Abstract
Background
Sleep in childhood and adolescence is crucial for mental and physical health; however several researches reported an increasing trend towards a sleep deprivation in this age. Due to the lack of recent epidemiological studies in Italy, the aim of our study was to depict sleep habits and patterns in Italian children aged 1–14 years and to evaluate their relationships with video devices use (TV, tablet, smartphone, PC) and evening/night child activities.
Methods
A structured interview was conducted during 2015 by 72 Family Pediatricians in 2030 healthy children aged 1–14 years by a cross-sectional survey named “Ci piace sognare”. Total sleep duration was calculated, 2015 National Sleep Foundation Recommendations were used as reference. Optimal sleepers were defined children sleeping in own bed all night without awakenings. Multivariable median regression was performed to identify predictors of sleep duration and multivariable logistic regression for predictors of optimal sleep.
Results
Total sleep duration and numbers of awakenings decreased with age. Only 66.9% of children had sleep duration in agreement with Recommendations (50% in 10–14 years group). Before sleeping 63.5% of children used video devices (39.6% at 1–3 years), 39.1% read, 27.5% drank and 19.5% ate. Bottle users at bedtime were 30.8% at 1–3 years, 16.6% at 3–5 years and 4.9% at 5–7 years. Overall, 23.4% of children changed sleeping place during the night, 22.4% referred sleeping problems in the first year of life.
Video devices use was negative predictor of sleep duration (-0.25 h [95%CI:-0.35,-0.14], p < 0.001). Optimal sleep was inversely related with bedroom TV (OR 0.63 [0.50,0.79], p < 0.001), with sleeping disorders in the first year (OR 0.62 [0.48,0.80], p < 0.001)), with bottle use (OR 0.64 [0.44,0.94], p < 0.05) and posivively related with high mother’s education level (OR 1.44 [1.11,1.88], p < 0.01).
Conclusions
About one third of 1 to 14 year Italian children sleep less than recommended, one half in teenage. Modifiable risk factors for sleep abnormalities such as video devices use, bedroom TV and bottle use should be target of preventive strategies for a correct sleep. Pediatricians should give priority to the identification of sleep disorders early in life.
Electronic supplementary material
The online version of this article (doi:10.1186/s13052-016-0324-x) contains supplementary material, which is available to authorized users.
Keywords: Sleep duration, Sleep recommendations, Sleep continuity, Video devices, Bottle use, Bedroom TV, Body Mass Index
Background
Sleep in childhood and adolescence is important for mental and physical health, as assessed by various papers in the last decade. Researches have shown that insufficient sleep is associated with obesity, metabolic risk, lower academic performance and emotional/behavior problems [1–4]. At the same time some studies have reported a reduction of sleep duration in pediatric ages [5, 6], thus suggesting to pediatricians the need for increasing their attention on this topic.
Empirical data demonstrated that several dimensions of sleep are related to health outcomes, and can be measured with self-report and objective methods, i.e., sleep duration, continuity and architecture [7]. Sleep duration and continuity (i.e., night awakenings) were the parameters more frequently studied in pediatric age.
Variables associated with short sleep duration in childhood have been proposed (latitude, cultural factors, late bedtime, etc.). In particular, a relationship between inadequate sleep and TV viewing and/or TV in the bedroom has been found by cross-sectional studies [8, 9]. Also more recent longitudinal studies showed a negative impact of daily TV viewing and use of other video devices (tablet, smartphone, PC) on sleep duration [10, 11]. TV viewing may directly displace bedtime or increase child emotional arousal and light exposure, all these mechanisms affecting sleep onset and duration [12]. However, few studies have investigated the impact of new devices (PC; tablet, smartphone, social network) on sleep quality.
Due to the lack of studies evaluating specifically all the evening activities at bedtime, aim of our study was to depict the sleep habits and the sleep patterns in a large national population of children aged 1–14 years and to evaluate their relationship with evening/night child activities.
Methods
Study design
Between April 2015 and November 2015 a cross sectional survey “Ci Piace Sognare” (CPS; literally: “We like dreaming”) was conducted among parents/caregivers of children aged 1 to 14 years referring to a group of Italian Family Paediatricians (FP) members of two Italian Pediatric Societies (Società Italiana di Pediatra Preventiva e Sociale and Società Italiana delle Cure Primarie Pediatriche).
The study was proposed in 2013 by the principal investigator (PB) to Scientific Board of the two Italian Pediatric Societies. A specific website was prepared for the puropse of the study.
Family pediatricians
The study was announced during the Annual Meetings of both Societies yield in 2014. The participation of FP to the study was voluntary. Interested FPs were asked to register on the study website at beginning of 2015.
Subjects
FPs were asked to enroll a maximum number of 2 children per day presenting in their office for a routine health visit and with the following characteristics: 1) age >1.0 and <14.0 years, 2) absence of any acute illness able to interfere with sleep. Children having parents with a poor command of the Italian language were excluded as well as children having any chronic disease able to interfere with sleep: celiac disease, diabetes, mucoviscidosis, cancer, chronic nephropathy, cardiopathy with hemodynamic impairment, syndrome with malformation, uncontrolled asthma, obstructive sleep apnea syndrome, neurological and neuropsychiatric disease (including autism and mental disability).
Study design
A written informed Consensus was achieved by FPs from at least one of parents of each participant. The study was approved by Ethical Committee of Azienda Ospedaliero Universitaria “Maggiore della Carita” of Novara on 2nd March 2015.
Structured interview
The structured interview was elaborated by the Working Group (by adapting other existing and validated questionnaires) [13, 14] and contains questions on:
child data (birth date, gender, actual weight and height)
family data (age, job and education level of both parents, number of family members living with the child, number of brothers/sisters).
sleep habits, pattern and bedtime/night environment during the last night (time of falling asleep and of waking up, night sleep duration, naps and duration of daytime sleep, mean number of awakenings per night, place of falling asleep and of sleeping for the most part of the night, dinner time, foods and/or drinks before sleeping and during the night, bottle use, use of video devices (TV; PC; tablet, smartphone, etc.) just before sleeping), child use of active or passive reading before sleeping, presence of TV or other screen in child’s bedroom, presence of sleep problems during the first year of life, use of product for sleeping in the past or at study time.
The structured interview was prepared as a specific form to be fulfilled online anonymously (closed format questions) on the website by previously registered and trained FPs in the presence of at least one parent, in a weekday (Tuesday to Friday) during the period from 1st April to 30 November 2015 (excluding school holidays and summertime).
A copy of the structured interview can be requested by mail to the corresponding author.
