Abstract
Background:
Propofol is associated with pain during injection, which is stressful to patients. The present study was designed to investigate the analgesic effect of pretreatment with remifentanil and esmolol in minimizing propofol injection pain, compared with placebo.
Methods:
In a randomized, double-blind, prospective trial, 120 patients, scheduled for elective dental surgery under general anesthesia, were randomized to 1 of the 4 treatment arms (n = 30 each) receiving normal saline, remifentanil 0.35 μg/kg, esmolol 0.5 mg/kg, and 1 mg/kg before administration of propofol. During injection of 1% propofol 0.5 mg/kg, pain was evaluated by a 4-point score (0 = none, 1 = mild, 2 = moderate, 3 = severe). Any adverse effects such as hypotension and bradycardia were recorded during the perioperative periods.
Results:
In all, 120 patients completed this study. There were no significant differences in terms of demographic data. The incidence of pain on injection of propofol was 11 (36.7%) with remifentanil 0.35 μg/kg, 12 (40%) with esmolol 0.5 mg/kg, and 11 (36.7%) with esmolol 1 mg/kg, compared with 25 (83.3%) with normal saline (respectively, P < 0.05). There were no significant differences in the incidence of pain between groups with remifentanil 0.35 μg/kg, and esmolol 0.5 mg/kg and 1 mg/kg. There were no emergence reactions such as hypotension and bradycardia in all groups.
Conclusions:
Pretreatment with esmolol 0.5 mg/kg and 1 mg/kg and remifentanil 0.35 μg/kg equally decreased pain during propofol injection.
Keywords: esmolol, injection, intravenous, pain, propofol, remifentanil
1. Introduction
Propofol is a short-acting intravenous hypnotic agent, which is widely used for sedation and general anesthesia. However, pain during injection of propofol can occur in up to 80% of patients, which can be very stressful to patients.[1–3] Many methods including cooling or diluting the propofol solution or the concomitant use of drugs such as methylene blue, pregabalin, or magnesium sulfate have been used to reduce this pain.[1–3] However, these treatments cannot alleviate the pain, which remains a challenge. It was reported that aqueous free propofol could be responsible for injection pain. Therefore, propofol long-chain triglycerides (LCTs)/medium-chain triglycerides (MCTs) were introduced to minimize injection pain, which has less concentration of aqueous free propofol than propofol-LCT.[4] This new formulation of propofol is more expensive than standard propofol. However, pain on injection still occurs despite use of propofol-LCT/MCT.[5,6]
Remifentanil is a potent, short-acting intravenous opioid. Pretreatment with small dose of remifentanil has been demonstrated to be effective in reducing pain from propofol injection without side effects.[7,8] Esmolol, a short-acting β1 adrenergic receptor antagonist, is widely used to reduce cardiovascular stress response to layngoscopy and tracheal intubation.[9–11] It was shown that perioperative infusion of esmolol reduced anesthetic requirement for surgery [12] and postoperative analgesic consumption.[13,14] Recently, it was reported that pretreatment with esmolol 0.5 mg/kg has analgesic effect on rocuronium injection pain without side effects.[15]
The present study was designed to compare the analgesic effect of pretreatment with remifentanil 0.35 μg/kg, and esmolol 0.5 mg/kg and 1 mg/kg in minimizing pain during injection of propofol-LCT, compared with placebo.
2. Methods
2.1. Patients and exclusion criteria
In all, 120 patients aged 18 to 70 years, American Society of Anesthesiologists physical status I and II, scheduled for elective dental surgery requiring general anesthesia were included. We excluded patients who have cardiac, neurologic or psychiatric problem, patients who had analgesic or sedative agents within 24 hours before surgery, and patients requiring a rapid sequence induction.
2.2. Anesthesia and data collection
The present study was approved by the Ethics Committee of Kyungpook National University Hospital (KNUH 2013–05–003–001) and informed written consent was obtained from all patients. This study was registered in the ClinicalTrials.GOV (NCT01885364). Premedication was not given. On arrival in the operating room, electrocardiogram, noninvasive blood pressure, and pulse oximetry were measured, and a 22-gauge catheter was inserted into a dorsal vein of the patient's nondominant hand. Using a computer-generated table, patients were randomized to 1 of the 4 treatment arms (n = 30 each) receiving normal saline, remifentanil 0.35 μg/kg, esmolol 0.5 mg/kg and 1 mg/kg as pretreatment. A study-blinded nurse prepared pretreatment substance using identically coded syringes at room temperature.
