Abstract
Background
Policy efforts to reduce the cost of prescription medications in the U.S. have failed to reduce disparities in cost-related underuse. Little is known about the relationships between pharmacy accessibility, utilization and cost-related underuse of prescription medications among residents of low-income minority communities.
Objectives
To examine the association between pharmacy accessibility, utilization and cost-related underuse of prescription medications among residents of predominantly low-income, Black and Hispanic urban communities.
Methods
Data from a population-based probability sample of adults 35 years and older residing on the South Side of Chicago in 2012–13 were linked with geocoded information on the type and location of primary and nearest pharmacy. Multivariable regression models were used to examine associations between pharmacy accessibility, utilization of, and travel distance to, primary pharmacy and cost-related underuse overall and by pharmacy type.
Results
One-third of South Side residents primarily filled their prescriptions at the pharmacy nearest to their home. Among those who did not use mail order, median distance traveled from home to the primary pharmacy was 1.2 miles. Residents whose primary pharmacy was at a community health center or clinic where they usually received care traveled the furthest but were least likely to report cost-related underuse of their prescription medications.
Conclusions
Most residents of minority communities on Chicago’s South Side were not using pharmacies closest to their home to obtain their prescription medications. Efforts to improve access to prescription medications in these communities should focus on improving the accessibility of affordable pharmacies at site of care.
Keywords: Disparities, pharmacy access, cost-related underuse, race/ethnicity, community resources
Introduction
Policy efforts to improve access to prescription medications in the United States focus almost exclusively on reducing the cost of prescription medications1 and have failed to reduce racial and ethnic disparities in cost-related underuse of prescription medications.2–5 While pharmacies are critical in facilitating access to prescription medications, poor pharmacy access has been found to disproportionately affect low-income Black and Hispanic communities.6 The costs of prescription medications are also higher for residents of low-income communities.7 Despite cost and distance barriers in accessing prescription medications, little is known about the relationships between pharmacy accessibility, utilization and cost-related underuse of prescription medications among residents of low-income minority communities.
The goal of this study is to examine the accessibility and utilization of pharmacies, and cost-related underuse of prescription medications, among residents of low-income, predominantly Black and Hispanic urban communities. Specifically, we identify where residents primarily fill their prescription medications and determine the extent to which pharmacy utilization or distance traveled to fill prescriptions are associated with cost-related underuse of prescription medications. We also examine whether individual factors (e.g. age, insured status, and income) and pharmacy type relate to patterns in pharmacy utilization and the cost-related underuse of prescription medications.
We hypothesize that pharmacy accessibility may be an overlooked contributor to cost-related underuse of prescription medications in lower income communities. This study seeks to inform health and community development strategies that aim to increase access to affordable prescription medications and potentially reduce cost-related underuse of prescription medications in underserved communities.
METHODS
Data Sources
Several data sources were used for this study. A population-based probability sample of households located on the South Side of Chicago was generated by the South Side Health and Vitality Studies (SSHVS). Individuals eligible for this study included those 35 years of age or older, English or Spanish speaking, and residing within the target census tracts. Study participants were sampled from two distinct regions, seven census tracts total. The northwest region was almost entirely African American (98%).8 The southeast region was majority Hispanic (83%). If more than one individual in a household was 35 years or older, random sampling was used to select which eligible household resident was approached for enrollment. The study was conducted with approval of the University of Chicago Institutional Review Board. All participants provided written documentation of informed consent. Eligible participants were recruited between November 2012 and July 2013 through mailed letters, telephone calls, and home visits. Once informed consent was obtained, participants took part in an in-person, interviewer-administered interview, lasting approximately one hour. Participants could choose to complete the interview in English or Spanish.
The SSHVS survey generated socio-demographic, health and access to resources data for 267 participants. The analytic sample for this study was restricted to the 169 adults who reported using at least one prescription medication on a regular basis. Prescription medication use and number of prescription medications were determined by responses to the question: “How many prescription medications do you use on a regular basis, either daily or weekly?”
Geocoded data on the primary pharmacy locations for the study sample were derived from the 2012 MAPSCorps asset census, a youth employment and STEM (Science Technology Engineering and Mathematics) training program that generated a comprehensive database of all public-facing businesses and organizations by direct observation in the study area.9,10 Data from the Illinois Department of Financial and Professional Regulation (IDFPR) pharmacy master files for 2012 provided pharmacy location and type (e.g. retail chain, retail independent, community health center, or clinic-based) for community pharmacies located in Chicago. Pharmacy addresses were geocoded using ArcGIS, version 10.0 (ESRI Co., Redlands, CA).
