Abstract
Objectives
The Joint United Nations Programme on HIV/AIDS (UNAIDS)/World Health Organization (WHO) 90‐90‐90 goals propose that 90% of all people living with HIV should know their HIV status, 90% of those diagnosed should receive antiretroviral therapy (ART), and 90% of those should have durable viral suppression. We have estimated the continuum of HIV care for the entire HIV‐1‐infected population in Sweden.
Methods
The Swedish InfCare HIV Cohort Study collects viral loads, CD4 counts, and viral sequences, along with demographic and clinical data, through an electronic clinical decision support system. Almost 100% of those diagnosed with HIV infection are included in the database, corresponding to 6946 diagnosed subjects living with HIV‐1 in Sweden by 31 December 2015.
Results
Using HIV surveillance data reported to the Public Health Agency of Sweden, it was estimated that 10% of all HIV‐infected subjects in Sweden remain undiagnosed. Among all diagnosed patients, 99.8% were linked to care and 97.1% of those remained in care. On 31 December 2015, 6605 of 6946 patients (95.1%) were on ART. A total of 6395 had been on treatment for at least 6 months and 6053 of those (94.7%) had a viral load < 50 HIV‐1 RNA copies/mL.
Conclusions
The 2014 UNAIDS/WHO 90‐90‐90 goals for HIV care means that > 73% of all patients living with HIV should be virologically suppressed by 2020. Sweden has already achieved this target, with 78% suppression, and is the first country reported to meet all the UNAIDS/WHO 90‐90‐90 goals.
Keywords: antiretroviral treatment, continuum of care, HIV, treatment cascade
Introduction
Antiretroviral therapy (ART) has dramatically reduced the HIV‐related mortality, morbidity, and infectiousness of treated patients. For viral suppression, a good clinical outcome, and a significant public health impact, HIV‐infected individuals must meet several targets along the HIV care continuum. In October 2014, the UNAIDS/WHO 90‐90‐90 treatment goals proposed that by 2020 90% of all people living with HIV should know their HIV status, 90% of those diagnosed should receive ART, and 90% of those should have durable viraological suppression. When this three‐part target is achieved, at least 73% of all HIV‐infected people world‐wide will be virally suppressed – a two‐ to three‐fold increase over current estimates 1.
The process of achieving viral suppression proceeds through a five‐stage administration cascade of care or HIV care continuum: diagnosis, linkage to care, retention in care, administration of ART, and viral suppression.
It has been estimated that, of all the HIV‐infected individuals in the USA, approximately 14% are unaware of their infection, and only 19% to 30% are virally suppressed 2, 3.
In 2014, Raymond et al. 4 reported large disparities in HIV treatment cascades between eight (mostly European) countries. The percentage of infected people with undetectable HIV RNA ranged from 20% in Georgia to 59% in Denmark. In a recent analysis of 12 national‐level treatment cascades, none achieved the UNAIDS goal of 73% of all HIV‐infected individuals having a suppressed viral load. Switzerland was closest at 68%, followed by Australia (62%) and the UK (61%) 5. Switzerland reported that 19% of people living with HIV were unaware of their infection, but linkage to and retention in care were high; 91% of those in care received ART, and 93% of them had a viral load < 50 HIV‐1 RNA copies/mL 6.
We have estimated the continuum of HIV care for the entire HIV‐1‐infected population in Sweden.
Methods and results
The Swedish InfCare HIV Cohort Study, established in 2003, collects viral loads, CD4 cell counts, and viral sequences, along with demographic and clinical data, through an electronic clinical decision support system (InfCare HIV®, Stockholm, Sweden). The implementation was finalized in all HIV care centres in 2008 7. The percentages of patients diagnosed with HIV and linked to care are included in the InfCare HIV database, corresponding to 6946 diagnosed subjects living with HIV‐1 in Sweden by 31 December 2015.
The six levels within the spectrum of engagement in HIV care 6 were separately analysed:
HIV‐infected;
HIV‐diagnosed;
linked to care;
retained in care;
on ART;
having suppressed viral load (< 50 copies/mL).
Using HIV surveillance data, the Public Health Agency of Sweden has recently estimated that 90% of those in Sweden infected with HIV have been diagnosed 8, so that < 8000 individuals are now living with HIV in Sweden.