Sleep items during the last night
Time of falling asleep and of waking up were approximated to 15 min (i.e., 21.15; 21.30; 21.45; 22.00, etc.), as well as dining time. Nocturnal sleep and daytime sleep duration were registered. Total sleep duration was calculated as the sum of nocturnal plus daytime sleep. Adequacy of total sleep duration was assessed by comparison with age-specific recommendations [15].
The place where the child fall asleep as well as where he/she slept for the most part of the night was registered among these options: own bed, parental bed, other room, outside the house. The presence of an own room, eventually shared with brothers/sisters, was investigated.
Drinks or foods consumed in 30-min interval before falling asleep or during the night was considered. The use of a device before sleeping were considered when it happened in the 30-min period before falling asleep.
The presence of TV in the room where the child usually sleeps, reading (active or passive) before sleeping and the history of sleep problems during the first year of life were investigated by means of closed answers. The use of products for sleeping in the past or at study time was investigated by means of multiple choice answers.
Optimal sleepers
Children were classified as “optimal sleepers” if all the following conditions were present: 1) place of falling asleep: own bed; 2) place of sleeping: own bed, 3) no use of product for sleeping at study time; and 4) number of awakening equal to 0 (≤1 for children under 3 years of age). All other children were classified as “not optimal sleepers”.
Child data
Pediatricians measured child weight and height (length up to 2 years of age) in the same day in which the interview was administered, using standard anthropometric procedures [16].
Body Mass Index (BMI) was calculated as weight (kg)/height (m2). BMI-Standard Deviation Score (SDS) as well as birth weight-SDS were calculated according with World Health Organization (WHO) Reference Tables, overweight and obese children were defined according with WHO BMI percentiles [17].
Family data
Age, job and education level of both parents, number of family members living with the child, and number of brothers/sisters were investigated by means of closed format answers.
Statistical analysis
Most continuous variables were not Gaussian-distributed and all are reported as 50th percentile (median) and interquartile range (IQR) (25th and 75th percentiles). Discrete variables are reported as the number and percentage of subjects with the characteristic of interest. Descriptive data were reported by 5 age groups: 1 to <3, 3 to <5, 5 to <7, 7 to <10 and 10 to <14 years. Univariable median regression and univariable logostic regression were used to quantify the association of continuous and binary outcomes with the predictors of interest [18, 19]. The response variable of the median regression models was total sleep (hours) and that of the logistic regression models was optimal sleeper (0 = no, 1 = yes). Multivariable median regression was performed with the following prespecified predictors: 1) age (years), 2) BMI (SDS), 3) presence of TV in the bedroom, 4) use of display devices before sleeping, 5) drinking before sleeping. The multivariable logistic regression model had the following additional predictors: 6) high school or university degree of the mother, 7) personal room, 8) reading before sleep, 9) being only child, 10) mother working at home, 11) bottle use, and 12) sleep problems during the first year of life. Univariable and multivariable fractional polynomials were used to test whether the relationship between the response variable and the continuous predictors was linear [20]. All relationships were to be linear and were modelled as such. Multivariable quantile regression was used to estimate the 5th, 25th, 50th, 75th and 95th percentiles of total sleep by age and sex. Total sleep (hours) was used as the response variable and age (continuous, years) and sex (discrete: 0 = female; 1 = male) as predictors. Multivariable fractional polynomials of degree 2 were used to select transformations linearizing the sleep-age relationship [20]. Such transformations were age-1 for the 5th percentile, age^0.5 for the 25th, 50th and 95th percentiles, and loge(age) for the 75th percentile.
Statistical analysis was performed using Stata 14.1 (Stata Corporation, College Station, TX, USA).
Results
The Working Group verified at study start that the 3 Italian macro-regions (North, Centre, South) were represented according with the known distribution of children under 14 years living in the country [21]. A hundred and one FPs expressed their interest to participate to CPS Study and 72 of them (71%) collected data, for a total of 2030 children. The median [IQR] number of children enrolled by each FP was 32 (28, 50).
Children characteristics are summarized in Table 1, stratified in the 5 age groups. Only in 2 cases parents refused to participate.
Table 1.
Clinical characteristics of 2030 studied children according with age groups
| 1 to 3 years | 3 to 5 years | 5 to 7 years | 7 to 10 year | 10 to 14 years | All subjects | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | 523 | 429 | 425 | 355 | 298 | 2030 | ||||||||||||
| Males (%) | 50.9 | 49.7 | 49.4 | 51.8 | 51.7 | 50.6 | ||||||||||||
| N/C/S | 252/92/179 | 182/80/167 | 189/63/173 | 164/57/134 | 173/49/76 | 960/341/729 | ||||||||||||
| P50 | P25 | P75 | P50 | P25 | P75 | P50 | P25 | P75 | P50 | P25 | P75 | P50 | P25 | P75 | P50 | P25 | P75 | |
| Weight (kg) | 11.8 | 10.5 | 13.0 | 16.0 | 14.7 | 17.9 | 21.0 | 19.0 | 24.0 | 28.9 | 25.0 | 33.6 | 43.0 | 35.5 | 52.0 | 19.0 | 14.0 | 28.5 |
| BMI (kg/m) | 16.2 | 15.4 | 17.2 | 15.7 | 14.8 | 16.7 | 15.7 | 14.7 | 17.1 | 16.7 | 15.3 | 18.9 | 18.6 | 17.0 | 21.5 | 16.3 | 15.2 | 17.9 |
| BMI (SDS) | 0.27 | -0.43 | 0.98 | 0.28 | -0.39 | 0.98 | 0.29 | -0.40 | 1.11 | 0.44 | -0.34 | 1.42 | 0.53 | -0.34 | 1.36 | 0.32 | -0.39 | 1.12 |
1 to 3 years: from 1.0 to 2.99 years; 3 to 5 years: from 3.0 to 4.99 years (similarly for other age groups)
n number of children
N North, C Centre, S South
BMI Body Mass Index
SDS Standard Deviation Score
P50, P25 and P75 represent median, 25th and 75th percentile
Median age was 5.25 years (IQR 5.12); 1027 of children (50.6%) were males, 960 (47%) lived in North Italy, 341 (17%) in Centre Italy and 729 (36%) in South Italy. The median (95%CI) BMI-SDS of children was 0.22 (0.13 to 0.32) in North Italy, 0.40 (0.25 to 0.56) in Centre Italy and 0.51 (95%CI 0.40 to 0.62) in South Italy. Overweight plus obese children were 27.3% in the overall population (21.8% at North, 29.1% at Centre, and 33.3% at South).
Seventy-seven percent of parents had high school or university education level with regional differences (83% North, 85% Centre and 66% South). Regional differences were observed also for mother’s job: employed mothers were 75% at North, 72% at Centre and 42% at South.