Pretreatment substances were injected over 10 seconds. Thirty seconds after injection of pretreatment drug, patients received propofol-LCT 0.5 mg/kg at rate of 0.5 mL/sec using syringe pump. A study-blinded anesthesiologist measured score of injection pain of propofol using a 4-point scale (0 = none [negative response to questioning], 1 = mild pain [pain reported in response to questioning only, without any behavioral sign], 2 = moderate pain [pain reported in response to questioning and accompanied by a behavioral sign, or pain reported simultaneously without questioning], 3 = severe pain [strong vocal response or response accompanied by facial grimacing, arm withdrawal or tears]).[2] Thereafter, propofol-LCT1.5 mg/kg and rocuronium 0.8 mg/kg were administered for tracheal intubation, and anesthesia was maintained with desflurane 4% to 7% in 50% N2O/O2. Emergence reactions associated with pretreatment substances such as hypotension and bradycardia were recorded. In the present study, the incidence and severity of pain after propofol injection was the primary outcome, and all other variables were secondary outcomes.
2.3. Sample size
On the basis of previously published data,[1] we estimated the incidence of pain during propofol injection in the placebo group to be around 80%. A 40% difference (80%–40%) between placebo group and treatment groups would be considered of clinical significance. Using a 2-tailed test of the proportions with α error of 0.05 and β error of 0.8, 30 patients per group were required to detect such difference.
2.4. Statistical analysis
Data were analyzed using statistical software (SPSS, version 23.0 for Windows; SPSS, Chicago, IL). The factorial analysis of variance was used for age and weight. Fisher exact test or the chi-square test was used for sex, incidence of pain, and incidence of side effects. P < 0.05 was considered to indicate statistical significance. SPSS (version 16.0) was used for statistical analysis.
3. Results
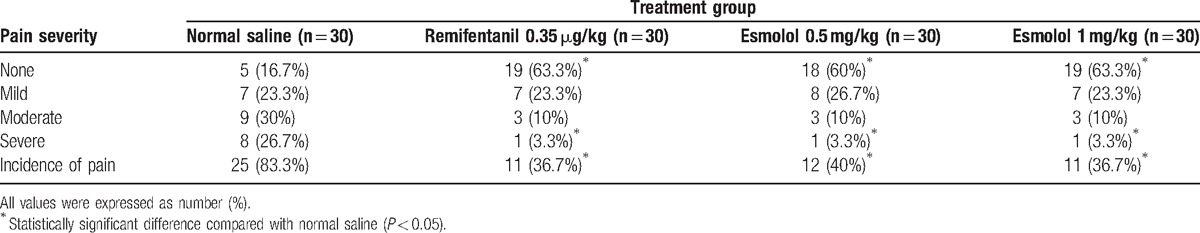
In all, 120 patients completed the study (Fig. 1). There was no difference in demographic data between groups (Table 1). The overall incidence of pain after propofol injection is demonstrated in Table 2. The incidence of pain during propofol injection was significantly reduced with remifentanil 0.35 μg/kg (36.7%), esmolol 0.5 mg/kg (40%) and 1 mg/kg (36.7%), compared with placebo group (83.3%) (respectively, P < 0.05). In addition, pretreatment with remifentanil (3.3%), and esmolol 0.5 mg/kg (3.3%) and 1 mg/kg (3.3%) significantly decreased the incidence of severe injection pain, compared with placebo (26.7%) (respectively, P < 0.05). There were no emergence reactions associated with pretreatment substances such as hypotension and bradycardia in all groups.
Figure 1.
