Abstract
The Hypertension Attitude PersPEctives and Needs (HAPPEN) survey was a real‐world survey of cardiologists, nephrologists, and patients with treated hypertension at level 3 hospitals in China. It aimed to characterize the attitudes and behavior of physicians and patients and to identify possible causes of poor blood pressure (BP) control. Randomly selected participants (100 cardiologists, 30 nephrologists, 400 patients) completed face‐to‐face interviews investigating BP control rates, consulting behavior, prescribing patterns, and attitudes toward hypertension management. Perceived levels of BP control were high; 70% of physicians and 85% of patients believed that BP targets were achieved, despite only 31% of patients achieving targets. Physician satisfaction with control rates and patient satisfaction with treatment were high. Differences in perceived and actual levels of BP control may be driving therapeutic inertia. In combination with inadequate patient evaluation and support services, therapeutic inertia may contribute to poor BP control among patients with treated hypertension in China.
Hypertension remains a global problem and is estimated to cause approximately 12.8% of all deaths annually.1 Despite the availability of effective treatments for lowering blood pressure (BP) and regularly updated guidelines for the management of hypertension,2 a high proportion of patients diagnosed with hypertension fail to achieve BP control. Although the prevalence of hypertension is similar in Europe, the Americas, and Asia,1 the rate of BP control among patients with treated hypertension shows some differences. For example, in the United States, the 2009–2010 results of the National Health and Nutrition Examination Survey (NHANES) demonstrated that 64.4% of patients with managed hypertension achieved BP control.3 In contrast, according to the 2009 the survey of BP control rates in Chinese hypertensive outpatients (China STATUS), the BP control rate in outpatients with managed hypertension was 30.6%.4
Evidence from many sources suggests that both patient and physician attitudes toward the treatment of hypertension contribute to poor BP control rates. Patients' intentional nonadherence to antihypertensive medications has been attributed to factors such as the beliefs that the treatment is unnecessary because of the lack of symptoms and that there is an unacceptably high risk of treatment‐related adverse events (AEs).5 Among physicians, a lack of knowledge or belief in the treatment guidelines, uncertainty regarding the accuracy of BP measurements, and a preference for providing treatment based on their own clinical experience are thought to contribute to “therapeutic inertia,” defined as the tendency of physicians not to change or intensify treatment even if it is clinically justified.6, 7 However, the majority of evidence supporting the generalizability of these patient and physician attitudes is from studies carried out in Western countries. The relevance of these findings to the poor rates of BP control in China is unknown. A detailed understanding of hypertension management from both the physician and patient perspective is required to identify areas of hypertension treatment that can be improved, to enable the development of initiatives to tackle poor BP control in China.
To gain a better understanding of why BP control rates remain poor in China, the Hypertension Attitude PersPEctives and Needs (HAPPEN) real‐world survey was conducted to investigate the role of physician and patient attitudes to BP control and factors that influence prescribing patterns of antihypertensive treatments.
The objective of the HAPPEN study was to characterize the attitudes, knowledge, and behavior of physicians and patients with hypertension toward the management of hypertension in level 3 hospitals in China. Specifically, this survey aimed to establish whether physicians utilize guidelines and treatment algorithms in their practice; to establish the proportion of patients who reach their target BP, and their perspective on BP control; to identify key drivers for treatment choices; and to understand physician and patient attitudes toward treatment choices and behaviors.
Methods
Study Design
The HAPPEN study was a real‐world survey of cardiologists, nephrologists, and patients with hypertension carried out at level 3 hospitals in China between November 2014 and January 2015. Level 3 hospitals are comprehensive or general hospitals at the city, provincial, or national level with a bed capacity exceeding 500. They are responsible for providing specialist health services, perform a key role with regard to medical education and scientific research, and serve as medical hubs that provide care to multiple regions.
The study design and surveys were developed by an expert panel (manuscript authors) with assistance from Research Partnership, an independent healthcare market research and consulting agency. Although the surveys were not formally validated, the development process involved comprehensive reviewing and piloting of the surveys. Surveys were conducted face‐to‐face, in Mandarin and Cantonese (Guangzhou), by trained interviewers who were previously unknown to the respondents. Interviews were conducted in accordance with the European Society for Opinion and Marketing Research (ESOMAR) guidelines.8 Extensive quality control checks were performed throughout the survey development, data collection, and data analysis. Review board approval was not required.
Study Population
Level 3 hospitals in Beijing, Shanghai, and Guangzhou were randomly selected for surveying. Cardiologists and nephrologists practicing at the selected hospitals were invited to participate in the survey. Following screening and verbal consent to participate, eligible physicians completed the survey. Physician inclusion criteria included being a practicing doctor for at least 5 years, having reached at least the seniority level of Doctor in Charge, spending at least 70% of their time in clinical care, being responsible for the treatment of at least 100 patients with hypertension per month, and prescribing all commonly available classes of antihypertensive drugs.
