Abstract
PURPOSE
Primary care visits for children with acute respiratory infections frequently result in antibiotic prescriptions, although antibiotics have limited benefits for common acute respiratory infections and can cause harms, including antibiotic resistance. Parental demands are often blamed for antibiotic prescription. We aimed to explore parents’ beliefs about antibiotic necessity, quantify their expectations of antibiotic benefit, and report experiences of other management options and exposure to and preferences for shared decision making.
METHODS
We conducted computer-assisted telephone interviews in an Australia-wide community sample of primary caregivers, hereafter referred to as parents, of children aged 1 to 12 years, using random digit dialing of household landline telephones.
RESULTS
Of the 14,505 telephone numbers called, 10,340 were eligible numbers; 589 potentially eligible parents were reached, of whom 401 were interviewed. Most believed antibiotics provide benefits for common acute respiratory infections, especially for acute otitis media (92%), although not using them, particularly for acute cough and sore throat, was sometimes acceptable. Parents grossly overestimated the mean benefit of antibiotics on illness symptom duration by 5 to 10 times, and believed they reduce the likelihood of complications. The majority, 78%, recognized antibiotics may cause harm. Recalling the most recent relevant doctor visit, 44% of parents reported at least some discussion about why antibiotics might be used; shared decision making about antibiotic use was inconsistent, while 75% wanted more involvement in future decisions.
CONCLUSIONS
Some parents have misperceptions about antibiotic use for acute respiratory infections, highlighting the need for improved communication during visits, including shared decision making to address overoptimistic expectations of antibiotics. Such communication should be one of several strategies that is used to reduce antibiotic use.
Keywords: antibiotics, antimicrobial agents, acute respiratory infections, resistance, acute otitis media, sore throat, cough, decision making, pediatrics
INTRODUCTION
Children experience 4 to 12 acute respiratory infections annually,1 and primary care clinicians too often prescribe antibiotics2–4 despite strong evidence that they typically provide only marginal benefits.5–8 Common harms and the contribution to antibiotic resistance,9 now a global public health crisis,10,11 are rarely addressed. Primary care clinicians resort to antibiotics for many reasons, including diagnostic uncertainty12,13; a desire to provide an unwell child with something to help13,14; and an attempt to reduce visit length12,13 and achieve parental satisfaction.15 Interacting with many of these reasons is parental pressure for antibiotics, both articulated and perceived by clinicians.13
It is known that patients overestimate benefits and underestimate harms for many medical treatments.16 We conducted a systematic review that found no studies specifically assessing these measures for acute respiratory infections,16 so we aimed to explore parents’ beliefs about antibiotic necessity, quantify their expectations of antibiotic benefit, and report the experiences of other management options and exposure to and preferences for shared decision making.
METHODS
We developed a questionnaire, pilot testing it to establish face validity and refine question format and sequence. We used convenience samples of 9 eligible parents interviewed face to face and 12 subsequently interviewed by telephone. Our Australia-wide survey of parents of at least 1 child aged 1 to 12 years used computer-assisted telephone interviewing (CATI) by an independent research organization. Randomly selected household landlines were telephoned between May and July 2014, and the child’s or children’s eligible primary caregiver, hereafter referred to as parent, was asked a series of questions (Supplemental Figure 1, available at http://www.AnnFamMed.org/content/15/2/149/suppl/DC1/). We analyzed responses from an initial 37 interviews to check internal quality and response validity, and to inform further interviewers’ training, before proceeding.
The questionnaire addressed 3 acute respiratory infections: acute otitis media, sore throat, and acute bronchitis. Questions were repeated for each of these infections (in random order to reduce bias), eliciting information from parents about their knowledge and expectations of antibiotic benefits and harms and other treatments; recall of the content of their last medical visit with their child for 1 of these acute respiratory infections (including discussion about antibiotic benefits or harms); shared decision making; and delayed prescribing (receipt of a prescription with the proviso that it not be filled immediately). Final questions sought sociodemographic information. Data were analyzed descriptively. Responses to open-ended questions were transcribed, coded, grouped into common themes by 2 researchers (P.D.C. and T.C.H), and ranked by frequency. Approval for the study was granted by the Bond University Human Research Ethics Committee.