Drinks or foods consumed before sleeping or at night time were reported in Table 2. The most frequent dining time was 7.30 P.M. at North and 8.00 P.M. at Centre and South. Overall, 28.2% of children drank before sleeping, especially at younger ages, mostly milk. Twenty percent of children ate before sleeping regardless to age, mostly sweets. During the night drinking or eating was markedly less frequent: 4.7% and 1.1%, respectively. The bottle use at bedtime was 30.8% at 1 to 3 years, 16.6% at 3 to 5 years and 4.9% at 5 to 7 years.
Table 2.
Drinks and foods consumed before sleeping or during the night in the study population
| Age groups (yrs) | All subjects | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 to 3 | 3 to 5 | 5 to 7 | 7 to 10 | 10 to 14 | ||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | |
| Subjects | 523 | 100.0 | 429 | 100.0 | 425 | 100.0 | 355 | 100.0 | 298 | 100.0 | 2030 | 100.0 |
| Drinks before sleep | ||||||||||||
| Nothing | 270 | 51.6 | 283 | 66.0 | 334 | 78.6 | 302 | 85.1 | 268 | 89.9 | 1457 | 71.8 |
| Milk | 214 | 40.9 | 94 | 21.9 | 51 | 12.0 | 23 | 6.5 | 14 | 4.7 | 396 | 19.5 |
| Juice | 27 | 5.2 | 38 | 8.9 | 25 | 5.9 | 19 | 5.4 | 9 | 3.0 | 118 | 5.8 |
| Milk & juice | 8 | 1.5 | 5 | 1.2 | 4 | 0.9 | 3 | 0.8 | 2 | 0.7 | 22 | 1.1 |
| Other | 2 | 0.4 | 3 | 0.7 | 7 | 1.6 | 6 | 1.7 | 5 | 1.7 | 23 | 1.1 |
| Unknown | 2 | 0.4 | 6 | 1.4 | 4 | 0.9 | 2 | 0.6 | 0 | 0.0 | 14 | 0.7 |
| Eats before sleep | ||||||||||||
| Nothing | 418 | 79.9 | 342 | 79.7 | 346 | 81.4 | 280 | 78.9 | 236 | 79.2 | 1622 | 79.9 |
| Fruit | 25 | 4.8 | 15 | 3.5 | 12 | 2.8 | 12 | 3.4 | 10 | 3.4 | 74 | 3.6 |
| Sweet | 41 | 7.8 | 47 | 11.0 | 38 | 8.9 | 47 | 13.2 | 29 | 9.7 | 202 | 10.0 |
| Salted | 13 | 2.5 | 15 | 3.5 | 11 | 2.6 | 7 | 2.0 | 11 | 3.7 | 57 | 2.8 |
| Fruit & sweet | 2 | 0.4 | 2 | 0.5 | 4 | 0.9 | 0 | 0.0 | 1 | 0.3 | 9 | 0.4 |
| Salted & sweet | 4 | 0.8 | 2 | 0.5 | 1 | 0.2 | 1 | 0.3 | 1 | 0.3 | 9 | 0.4 |
| Fruit & salted | 7 | 1.3 | 0 | 0.0 | 2 | 0.5 | 3 | 0.8 | 4 | 1.3 | 16 | 0.8 |
| Other | 10 | 1.9 | 5 | 1.2 | 6 | 1.4 | 4 | 1.1 | 4 | 1.3 | 29 | 1.4 |
| Unknown | 3 | 0.6 | 1 | 0.2 | 5 | 1.2 | 1 | 0.3 | 2 | 0.7 | 12 | 0.6 |
| Drinks during night | ||||||||||||
| Nothing | 454 | 86.8 | 403 | 93.9 | 418 | 98.4 | 350 | 98.6 | 296 | 99.3 | 1921 | 94.6 |
| Milk | 55 | 10.5 | 13 | 3.0 | 4 | 0.9 | 1 | 0.3 | 0 | 0.0 | 73 | 3.6 |
| Juice | 8 | 1.5 | 8 | 1.9 | 1 | 0.2 | 2 | 0.6 | 0 | 0.0 | 19 | 0.9 |
| Milk & juice | 1 | 0.2 | 2 | 0.5 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 3 | 0.1 |
| Other | 1 | 0.2 | 1 | 0.2 | 0 | 0.0 | 0 | 0.0 | 1 | 0.3 | 3 | 0.1 |
| Unknown | 4 | 0.8 | 2 | 0.5 | 2 | 0.5 | 2 | 0.6 | 1 | 0.3 | 11 | 0.5 |
| Eats during night | ||||||||||||
| Nothing | 509 | 97.3 | 426 | 99.3 | 419 | 98.6 | 346 | 97.5 | 290 | 97.3 | 1990 | 98.0 |
| Fruit | 4 | 0.8 | 0 | 0.0 | 0 | 0.0 | 2 | 0.6 | 4 | 1.3 | 10 | 0.5 |
| Sweet | 2 | 0.4 | 1 | 0.2 | 0 | 0.0 | 1 | 0.3 | 0 | 0.0 | 4 | 0.2 |
| Salted | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 0.3 | 0 | 0.0 | 1 | 0.1 |
| Fruit & sweet | 1 | 0.2 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 0.3 | 2 | 0.1 |
| Other | 3 | 0.6 | 1 | 0.2 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 4 | 0.2 |
| Unknown | 4 | 0.8 | 1 | 0.2 | 6 | 1.4 | 5 | 1.4 | 3 | 1.0 | 19 | 0.9 |
| Bottle use before sleep | 161 | 30.8 | 71 | 16.6 | 21 | 4.9 | 2 | 0.6 | 4 | 1.3 | 259 | 12.8 |
Sleep variables were reported in Table 3. Total sleep decreased with age from 11.5 h (1.5) (median (IQR)) in 1 to 3 years old children to 9.0 h (1.25) in 10 to 14 years old. Daytime sleep was negligible after 5 years of age. Overall, 1358 children (66.9%) had a total sleep duration in agreement with the NSF 2015 recommendations. Such proportion varied between 64 and 77% up to 10 years of age and dropped to 50% thereafter. Sleep duration was shorter than recommended in 642 children (31.6%) and longer than recommended in 30 children (1.5%). Children living at South (62.4%) and at Centre (66.9%) followed recommendations in lower percentages than those living at North (72.6%).
Table 3.