At the selected hospitals, patients attending an outpatient cardiology or nephrology clinic for the treatment of hypertension were randomly intercepted and invited to take part in the survey. Patients were screened to assess their eligibility and provided written informed consent to participate in the survey. Patient inclusion criteria included having a diagnosis of hypertension for at least 1 year, having consistently received prescription treatment for hypertension for at least 6 months, and being resident in a level 1 city.
All participants received appropriate monetary compensation for their time.
Patient and Physician Interviews
Interviews were designed to be completed in approximately 30 minutes. The physician survey (Supplementary File 1) consisted of five sections examining consulting behavior, current hypertension treatment behavior, attitudes toward hypertension, treatment barriers and adherence, and 10 case studies. For the case studies, physicians were provided with profiles of patients with hypertension with varying degrees of severity, comorbidities, and additional risk factors and were asked how they would treat the patients initially and if their BP remained uncontrolled.
The patient survey (Supplementary File 2) was designed to reflect the physician survey to enable responses from the two groups to be compared. It consisted of five sections examining demographics, consulting behavior and BP assessment, treatment, adherence, and attitudes/behavior toward managing high BP. BP was not directly measured for this study; patients were asked their average BP during the previous 2 weeks.
Data Analysis
Sample sizes of 130 physicians (100 cardiologists and 30 nephrologists) and 400 patients were determined to be optimal to provide statistical accuracy. Four hundred patients provided a margin of error of ±4.9 at a 95% confidence interval. Given the practical constraints of recruiting physicians (small universe size, location of the cities, and restriction to level 3 hospitals), 130 was a feasible number to achieve within the period fieldwork and that would still allow statistically relevant comparisons across the key data variables such as location and specialty type. This sample provided a margin of error of ±8.4 at 95% confidence interval.
The interview responses were manually entered into a database and underwent a thorough quality check procedure to ensure data accuracy. The data were converted into a raw SPSS (SPSS Inc, Chicago, IL) and comma‐separated value file for analysis purposes. For efficiency purposes at the data‐analysis stage, predetermined Excel tables were created from the raw SPSS file based on the key research objectives of the study. Comparisons of the physician and patient data were made where appropriate. Quality control checks were conducted on 10% of all completed interviews to ensure data quality.
Results
Study Population
The study population was recruited from 34 hospitals in Beijing (40 physicians, 131 patients), 18 hospitals in Shanghai (45 physicians, 134 patients), and 25 hospitals in Guangzhou (45 physicians, 135 patients). Of 814 physicians invited to participate, the response rate was 16.0%, with 130 physicians completing the interview (Figure 1A). Of 1525 patients invited to participate, the response rate was 26.2%, with 400 completing the interview (Figure 1B). Among eligible physicians and patients, response rates were similar (35.4% and 36.4%, respectively). Key demographic and clinical characteristics of the sample populations are shown in Table 1. The most common current treatments used by the patients were calcium channel blockers (CCBs), angiotensin receptor blockers (ARBs), and angiotensin‐converting enzyme (ACE) inhibitors. Combination therapy was used by 32% of patients, with 10% receiving single‐pill combination (SPC) therapy.
Figure 1.
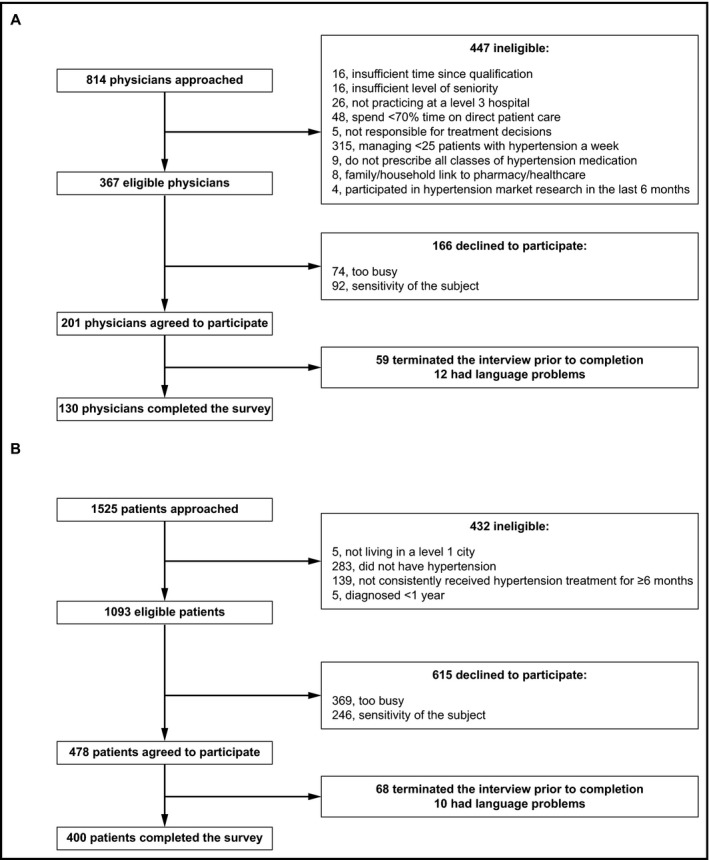
Physician (A) and patient (B) response rates.