We also used data from the 2008–2012 U.S. Census Bureau American Community Survey (ACS), the largest national household survey in the United States to derive community characteristic variables, including median household income at the census tract level.11 We used 2010 decennial U.S. Census data to derive variables on racial and ethnic composition at the census tract level.12
Outcome Variables
We examined three key outcomes. The first key outcome was a measure of pharmacy accessibility. We examined pharmacy accessibility at the community- and individual-level. IDFPR data were used to examine pharmacy availability (defined as the total number of pharmacies) and accessibility (defined as the total number of pharmacies per square mile) by pharmacy type at the community-level. We also determined whether the pharmacy was located in or outside the South Side Chicago study area. A square-mile grid for the City of Chicago was used to calculate the number of pharmacies per square mile using ArcGIS version 10.0 (ESRI Co., Redlands, CA). At the individual-level, we defined pharmacy accessibility based on travel distance from respondent’s home to the nearest pharmacy location; respondents living more than 1 mile from their nearest pharmacy were categorized as having low-access to a pharmacy. This definition is derived from the definition of “pharmacy deserts” or low-access used in an earlier study to define pharmacy accessibility in Chicago.6 The 1 mile benchmark is also used by the US Department of Agriculture and the Centers for Disease Control and Prevention to define pharmacy deserts. 13
The second key outcome, pharmacy utilization, was measured as distance traveled to primary pharmacy and primary pharmacy type. The “primary pharmacy” was identified by response to the question: “If you need to fill a prescription or buy other medications, where do you go?” We then used geospatial methods to calculate travel (driving or walking) distance (in miles) from each respondent’s home address to his or her primary pharmacy.
The third key outcome, cost-related underuse of prescription medication, was derived from the question “Do you ever skip your medication or take less than the prescribed dose to stretch your prescriptions because you can not afford it?” This is a standard and widely used measure of cost-related medication underuse, often used as a national indicator of affordability barriers to filling prescription medications, including in the National Health Interview Survey (NHIS).14 Those who responded affirmatively with a “yes” were categorized as reporting cost-related underuse.
Other Variables
Pharmacy Characteristics
IDFPR data were used to classify primary pharmacy type into five categories: 1) chain (e.g. Walgreens, CVS, Costco, Wal-Mart); 2) independent (e.g. independently owned); 3) community health center (CHC) or outpatient clinic (not a CHC), and; 4) mail order. The term “retail pharmacy” was used to include both chain and independent pharmacies. The MAPSCorps data were linked with the population survey data to identify the respondent’s “nearest pharmacy.” A respondent’s nearest pharmacy was defined as the pharmacy with the shortest travel distance from the respondent’s home residence. Respondents whose primary pharmacy was also the nearest pharmacy were also classified as utilizing the nearest pharmacy.
Individual Characteristics
Individual characteristics were derived from self-reported data in the population survey. Individual income was dichotomously categorized as poor (<$25,000 annual household income) or non-poor (≥$25,000 annual household income) based on the federal poverty threshold for 2012.13 Health status (insured or uninsured) and type of insurance coverage (private, Medicaid, Medicare, other) were ascertained by self-report. We did not capture information on prescription drug coverage, including Medicare Part D. Respondents were asked if they had a regular place they went when they were sick; those who responded affirmatively were classified as having a usual source of care. Number of chronic conditions was based on respondent reporting ever being diagnosed with any of the following health conditions: arthritis, asthma, chronic obstructive pulmonary disease, myocardial infarction, cirrhosis, poor kidney function, thyroid, diabetes, Alzheimer’s Disease or dementia. Other individual-level variables included self-reported gender (male or female) and education, the latter of which was categorized as less than high school, high school graduate, or at least some college.
Statistical Analysis
Sample weights were applied to adjust for differential probability of selection and differential non-response, thereby generating estimates generalizable to the Chicago South Side target population. Descriptive statistics were used to characterize individual and pharmacy characteristics associated with our key outcomes. Logistic regression was used to examine pharmacy and individual characteristics associated with cost-related underuse of prescription medication. All analyses were conducted using Stata release 12 (StataCorp LP, College Station, TX).
RESULTS
Population characteristics
The median age of our sample was 59 years (Table 1). Poverty rates were high (42%) and nearly one in five people was uninsured. Nearly everyone (90%) had been diagnosed with at least one chronic condition, and more than two thirds regularly used 3 or more prescription medications. Two thirds of prescription medication users lived less than one mile from their nearest pharmacy (all of which were retail chain or independent). The probability sample of 7 census tracts exhibited demographic characteristics generally similar to the population ages 35 years and older living on Chicago’s South Side (Appendix A, available on JAPhA.org as supplemental content for this article).
TABLE 1.
