S, et al. Comparison of the efficacy of granulocyte and monocyte/macrophage adsorptive apheresis and leukocytapheresis in active ulcerative colitis patients: a prospective randomized study. Eur J Gastroenterol Hepatol. 2008;20:629–633. doi: 10.1097/MEG.0b013e3282f5e9a4. [DOI] [PubMed] [Google Scholar]
- 12.Yokoyama Y, Kawai M, Fukunaga K, et al. Looking for predictive factors of clinical response to adsorptive granulocyte and monocyte apheresis in patients with ulcerative colitis: markers of response to GMA. BMC Gastroenterol. 2013;13:27. doi: 10.1186/1471-230X-13-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Passalacqua S, Ferraro PM, Bresci G, et al. The Italian Registry of Therapeutic Apheresis: granulocyte-monocyte apheresis in the treatment of inflammatory bowel disease. A multicentric study. J Clin Apher. 2011;26:332–337. doi: 10.1002/jca.20315. [DOI] [PubMed] [Google Scholar]
- 14.Takahashi H, Sugawara K, Sugimura M, et al. Flare up of ulcerative colitis during pregnancy treated by adsorptive granulocyte and monocyte apheresis: therapeutic outcomes in three pregnant patients. Arch Gynecol Obstet. 2013;288:341–347. doi: 10.1007/s00404-013-2748-5. [DOI] [PubMed] [Google Scholar]
- 15.Rosenberg L, Lawlor GO, Zenlea T, et al. Predictors of endoscopic inflammation in patients with ulcerative colitis in clinical remission. Inflamm Bowel Dis. 2013;19:779–784. doi: 10.1097/MIB.0b013e3182802b0e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tanaka T, Sugiyama S, Goishi H, Kajihara T, Akagi M, Miura T. Treatment of children and adolescents with ulcerative colitis by adsorptive depletion of myeloid lineage leucocytes as monotherapy or in combination with low dose prednisolone after failure of first-line medications. BMC Gastroenterol. 2013;13:130. doi: 10.1186/1471-230X-13-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Suzuki Y, Yoshimura N, Saniabadi AR, Saito Y. Selective granulocyte and monocyte adsorptive apheresis as a first-line treatment for steroid naïve patients with active ulcerative colitis: a prospective uncontrolled study. Dig Dis Sci. 2004;49:565–571. doi: 10.1023/B:DDAS.0000026299.43792.ae. [DOI] [PubMed] [Google Scholar]
- 18.Noguchi A, Watanabe K, Narumi S, et al. The production of interferon-gamma-inducible protein 10 by granulocytes and monocytes is associated with ulcerative colitis disease activity. J Gastroenterol. 2007;42:947–956. doi: 10.1007/s00535-007-2118-9. [DOI] [PubMed] [Google Scholar]
- 19.Isomoto H, Uehara R, Hayashi T, et al. Magnifying endoscopic findings can predict clinical outcome during long-term follow-up of more than 12 months in patients with ulcerative colitis. Gastroenterol Res Pract. 2013;2013:671576. doi: 10.1155/2013/671576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yoshida A, Kobayashi K, Ueno F, et al. Possible role of early transabdominal ultrasound in patients undergoing cytapheresis for active ulcerative colitis. Intern Med. 2011;50:11–15. doi: 10.2169/internalmedicine.50.4135. [DOI] [PubMed] [Google Scholar]
- 21.Cabriada JL, Domènech E, Ibargoyen N, et al. Leukocytapheresis for steroid-dependent ulcerative colitis in clinical practice: results of a nationwide Spanish registry. J Gastroenterol. 2012;47:359–365. doi: 10.1007/s00535-011-0499-2. [DOI] [PubMed] [Google Scholar]
- 22.Naganuma M, Ichikawa H, Inoue N, et al. Novel endoscopic activity index is useful for choosing treatment in severe active ulcerative colitis patients. J Gastroenterol. 2010;45:936–943. doi: 10.1007/s00535-010-0244-2. [DOI] [PubMed] [Google Scholar]