RESULTS
From 14,505 available random household landline telephone calls, 10,340 numbers were classified as eligible numbers, of which 589 numbers were reachable, and 401 parent interviews were completed (Supplemental Figure 2, available at http://www.AnnFamMed.org/content/15/2/149/suppl/DC1/). Parent sociodemographic characteristics indicated the large majority of parents were Australian born (77%), female (77%), aged 36 to 45 years (62%), and married or living with a partner (89%) (Table 1).
Table 1.
Parent Characteristics (N = 401)
| Characteristic | Parents, No. (%) | General Public, %a |
|---|---|---|
| Female | 309 (77) | 51 |
| Age-group, y | ||
| ≤25 | 5 (1) | 14 |
| 26–35 | 84 (21) | 18 |
| 36–45 | 248 (62) | 19 |
| 46–55 | 59 (15) | 18 |
| ≥56 | 5 (1) | 32 |
| Born in Australia | 309 (77) | – |
| English spoken as main language at home | 380 (95) | – |
| Aboriginal or Torres Strait Islander | 7 (2) | 3 |
| Current living situation | ||
| Married or living with partner | 355 (89) | – |
| Sole caregiving responsibility | 39 (10) | – |
| Other | 7 (2) | – |
| Highest level of education | ||
| Primary school | 1 (0) | 5 |
| Junior high school | 15 (4) | 17 |
| Senior high school | 50 (13) | 38 |
| Trade or apprenticeship | 31 (8) | – |
| Diploma or certificate | 103 (26) | 21 |
| Bachelor’s degree | 133 (33) | 11 |
| Post-graduate degree | 68 (17) | 4 |
| Employment status | ||
| Full time (>30 h/wk) | 146 (36) | – |
| Part time (<30 h/wk) | 139 (35) | – |
| Casual employment | 29 (7) | – |
| Not currently in paid employment | 86 (21) | 5.7 |
| Number of children ≤12 years, mean (SD) [range] | 2 (0.85) [1–6] |
– |
| Annual gross household income, $b | ||
| <20,000 | 11 (3) | – |
| 20,001–40,000 | 24 (6) | – |
| 40,001–60,000 | 34 (9) | – |
| 60,001–80,000 | 44 (11) | – |
| 80,001–100,000 | 63 (16) | – |
| 100,001–140,000 | 115 (29) | – |
| 140,001–180,000 | 52 (13) | – |
| >180,000 | 33 (8) | – |
| Health Care Card holderc | 72 (18) | – |
| Time since most recent visit to doctor for child with AOM, sore throat, or acute cough, median (IQR), wk | 43 (9–104) |
– |
| Age of child at last visit, median (IQR), y | 6 (3–8) | – |
AOM = acute otitis media; IQR = interquartile range.
From the Australian Bureau of Statistics, for comparison.
In Australian dollars. Mean yearly income was $107,276.
Concession for access to Australian Medicare.
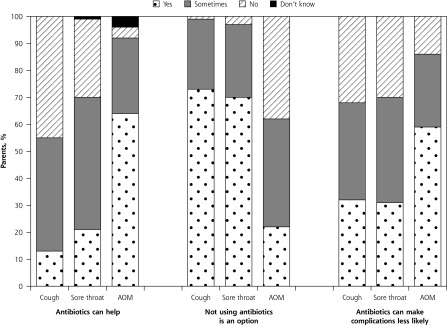
Figure 1 shows that most parents believed that antibiotics help (giving a response of yes or sometimes) for acute otitis media (92%), sore throat (70%), and cough (55%), most commonly by treating the infection and killing bacteria (Supplemental Table 1, available at http://www.AnnFamMed.org/content/15/2/149/suppl/DC1/). A minority thought antibiotics do not help (Figure 1), most commonly for sore throat and cough, because the illness was viral or other (nonbacterial) in etiology (Supplemental Table 2, available at http://www.AnnFamMed.org/content/15/2/149/suppl/DC1/). Similar reasons were also cited commonly when parents were asked why not using antibiotics is sometimes an option (Supplemental Table 3, available at http://www.AnnFamMed.org/content/15/2/149/suppl/DC1/), along with the response that the illness will resolve without treatment. Some parents believed that not using antibiotics, at least sometimes, was an option (Figure 1), particularly for cough (99%) and sore throat (97%), but less so for acute otitis media (61%). For those who thought antibiotics were necessary, the most common reason given was that the illness would not get better without treatment (Supplemental Table 4, available at http://www.AnnFamMed.org/content/15/2/149/suppl/DC1/).