Sleep duration and sleep related characteristics in the study population
| Age groups (yrs) | All subjects | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 to 3 | 3 to 5 | 5 to 7 | 7 to 10 | 10 to 14 | ||||||||
| Subjects | 523 | 100.0 | 429 | 100.0 | 425 | 100.0 | 355 | 100.0 | 298 | 100.0 | 2030 | 100.0 |
| Med | IQR | Med | IQR | Med | IQR | Med | IQR | Med | IQR | Med | IQR | |
| Nocturnal sleep (hrs) | 9.50 | 1.25 | 9.75 | 1.25 | 9.75 | 1.00 | 9.50 | 0.75 | 8.88 | 1.25 | 9.50 | 1.00 |
| Daytime sleep (hrs) | 2.00 | 1.00 | 0.75 | 1.50 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 1.50 |
| Total sleep (hrs) | 11.50 | 1.50 | 10.50 | 1.00 | 9.75 | 1.00 | 9.50 | 1.00 | 9.00 | 1.25 | 10.00 | 1.75 |
| N | % | N | % | N | % | N | % | N | % | N | % | |
| Sleep duration according with Recommendationsa | ||||||||||||
| Under | 171 | 32,7 | 104 | 24.2 | 141 | 33.2 | 82 | 23.1 | 144 | 48.3 | 642 | 31.6 |
| Recommended | 346 | 66.2 | 319 | 74.4 | 272 | 64.0 | 272 | 76.6 | 149 | 50.0 | 1358 | 66.9 |
| Over | 6 | 1.1 | 6 | 1.4 | 12 | 2.8 | 1 | 0.3 | 5 | 1.7 | 30 | 1.5 |
| Awakenings | ||||||||||||
| 0 | 170 | 32.5 | 204 | 47.6 | 294 | 69.2 | 272 | 76.6 | 223 | 74.8 | 1163 | 57.3 |
| 1 | 156 | 29.8 | 144 | 33.6 | 96 | 22.6 | 60 | 16.9 | 52 | 17.4 | 508 | 25.0 |
| 2 | 120 | 22.9 | 46 | 10.7 | 31 | 7.3 | 14 | 3.9 | 18 | 6.0 | 229 | 11.3 |
| 3 | 39 | 7.5 | 27 | 6.3 | 3 | 0.7 | 6 | 1.7 | 4 | 1.3 | 79 | 3.9 |
| ≥4 | 38 | 7.3 | 8 | 1.8 | 1 | 0.2 | 2 | 0.6 | 1 | 0.3 | 50 | 2.4 |
| Unknown | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 0.3 | 0 | 0.0 | 1 | 0.0 |
| Owns a room | ||||||||||||
| Yes | 212 | 40.5 | 234 | 54.5 | 211 | 49.6 | 181 | 51.0 | 164 | 55.0 | 1002 | 49.4 |
| No | 209 | 40.0 | 90 | 21.0 | 48 | 11.3 | 27 | 7.6 | 7 | 2.3 | 381 | 18.8 |
| Shared | 97 | 18.5 | 100 | 23.3 | 166 | 39.1 | 146 | 41.1 | 127 | 42.6 | 636 | 31.3 |
| Unknown | 5 | 1.0 | 5 | 1.2 | 0 | 0.0 | 1 | 0.3 | 0 | 0.0 | 11 | 0.5 |
| Has TV in bedroom | 131 | 25.0 | 155 | 36.1 | 182 | 42.8 | 184 | 51.8 | 158 | 53.0 | 810 | 39.9 |
| Display devices use | 207 | 39.6 | 281 | 65.5 | 295 | 69.4 | 269 | 75.8 | 237 | 79.5 | 1289 | 63.5 |
| Reads before sleep | 189 | 36.1 | 208 | 48.5 | 183 | 43.1 | 120 | 33.8 | 93 | 31.2 | 793 | 39.1 |
| Where falls asleep | ||||||||||||
| Own bed | 245 | 46.8 | 218 | 50.8 | 264 | 62.1 | 255 | 71.8 | 260 | 87.2 | 1242 | 61.2 |
| Parents’ bed | 203 | 38.8 | 157 | 36.6 | 109 | 25.6 | 70 | 19.7 | 23 | 7.7 | 562 | 27.7 |
| Other room | 67 | 12.8 | 48 | 11.2 | 49 | 11.5 | 28 | 7.9 | 15 | 5.0 | 207 | 10.2 |
| Outside home | 5 | 1.0 | 5 | 1.2 | 2 | 0.5 | 2 | 0.6 | 0 | 0.0 | 14 | 0.7 |
| Unknown | 3 | 0.6 | 1 | 0.2 | 1 | 0.2 | 0 | 0.0 | 0 | 0.0 | 5 | 0.2 |
| Where sleeps | ||||||||||||
| Own bed | 363 | 69.4 | 284 | 66.2 | 333 | 78.4 | 289 | 81.4 | 278 | 93.3 | 1547 | 76.2 |
| Parents’ bed | 157 | 30.0 | 137 | 31.9 | 84 | 19.8 | 61 | 17.2 | 17 | 5.7 | 456 | 22.5 |
| Other room | 2 | 0.4 | 5 | 1.2 | 6 | 1.4 | 3 | 0.8 | 2 | 0.7 | 18 | 0.9 |
| Outside home | 0 | 0.0 | 2 | 0.5 | 1 | 0.2 | 2 | 0.6 | 0 | 0.0 | 5 | 0.2 |
| Unknown | 1 | 0.2 | 1 | 0.2 | 1 | 0.2 | 0 | 0.0 | 1 | 0.3 | 4 | 0.2 |
aNSF recommendations (ref. [15])
Figure 1 plots the percentiles of sleep duration as function of age in the whole sample (n = 2030). Such percentiles were estimated from quantile regression (see Statistical analysis for details).
Fig. 1.
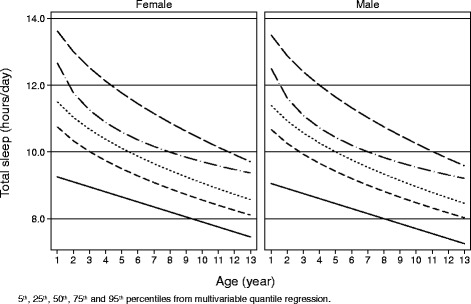
Percentiles of total sleep duration as function of age and gender in the study population
Table 3 reported the number of night awakenings divided by age: specifically no awakenings were reported in 32.5% in 1–3 years group and increased to 74.8% in 10–14 years group; more than 2 awakenings were reported 14.8% in the younger group and decreased to 1.6% in the older group.