All new HIV diagnoses are reported to the Public Health Agency by both the laboratory and the treating physician. To estimate linkage to care, we manually reviewed all cases reported from 1 January to 31 December 2014. Out of 471 cases, 469 were entered into InfCare HIV and linked to an HIV care centre. One patient with tuberculosis at diagnosis was admitted to an infectious disease clinic, but left the country prior to being discharged from the hospital or visiting the HIV clinic. Another patient was diagnosed by a forensic medical department and never included in InfCare HIV, and therefore considered lost to follow‐up. Thus, 99.8% of patients diagnosed with HIV during 2014 were linked to HIV care.
To study retention in care, we analysed 661 new cases entered into InfCare HIV in 2013 to 2014. In December 2015, 612 were still active in InfCare HIV and had ongoing contact with a national HIV centre. Out of 49 deregistered subjects, 40 had either moved abroad (n = 29) or died (n = 11) and were thus excluded. Nine patients were lost to follow‐up. Another nine with no registered laboratory HIV monitoring during the last 9 months were considered lost to follow‐up. Accordingly, 603 of 621 patients (97.1%) were linked and retained in care.
On 31 December 2015, 6605 of 6946 patients (95.1%) were on ART. A total of 6395 had been on treatment for at least 6 months and 6053 of those (94.7%) had a viral load < 50 copies/mL. Ninety‐eight patients on treatment had a viral load > 200 copies/mL, giving 98.5% with a viral load < 200 copies/mL. Most patients with HIV RNA between 50 and 200 copies/mL (n = 244) were assumed to have had a viral blip and would probably be suppressed at the next measurement 9.
Conclusions
The Swedish continuum of HIV care is shown in Figure 1. In summary, the UNAIDS/WHO 90‐90‐90 coverage target of 73% of HIV‐infected individuals with undetectable HIV RNA has been achieved, with 90% of all those infected diagnosed, 83% of those infected on ART, and 78% of those infected with a suppressed viral load (< 50 copies/mL).
Figure 1.
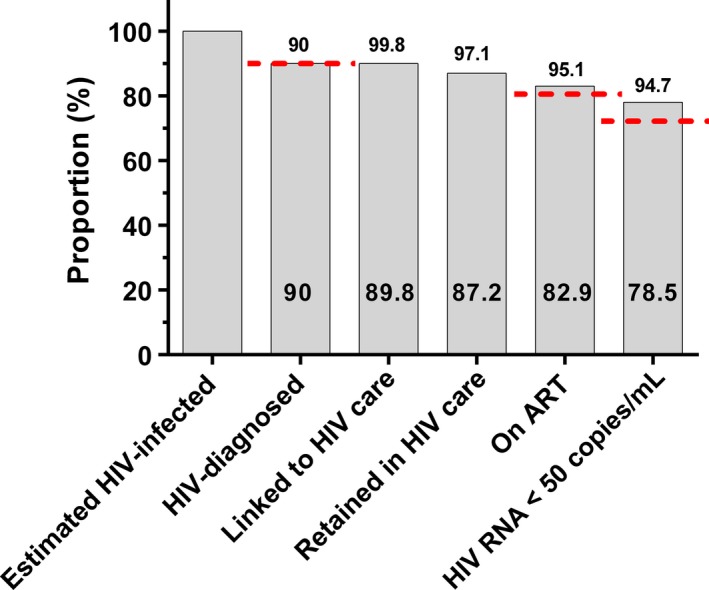
The Swedish HIV continuum of care 2015, showing the estimated proportion of all HIV‐1‐infected subjects in Sweden achieving various goals of engagement in HIV care. Red horizontal lines indicate 2014 Joint United Nations Programme on HIV/AIDS (UNAIDS)/World Health Organization (WHO) 90‐90‐90‐targets. Numbers above bars indicate the proportion of the number at the previous level; numbers within bars indicate the proportion of all HIV‐infected individuals. ART, antiretroviral therapy.
Several factors probably contribute to these favourable results. Sweden is a low‐endemic country, with < 8000 individuals estimated to be HIV‐infected; the Swedish Communicable Diseases Act obliges laboratories and clinics to report cases and patients must keep appointments and submit to tests that health care providers consider necessary; all HIV‐infected patients are linked to specialized HIV care centres with dedicated multidisciplinary teams of physicians, nurses, and social workers; the InfCare HIV clinical database facilitates high‐quality care and treatment; ART is prescribed free of charge for the patient; and adherence to national HIV treatment guidelines is high. Since 2014, these guidelines recommend treating all HIV‐infected individuals irrespective of CD4 cell count 10.