CHARACTERISTICS OF SOUTH SIDE CHICAGO POPULATION OF PRESCRIPTION MEDICATION USERS (N=169)
| Weighted % (95% Confidence Interval) | |
|---|---|
| Age (years) (Mean, CI) | 59.0 (56.9, 61.7) |
| Age (years) (Median, Range) | 58.7 (35.7, 86.0) |
| % Women (N=108) | 57.7 (48.4, 66.6) |
| Household Income | |
| <25K/yr (N=66) | 41.7 (32.5, 51.5) |
| ≥25K–49K/yr (N=44) | 33.6 (25.0, 43.5) |
| ≥50K–99K/yr (N=24) | 17.3 (11.2, 25.6) |
| ≥100K/yr (N=9) | 7.4(3.6, 14.6) |
| Number of Chronic Conditions (Mean (CI)) | 2.1 (1.9, 2.4) |
| Number of Chronic Conditions (median (range)) | 2.0 (0–13) |
| 0 (N=16) | 10.5 (6.0, 17.6) |
| 1 (N=43) | 26.9 (19.4, 36.1) |
| 2 (N=47) | 29.8 (22.1, 38.8) |
| 3 or more (N=60) | 32.8 (25.0, 41.7) |
| Number of Prescription Medications (mean (CI)) | 4.5 (3.0, 6.1) |
| Number of Prescription (median (range)) | 3.0 (1–40) |
| 1 (N=26) | 14.9 (9.7, 22.2) |
| 2 (N=32) | 17.1 (11.4, 24.7) |
| 3 or more (N=111) | 68.1 (59.3, 75.7) |
| Insurance Status1 | |
| Private Insurance (N=64) | 43.0 (34.3, 52.2) |
| Medicare (N=50) | 28.2 (20.8, 36.9) |
| Medicaid (N=18) | 8.7 (5.2, 14.2) |
| Other Insurance (N=4) | 1.3 (0.4, 4.1) |
| Uninsured (N=31) | 18.9 (12.2, 28.0) |
| Nearest pharmacy type | |
| Chain (N=128) | 87.9(81.7, 92.2) |
| Independent (N=25) | 12.1 (7.8, 18.3) |
| Distance to nearest Pharmacy | |
| < 1 mile (N=95) | 67.0(58.1, 74.9) |
| ≥ 1 mile (N=58) | 33.0(25.1, 41.9) |
| Cost-related underuse (N=21) | 10.3 (6.4, 16.3) |
This measure did not include information on prescription drug coverage.
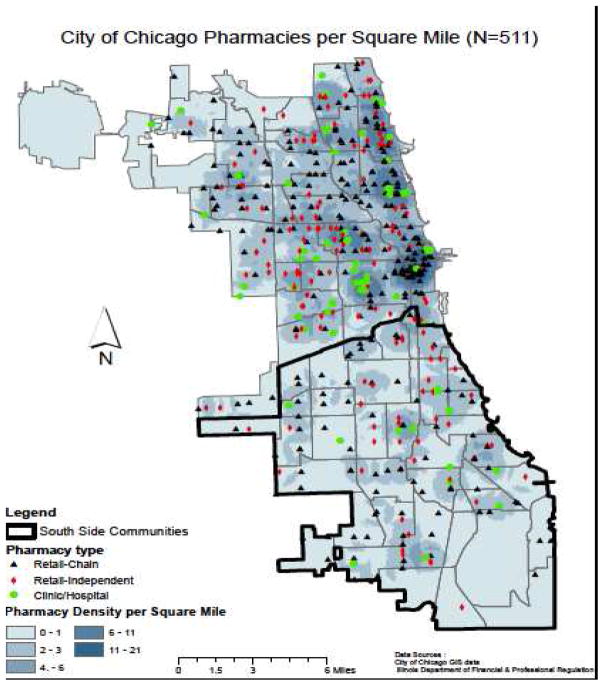
Pharmacy Accessibility
As presented in Table 2, there were more than 500 pharmacies in Chicago in 2012, the majority of which were retail chain operations. The distribution of pharmacies in Chicago illustrates differences between the South Side and other communities in the city. A total of 147 pharmacies were located in the 349 census tracts in the South Side study region. Compared to other regions of the city, more independent retail pharmacies and fewer clinic- or CHC-based pharmacies were available on Chicago’s South Side. The accessibility of pharmacies (of any type) on Chicago’s South Side was half that in the rest of Chicago (1.8 per mi2 versus 3.5 per mi2). Figure 1 provides a map depicting pharmacy accessibility.
TABLE 2.