Overall, 63.5% of children used video devices (39.6% at age 1–3, increasing thereafter till 79.5% at age 10–13) and 39.1% read before sleeping (with a maximum of 48.5% at age 3–5 and then a progressive decrease). Overall, 61.2% of children fell asleep in their own bed, 27.7% in parents’ bed and 10.2% in other room. Children falling asleep in their bed increased with age and those falling asleep in parents’ bed decreased. Children sleeping in their own bed for the most part of the night increased with age from 69,4% at 1 to 3 years to 93.3% at 10 to 14 years. Overall, 23.4% of children changed place of sleeping during the night, mostly from parents’ to own bed (10.1%), from other room to own bed (7.6%) or from own to parents’ bed (3.0%).
Use of products for sleep were reported in Table 4. At study time 2.1% of parents reported use of products for sleeping, while 10.0% reported its use in the past. In 22.4% of children an history of sleeping problems in the first year of life was found.
Table 4.
Use of products for sleeping in the study population
| Age groups (yrs) | All subjects | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 to 3 | 3 to 5 | 5 to 7 | 7 to 10 | 10 to 14 | ||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | |
| Subjects | 523 | 100.0 | 429 | 100.0 | 425 | 100.0 | 355 | 100.0 | 298 | 100.0 | 2030 | 100.0 |
| Sleep disorder in 1st year | ||||||||||||
| No | 342 | 65.4 | 302 | 70.4 | 317 | 74.6 | 267 | 75.2 | 209 | 70.1 | 1437 | 70.8 |
| Yes | 136 | 26.0 | 98 | 22.8 | 88 | 20.7 | 67 | 18.9 | 65 | 21.8 | 454 | 22.4 |
| Sometimes | 44 | 8.4 | 29 | 6.8 | 20 | 4.7 | 21 | 5.9 | 21 | 7.0 | 135 | 6.7 |
| Unknown | 1 | 0.2 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 3 | 1.0 | 4 | 0.2 |
| Has used products to sleep | ||||||||||||
| No | 462 | 88.3 | 391 | 91.1 | 390 | 91.8 | 316 | 89.0 | 266 | 89.3 | 1825 | 89.9 |
| Yes | 59 | 11.3 | 38 | 8.9 | 35 | 8.2 | 39 | 10.7 | 32 | 10.7 | 202 | 10.0 |
| Unknown | 2 | 0.4 | 0 | 0.0 | 0 | 0.0 | 0 | 0.3 | 0 | 0.0 | 3 | 0.1 |
| Has used: | ||||||||||||
| Melatonin | 35 | 6.7 | 23 | 5.4 | 17 | 4.0 | 14 | 3.9 | 8 | 2.7 | 97 | 4.8 |
| Phytotherapy | 19 | 3.6 | 14 | 3.3 | 13 | 3.1 | 15 | 4.2 | 9 | 3.0 | 70 | 3.4 |
| Tryptophan | 2 | 0.4 | 1 | 0.2 | 0 | 0.0 | 1 | 0.3 | 2 | 0.7 | 6 | 0.3 |
| Vitamin B6 | 3 | 0.6 | 2 | 0.5 | 0 | 0.0 | 1 | 0.3 | 0 | 0.0 | 6 | 0.3 |
| Homeopathy | 12 | 2.3 | 6 | 1.4 | 9 | 2.1 | 10 | 2.8 | 7 | 2.3 | 44 | 2.2 |
| Other products | 3 | 0.6 | 3 | 0.7 | 5 | 1.2 | 7 | 2.0 | 9 | 3.0 | 27 | 1.3 |
| Suggested by: | ||||||||||||
| Pediatrician | 47 | 9.0 | 32 | 7.5 | 27 | 6.4 | 32 | 9.0 | 24 | 8.1 | 162 | 8.0 |
| Other parents | 2 | 0.4 | 1 | 0.2 | 0 | 0.0 | 1 | 0.3 | 0 | 0.0 | 4 | 0.2 |
| Pharmacist | 9 | 1.7 | 5 | 1.2 | 4 | 0.9 | 6 | 1.7 | 3 | 1.0 | 27 | 1.3 |
| Auto-prescription | 2 | 0.4 | 1 | 0.2 | 5 | 1.2 | 2 | 0.6 | 6 | 2.0 | 16 | 0.8 |
| Are products to sleep effective | ||||||||||||
| No | 20 | 3.8 | 11 | 2.6 | 14 | 3.3 | 10 | 2.8 | 11 | 3.7 | 66 | 3.3 |
| Sometimes | 26 | 4.8 | 20 | 4.7 | 14 | 3.3 | 17 | 4.8 | 8 | 2.7 | 84 | 4.1 |
| Yes | 13 | 2.5 | 7 | 1.6 | 7 | 1.6 | 12 | 3.4 | 13 | 4.4 | 52 | 2.6 |
| Uses products to sleep now | ||||||||||||
| No | 502 | 96.0 | 420 | 97.9 | 421 | 99.1 | 352 | 99.2 | 291 | 97.7 | 1986 | 97.8 |
| Yes | 21 | 4.0 | 9 | 2.1 | 3 | 0.7 | 3 | 0.8 | 7 | 2.3 | 43 | 2.1 |
| Unknown | 0 | 0.0 | 0 | 0.0 | 1 | 0.2 | 0 | 0.0 | 0 | 0.0 | 1 | 0.0 |
Table 5 reports sleep related variables observed in optimal sleepers (752 children, 37.0%) and not optimal sleepers (1278 children, 63.0%), as defined in Methods section. Mean age (7.1 year [5.0, 10.0] (median [IQR]) was higher in optimal sleepers than in not optimal sleepers (4.0 year [2.3, 6.3]), while total sleep duration was lower (9.5 h [9.0, 10.2] vs 10.2 h [9.5, 11.2]). BMI SDS was similar in both groups (optimal sleepers 0.34 [-0.40, 1.19], not optimal sleepers 0.31 [-0.38, 1.08]).
Table 5.