Table 1.
Physician and Patient Demographics and Clinical Characteristics
| Physician Survey | Cardiologists (n=100) | Nephrologists (n=30) |
|---|---|---|
| Mean duration of practice, y | 17.3 | 17.1 |
| Seniority, % | ||
| Department director | 1 | 10 |
| Assistant director | 2 | 3 |
| Doctor in charge | 28 | 43 |
| Chief doctor | 12 | 3 |
| Vice chief doctor | 57 | 40 |
| Median number of hypertension patients managed per week | 60 | 50 |
| Patient classification, % | ||
| Grade 1 hypertension | 20 | 22 |
| Grade 2 hypertension | 48 | 38 |
| Grade 3 hypertension | 32 | 40 |
| Patient comorbidities | ||
| None | 30 | 17 |
| CAD | 48 | 27 |
| Stroke | 23 | 17 |
| CKD without microproteinuria | 40 | 30 |
| CKD with microproteinuria | 28 | 47 |
| Diabetes | 33 | 29 |
| Patient survey | Male (n=156) | Female (n=244) |
| Mean age, y | 57 | 59 |
| Mean BMI | 24.7 | 25.2 |
| Mean time since diagnosis, y | 6.5 | 7.6 |
| Comorbidities, % | ||
| None | 44 | 39 |
| Dyslipidemia/high blood cholesterol | 32 | 30 |
| CKD | 20 | 28 |
| CAD | 12 | 14 |
| Arrhythmia | 6 | 14 |
| Diabetes | 11 | 16 |
| Chronic heart failure | 3 | 2 |
| Stroke | 2 | 5 |
| Current medication, % | ||
| CCB | 58 | 55 |
| ARB | 29 | 34 |
| ACE inhibitor | 19 | 16 |
| Diuretic | 3 | 4 |
| Beta‐blocker | 13 | 12 |
| SPC | 12 | 9 |
| Traditional Chinese medicine | 3 | 5 |
| Alpha blocker | 1 | 1 |
Abbreviations: ACE, angiotensin‐converting enzyme; ARB, angiotensin receptor blocker; BMI, body mass index; CAD, coronary artery disease; CCB, calcium channel blocker; CKD, chronic kidney disease; SPC, single‐pill combination.
Guideline Preferences
The majority of physicians reported following the US Joint National Committee (JNC) and/or Chinese national guidelines for the diagnosis (75% and 71%, respectively), management (66% and 68%, respectively), and treatment of hypertension (70% and 72%, respectively). When asked how the guidelines could be improved, 33% of physicians indicated they would prefer them to be simpler and easier to follow, 25% thought the guidelines should contain real clinical scenarios or case studies, and 25% said they would not change the guidelines.
BP Monitoring
Physicians recommended that patients have their BP measured more than once a week (67%) or once a week (28%). All patients reported having their BP measured at a hospital, most commonly once a month (58% of patients). Home BP monitoring (HBPM) was less common, with 66% of patients having used it. Of patients who did measure their BP at home, 35% did so more than once a week. Ambulatory BP monitoring (ABPM) was uncommon; 20% of patients reported ever having done so, and of these, 75% had done so over 1 year ago. However, 88% of physicians recommended that their patients use HBPM and 95% of physicians reported typically using ABPM for diagnosing hypertension.
Target BPs and BP Control Rates
Physicians most commonly recommended a BP target of <140/90 mm Hg for patients, irrespective of the presence of comorbid conditions (Table 2). This is in accordance with the JNC 8 guidelines9; however, the Chinese national guidelines recommend a lower target of <130/80 mm Hg for patients with hypertension and comorbidities such as diabetes or chronic kidney disease (CKD).10
Table 2.
Physician‐Reported Target BP for Patient Groups
| Patient Group | Most Commonly Reported BP Target, SBP/DBP mm Hg (% of Physicians) | Target BP According to the JNC 8 Committee Guidelines,9 mm Hg | Target BP According to Chinese National Guidelines,10 mm Hg | ||
|---|---|---|---|---|---|
| 1 | 2 | 3 | |||
| Primary hypertension | <140/90 (66) | <130/80 (17) | <120/80 (8) | <140/90 | <140/90 |
| Hypertension and diabetes | <140/90 (40) | <130/80 (31) | <130/90 (8) | <140/90 | <130/80 |
| Hypertension and CAD | <140/90 (57) | <130/80 (25) | <130/90 (5) | <140/90 | <130/80 |
| Hypertension and CKD with microproteinuria | <130/90 (38) | <140/80 (38) | <120/80 (5) | <140/90 | <130/80 |
| Hypertension and CKD without microproteinuria | <140/90 (45) | <130/80 (29) | <130/85 (5) | <140/90 | <130/80 |
| Hypertension and stroke | <140/90 (60) | <130/80 (12) | <150/85 (5) | <140/90 | <140/90 |
Abbreviations: BP, blood pressure; CAD, coronary artery disease; CKD, chronic kidney disease; DBP, diastolic blood pressure; JNC 8, Eighth Joint National Committee; SBP, systolic blood pressure.