AVAILABILITY AND ACCESSIBILITY OF PHARMACIES WITHIN AND OUTSIDE THE SOUTH SIDE OF CHICAGO STUDY REGION BY PHARMACY TYPE, 2012
| South Side Communities (N=329) | Other Communities in Chicago (N=473) | All Communities in Chicago (N=802) | ||||
|---|---|---|---|---|---|---|
| Pharmacy Type | Availability | Accessibility | Availability | Accessibility | Availability | Accessibility |
| Total Number (%)of Pharmacies | Pharmacy Density (per sq. mile) [Median (Range)] | Total Number (%) of Pharmacies | Pharmacy Density (per sq. mile) [Median (Range)] | Total Number (%) of Pharmacies | Pharmacy Density (per sq. mile) [Median (Range)] | |
| Chain*± | 83 (57%) | 1.6 (0, 4)* | 197 (54%) | 2.9 (0, 19) | 280 (55%) | 1.8 (0,19) |
| Independent* | 49 (33%)* | 1.4 (0, 6) | 111 (30%) | 1.1 (0, 4) | 160 (31%) | 1.2 (0, 4) |
| CHC/Clinic*± | 15 (10%)* | 0 (0, 3) | 56 (15%) | 0 (0, 7) | 71 (14%) | 0.0 (0,7) |
| Total | 147 (100%) | 1.8 (0, 5)* | 364 (100%) | 3.5 (0, 21) | 511(100%) | 2.7 (0, 21) |
Note: South Side of Chicago study region consists of 329 census-tracts.
Pearson chi-square was used to test the differences between proportions of pharmacy type between South Side Chicago communities and other communities. Wilcoxon rank sum statistics was used to test the differences between the median pharmacies per square mile by community type (South Side Chicago vs. other).
Statistical significance in the difference in the proportion of pharmacy type by community type (South Side Chicago vs. other) at p<0.05.
Statistical significance in differences between median pharmacies per square mile by community (South Side Chicago vs. other) at p<0.05.
FIGURE 1.
PHARMACY AVAILABILITY AND ACCESSIBILITY IN AND OUTSIDE THE SOUTH SIDE OF CHICAGO
Pharmacy Accessibility and Utilization
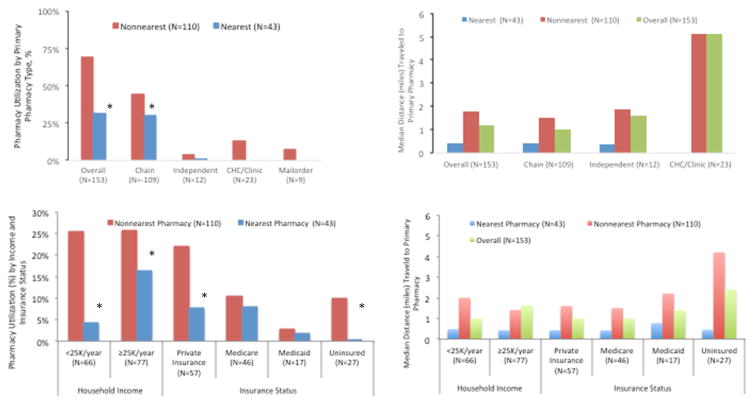
Less than one-third (31%) of residents filled their prescriptions at this nearest pharmacy (Figure 2A). Although a third of available pharmacies on the South Side of Chicago were independent retail pharmacies, only 7.8% of residents filled their prescription medications at this pharmacy type. Among prescription medication users who did not use mail order, median distance traveled from home to the primary pharmacy was 1.2 miles (range 0.0, 28.5).
FIGURE 2.
PHARMACY AND INDIVIDUAL CHARACTERISTICS ASSOCIATED WITH PHARMACY UTILIZATION AND DISTANCE TRAVELED TO PRIMARY PHARMACY OVERALL AND ACCORDING TO USE OF NEAREST PHARMACY (N=153)
Notes: 16/169 respondents excluded due to missing data on nearest or primary pharmacy type. Pearson chi-square was used to test the difference between proportion of users and non-users of nearest pharmacy. Wilcoxon rank sum statistics was used to test the differences between the median distance traveled to primary pharmacy between users and non-users of nearest pharmacy. * Statistically significant (p<0.05). Statistically significant differences were found comparing users and non-users of nearest pharmacy for all pharmacy types and individual characteristics (p<0.05).
Nearly 1 in 6 of South Side residents (15%) reported using a clinic- or CHC pharmacy and these people traveled further from their home (median 5.1 miles, range 2.3, 9.0) than those primarily using retail chain (0.99 miles) or independent (1.6 miles) pharmacies. All people who filled their prescription medication at a clinic/CHC pharmacy identified that site as their usual source of care (data not shown).
Among the people who did use their nearest pharmacy, nearly all were using a retail chain pharmacy and, on average, traveled less than a half mile (0.43 miles, range 0.33, 0.60). People who primarily filled their prescriptions at a pharmacy other than the one nearest to their home, however, traveled a median distance of 1.8 miles (range 0.13, 4.9).
The distance traveled to the primary pharmacy, and the type of pharmacy, were also associated with individual characteristics, specifically Insured status and household income (Figure 2B). In comparison to their counterparts, low-income and uninsured residents were less likely to utilize their nearest pharmacy and traveled significantly farther to fill their prescription medications.
Individuals who did not utilize the nearest pharmacy (N=110), were also asked to report reasons for not using this pharmacy to fill their prescription medications. The most commonly reported reasons were cost, personal preference, insurance, and inconvenience (including too far) (see Appendix 3).