Sleep related variables observed in optimal sleepers and not optimal sleepers
| Not optimal sleepers (n = 1278) |
Optimal sleepers (n = 752) |
|||
|---|---|---|---|---|
| N | % | N | % | |
| Child | ||||
| Male | 627 | 49.1 | 400 | 53.2* |
| Normal weight | 704 | 67.8 | 490 | 68.8 |
| Firstborn | 754 | 59.0 | 450 | 59.8 |
| Only child | 490 | 38.3 | 158 | 21.0* |
| Family | ||||
| Mother’edu: high school or univ | 964 | 75.4 | 606 | 80.6* |
| Mother employed | 780 | 61.0 | 487 | 64.8* |
| Father’s edu: high school or univ | 893 | 69.9 | 522 | 69.4 |
| Father employed | 1164 | 92.8 | 684 | 92.1 |
| Sleep items | ||||
| Follows NSF recommendations | 872 | 68.2 | 508 | 67.6 |
| Has TV in bedroom | 523 | 41.1 | 287 | 38.3* |
| Display devices use before sleeping | 783 | 61.5 | 506 | 67.3* |
| Reads before sleep | 486 | 38.2 | 307 | 40.9* |
| Sleep problems during the 1st year | 325 | 25.5 | 129 | 17.2* |
| Has used products to sleep in the past | 151 | 11.8 | 51 | 6.8* |
| Drink & food items | ||||
| -Drinks before sleep: | ||||
| Nothing | 848 | 66.8 | 609 | 81.5* |
| Milk | 311 | 24.5 | 85 | 11.4* |
| Juice | 84 | 6.6 | 34 | 4.6* |
| -Bottle use | 218 | 17.2 | 41 | 5.5* |
| -Eats before sleep: | ||||
| Nothing | 1012 | 79.7 | 610 | 81.4 |
| Fruit | 53 | 4.2 | 21 | 2.8 |
| Sweet | 119 | 9.4 | 83 | 11.1 |
| Salted | 42 | 3.3 | 15 | 2.0 |
| -Eats during night: | ||||
| Nothing | 1250 | 98.7 | 740 | 99.3 |
| -Drinks during night: | ||||
| Nothing | 1178 | 92.7 | 743 | 99.3* |
| Milk | 70 | 5.5 | 3 | 0.4* |
| Juice | 17 | 1.3 | 2 | 0.3* |
*p value < 0.05 respect to not optimal sleepers
Optimal sleepers showed a higher proportion of males, their mothers had higher education level and were more frequently employed. Optimal sleepers were less frequently only child, used bottle, had TV in the bedroom, drank before sleeping, presented sleep disorders during the first year of life and used product for sleeping, while they read before sleeping more frequently. Percentages of children in agreement with 2015 NSF recommendations for sleep duration were similar in both groups.
Predictors of total sleep duration
At multivariable median regression, (Table 6) an increase of 1 year of age was associated with a decrease of 0.24 h [95%CI -0.25 to -0.22, p < 0.001] of total sleep, the use of display devices before sleeping was associated with a decrease of 0.25 h [95%CI -0.35 to -0.14, p < 0.001]. Other significant predictors found at univariable level (i.e., having TV in the bedroom, and drinking before sleeping.) were no more associated with total sleep duration when age and display devices use were taken into account at multivariable level. BMI-SDS was not associated with total sleep duration (-0.02 h [-0.06, 0.02]), even in the obese group alone. Similarly no association was found with parental age, parental education or job, number of family members, birth weight, to be firstborn or only child, feel asleep in own bed, bottle use, reading or eating before sleeping, or the presence of sleep disorders in the first year of life.
Table 6.
Multivariable median regression for total sleep duration
| Total sleep (hours) | |
|---|---|
| Age (years) | -0.24*** [-0.25,-0.22] |
| BMI (SDS) | -0.02 [-0.06,0.02] |
| Has TV in bedroom | -0.08 [-0.18,0.03] |
| Use of display devices | -0.25*** [-0.35,-0.14] |
| Drinks before sleep | -0.06 [-0.13,0.00] |
| Constant | 11.76*** [11.61,11.90] |
| Observations | 2006 |
Multivariable median regression
Value are regression coefficients [95% CI]
***p < 0.001
Predictors of optimal sleep
At multivariable logistic regression (Table 7), optimal sleeper condition was positively associated with age (OR 1.28 [1.23, 1.32], p < 0.001), and with mother’s high education level (OR 1.44 [1.11, 1.88], p < 0.01) and negatively associated with having TV in the bedroom (OR 0.63 [0.50, 0.79], p < 0.001), being only child (OR 0.60 [0.47, 0.78], p < 0.001), bottle use (OR 0.64 [0.44, 0.94], p < 0.05), and sleep disorders during the first year of life (OR 0.62 [0.48, 0.80], p < 0.001). Other significant predictors found at univariable level (i.e., use of display devices, drinking or before sleeping, own a room, or mother working at home) were no more associated with optimal sleep when the previous predictors were taken into account at multivariable level. BMI-SDS was not associated with good sleeping (OR 1.00 [0.92, 1.09]) as well as all other variables.
Table 7.
Multivariable logistic regression for optimal sleep condition
| Optimal sleep | |
|---|---|
| Age (years) | 1.28*** [1.23,1.32] |
| BMI (SDS) | 1.00 [0.92,1.09] |
| Has TV in bedroom | 0.63*** [0.50,0.79] |
| Use of display devices | 0.91 [0.72,1.14] |
| Drinks before sleep | 0.99 [0.85,1.14] |
| Mother has high school or university degree | 1.44** [1.11,1.88] |
| Owns a room | 1.06 [0.94,1.19] |
| Reads before sleep | 1.17 [0.94,1.44] |
| Only child | 0.60*** [0.47,0.78] |
| Mother works at home | 0.95 [0.75,1.20] |
| Bottle use | 0.64* [0.44,0.94] |
| Sleep disorder at < 1 year of age | 0.62*** [0.48,0.80] |
| Observations | 1977 |
Multivariable logistic regression. Values are odds ratios
Values are odds ratios [95% CI]
*p < 0.05, **p < 0.01, ***p < 0.001
Discussion
The main results of the present study was that 33.1% of 1 to 14 years old children did not follow sleep duration recommendations, and that the percentage dropped to 50% in teenage. Because the study used convenience sampling, its results should not be extrapolated to the general population. However, the large sample size and the regional distribution of studied children, very close to that known in Italy, let us suggest that these data could describe a real phenomenon, as nationalwide collected sleep data are still lacking in our country at present. Of the 33.1% of children not coping with recommendations, the great majority are referred to sleep less than the lower limit and only the 1.5% more than the upper limit of recommendations. Multivariable regression analysis indicated that the only independent factor associated with sleep duration was the use of a video device in the imminence of bedtime. A negative relationship between videotime and sleep has been already suggested by others studies [8–11, 22, 23], in adolescence but recently also in younger ages due to the widespread and earlier use of technology [24]. We found that the use of a video device close to bedtime in childhood was related to a short sleep independently of the presence of bedroom TV, and this fact might be explained by the increasing use of mobile devices [25]. Literature reports a relationship between light exposure from video devices at bedtime and melatonin suppression, suggesting a possible explaination for the linking between video use and sleep duration [12, 23, 24]. We acknowledge that it seems unfeasible to avoid any video dependence for children at present time, but the relationship between video use close to bedtime and short sleep should be stressed. Of note, we did not found any relationship between sleep duration and child BMI, in contrast with the prevalent literature on this topic [26, 27], but in accordance with others [28]. This discrepancy among different studies might be due to variables considered, as it is known that many factors (and video use above all) are related with both sleep and obesity status.