Figure 1.
Percentages of parents giving various responses to statements about antibiotic use.
AOM = acute otitis media.
For each acute respiratory infection, parents grossly overestimated the benefits of antibiotics in reducing the duration of illness as compared with benefits seen from current empirical evidence (Table 2). Similarly, the minimum reduction in illness duration that parents reported they would want from antibiotics before considering their use (the minimally important difference) grossly exceeded evidence-based estimates, by 5 to 10 times.
Table 2.
Parent-Perceived and Actual Reduction of Illness Duration From Antibiotic Use
| Illness Type | Parent-Estimated Benefit, Mean (SD) [Range], Days
|
Actual Benefit, Based on Empirical Evidence, Mean, Days | |
|---|---|---|---|
| Reduction in Illness Duration From Antibiotics | Minimum Reduction in Duration Before Antibiotics Considered Worth Using | ||
| Acute otitis media | 3.0 (1.4) [0–7.0] | 3.0 (1.5) [0–7.0] | 0.55 |
| Sore throat | 2.6 (1.4) [0–7.0] | 2.7 (1.6) [0–7.0] | 0.57 |
| Acute cough | 5.4 (3.1) [0–14.0] | 5.0 (3.0) [0–14.0] | <0.56 |
Many believed complications from the acute respiratory infections could be avoided by using antibiotics, with highest agreement seen for acute otitis media. The most commonly cited complications were hearing loss, other infections, and perforated eardrum for acute otitis media; other infections and tonsillitis for sore throat; and chest infection and pneumonia for acute cough (Supplemental Table 5, available at http://www.AnnFamMed.org/content/15/2/149/suppl/DC1/).
The large majority of parents, 78%, knew antibiotics could potentially harm. Responses for how included: weakening the immune system (18%); killing good bacteria (11%); harming the balance of gut microbiota (11%); and causing adverse effects such as allergy (13%), gastrointestinal upset (7%), rash (7%), teeth damage/discoloration (7%), and candidiasis (3%). Antibiotic resistance was mentioned by 49%; it was articulated in various ways, some (16%) incorrect, such as the body developing immunity or tolerance to antibiotics.
Overall, 63% of parents reported using treatments other than antibiotics (range of 1 to 4 treatments), including over-the-counter products, simple analgesics, and complementary and alternative medicine. Analgesics and antipyretics (eg, acetaminophen, ibuprofen) were the most commonly used treatments for acute otitis media (82%) and sore throat (71%), and antihistamines and mucolytics were the ones most commonly used for cough (64%). Minor adverse effects were mentioned for many of these alternate treatments (Supplemental Table 6, available at http://www.AnnFamMed.org/content/15/2/149/suppl/DC1/).
When recalling the most recent visit to a doctor for their child with an acute respiratory infection, 44% of parents reported some discussion (giving a response of some or a lot) about why antibiotics might be used; however, 72% reported little or no discussion about reasons why antibiotics might not be used, and 78% did not remember any discussion about possible antibiotic harms (Table 3). Nearly all (93%) preferred involvement in future decisions about antibiotic use. Slightly more than one-half (58%) of parents recalled being given an antibiotic prescription but instructed not to have it filled immediately (ie, delayed prescribing). Of these parents, 21% filled the prescription, of whom 18% administered the antibiotic to their child.
Table 3.
Parents’ Recall of the Last Visit With Their Child to a Doctor for an Acute Respiratory Infection
| Question | Parents Giving Response, %
|
|||
|---|---|---|---|---|
| A Lot | Some | A Little | Not at All | |
| Were reasons you might want an antibiotic for your child discussed with the doctor? | 18 | 26 | 32 | 24 |
| Were reasons you might not want to use an antibiotic discussed with the doctor? | 12 | 15 | 24 | 48 |
| Would you prefer involvement in future decisions about the use of antibiotics for acute respiratory infections for your child? | 75 | 18 | 5 | 2 |
|
Parents Responding “No,” %
|
||||
| Was there any discussion about possible harms of antibiotics? | 78 | |||
| Were you asked by the doctor whether or not you wanted an antibiotic for your child? | 61 | |||
| Did the doctor explain that you had a choice about whether or not an antibiotic was prescribed? | 61 | |||
| Was the decision about antibiotic prescribing shared between you and your doctor? | 56 | |||
DISCUSSION
Our principal findings were that most, but not all, parents believe antibiotics are needed for their children’s common acute respiratory infections (particularly acute otitis media), and parents have a number of misperceptions about perceived benefit and need. Parents grossly overestimated antibiotic benefits on illness duration, which largely matched the minimally important effect of antibiotics that parents nominated as required for antibiotics to be worth using. Nevertheless, many were aware of potential harms from antibiotics, with some inaccuracies in knowledge identified.