The majority of physicians (82%) claimed to inform over 80% of their patients of their target BP, with a mean of 90% of patients informed of their target. In contrast, 67% of patients stated that they had been informed of their target BP. Of these patients, 85% claimed to reach their BP target all or most of the time (Table 3). Physicians also perceived that 70% of their patients were achieving their target BP. However, according to patient‐reported average BP during the previous 2 weeks and patient‐reported BP targets, 31% of patients were achieving their target BP. Patients with primary hypertension demonstrated the greatest overestimation in BP control rates (Table 3).
Table 3.
Perceived and Actual Levels of BP Control
| Patient Group | Physician‐Perceived Percentage of Patients Achieving BP Target | Percentage of Patients Reporting to Achieve Their BP Target Every Time or Most of the Time it is Measured | Percentage of Patients Achieving BP Target According to Measurements in the Past 2 Weeks | Percentage of Physicians Completely or Somewhat Satisfied with their Patients' Level of BP Control |
|---|---|---|---|---|
| All patients | 70 | 85 | 31 | 62 |
| Primary hypertension | 77 | 95 | 28 | 93 |
| Hypertension and diabetes | 71 | 75 | 33 | 65 |
| Hypertension and CAD | 72 | 77 | 40 | 69 |
| Hypertension and CKD | 67 | 75 | 24 | 52 |
| Hypertension and stroke | 64 | 69 | 23 | 47 |
Abbreviations: BP, blood pressure; CAD, coronary artery disease; CKD, chronic kidney disease.
Physician and Patient Perspectives on BP Control
Physicians reported a high level of satisfaction with the rates of BP control among their patients (Table 3). Satisfaction was highest for patients with primary hypertension and lowest for patients with hypertension and a previous stroke.
Patient concern regarding not reaching their target BP was low. Of patients who were aware of their BP target, 56% agreed with the statement “I believe I have done my best to reach my target BP level so it is fine even if I do not reach my target levels,” 30% agreed with the statement “I am already on medication so I'm not overly concerned about reaching my target BP,” and 14% agreed with the statement “I am extremely concerned about reaching my target BP level and am very upset if I do not reach it consistently.”
Both physicians and patients expect BP control to be achieved within a short period of time. The majority of physicians (80%) expect patients to achieve their target BP within 1 to 3 weeks of initiating treatment, 48% of patients expect to achieve their target BP within 1 to 2 weeks, and 28% of patients expect to achieve it in less than a week after a change in their medication. Among patients initiating treatment for hypertension, the main reasons physicians believe they do not reach their target BP within the expected time frame are that the initial dose is not high enough (53%), a lack of patient adherence (35%), and patient comorbidities (12%). Among patients receiving ongoing treatment for hypertension, physicians believed that the most likely reasons patients do not achieve their BP target were treatment‐related AEs (83%), severity of hypertension (81%), lack of patient adherence (78%), and lack of patient education about the management of hypertension (75%). However, only 16% of patients reported ever having a treatment‐related AE and both physicians and patients reported good levels of adherence; 90% of physicians thought that patient adherence to medication was moderate or high, and 91% of patients reported missing a dose of their medication once a month or less often. Although 87% of patients said they would not adjust their medication without their physician's consent, 55% of patients stated that they would stop taking their medication without consulting their physician if they experienced an AE and 28% said they stop taking their medication when they feel better.
Overall, 88% of patients reported that they were satisfied with their current BP treatment.
Physician Prescribing Patterns
The most important factors that influenced physicians' choice of treatment were the severity of the patient's hypertension, known treatment‐related AEs, and patient comorbidities (Figure 2).
Figure 2.
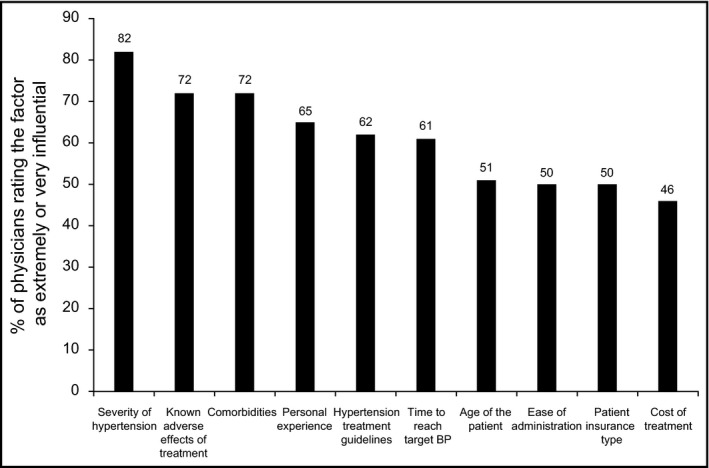
Factors that influence physicians' prescribing choices. BP indicates blood pressure.