We believe that Sweden is the first country to achieve all the UNAIDS/WHO 90‐90‐90 goals. The estimations of the clinical targets − linkage to and retention in care, ART coverage, and ART viral suppression − are high compared with earlier reports. Previous studies have used different methodologies to estimate percentages at the various steps in the continuum of HIV care, and several reports have been based on unreliable data sources. We used a similar approach to that used in the recently published study from the Swiss HIV Cohort 6. The comprehensive National Quality Registry InfCare HIV makes the credibility of our data very high. While estimating how many individuals are unaware of their infection is uncertain, even using older approximations that 15% are unaware of it 11, the coverage target of 73% would have been met. We used 50 copies/mL as the cut‐off for viral suppression, whereas using 200 copies/mL, as in many other studies, would have resulted in even greater coverage.
However, we should not be content with these good results, but should continue to improve prevention strategies and increase our efforts to diagnose those still unaware of their infection.
Acknowledgements
This work was supported by the Swedish Research Council (2012‐3476), Stockholm County Council (20130042), and Sahlgrenska University Hospital (ALFGBG‐430271).
References
- 1. WHO . 90–90–90. An ambitious treatment target to help end the AIDS epidemic; 2014. http://www.unaids.org/sites/default/files/media_asset/90-90-90_en_0.pdf, October, 2014.
- 2. Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test‐and‐treat strategies for prevention of HIV infection. Clin Infect Dis 2011; 52: 793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hall HI, Frazier EL, Rhodes P et al Differences in human immunodeficiency virus care and treatment among subpopulations in the United States. JAMA Intern Med 2013; 173: 1337–1344. [DOI] [PubMed] [Google Scholar]
- 4. Raymond A, Hill A, Pozniak A. Large disparities in HIV treatment cascades between eight European and high‐income countries ‐ analysis of break points. J Int AIDS Soc 2014; 17: 19507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Levi J, Raymond A, Pozniak A et al Can the UNA IDS 90‐90‐90 target be reached? Analysis of 12 national level HIV treatment cascades (MOAD0102). IAS 2015. Vancouver, Canada, 2015.
- 6. Kohler P, Schmidt AJ, Cavassini M et al The HIV care cascade in Switzerland: reaching the UNAIDS/WHO targets for patients diagnosed with HIV. AIDS 2015; 29: 2509–2515. [DOI] [PubMed] [Google Scholar]
- 7. Helleberg M, Haggblom A, Sonnerborg A, Obel N. HIV care in the Swedish‐Danish HIV cohort 1995‐2010, closing the gaps. PLoS One 2013; 8: e72257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. European Centre for Disease Prevention and Control . Thematic report: HIV continuum of care. Monitoring implementation of the Dublin Declaration on Partnership to Fight HIV/AIDS in Europe and Central Asia: 2014 progress report. Stockholm: ECDC; 2015. http://ecdc.europa.eu/en/publications/Publications/dublin-declaration-continuum-of-care-2014.pdf, September, 2015.
- 9. Sörstedt E, Nilsson S, Blaxhult A, Gisslén M, Flamholc L, Sönner borg A, Yilmaz A. Viral blips during suppressive antiretroviral treatment are associated with high baseline HIV‐1 RNA levels. BMC Infect Dis 2016; 16: 305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Referensgruppen för Antiviral Terapi (RAV) . Antiretroviral behandling av HIV‐infektion 2014, uppdaterad version – Behandlingsrekommendation. http://www.sls.se/Global/RAV/Dokument/RAV_HIV_2014_final_141114.pdf, October, 2014.
- 11. Bengtsson L, Blaxhult A. Uppskattning av antalet hivpositiva i Sverige. Epi‐aktuellt. Vol 6. http://www.folkhalsomyndigheten.se/nyheter-och-press/historik-smi-2003-2013/historik-epi-aktuellt/epi-aktuellt-2007/epi-aktuellt-vol-6-nr-42-18-oktober-2007/, October, 2007.