Pharmacy Accessibility, Utilization and Cost-related Underuse
Overall, one in ten people ages 35 and older on Chicago’s South Side using prescription medications exhibited cost-related underuse of prescription medications (Table 3). Residents traveling less than 1 mile to fill their prescription were less likely to report cost-related underuse (8.7%) than their counterparts (14.3%). When compared to uninsured people, those with insurance (particularly private insurance) were less likely to report cost-related underuse independent of primary pharmacy type and distance. People using clinic- or CHC-based pharmacies were less likely to report cost-related underuse (0.42, 95% CI 0.04, 4.1) than those using independent or chain retail pharmacies. This difference, however, was not statistically significant.
TABLE 3.
INDIVIDUAL AND PHARMACY CHARACTERISTICS ASSOCIATED WITH COST-RELATED UNDERUSE AMONG PRESCRIPTION MEDICATION USERS ON CHICAGO’S SOUTH SIDE (N=169)
| PHARMACY CHARACTERISTICS | Estimated Prevalence, % (95% CI) | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|---|
| Primary pharmacy type | |||
| Retail Independent (N=12) | 15.5 (3.5, 47.8) | Reference | Reference |
| Retail Chain (N=109) | 11.2 (6.4, 18.7) | 0.69 (0.12, 3.8) | 1.3 (0.19, 8.5) |
| CHC/Clinic (N=23) | 9.2 (3.2, 23.5) | 0.55 (0.08, 3.9) | 0.42 (0.04, 4.1) |
| Distance traveled to primary pharmacy (in miles) | 0.21 (0.16, 0.27)* | 1.1 (0.94, 1.2) | |
| < 1 mile (N=95) | 8.7 (4.9, 15.2) | Reference | Reference |
| ≥ 1 mile (N=58) | 14.3 (6.4, 28.9) | 1.7 (0.59, 5.2) | 2.1 (0.62, 6.9) |
| INDIVIDUAL CHARACTERISTICS | |||
| Household Income | |||
| <25K/year (N=66) | 14.4 (7.9, 27.2) | Reference | Reference |
| ≥25K/year (N=77) | 9.1 (4.5, 17.5) | 0.55 (0.20, 1.5) | 0.90 (0.26, 3.1) |
| Insurance status | |||
| Uninsured (N=31) | 18.9 (7.4, 40.4) | Reference | Reference |
| Private Insurance (N=64) | 5.0 (1.7, 13.6) | 0.22 (0.05, 1.0) | 0.13 (0.02, 0.68)* |
| Medicare (N=50) | 13.4 (6.3, 26.3) | 0.67 (0.17, 2.6) | 0.46 (0.10, 2.2) |
| Medicaid (N=18) | 10.4 (3.0, 30.2) | 0.50 (0.09, 2.7) | 0.29 (0.05, 1.8) |
| Other Insurance (N=4) | 0 (0, 0) | - | - |
Notes: Logistic regression was used to examine individual and pharmacy characteristics associated with cost-related underuse. Adjusted model includes pharmacy and individual characteristics, plus age and number of prescription medications.
Statistically significant difference at p<0.05
DISCUSSION
Policy efforts to improve access to prescription medications—such as implementation of Medicare Part D and Medicaid expansions—have focused almost exclusively on reducing the costs of prescription medications.4,15,16 These efforts, however, have failed to reduce the cost-related underuse of prescription medications, particularly among Black and Hispanic populations.1–3, 17 To our knowledge, our study is the first to examine the association between pharmacy accessibility, utilization and cost-related underuse of prescription medications among residents of Black and Hispanic urban communities. Despite the limitations of our relatively small sample, our findings provide important new insights that can be used to guide future work.
In this study, we found that the majority of Black and Hispanic prescription medication users on Chicago’s South Side live within1 mile of at least one retail pharmacy, but many did not use this nearest pharmacy to fill their prescriptions. Residents relying on their nearest retail pharmacy at their site of care were the least likely to report cost-related underuse. In contrast, low-income and uninsured residents traveled the furthest to fill their prescription medications and were more likely to report cost-related underuse than their counterparts. These findings suggest that both insurance and the affordability of accessible pharmacies are important in ensuring access to prescription medications and reducing cost-related underuse among urban Black and Hispanic communities.
In comparison to other areas of Chicago, people living on the South Side have access to fewer chain and CHC/clinic-based pharmacies, and more independent pharmacies within a mile from their home. This observation corroborates findings from a previous report that indicates more than half of community pharmacies available in low-income, minority communities in Chicago are independent retail pharmacies.6 Our study found, however, that very few people in these communities utilize independent pharmacies; the majority fill prescriptions at a retail chain pharmacy. This finding suggests that pharmacy type may influence utilization patterns. Additionally, we found that one in ten prescription medication users filled prescriptions at a CHC or clinic where they usually received care. This finding has not been previously reported.