Following a diagnosis of hypertension, 40% of physicians reported that they prescribe monotherapy, 45% combination therapy, and 15% an SPC. As initial treatment, the most commonly prescribed class of antihypertensive were CCBs (Figure 3).
Figure 3.
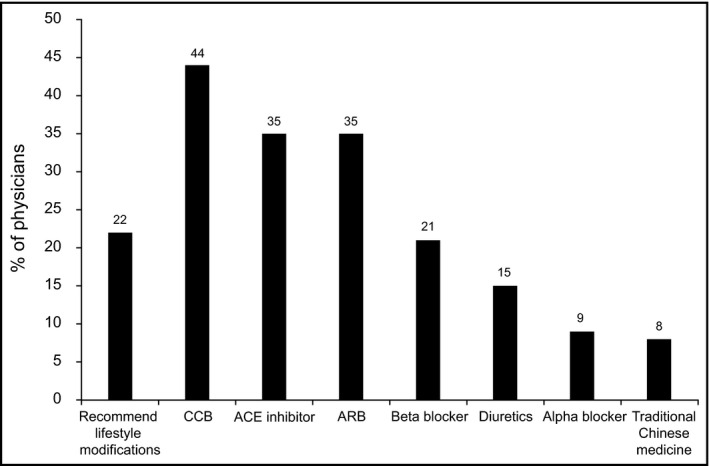
Physician‐reported initial treatment of hypertension. ACE indicates angiotensin‐converting enzyme; ARB, angiotensin receptor blocker; CCB, calcium channel blocker.
The prescribing patterns identified in the case studies suggest that physicians commonly initiate treatment for hypertension with monotherapy, irrespective of a patient's comorbidities and additional risk factors (Figure 4A, Supplementary file 3). The only patients for whom combination therapy was the most common form of initial treatment were the most complex cases: a patient with grade 2 hypertension, type 2 diabetes, and stage 3 CKD (case study 9) and a patient with grade 3 hypertension who had experienced a recent stroke (case study 10).
Figure 4.
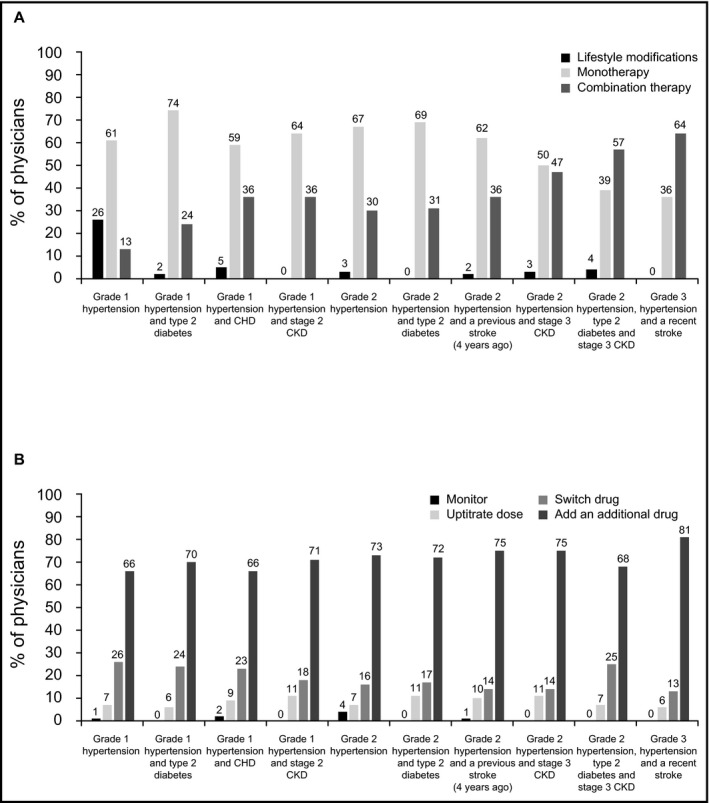
Summary of treatment of case studies. (A) Initial treatment. (B) Treatment if blood pressure (BP) remained uncontrolled. CHD indicates coronary heart disease; CKD, chronic kidney disease.
According to the case studies, if BP remained uncontrolled then physicians most frequently would choose to add an additional class of antihypertensive to the patients' treatment (66%–81% of physicians) (Figure 4B, Supplementary file 3). Fewer physicians reported that they would choose to increase the dose of the current treatment (6%–11%) or switch to another drug (13%–26%). For all case studies, less than 5% of physicians reported that they would continue to monitor a patient but not change their medication if their BP was uncontrolled.