Strengths of our study included the large sample size and careful development of the questionnaire, with inclusion of novel questions about the size of expected benefit. Weaknesses included telephoning only landline numbers and not cell phones, although how this approach might bias responses is not clear. Also, we had a modest response rate which was nonetheless comparable to those considered satisfactory in other community surveys.17 Our sample had a higher level of education which may have introduced a bias toward more informed responses, although an exaggeration of misconceptions about antibiotic benefits seems unlikely. Most respondents were women, which probably reflects the inclusion criteria for eligibility (primary caregivers of children at home when the call came through). Recall bias may have distorted questions about the most recent visit to the doctor, and not all parents provided responses to all open-ended questions.
Our findings are largely in line with those of previous studies on parental beliefs about antibiotics’ benefits for acute respiratory infections,18–26 although our study is among the first to quantify them. Of course, such expectations were not homogeneous across parents and illnesses—parents knew that not using antibiotics is sometimes acceptable, consistent with previous findings.26 Beliefs about the need for antibiotics for acute otitis media were different from those for sore throat and cough, suggesting a role for clinicians in carefully eliciting perceptions and misperceptions that parents might have and tailoring their communication accordingly.27,28
About one-half of parents reported antibiotic resistance as a potential harm, similar to proportions found in other cross-sectional studies,21,28,29 although there was confusion among many about what resistance actually was, as has been reported by others.18,25,29 Fewer parents mentioned common antibiotic harms consistent with empirical evidence, such as diarrhea and candidiasis30, and some of the complications that parents nominated as being reduced by antibiotic use are not clearly supported by evidence from randomized trials. Parents reported widespread use of alternatives to antibiotics in line with previous findings,18,23 most of which have no or weak empirical evidence of efficacy,31,32 with the exceptions being analgesics and antipyretics, and honey for cough.33
Antibiotic use for acute respiratory infections is usually a decision that is sensitive to patient preference34 because the benefit-harm trade-off is marginal. Yet few parents recalled discussing benefits and harms, and the option of forgoing antibiotic use with their clinician. These findings suggests opportunities for improving acute respiratory infection visits by adopting shared decision making, in which the options (using or not using antibiotics) and the benefits and harms of each are explained; parents’ concerns, beliefs, expectations, and preferences are explored; and a decision is reached collaboratively.35 Shared decision making is an effective strategy for reducing antibiotic prescribing for acute respiratory infections in primary care,36 but widespread implementation is limited. This study found most parents wanted to be involved in these decisions. Using shared decision making and possibly incorporating delayed prescribing as a presented option37 in acute respiratory infection visits may enable clinicians and parents to discuss perceived need for and beliefs about antibiotic use and promote informed decision making.
Acknowledgments
We thank the CATI interviewers and staff of the Institute for Social Science Research (ISSR), University of Queensland, who conducted the interviews.
Footnotes
Conflicts of interest: authors report none.
Funding support: The study was conducted as part of the Centre for Research Excellence in Minimizing Antibiotic Resistance from Acute Respiratory Infections APP1044904), for which funding is provided by the National Health and Medical Research Council of Australia.
Previous presentations: Coxeter P, Hoffmann T, Del Mar C. Exploring primary caregivers’ expectations about the benefits and risks of treatment for acute respiratory infections in children and involvement in management decisions presented at the Gold Coast Health and Medical Research Conference 2014; December 4–5, 2014; Gold Coast, Australia; and Coxeter P, Del Mar C, Hoffmann T. Parents’ expectations about the benefits and risks of treatment for acute respiratory infections in children and preferred level of involvement in management decisions, presented at the International Shared Decision Making (ISDM) and International Society for Evidence-Base Health Care (ISEHC) Conference 2015; July 19–22, 2015; Sydney, Australia.