In our study we considered also sleep continuity, defining as optimal sleepers those children sleeping in their own bed without awakenings throughout the night. Number of awakenings was higher in younger age groups as well as number of children falling asleep or sleeping out of their own bed. We consider very impressive that about one fourth of children changed place of sleeping during the night. Children defined as optimal sleepers (globally the 37% of our population) were generally older but with a similar median BMI-SDS respect to not optimal ones, thus confirming the low impact of BMI status on sleep in our population. Multivariable regression analysis indicated that independent factors associated with optimal sleep condition were high mother’s educational level, being only child, an history of sleep problems during the first year of life, present bottle use and bedroom TV. Some of these findings deserve a specific discussion.
An early history of sleep problems affecting further sleep continuity suggests the importance of establishing a correct sleep pattern very soon after birth, taking into account that a relative stability of sleep characteristics has been described starting from 6 month of age [29]. Moreover, parents and pediatricians should give an extreme importance to prevent sleep problems from birth.
Pediatricians usually suggest bottle use weaning at or around 12 months of age, but this recommendation is greatly ignored [30]. In our population, 4.9% of 5 to 7 years children used bottle in the imminence of sleeping time, and the use decreased thereafter but was still detectable (0.6% at 7 to 10 years and 1.3% at 10 to 14 years). A prolunged bottle use seems to be related to an alteration of sleep pattern, at least for children under 3 years of age, as found by other studies [31]. The negative effect of bottle use on sleep continuity found in our analysis suggests that this relationship might be present also in older children and underlines the need for an identification and possibly correction of such neglected attitude in late bottle consumers.
Also bedroom TV was associated with not optimal sleep, and this confirmed previous finding of the negative impact of video devices on sleep [8, 10, 11].
No effect of bedtime reading, and drink or food consumption was found on sleep continuity or duration in our population, when previous reported variables were taken into account.
A strenght of the present study is the characterization of sleep duration percentiles for age and gender, specific for Italian population and useful in clinical practice, which are similar but not coincident with those already available from other Countries. For instances, sleep duration in Italian children seems to be shorter than that reported in English peers [32].
Among study limitations we should consider first of all the cross sectional design which does not allow to determine casuality between considered variables and sleep items. Moreover, the lack of sleep latency data among studied parameters limits the assessment of sleep quality in our population. Finally, we considered only video devices use in the imminence of sleeping and we did not collect information concerning daily video consume, thus making impossible any correction for that in the analysis.
A recent technical report of the American Academy of Pediatrics [33], analysing both benefits and risks of new media use on child health, stressed the negative impact of video use on sleep characteristics and suggested the adoption of an healthy Family Media Use Plan individualized for a specific child and family, in order to identify an appropriate balance between video time and other activities.
Conclusion
In conclusion there is a consistent percentage of children and adolescent that do not sleep sufficiently and this sleep deprivation could lead to neurobehavioral dysfunction. Pediatricians and mainly family pediatricians should give relevance to the identification of sleep problems early in life and in particular acting on the modifiable risk factors identified in the present study like video use at bedtime, bedroom TV, bottle use before sleep. Furthermore the fact that an history of sleep problems during the first year is related to not optimal sleep later in the life highlights the importance of ensuring a good sleep since the first months of life adopting correct preventive strategies.
Acknowledgements
We thank all FPs collecting data and Dr. Giorgio Bedogni for statistical support.
on behalf of the “Ci piace sognare” Study Group:
Salvatore Barberi, Sergio Bernasconi, Gianni Bona, Guido Brusoni, Carmen Buongiovanni, Marco Carotenuto, Mattia Doria, Daniele Ghiglioni, Manuel Gnecchi, Lorenzo Iughetti, Claudio Maffeis, Paola Manzoni, Maura Sticco, Gianni Tamassia, Elvira Verduci.
Funding
the study was financially supported by an unconditioned funding from Milte Italia S.p.A.
Availability of data and materials
All data generated or analysed during this study are included in this published article [as Additional file 1].
Authors’ contributions
PB: study conception, study design, data analysis, paper writing and editing. MG, AP, LV and FP: study design, population recruitments, data analysis, paper writing and editing. EMG, MP, GDM, SS and EC: data analysis, paper writing and editing. OB: data analysis, major contributor in writing the manuscript. All Authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study was approved by Ethical Committee of Azienda Ospedaliero Universitaria “Maggiore della Carita” of Novara on 2nd March 2015 (#124).
Abbreviations
- BMI
Body Mass Index
- CI
Confidence interval
- FP
Family Pediatricians
- IQR
Inter quartile range
- NSF
National Sleep Foundation
- OR
Odds ratio
- PC
Personal computer
- SDS
Standard Deviation Score
- TV
Television set
- WHO
World Health Organization
Additional file
Dataset. (XLS 4134 kb)
Contributor Information
Paolo Brambilla, Phone: +393392238772, Email: paolo.brambilla3@gmail.com.
Marco Giussani, Email: abrjg@tin.it.
Angela Pasinato, Email: pasinato.angela@gmail.com.
Leonello Venturelli, Email: leoventu@libero.it.
Francesco Privitera, Email: docprivitera@tiscali.it.
Emanuele Miraglia del Giudice, Email: emanuele.miraglia@unina2.it.
Sara Sollai, Email: sarasollai@gmail.com.
Marina Picca, Email: piccamarina@gmail.com.
Giuseppe Di Mauro, Email: giuseppedimauro@sipps.it.
Oliviero Bruni, Email: oliviero.bruni@uniroma1.it.
Elena Chiappini, Email: elena.chiappini@unifi.it.