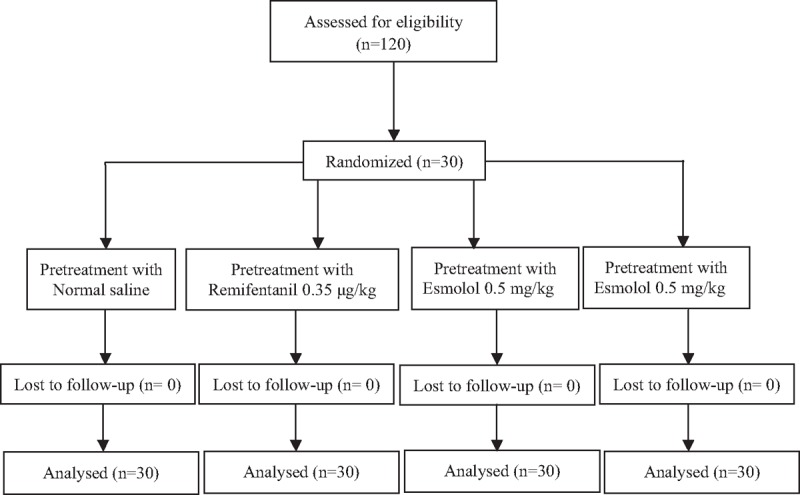
Flow diagram of the study.
Table 1.
Demographic characteristics of the study population (n = 120).
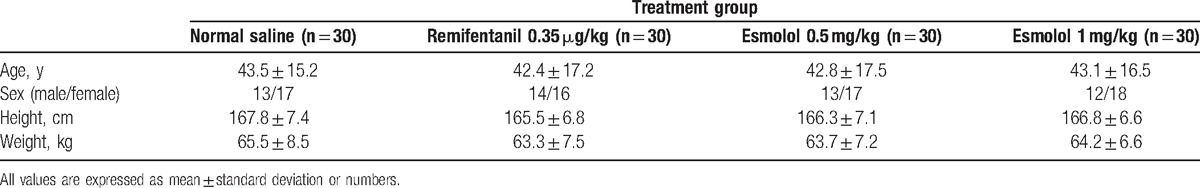
Table 2.
Incidence and pain severity during injection of propofol.
4. Discussion
This study showed that pretreatment with remifentanil 0.35 μg/kg, and esmolol 0.5 mg/kg and 1 mg/kg, was equally effective to reduce pain during propofol injection, compared with placebo.
Propofol formulated in a lipid emulsion is widely used in various clinical procedures. But propofol is associated with high incidence of pain at injection site, which is often very stressful to patients.[1–3] The exact mechanism of pain on propofol injection is unknown. The direct exposure of nociceptive receptors or free nerve ending in the vein by free propofol can increase the pain on injection.[16,17] Propofol-LCT/MCT was specially proposed to decrease injection pain. Varghese et al[18] reported that when added with lidocaine, both propofol-LCT/MCT and propofol-LCT had similar incidence of injection pain. By a systemic review and meta-analysis in 2011, pretreatment with a small dose of opioids halved the incidence of pain after propofol injection, which can generally be recommended.[19] The previous study demonstrated that pretreatment with remifentanil 0.35 μg/kg reduced injection pain of propofol by 38.8% without any side effects.[8,19] In the present study, the incidence of pain from propofol injection was 33.3% in the patients who received remifentanil 0.35 μg/kg, which is consistent with the previous study.[8]
Esmolol, antagonist of β1 adrenergic receptor, is often used to blunt adrenergic response to perioperative stimuli.[10–14,20] It was demonstrated that a single injection of esmolol 1 to 2 mg/kg is effective to attenuate the increase of heart rate after intubation without adverse effects.[10] In the previous studies, intraoperative infusion of esmolol decreased the requirement of opioid and inhalation anesthetic without causing hemodynamic change,[12] and reduced postoperative analgesic consumption.[13,14] Up to date, the exact analgesic mechanism of β adrenergic receptor antagonist remains unclear. Adrenal hormone, commonly known as stress hormone, increases during emotional distress and anxiety, which are associated with activation of hypocampal neurons.[21,22] β adrenergic receptors are involved in learning-facilitated plasticity in the mammalian hippocampus, which requires activation of N-methyl-d-aspartate (NMDA) receptor.[23,24] The activation of NMDA receptor in the hippocampus is involved in nociceptive processing, at least, in part. Therefore, esmolol with lipophilic property can decrease adrenergic activity in the hippocampus.[25] In addition, it was found that esmolol can facilitate inhibitory transmitter release in spinal trigeminal nucleus, which produces analgesic effects.[26] In the present study, pretreatment with esmolol 0.5 mg/kg and 1 mg/kg and remifentanil 0.35 μg/kg equally decreased pain during propofol injection.