South Side residents may be traveling further to fill their prescription medications because prescriptions may cost more at the pharmacies closer to their home. According to our study, residents without insurance traveled significantly further to fill their prescription medications, compared to the insured and many residents reported not using their nearest pharmacy due to cost. This finding corroborates previous studies that report the cost of prescription medications is higher, and that low-cost prescription program offerings are fewer, at retail pharmacies in low-income communities than those in higher income communities.7, 18,19 Additionally, retail chain pharmacies located in low-income minority communities may not offer services important to local residents, including on-site clinics, 24-hour and drive-through services. Previous studies report that fewer pharmacy services are offered at pharmacies located in low-income, compared to higher income, communities.20
Current efforts under the Affordable Care Act (ACA) to expand insurance coverage and community health centers21–23 should also consider pharmacy accessibility, particularly for low-income residents. Policies supporting the development of pharmacies within existing and new CHCs may increase accessibility to and decrease cost-related underuse of prescription medication for lower income residents.
Implementing a publicly funded program to lower the costs of prescription medications, similar to either the 340B program18 or low-cost pharmacy programs19 might also be an effective way to improve access to prescription medications, and reduce cost-related underuse. Implementing these types of programs at independent pharmacies that are disproportionately underutilized in low-income, minority communities may be one strategy to reduce cost-related underuse and increase pharmacy access, especially for people with limited mobility and transportation access.
Our study has several limitations. First, our analysis is limited to prescription medication users, and thus our findings may very well underestimate the cost-related underuse of prescription medications among residents not filling any of their prescription due to cost. Second, our measure of pharmacy accessibility used driving or walking distance, rather than travel time. Travel time would additionally account for time waiting for public transportation and inefficient walking routes taken to avoid streets perceived to be unsafe. Therefore, our findings may underestimate the accessibility of pharmacies. Third, the relatively small sample size limits power to detect a statistically significant difference in some of the analyses. Fourth, we do not account for other factors that may influence the cost-related underuse of prescription medications, including prescription drug coverage and drug costs. Fifth, we defined nearest pharmacy based on place of residence, and some individuals may consider their nearest pharmacy based on their place of employment or other place (e.g. clinic). Finally, our findings may not be generalizable to all low-income communities.
CONCLUSION
Among Black and Hispanic residents of Chicago’s South Side, the vast majority of prescription medication users were primarily filling their prescriptions at pharmacies other than those nearest to their home. Residents who relied on CHCs or clinics where they usually receive health care were the least likely to exhibit cost-related underuse. Our study points to engagement of independent pharmacies in pharmaceutical cost reduction programs as one opportunity and expansion of community health center-based pharmacies as another opportunity to increase access and reduce cost-related underuse in this population.
Acknowledgments
We would like to acknowledge insights shared by Katherine M. Huff and Marcus B. Wolfe that helped inform our discussion.
APPENDIX 1: WEIGHTED ESTIMATES OF STUDY SAMPLE CHARACTERISTICS COMPARED TO SOUTH SIDE OF CHICAGO POPULATION
| Total sample (N=267) | South Side (n=496,829)* | |
|---|---|---|
| Population characteristics | ||
| Race/Ethnicity | ||
| NH White | 10.0% (6.5–15.0) | 16% (78,189) |
| NH Black | 53.2% (45.8–60.5) | 60% (299,853) |
| NB Hispanic | 34.6% (27.4–42.6) | 20% (97,481) |
| Other | 1.5% (0.5–4.6) | 4% (21,306) |
| Missing | 0.67% (0.20–2.2) | -- |
| Women | 57.8% (50.4–64.9) | 56% (277,434) |
| Age Groups (Year) | ||
| <50 | 45.3% (38.1–52.7) | 41% (200.461) |
| 50–64 | 30.0% (24.4–36.2) | 35% (175;395) |
| 65+ | 24.7% (18.9–31.73 | 24% (120,973) |
| Education* | ||
| < High School | 30.4% (24.0–37.8) | 27% (128,602) |
| High School graduate | 34.8% (28.2–42.1) | 27% (132,008) |
| Some college/college plus | 34.8% (28.4–41.6) | 46% (220,552) |
| % Low-Income | 100% (6) | 81 % (267) |
Sources: Population: 2010 Decennial United States Census; Education: American Community Survey 5 years 2008–2012; Survey weighted sample population size: 10936;
Population totals for those 35 years and older living on Chicago’s South Side. South Side study region consists of 329 census-tracts.