on behalf of the “Ci piace sognare” Study Group:
Salvatore Barberi, Sergio Bernasconi, Gianni Bona, Guido Brusoni, Carmen Buongiovanni, Marco Carotenuto, Mattia Doria, Daniele Ghiglioni, Manuel Gnecchi, Lorenzo Iughetti, Claudio Maffeis, Paola Manzoni, Maura Sticco, Gianni Tamassia, and Elvira Verduci
References
- 1.Cappuccio FP, Taggart FM, Ngianga-Bakwin K, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31:619–626. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Matthews KA, Pantesco EJM. Sleep characteristics and cardiovascular risk in children and adolescents: an enumerative review. Sleep Med. 2016;18:36–49. doi: 10.1016/j.sleep.2015.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Paavonen EJ, Raikkonen K, Pesonen A-K, et al. Sleep quality and cognitive performance in 8 year old children. Sleep Med. 2010;11:386–392. doi: 10.1016/j.sleep.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 4.Cortesi F, Giannotti F, Ivanenko A, Johnson K. Sleep in children with autistic spectrum disorder. Sleep Med. 2010;11:659–664. doi: 10.1016/j.sleep.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 5.Iglowstein I, Jenni OG, Molinari L, Largo RH. Sleep duration from infancy to adolescence: Reference values and generational trends. Pediatrics. 2003;111:302–307. doi: 10.1542/peds.111.2.302. [DOI] [PubMed] [Google Scholar]
- 6.Matricciani L, Olds T, Petkov J. In search of lost sleep: secular trends in the sleep time of school-aged children and adolescents. Sleep Med Rev. 2012;16:203–211. doi: 10.1016/j.smrv.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 7.Buysse DJ. Sleep health: can we define it? Does it matter? Sleep. 2014;37:9–17. doi: 10.5665/sleep.3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garrison MM, Liekweg K, Christakis DA. Media use and child sleep: the impact of content, timing, and environment. Pediatrics. 2011;128:29–35. doi: 10.1542/peds.2010-3304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Calamaro CJ, Yang K, Ratcliffe S, Chasens ER. Wired at a young age: the effect of caffeine and technology on sleep duration and body mass index in school-aged children. J Pediatr Health Care. 2012;26:276–282. doi: 10.1016/j.pedhc.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 10.Nuutinen T, Ray C, Roos E. Do computer use, TV viewing, and the presence of the media in the bedroom predict schoolaged children’s sleep habits in a longitudinal study? BMC Public Health. 2013;13:684. doi: 10.1186/1471-2458-13-684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cespedes EM, Gillman MW, Kleinman K, Rifas-Shiman SL, Redline S, Taveras EM. Television viewing, bedroom television and sleep duration from infancy to mid-childhood. Pediatrics. 2014;133:e1163–e1171. doi: 10.1542/peds.2013-3998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cain N, Gradisar M. Electronic media use and sleep in school-aged children and adolescents: A review. Sleep Med. 2010;11:735–742. doi: 10.1016/j.sleep.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 13.Bruni O, Ottaviano S, Guidetti V, et al. The Sleep Disturbance Scale for Children (SDSC). Construction and validation of an instrument to evaluate sleep disturbances in childhood and adolescence. J Sleep Res. 1996;5:251–261. doi: 10.1111/j.1365-2869.1996.00251.x. [DOI] [PubMed] [Google Scholar]
- 14.Owens JA, Spirito A, McGuinn M. The Children’s Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep. 2000;23:1043–1051. [PubMed] [Google Scholar]
- 15.Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1:40–43. doi: 10.1016/j.sleh.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 16.Lohman TG, Roche AF, Martorell R. Anthropometric standardization reference manual. Edited by Lohman, Roche & Martorell. Champaign IL Human Kinetics Books, 1988.
- 17.http://www.who.int/childgrowth/. Accessed 01 July 2015.
- 18.Koenker R. Quantile regression. Cambridge: Cambridge University Press; 2005. [Google Scholar]
- 19.Hosmer DW, Lemeshow S, Sturdivant RX. Applied Logistic Regression. Hoboken: Wiley; 2013. [Google Scholar]
- 20.Royston P, Sauerbrei W. Multivariable model-building: a pragmatic approach to regression analysis based on fractional polynomials for modelling continuous variables. Chichester: Wiley; 2008. [Google Scholar]
- 21.http://www.istat.it/it/informazioni/. Accessed 01 Apr 2015.
- 22.Dong S, Song Y, Jiang Y, Sun W, Wang Y, Jiang F. Multi-center study on the effects of television viewing on sleep quality among children under 4 years of age in China. Zhonghua Er Ke Za Zhi. 2015;53:907–912. [PubMed] [Google Scholar]
- 23.Bruni O, Sette S, Fontanesi L, Baiocco R, Laghi F, Baumgartner E. Technology use and sleep quality in preadolescence and adolescence. J Clin Sleep Med. 2015;11:1433–1441. doi: 10.5664/jcsm.5282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brockmann PE, Diaz B, Damiani F, Villarroel L, Nunez F, Bruni O. Impact of television on the quality of sleep in preschool children. Sleep Med. 2016;20:140–144. doi: 10.1016/j.sleep.2015.06.005. [DOI] [PubMed] [Google Scholar]
- 25.Yland J, Guan S, Emanuele E, Hale L. Interactive vs passive screen time and nighttime sleep duration among school-aged children. Sleep Health. 2015;1:191–196. doi: 10.1016/j.sleh.2015.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baird J, Hill CM, Harvey NC, SWS Study Group et al. Duration of sleep at 3 years of age is associated with fat and fat-free mass at 4 years of age: the Southampton Women’s Survey. J Sleep Res. 2016;25:412–418. doi: 10.1111/jsr.12389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carter PJ, Taylor BJ, Williams SM, Taylor RW. Longitudinal analysis of sleep in relation to BMI and body fat in children: the FLAME study. BMJ. 2011;342:d2712. doi: 10.1136/bmj.d2712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Klingenberg L, Christensen LB, Hjorth MF, et al. No relation between sleep duration and adiposity indicators in 9-36 months old children: the SKOT cohort. Pediatr Obes. 2013;8:e14–e18. doi: 10.1111/j.2047-6310.2012.00109.x. [DOI] [PubMed] [Google Scholar]
- 29.Bruni O, Baumgartner E, Sette S, et al. Longitudinal study of sleep behavior in normal infants during the first year of life. J Clin Sleep Med. 2014;10:1119–1127. doi: 10.5664/jcsm.4114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bonuch K, Huang V, Fletcher J. Inappropriate bottle use: an early risk for overweight? Literature review and pilot data for a bottle-weaning trial. Matern Child Nutr. 2010;6:38–52. doi: 10.1111/j.1740-8709.2009.00186.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sadeh A, Mindell JA, Luedtke K, Wiegand B. Sleep and sleep ecology in the first 3 years: a web-based study. J Sleep Res. 2009;18:60–73. doi: 10.1111/j.1365-2869.2008.00699.x. [DOI] [PubMed] [Google Scholar]
- 32.Blair PS, Humphreys JS, Gringras P, et al. Childhood sleep duration and associated demographic characteristics in an English cohort. Sleep. 2012;35:353–360. doi: 10.5665/sleep.1694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Reid Chassiakos Y, Radesky J, Christakis D, Moreno MA, Cross C, Children and Adolescents and Digital Media AAP Council on Communications and Media. Pediatrics. 2016;138:e20162593. doi: 10.1542/peds.2016-2593. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analysed during this study are included in this published article [as Additional file 1].