- 23.Rutgeerts P, Sandborn WJ, Feagan BG, et al. Infliximab for induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2005;353:2462–2476. doi: 10.1056/NEJMoa050516. [DOI] [PubMed] [Google Scholar]
- 24.Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis: a randomized study. N Engl J Med. 1987;317:1625–1629. doi: 10.1056/NEJM198712243172603. [DOI] [PubMed] [Google Scholar]
- 25.Hu PJ. The consensus for the diagnosis and treatment of inflammatory bowel disease. Chin J Dig. 2012;32:796–813. [Google Scholar]
- 26.Puri AS. Epidemiology of ulcerative colitis in South Asia. Intest Res. 2013;11:250–255. doi: 10.5217/ir.2013.11.4.250. [DOI] [Google Scholar]
- 27.Yoshino T, Nakase H, Matsuura M, et al. Effect and safety of granulocyte-monocyte adsorption apheresis for patients with ulcerative colitis positive for cytomegalovirus in comparison with immunosuppressants. Digestion. 2011;84:3–9. doi: 10.1159/000321911. [DOI] [PubMed] [Google Scholar]
- 28.Yokoyama Y, Fukunaga K, Kamikozuru K, et al. Crohn’s disease complicated by hepatitis B virus successfully treated with the use of adsorptive depletion of myeloid lineage leucocytes to suppress inflammatory cytokine profile. Cytotherapy. 2014;16:821–825. doi: 10.1016/j.jcyt.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 29.Saniabadi AR, Hanai H, Fukunaga K, et al. Therapeutic leukocytapheresis for inflammatory bowel disease. Transfus Apher Sci. 2007;37:191–200. doi: 10.1016/j.transci.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 30.Suzuki Y, Yoshimura N, Fukuda K, Shirai K, Saito Y, Saniabadi AR. A retrospective search for predictors of clinical response to selective granulocyte and monocyte apheresis in patients with ulcerative colitis. Dig Dis Sci. 2006;51:2031–2038. doi: 10.1007/s10620-006-9199-9. [DOI] [PubMed] [Google Scholar]
- 31.Tanaka T, Okanobu H, Yoshimi S, et al. In patients with ulcerative colitis, adsorptive depletion of granulocytes and monocytes impacts mucosal level of neutrophils and clinically is most effective in steroid naïve patients. Dig Liver Dis. 2008;40:731–736. doi: 10.1016/j.dld.2008.02.012. [DOI] [PubMed] [Google Scholar]
- 32.Yokoyama Y, Watanabe K, Ito H, et al. Factors associated with treatment outcome, and long-term prognosis of patients with ulcerative colitis undergoing selective depletion of myeloid lineage leucocytes: a prospective multicenter study. Cytotherapy. 2015;17:680–688. doi: 10.1016/j.jcyt.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 33.Saniabadi AR, Tanaka T, Ohmori T, Sawada K, Yamamoto T, Hanai H. Treating inflammatory bowel disease by adsorptive leucocytapheresis: a desire to treat without drugs. World J Gastroenterol. 2014;20:9699–9715. doi: 10.3748/wjg.v20.i29.9699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sacco R, Tanaka T, Yamamoto T, Bresci G, Saniabadi AR. Adacolumn leucocytapheresis for ulcerative colitis: clinical and endoscopic features of responders and unresponders. Expert Rev Gastroenterol Hepatol. 2015;9:327–333. doi: 10.1586/17474124.2014.953060. [DOI] [PubMed] [Google Scholar]
- 35.Sands BE, Sandborn WJ, Feagan B, et al. A randomized, double-blind, sham-controlled study of granulocyte/monocyte apheresis for active ulcerative colitis. Gastroenterology. 2008;135:400–409. doi: 10.1053/j.gastro.2008.04.023. [DOI] [PubMed] [Google Scholar]
- 36.Yamamoto T, Umegae S, Matsumoto K. Long-term clinical impact of early introduction of granulocyte and monocyte adsorptive apheresis in new onset, moderately active, extensive ulcerative colitis. J Crohns Colitis. 2012;6:750–755. doi: 10.1016/j.crohns.2011.12.009. [DOI] [PubMed] [Google Scholar]