The incidence of pain when propofol was injected into vein of the dorsum of hand can reach as high as 80%.[1,19] Therefore, it was considered unethical to use placebo in this study. Pretreatment substances such as remifentanil and esmolol can cause dose-dependent decrease in blood pressure and heart rate. Therefore, a placebo group was included to investigate the adverse effect of the pretreatment substances. In the present study, there were no emergence reactions associated with pretreatment with remifentanil 0.35 μg/kg, and esmolol 0.5 mg/kg and 1 mg/kg. These results were compatible with the previous studies.[8,10]
The present study had some limitations. In the present study, premedication, such as sedatives, was not given. This might increase the patient's anxiety and dissatisfaction about anesthetic care.[27] The previous study showed that 87% of patients who did not receive anxiolytic premedication reported the recall about injection pain after propofol injection.[28] Therefore, another study is needed to examine the patient's satisfaction about anesthetic care and the incidence of recall for pain during propofol injection.
5. Conclusions
In conclusion, pretreatment with esmolol 0.5 mg/kg and 1 mg/kg, and remifentanil 0.35 μg/kg were equally effective in reducing pain during injection of propofol without adverse effects.
Footnotes
Abbreviations: LCT = long-chain triglyceride, MCT = medium-chain triglyceride, NMDA = N-methyl-d-aspartate.
The authors have no competing interests to disclose.
References
- [1].Salman AE, Salman MA, Saricaoglu F, et al. Pain on injection of propofol: a comparison of methylene blue and lidocaine. J Clin Anesth 2011;23:270–4. [DOI] [PubMed] [Google Scholar]
- [2].Choi E, Kim D, Jeon Y. Comparative study between 2 different doses of pregabalin and lidocaine on pain following propofol injection: a double-blind, randomized clinical consort study. Medicine (Baltimore) 2016;95:e5153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Li M, Zhao X, Zhang L. Effects and safety of magnesium sulfate on propofol-induced injection pain, a meta-analysis of randomized controlled trials. Int J Clin Exp Med 2015;15:6813–21. [PMC free article] [PubMed] [Google Scholar]
- [4].Doenicke AW, Roizen MF, Rau J, et al. Pharmacokinetics and pharmacodynamics of propofol in a new solvent. Anesth Analg 1997;85:1399–403. [DOI] [PubMed] [Google Scholar]
- [5].Schaub E, Kern C, Landau R. Pain on injection: a double-blind comparison of propofol with lidocaine pretreatemt versus propofol formulated with long-and medium-chain triglycerides. Anesth Analg 2004;99:1699–702. [DOI] [PubMed] [Google Scholar]
- [6].Krobbuaban B, Siriwan D, Kumkeaw S. Does addition of lidocaine to medium- and long-chain triglyceride propofol emulsions significantly reduce pain on injection? J Med Assoc Thai 2008;91:383–7. [PubMed] [Google Scholar]
- [7].Iyilikci L, Balkan BK, Gokel E, et al. The effects of alfentanil or remifentanil pretreatment on propofol injection pain. J Clin Anesth 2004;16:499–502. [DOI] [PubMed] [Google Scholar]
- [8].Kwak K, Kim J, Park S, et al. Reduction of pain on injection of propofol: combination of pretreatment of remifentanil and premixture of lidocaine with propofol. Eur J Anaesthesiol 2007;24:746–50. [DOI] [PubMed] [Google Scholar]
- [9].Fernandez-Galinski S, Bermejo S, Mansilla R, et al. Comparative assessment of the effects of alfentanil, esmolol or clonidine when used as adjuvants during induction of general anaesthesia. Eur J Anaesthesiol 2004;21:476–82. [DOI] [PubMed] [Google Scholar]
- [10].Kindler CH, Schumacher PG, Schneider MC, et al. Effects of intravenous lidocaine and/or esmolol on hemodynamic responses to laryngoscopy and intubation: a double-blind, controlled clinical trial. J Clin Anesth 1996;8:491–6. [DOI] [PubMed] [Google Scholar]