APPENDIX 2: CHARACTERISTICS OF PRIMARY PHARMACIES UTILIZED BY PHARMACY TYPE AND LOCATION AMONG RESIDENTS OF THE SOUTH SIDE OF CHICAGO IN 2012 (N=144)
| PRIMARY PHARMACY LOCATION | |||
|---|---|---|---|
| Located within Study Region | Not Located within Study Region | All Primary Pharmacies | |
| Number of Pharmacies, % | 34 (65.0%) | 18 (35.0%) | 52 (100.0%) |
| Utilization Rate, N (%) | 117(81%) | 27 (19%) | 144(100.0%) |
| Pharmacy Type | |||
| Chain | 22 (64.1%) | 14 (77.8%) | 36 (69.2%) |
| Independent | 6 (17.7%) | 1 (5.6%) | 7 (13.5%) |
| Clinic/CHC | 6 (17.6%) | 3 (16.7%) | 9 (17.3%) |
| Community Racial/Ethnic Composition* | |||
| Predominately Black | 25 (83.3%) | 5 (27.8%) | 30 (62.5%) |
| Predominately Hispanic | 1 (3.3%) | 0 (0.0%) | 1 (2.1%) |
| Predominately White | 2 (6.7%) | 11 (61.1%) | 13 (27.1%) |
| Diverse/Integrated | 2 (6.7%) | 2 (11.1%) | 4 (8.3%) |
Notes: Sample of 144 respondents excludes 9 respondents reporting the use of mail-order pharmacies. Differences in primary pharmacy utilization rates between pharmacy locations (located on Chicago’s South Side vs. not located on Chicago’s South Side) were tested using Pearson Chi Square Statistic;
Statistically significant difference at p<0.05
APPENDIX 3: SELF-REPORTED REASONS FOR NOT USING NEAREST PHARMACY (N=110)
| Self-Reported Reasons | N (%) |
|---|---|
| Costs (e.g. too expensive) | 27 (23.7%) |
| Personal preference (e.g. I prefer to go this pharmacy) | 28 (23.6%) |
| Insurance? (e.g. doesn’t take my insurance) | 13 (15.0%) |
| Unaware (e.g. didn’t know about pharmacy) | 13 (11.9%) |
| Inconvenience (e.g. too far, not opened) | 10 (10.0%) |
| Other? (e.g. not safe) | 11 (8.0%) |
| Provider preference (e.g. doctor told me I should go to this pharmacy) | 8 (7.8%) |
Footnotes
Disclosures: This research was supported in part by the South Side Health and Vitality Studies at the University of Chicago and the Urban Health Initiative at the University of Chicago Medicine. Data collection for the project described was supported in part by Grant Number 1C1CMS330997-03-00 from the Department of Health and Human Services, Centers for Medicare & Medicaid Services for the CommunityRx project (Stacy Lindau, PI). Under the terms of the CMS funding opportunity, awardees were expected to develop a sustainable business model to continue and support the model that was tested after award funding ends. Dr. Stacy Lindau is the founder and owner of a social impact company NowPow, LLC and is President of the Board of Directors of MAPSCorps. Neither NowPow, LLC nor MAPSCorps is supported through CMS. Neither the University nor University of Chicago Medical Center is endorsing or promoting any NowPow/MAPSCorps entity or its business, products, or services. Effort of Drs. Lindau and Makelarski was also supported by NIH R01AG047869. The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of the U.S. Department of Health and Human Services or any of its agencies. Dr. Qato’s effort was supported by the National Institutes of Health, National Institute on Aging grant number R21AG04923. The funding source had no role in the design and conduct of the study, analysis, or interpretation of the data; and preparation or final approval of the manuscript prior to publication.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gellad WF, Donohue JM, Zhao X, Zhang Y, Banthin JS. The financial burden from prescription drugs has declined recently for the nonelderly, although it is still high for many. Health Aff (Millwood) 2012;31(2):408–416. doi: 10.1377/hlthaff.2011.0469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bakk L. Racial/Ethnic Differences in Cost-Related Nonadherence and Medicare Part D: A Longitudinal Comparison. J Health Care Poor Underserved. 2015;26(4):1132–48. doi: 10.1353/hpu.2015.0113. [DOI] [PubMed] [Google Scholar]
- 3.Tseng CW, Tierney EF, Gerzoff RB, et al. Race/ethnicity and economic differences in cost-related medication underuse among insured adults with diabetes: the Translating Research Into Action for Diabetes Study. Diabetes Care. 2008;31(2):261–266. doi: 10.2337/dc07-1341. [DOI] [PubMed] [Google Scholar]
- 4.Yin W, Basu A, Zhang JX, Rabbani A, Meltzer DO, Alexander GC. The effect of the Medicare Part D prescription benefit on drug utilization and expenditures. Ann Intern Med. 2008;148(3):169–177. doi: 10.7326/0003-4819-148-3-200802050-00200. [DOI] [PubMed] [Google Scholar]