Consultations and Support Services
Approximately two thirds of physicians and patients reported that they have follow‐up appointments once a month. According to 57% of physicians and 48% of patients, a routine consultation typically lasted between 6 and 10 minutes; 22% of physicians and 38% of patients reported shorter consultations of between 1 and 5 minutes. A total of 65% of physicians and 73% of patients thought the duration of consultations was not sufficient. Patients and physicians were in agreement that the most important topics for discussion during consultations are how to take BP medications at home, education on the risks of high BP, and lifestyle modifications to reduce BP. There was also agreement on the topics that are most commonly discussed at consultations, with the importance of taking medications as instructed, the routine use of BP monitoring, and reducing salt intake most frequently discussed.
In addition to routine physician consultations, 47% of physicians thought their patients had access to other support services such as pharmacists (26%), dieticians (26%), and nurse educators (20%). However, only 1% of patients reported that these services were available to them.
Discussion
The HAPPEN survey was a real‐world survey designed to comprehensively examine physician and patient perspectives on hypertension management in level 3 hospitals in China, with the aim of identifying aspects of care that could be associated with low BP control rates among treated patients with hypertension.
An important finding of this study is that both physicians and patients greatly overestimate the level of BP control that is being achieved. The results suggest that less than one third of the patients were reaching their target BP; however, physicians and patients believed that at least two thirds of patients achieved their target. The overestimation of BP control rates was greatest for patients with primary hypertension, suggesting that it may in part be due to the asymptomatic nature of the condition.
The overestimation of BP control rates combined with the high level of physician satisfaction with BP control rates and the lack of patient concern when they do not achieve their target BP likely contribute to poor BP control among treated patients with hypertension. These findings are not unique to China. A study conducted across numerous Asian countries found that patients believed that taking their medication and trying to achieve their BP target is sufficient, even if their BP remains uncontrolled.11 Previous studies have also found that BP control rates may be overestimated by physicians12 and physician misperception of good BP control can contribute to lack of treatment intensification.13
The results of the HAPPEN survey suggest that both physicians and patients are unaware of the ineffectiveness of their current treatment; therefore, there is no drive for the treatment intensification required to improve BP control, and this results in therapeutic inertia.
The majority of patients in the study had their BP measured once a month, the time point at which most patients would collect their repeat prescriptions from their physician. However, it is not mandatory for physicians to monitor BP at each visit. Infrequent BP monitoring may also contribute to poor BP control rates and therapeutic inertia. More frequent monitoring of BP and self‐monitoring may increase awareness of poor BP control and there is evidence to show that this can improve BP control rates and reduce therapeutic inertia.14
Low adherence to medication may also contribute to poor BP control rates. Although both physicians and patients reported good levels of adherence, it was a concern of physicians. Furthermore, when patients were questioned regarding situations where they would stop taking their medication as prescribed, such as in response to an AE, over half of patients said that they would. However, it is difficult to accurately assess the level of adherence of patients in this study as it was not directly measured.
The HAPPEN survey has generally found good alignment between physician and patient perception of hypertension management. Although physicians and patients were in agreement regarding the duration and content of routine consultations, one of the greatest discrepancies was the availability of additional support services. Approximately half of physicians thought their patients had access to services such as dieticians and pharmacists, whereas almost no patients reported having these services. Based on our experience, due to the vast number of patients who pass through level 3 hospitals, such support services are not normally available to patients. We believe this is a fundamental problem in the medical system in China. Patients may therefore be more reliant on effective use of consultation time than physicians are aware of, and, in combination with the insufficient duration of consultations, this may be contributing to the low BP control rates.
Despite substantial amounts of evidence demonstrating the benefits of combination therapy,15 the results suggest that its use is relatively low in the survey population. Although physicians stated that they initiate treatment with combination therapy for 45% of patients, only 32% of patients reported that they were currently prescribed combination therapy. This is substantially lower than the rates reported in other regions; for example, data from Europe demonstrated that 67% of all patients with hypertension and 73% of patients with comorbidities are prescribed combination therapy.15
The case study element of the HAPPEN survey has provided interesting insight into physician prescribing patterns. Although physicians stated that two of the key factors they base their prescribing decisions on are hypertension severity and comorbidities, the case studies suggest that in the majority of cases physicians initiate treatment with monotherapy irrespective of the patient's risk factors. However, if a patient's BP remains uncontrolled, the majority of physicians stated that they would prescribe combination therapy and almost all physicians claimed that they would modify the prescribed treatment in some form. This demonstrates that physicians do understand the need to intensify treatment when BP remains uncontrolled; however, in practice, the high proportion of patients with uncontrolled BP and low use of combination therapy suggests that this is not occurring and that therapeutic inertia is a major problem in China. In part, this may be due to the lack of awareness of the poor level of BP control among their patients. An additional factor that may contribute to lack of treatment intensification is that physicians reported a high degree of concern regarding treatment‐related AEs. The results of this study suggest that they may be overestimating the risk and impact of AEs as they did not seem to be a major concern of patients and only 16% of patients reported ever having experienced a treatment‐related AE.