Supplementary materials: Available at http://www.AnnFamMed.org/content/15/2/149/suppl/DC1/
References
- 1.Grüber C, Keil T, Kulig M, Roll S, Wahn U, Wahn V; MAS-90 Study Group. History of respiratory infections in the first 12 yr among children from a birth cohort. Pediatr Allergy Immunol. 2008;19(6):505–512. [DOI] [PubMed] [Google Scholar]
- 2.Vaz LE, Kleinman KP, Raebel MA, et al. Recent trends in outpatient antibiotic use in children. Pediatrics. 2014;133(3):375–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hersh AL, Shapiro DJ, Pavia AT, Shah SS. Antibiotic prescribing in ambulatory pediatrics in the United States. Pediatrics. 2011;128(6):1053–1061. [DOI] [PubMed] [Google Scholar]
- 4.Meropol SB, Chen Z, Metlay JP. Reduced antibiotic prescribing for acute respiratory infections in adults and children. Br J Gen Pract. 2009;59(567):e321–e328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Venekamp RP, Sanders SL, Glasziou PP, Del Mar CB, Rovers MM. Antibiotics for acute otitis media in children. Cochrane Database Syst Rev. 2015;(6):CD000219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Smith SM, Fahey T, Smucny J, Becker LA. Antibiotics for acute bronchitis. Cochrane Database Syst Rev. 2014;(3):CD000245. [DOI] [PubMed] [Google Scholar]
- 7.Spinks A, Glasziou PP, Del Mar CB. Antibiotics for sore throat. Cochrane Database Syst Rev. 2013;(11):CD000023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kenealy T, Arroll B. Antibiotics for the common cold and acute purulent rhinitis. Cochrane Database Syst Rev. 2013;(6):CD000247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chung A, Perera R, Brueggemann AB, et al. Effect of antibiotic prescribing on antibiotic resistance in individual children in primary care: prospective cohort study. BMJ. 2007;335(7617):429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. The Evolving Threat of Antimicrobial Resistance: Options for Action. Geneva, Switzerland: World Health Organization; 2012. http://whqlibdoc.who.int/publications/2012/9789241503181_eng.pdf Accessed Aug 9, 2016. [Google Scholar]
- 11.Center for Disease Dynamics Economics & Policy. State of the World’s Antibiotics, 2015. Washington, DC: Center for Disease Dynamics Economics & Policy; 2015. [Google Scholar]
- 12.Horwood J, Cabral C, Hay AD, Ingram J. Primary care clinician antibiotic prescribing decisions in consultations for children with RTIs: a qualitative interview study. Br J Gen Pract. 2016;66(644):e207–e213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lucas PJ, Cabral C, Hay AD, Horwood J. A systematic review of parent and clinician views and perceptions that influence prescribing decisions in relation to acute childhood infections in primary care. Scand J Prim Health Care. 2015;33(1):11–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Doust J, Del Mar C. Why do doctors use treatments that do not work? BMJ. 2004;328(7438):474–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Christakis DA, Wright JA, Taylor JA, Zimmerman FJ. Association between parental satisfaction and antibiotic prescription for children with cough and cold symptoms. Pediatr Infect Dis J. 2005; 24(9):774–777. [DOI] [PubMed] [Google Scholar]
- 16.Hoffmann TC, Del Mar C. Patients’ expectations of the benefits and harms of treatments, screening, and tests: a systematic review. JAMA Intern Med. 2015;175(2):274–286. [DOI] [PubMed] [Google Scholar]
- 17.The Pew Research Center. Assessing the representativeness of public opinion surveys. http://www.people-press.org/2012/05/15/assessing-the-representativeness-of-public-opinion-surveys/. Published May 15, 2012 Accessed May 22, 2016.