- [11].Menigaux C, Guignard B, Adam F, et al. Esmolol prevents movement and attenuates the BIS response to orotracheal intubation. Br J Anaesth 2002;89:857–62. [DOI] [PubMed] [Google Scholar]
- [12].Johansen JW, Schneider G, Windsor AM, et al. Esmolol potentiates reduction of minimum alveolar isoflurane concentration by alfentanil. Anesth Analg 1998;87:671–6. [DOI] [PubMed] [Google Scholar]
- [13].Chia YY, Chan MH, Ko NH, et al. Role of beta-blockade in anaesthesia and postoperative pain management after hysterectomy. Br J Anaesth 2004;93:799–805. [DOI] [PubMed] [Google Scholar]
- [14].Haghighi M, Sedighinejad A, Mirbolook A, et al. Effect of intravenous intraoperative esmolol on pain management following lower limb orthopedic surgery. Korean J Pain 2015;28:198–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Yavascaoglu B, Kaya FN, Ozcan B. Esmolol pretreatment reduces the frequency and severity of pain on injection of rocuronium. J Clin Anesth 2007;19:413–7. [DOI] [PubMed] [Google Scholar]
- [16].Iwama H, Nakane M, Ohmori S. Nafamostat mesilate, a kallikrein inhibitor, prevents pain on injection with propofol. Br J Anaesth 1998;81:963–4. [DOI] [PubMed] [Google Scholar]
- [17].Kim DH, Chae YJ, Chang HS, et al. Intravenous lidocaine pretreatment with venous occlusion for reducing microemulsion propofol induced pain: comparison of three doses of lidocaine. J Int Med Res 2014;42:368–75. [DOI] [PubMed] [Google Scholar]
- [18].Varghese E, Krishna HM, Nittala A. Does the newer preparation of propofol, an emulskon of medium/long chain trigrlycerides cause less injection pain in children when premixed with lignocaine? Paediatr Anaesth 2010;20:338–42. [DOI] [PubMed] [Google Scholar]
- [19].Jalota L, Kalira V, George E. Prevention of pain on injection of propofol: systematic review and meta-analysis. BMJ 2011;342:d1110. [DOI] [PubMed] [Google Scholar]
- [20].Ozturk T, Kaya H, Aran G, et al. Postoperative beneficial effects of esmolol in treated hypertensive patients undergoing laparoscopic cholecystectomy. Br J Anaesth 2008;100:211–4. [DOI] [PubMed] [Google Scholar]
- [21].Sinha R, Lacadie C, Skudlarski P, et al. Neural circuits underlying emotional distress in humans. Ann N Y Acad Sci 2004;1032:254–7. [DOI] [PubMed] [Google Scholar]
- [22].Surguladze SA, Brammer MJ, Young AW, et al. A preferential increase in the extrastriate response to signals of danger. NeuroImage 2003;19:1317–28. [DOI] [PubMed] [Google Scholar]
- [23].Hansen N, Manahan-Vaughan D. Hippocampal long-term potentiation that is elicited by perforant path stimulation or that occurs in conjunction with spatial learning is tightly controlled by beta-adrenoreceptors and the locus coeruleus. Hippocampus 2015;25:1285–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].MacDonald JF, Jackson MF, Beazely MA. Hippocampal long-term synaptic plasticity and signal amplification of NMDA receptors. Crit Rev Neurobiol 2006;18:71–84. [DOI] [PubMed] [Google Scholar]
- [25].Gorczynski RJ, Shaffer JE, Lee RJ. Pharmacology of ASL-8052, a novel beta-adrenergic receptor antagonist with an ultrashort duration of action. J Cardiovasc Pharmacol 1983;5:668–77. [DOI] [PubMed] [Google Scholar]
- [26].Yasui Y, Masaki E, Kato F. Esmolol modulates inhibitory neurotransmission in the substantia gelatinosa of the spinal trigeminal nucleus of the rat. BMC Anesthesiol 2011;11:15–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Choi YM, Kim KH. Etifoxine for pain patients with anxiety. Korean J Pain 2015;28:4–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Fletcher JE, Seavell CR, Bowen DJ. Pretreatment with alfentanil reduces pain caused by propofol. Br J Anaesth 1994;72:342–4. [DOI] [PubMed] [Google Scholar]