Although the majority of physicians claimed to follow the Chinese national hypertension guidelines10 and JNC guidelines,9, 17 the results of the HAPPEN survey reveal differences between guidelines and practice. The target BPs recommended by physicians tended to follow the guidelines that were developed by members of the JNC 8 process rather than the lower targets recommended by the Chinese guidelines for patients with comorbidities. The guidelines recommend achieving target BP within several weeks to a month of initiating treatment,9, 10, 17 whereas patients and physicians expect BP control to be achieved within shorter time frames. The guidelines recommend commencing treatment for high‐risk patients with combination therapy,10, 17 whereas the results of the case studies and the low use of combination therapy in the study population suggest that this is not common practice. When BP remains uncontrolled, guidelines suggest either increasing the dose of the existing therapy or adding another drug. Although physicians reported that they would add another drug, uptitration of existing treatment appeared to be rare.
Study Limitations
Limitations of this study should be noted. The study population was sampled at level 3 hospitals in three major cities in China; therefore, the results may not be representative of physicians and patients in other locations such as rural areas or, indeed, the diverse population of China. The study also focused on patients who had a diagnosis of hypertension for at least 1 year and who had been receiving treatment for at least 6 months. The findings are not relevant to patients with hypertension who are unaware of their condition, not receiving treatment, or have more recently begun treatment for hypertension. In addition, although physicians and patients were randomly invited to take part in the survey, those who agreed to participate may not be representative of the general population. Where physician and patient responses have been compared, it is important to note that the patients who participated may not have to be treated by a physician who completed the survey; they may have been treated by another physician practicing within the same clinic.
Due to the nature of the survey it was not possible to directly measure patients' BP or treatment adherence. Although BP was not directly measured in this study, the reported rates of control (31%) are similar to those previously reported for patients at level 3 hospitals in China (30.6%),4 suggesting that the estimates used are reliable. Finally, patient‐reported adherence may be subject to bias.
Conclusions
The HAPPEN survey has provided important insight into physician, patient, and healthcare system factors that influence the management of hypertension in level 3 hospitals in China and has identified a number of factors that may contribute to the poor levels of BP control. Although physicians are aware of treatment guidelines, an overestimation of BP control rates and high levels of treatment satisfaction suggest that in practice both physicians and patients are unaware of the need to intensify their treatment regimen; therefore, therapeutic inertia is a significant problem.
Initiatives that tackle multiple aspects of hypertension management are required. In particular, the gap between perceived and actual BP control rates needs highlighting to physicians to increase awareness of this problem and stimulate change in prescribing patterns. From a patient perspective, greater patient awareness of the importance of BP control and greater involvement in the monitoring and treatment of their BP may help to improve control rates. From a physician perspective, greater appreciation of BP targets and greater use of SPCs may be two means of reducing the extent of therapeutic inertia, a global issue not unique to China.13, 18, 19, 20 Simple initiatives such as those used in the Canadian Simplified Treatment Intervention to Control Hypertension (STITCH) study21, 22 could be utilized in China to improve BP control rates. Deficiencies in the Chinese medical system contribute to many of the problems associated with the management of hypertension identified in this study and reform is urgently required.
Supporting information
File S1. Physician questionnaire.
File S2. Patient questionnaire.
Case study 1. Primary grade 1 hypertension.
Case study 2. Grade 1 hypertension and diabetes.
Case study 3. Grade 1 hypertension and CHD.
Case study 4. Grade 1 hypertension and stage 2 CKD.
Case study 5. Grade 2 hypertension.
Case study 6. Grade 2 hypertension and diabetes.
Case study 7. Grade 2 hypertension and prior stroke.
Case study 8. Grade 2 hypertension and stage 2 CKD.
Case study 9. Grade 2 hypertension stage 3 CKD.
Case study 10. Grade 2 hypertension and stroke.
Disclosure
All authors have received advisory board honoraria from Bayer HealthCare. RDF has received honoraria from Bayer, Servier, and Valeant. YZ has received honoraria from Novartis, Sanofi, Daiichi‐Sankyo, and AstraZeneca.
The study and data analyses were conducted by Will Tolley and Marc Yates of Research Partnership, and were funded by Bayer HealthCare. Medical writing assistance was provided by Katie White, PhD, of Fishawack Communications Ltd, UK, and was funded by Bayer HealthCare.
Authors' contributions
All authors contributed to the design of the study, analysis, and interpretation of the data. All authors participated in the drafting and revising of the manuscript, approved the final version, and agreed to be accountable for the work.
J Clin Hypertens (Greenwich). 2017;19:256–264. 10.1111/jch.12912 © 2016 The Authors. The Journal of Clinical Hypertension published by Wiley Periodicals, Inc.