- 18.Zyoud SH, Abu Taha A, Araj KF, et al. Parental knowledge, attitudes and practices regarding antibiotic use for acute upper respiratory tract infections in children: a cross-sectional study in Palestine. BMC Pediatr. 2015;15:176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Siddiqui S, Cheema MS, Ayub R, et al. Knowledge, attitudes and practices of parents regarding antibiotic use in children. J Ayub Med Coll Abbottabad. 2014;26(2):170–173. [PubMed] [Google Scholar]
- 20.Yu M, Zhao G, Stålsby Lundborg C, Zhu Y, Zhao Q, Xu B. Knowledge, attitudes, and practices of parents in rural China on the use of antibiotics in children: a cross-sectional study. BMC Infect Dis. 2014;14:112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cho HJ, Hong SJ, Park S. Knowledge and beliefs of primary care physicians, pharmacists, and parents on antibiotic use for the pediatric common cold. Soc Sci Med. 2004;58(3):623–629. [DOI] [PubMed] [Google Scholar]
- 22.Grossman Z, del Torso S, Hadjipanayis A, van Esso D, Drabik A, Sharland M. Antibiotic prescribing for upper respiratory infections: European primary paediatricians’ knowledge, attitudes and practice. Acta Paediatr. 2012;101(9):935–940. [DOI] [PubMed] [Google Scholar]
- 23.Finkelstein JA, Dutta-Linn M, Meyer R, Goldman R. Childhood infections, antibiotics, and resistance: what are parents saying now? Clin Pediatr (Phila). 2014;53(2):145–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Panagakou SG, Spyridis N, Papaevangelou V, et al. Antibiotic use for upper respiratory tract infections in children: a cross-sectional survey of knowledge, attitudes, and practices (KAP) of parents in Greece. BMC Pediatr. 2011;11:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bagshaw SM, Kellner JD. Beliefs and behaviours of parents regarding antibiotic use by children. Can J Infect Dis. 2001;12(2):93–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kautz-Freimuth S, Redaèlli M, Samel C, Civello D, Altin SV, Stock S. Parental views on acute otitis media (AOM) and its therapy in children—results of an exploratory survey in German childcare facilities. BMC Pediatr. 2015;15:199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hansen MP, Howlett J, Del Mar C, Hoffmann TC. Parents’ beliefs and knowledge about the management of acute otitis media: a qualitative study. BMC Fam Pract. 2015;16:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cabral C, Ingram J, Hay AD, Horwood J; TARGET team. “They just say everything’s a virus”—parent’s judgment of the credibility of clinician communication in primary care consultations for respiratory tract infections in children: a qualitative study. Patient Educ Couns. 2014;95(2):248–253. [DOI] [PubMed] [Google Scholar]
- 29.McCullough AR, Parekh S, Rathbone J, Del Mar CB, Hoffmann TC. A systematic review of the public’s knowledge and beliefs about antibiotic resistance. J Antimicrob Chemother. 2016;71(1):27–33. [DOI] [PubMed] [Google Scholar]
- 30.Gillies M, Ranakusuma A, Hoffmann T, et al. Common harms from amoxicillin: a systematic review and meta-analysis of randomized placebo-controlled trials for any indication. CMAJ. 2015;187(1):E21–E31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith SM, Schroeder K, Fahey T. Over-the-counter OTC) medications for acute cough in children and adults in community settings. Cochrane Database Syst Rev. 2014;(11):CD001831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vassilev ZP, Kabadi S, Villa R. Safety and efficacy of over-the-counter cough and cold medicines for use in children. Expert Opin Drug Saf. 2010;9(2):233–242. [DOI] [PubMed] [Google Scholar]
- 33.Oduwole O, Meremikwu MM, Oyo-Ita A, Udoh EE. Honey for acute cough in children. Cochrane Database Syst Rev. 2014;12(12): CD007094. [DOI] [PubMed] [Google Scholar]
- 34.Elwyn G, Edwards A, Kinnersley P, Grol R. Shared decision making and the concept of equipoise: the competences of involving patients in healthcare choices. Br J Gen Pract. 2000;50(460):892–899. [PMC free article] [PubMed] [Google Scholar]
- 35.Hoffmann TC, Légaré F, Simmons MB, et al. Shared decision making: what do clinicians need to know and why should they bother? Med J Aust. 2014;201(1):35–39. [DOI] [PubMed] [Google Scholar]
- 36.Coxeter P, Del Mar CB, McGregor L, Beller EM, Hoffmann TC. Interventions to facilitate shared decision making to address antibiotic use for acute respiratory infections in primary care. Cochrane Database Syst Rev. 2015;11:CD010907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Spurling GK, Del Mar CB, Dooley L, Foxlee R, Farley R. Delayed antibiotics for respiratory infections. Cochrane Database Syst Rev. 2013;4(4):CD004417. [DOI] [PubMed] [Google Scholar]