- 5.Qato DM, Lindau ST, Conti RM, Schumm LP, Alexander GC. Racial and ethnic disparities in cardiovascular medication use among older adults in the United States. Pharmacoepidemiol Drug Saf. 2010;19(8):834–842. doi: 10.1002/pds.1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Qato DM, Daviglus ML, Wilder J, Lee T, Qato D, Lambert B. ‘Pharmacy deserts’ are prevalent in Chicago’s predominantly minority communities, raising medication access concerns. Health Aff (Millwood) 2014;33(11):1958–1965. doi: 10.1377/hlthaff.2013.1397. [DOI] [PubMed] [Google Scholar]
- 7.Gellad WF, Choudhry NK, Friedberg MW, Brookhart MA, Haas JS, Shrank WH. Variation in drug prices at pharmacies: are prices higher in poorer areas? Health Serv Res. 2009;44(2 Pt 1):606–617. doi: 10.1111/j.1475-6773.2008.00917.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lindau ST, Makelarski JA, Abramsohn E, Beiser D, Escamilla V, Jerome J, Johnson D, Kho A, Lee K, Long T, Miller D. CommunityRx: A Population Health Improvement Innovation that Connects Clinics to Communities. Health Aff (Millwood) 2016;35(11):2020–2029. doi: 10.1377/hlthaff.2016.0694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lindau ST, James R, Makelarski JA, Sanders E, Johnson D. Comments From the South Side of Chicago on New Haven’s Inspiring Initiative. Am J Public Health. 2012;102(7):e3–4. doi: 10.2105/AJPH.2012.300684. author reply e4–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Makelarski JA, Lindau ST, Fabbre VD, et al. Are your asset data as good as you think? Conducting a comprehensive census of built assets to improve urban population health. J Urban Health. 2013;90(4):586–601. doi: 10.1007/s11524-012-9764-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Community Survey Public Use Microdata Sample Files. Washington, DC: US Census Bureau; 2016. [Accessed June 1, 2013]. http://www2.census.gov/programs-surveys/acs/data/pums. [Google Scholar]
- 12.2010 Census. Washington, DC: United States Census Bureau; Jun 1, 2013. http://www.census.gov/2010census/data/ [Google Scholar]
- 13.Food environment atlas. [Accessed August 2015];US Department of Agriculture Economic Research Service website. http://ers.usda.gov/data-products/food-environment-atlas.aspx. http://ers.usda.gov/data-products/foodenvironment-atlas.aspx#.Up48HJVvf8s.
- 14.Cox C, Kamal R, Jankiewicz A, Rousseau D. Recent Trends in Prescription Drug Costs. JAMA. 2016;315(13):1326. [Google Scholar]
- 15.Wagner TH, Heisler M, Piette JD. Prescription drug co-payments and cost-related medication underuse. Health Econ Policy Law. 2008;3(Pt 1):51–67. doi: 10.1017/S1744133107004380. [DOI] [PubMed] [Google Scholar]
- 16.Sommers BD, Musco T, Finegold K, Gunja MZ, Burke A, McDowell AM. Health reform and changes in health insurance coverage in 2014. N Engl J Med. 2014;371(9):867–874. doi: 10.1056/NEJMsr1406753. [DOI] [PubMed] [Google Scholar]
- 17.Madden JM, Graves AJ, Ross-Degnan D, Briesacher BA, Soumerai SB. Cost-related medication nonadherence after implementation of Medicare Part D, 2006–2007. JAMA. 2009;302(16):1755–1756. doi: 10.1001/jama.2009.1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Conti RM, Bach PB. The 340B drug discount program: hospitals generate profits by expanding to reach more affluent communities. Health Aff (Millwood) 2014;33(10):1786–1792. doi: 10.1377/hlthaff.2014.0540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang Y, Gellad WF, Zhou L, Lin YJ, Lave JR. Access to and use of $4 generic programs in Medicare. J Gen Intern Med. 2012;27(10):1251–1257. doi: 10.1007/s11606-012-1993-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pollack CE, Armstrong K. The geographic accessibility of retail clinics for underserved populations. Arch Intern Med. 2009;169(10):945–949. doi: 10.1001/archinternmed.2009.69. discussion 950–943. [DOI] [PubMed] [Google Scholar]
- 21.Kaiser Family Foundation. [accessed December 8, 2016];Focus on Health Reform: Summary of Affordable Care Act. 2013 http://kff.org/health-reform/fact-sheet/summary-of-the-affordable-care-act/
- 22.Rasmussen PW, Collins SR, Doty MM, Beutel S. Are Americans finding affordable coverage in the health insurance marketplaces? Results from the Commonwealth Fund Affordable Care Act Tracking Survey. Issue Brief (Commonw Fund) 2014 Sep;25:1–15. [PubMed] [Google Scholar]
- 23.Patient Protection and Affordable Care Act, 42 USC § 18001. United States Government; 2010. [Accessed August 2016]. http://www.gpo.gov/fdsys/pkg/PLAW-111publ148/html/PLAW-111publ148.htm. [Google Scholar]