References
- 1. World Health Organization . Global status report on noncommunicable diseases, 2010. http://www.whoint/nmh/publications/ncd_report2010/en/. Accessed October 2015. [DOI] [PubMed]
- 2. Kjeldsen S, Feldman RD, Lisheng L, et al. Updated national and international hypertension guidelines: a review of current recommendations. Drugs. 2014;74:2033–2051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Guo F, He D, Zhang W, Walton RG. Trends in prevalence, awareness, management, and control of hypertension among United States Adults, 1999 to 2010. J Am Coll Cardiol. 2012;60:599–606. [DOI] [PubMed] [Google Scholar]
- 4. Hu DY, Liu L, Yu JM, Yao CH; China STATUS Study Group . National survey of blood pressure control rate in Chinese hypertensive outpatients–China STATUS. Zhonghua Xin Xue Guan Bing Za Zhi. 2010;38:230–238. [PubMed] [Google Scholar]
- 5. Marshall IJ, Wolfe CD, McKevitt C. Lay perspectives on hypertension and drug adherence: systematic review of qualitative research. BMJ. 2012;345:e3953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Aujoulat I, Jacquemin P, Rietzschel E, et al. Factors associated with clinical inertia: an integrative review. Adv Med Edu Prac. 2014;5:141–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lebeau JP, Cadwallader JS, Aubin‐Auger I, et al. The concept and definition of therapeutic inertia in hypertension in primary care: a qualitative systematic review. BMC Fam Pract. 2014;15:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.European Society for Opinion and Marketing Research. European Society for Opinion and Marketing Research (ESOMAR) guidelines, 2015. https://www.esomar.org/uploads/public/knowledge-and-standards/codes-and-guidelines/ICCESOMAR_Code_English_.pdf. Accessed October 2015.
- 9. James PA, Oparil S, Carter BL, et al. 2014 evidence‐based guideline for the management of high blood pressure in adults: report from the panel members appointed to the eighth joint national committee (JNC 8). JAMA. 2014;311:507–520. [DOI] [PubMed] [Google Scholar]
- 10. Liu LS. 2010 Chinese guidelines for the management of hypertension. Zhonghua Xin Xue Guan Bing Za Zhi. 2011;39:579–615. [PubMed] [Google Scholar]
- 11. Rahman AR, Wang JG, Kwong GM, et al. Perception of hypertension management by patients and doctors in Asia: potential to improve blood pressure control. Asia Pacific Fam Med. 2015;14:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rose AJ, Shimada SL, Rothendler JA, et al. The accuracy of clinician perceptions of “usual” blood pressure control. J Gen Intern Med. 2008;23:180–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Alonso‐Moreno FJ, Llisterri Caro JL, Rodríguez‐Roca GC, et al. Primary care physicians behaviour on hypertensive patients with poor blood pressure control. The PRESCAP 2006 study. Rev Clin Esp. 2008;208:393–399. [DOI] [PubMed] [Google Scholar]
- 14. Agarwal R, Bills JE, Hecht TJ, Light RP. Role of home blood pressure monitoring in overcoming therapeutic inertia and improving hypertension control: a systematic review and meta‐analysis. Hypertension. 2011;57:29–38. [DOI] [PubMed] [Google Scholar]
- 15. Wald DS, Law M, Morris JK, Bestwick JP, Wald NJ. Combination therapy versus monotherapy in reducing blood pressure: meta‐analysis on 11,000 participants from 42 trials. Am J Med. 2009;122:290–300. [DOI] [PubMed] [Google Scholar]
- 16. Roas S, Bernhart F, Schwarz M, et al. Antihypertensive combination therapy in primary care offices: results of a cross‐sectional survey in Switzerland. Int J Gen Med. 2014;7:549–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. [DOI] [PubMed] [Google Scholar]
- 18. Escobar C, Barrios V, Alonso‐Moreno FJ, et al. Evolution of therapy inertia in primary care setting in Spain during 2002‐2010. J Hypertens. 2014;32:1138–1145. [DOI] [PubMed] [Google Scholar]
- 19. Ferrari P. Reasons for therapeutic inertia when managing hypertension in clinical practice in non‐Western countries. J Hum Hypertens. 2008;23:151–159. [DOI] [PubMed] [Google Scholar]
- 20. Ogedegbe G. Barriers to optimal hypertension control. J Clin Hypertens (Greenwich). 2008;10:644–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Feldman RD, Zou GY, Vandervoort MK, et al. A simplified approach to the treatment of uncomplicated hypertension: a cluster randomized, controlled trial. Hypertension. 2009;53:646–653. [DOI] [PubMed] [Google Scholar]
- 22. Nelson SA, Dresser GK, Vandervoort MK, et al. Barriers to blood pressure control: a STITCH substudy. J Clin Hypertens (Greenwich). 2011;13:73–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
File S1. Physician questionnaire.
File S2. Patient questionnaire.
Case study 1. Primary grade 1 hypertension.
Case study 2. Grade 1 hypertension and diabetes.
Case study 3. Grade 1 hypertension and CHD.
Case study 4. Grade 1 hypertension and stage 2 CKD.
Case study 5. Grade 2 hypertension.
Case study 6. Grade 2 hypertension and diabetes.
Case study 7. Grade 2 hypertension and prior stroke.
Case study 8. Grade 2 hypertension and stage 2 CKD.
Case study 9. Grade 2 hypertension stage 3 CKD.
Case study 10. Grade 2 hypertension and stroke.


