Abstract
Background
Recent data suggest that patient activation, or having the knowledge, skills and confidence to engage and manage one's own health, favorably impacts patient behaviors and health outcomes. However, the role of activation in patients with heart failure is unknown.
Objectives
To measure the level of activation of patients hospitalized with acute decompensated heart failure (ADHF) and to determine whether activation is associated with in-hospital and early post-discharge outcomes.
Methods
We prospectively recruited Southeastern Minnesota residents hospitalized at Mayo Clinic hospitals with ADHF from January 2014- July 2015. Activation was measured using the Patient Activation Measure questionnaire.
Results
Among the 302 patients enrolled, the mean age was 77.3 years, 57.3% were men, and 46.8% had preserved ejection fraction. The median (25th-75th percentile) length of stay was 4 (3-7) days. In total, 7 (2.3%) patients died prior to discharge. Most survivors discharged to home (73.6%) or skilled nursing facilities (23.7%). The number (%) of patients in each activation level from highest to lowest was 9 (3.0%), 121 (40.1%), 122 (40.4%), and 50 (16.6%). Patients with lower activation were older, less educated, had lower patient satisfaction, and worse health literacy. They more often discharged to skilled nursing facilities and had higher 30-day mortality, though 30-day readmission did not differ by activation.
Conclusions
Patients hospitalized with ADHF with lower activation are less satisfied, have worse health literacy, more often require skilled care and are at increased risk for early post-discharge mortality. Activation can be easily measured and may help clinicians identify high-risk patients.
Keywords: heart failure, activation, mortality, readmission, health literacy
INTRODUCTION
Heart failure (HF) is a chronic life-limiting syndrome that negatively impacts health and places a huge burden on patients, families, and society. The morbidity and mortality associated with HF is substantial; the 5-year mortality is 50%(1, 2), and HF contributes to 1 in 9 deaths and more than 1 million hospitalizations each year in the United States(3). The risk for adverse outcomes in HF is highest around the time of a hospitalization for acute decompensated HF (ADHF)(4) and, as a result, HF has the highest 30-day readmission rate of any condition(5). Optimal disease management is critical to maintaining clinical stability and avoiding adverse outcomes in HF. However, it relies upon a patient's ability to actively manage their health by assimilating multiple tasks into their daily life(6, 7), such as taking medications as prescribed, adhering to dietary and fluid restrictions, exercising regularly, attending frequent clinical appointments, and recognizing and communicating with their clinicians when problems arise.
Recent studies have suggested that patient activation, or having the knowledge, skills, and confidence to engage in managing one's own health, favorably impacts patient behaviors and health outcomes. In a general population and in those with chronic illnesses such as diabetes, higher activation has been linked to healthier behaviors(8), higher use of preventive care(8), better disease management(9), lower resource utilization(9, 10), and lower costs of care(11). Given the complexity of HF self-care tasks, activated patients with HF may be better prepared to manage their health and, as a result, have better disease management and outcomes. However, the level of activation and association with outcomes in patients with HF has not been thoroughly examined. Therefore, we hypothesized that patient activation would be associated with in-hospital outcomes (length of stay, discharge location, mortality) and early post-discharge outcomes (30-day mortality, 30-day readmission) in HF. As a potentially modifiable factor(12, 13), if activation is associated with these outcomes, then it may represent a target for intervention.
The aim of this study was to delineate the level of activation of patients hospitalized with ADHF, and examine its association with patient characteristics and in-hospital and early post-discharge outcomes.
METHODS
Study Design
This is a prospective cohort study that was conducted in Southeastern Minnesota, an area relatively isolated from other urban centers with a limited number of providers, the largest of which is the Mayo Clinic, which delivers the vast majority of medical care to local residents. The Rochester Epidemiology Project(14), a medical record linkage system, allows the indexing of data for medical care of residents of Southeastern Minnesota, thus enabling the comprehensive capture of health-related events for the community's residents.
Patient Population
Patients hospitalized with ADHF at Mayo Clinic hospitals in Rochester, Minnesota were identified using a 2-step process. First, we used a validated natural language processing algorithm to screen electronic clinical notes for terms consistent with HF(15, 16). Each morning, computerized software screened the text of all notes generated and produced an excel file comprising patients identified as potential HF cases. Then, a research nurse would manually review the medical record of each potential HF case to determine whether they met study entry criteria. Patients were included in the study if they (1) had chronic HF, (2) were currently hospitalized with ADHF meeting Framingham criteria (3) were at least 20 years old, and (4) were residents of one of seven Southeastern Minnesota counties. Patients were excluded if they were incapable of completing the questionnaires due to mental or physical limitations. From January 21, 2014 through July 14, 2015, patients meeting entry criteria were approached in the hospital and invited to participate. All participants provided written authorization, and the study was approved by the Mayo Clinic Institutional Review Board.
Patient-Reported Data
Immediately following enrollment, participants were administered face-to-face questionnaires by a study coordinator. Activation was measured using the validated 13-item Patient Activation Measure (PAM)(17, 18). According to the developers of the PAM(18), patients who are activated believe patients have important roles in maintaining their health, know how to manage their condition and prevent health decline, and have the skills to maintain their health, collaborate with clinicians, and access appropriate care. Examples of items in the PAM include “I am confident that I can follow through on medical treatments I may need to do at home” and “When all is said and done, I am the person who is responsible for taking care of my health”. A summary score (range 0-100), with higher levels indicative of higher activation is generated based on the responses to the 13 PAM items using a proprietary conversion. Users are provided with a spreadsheet that calculates the PAM summary score upon purchasing a user license. Patients are assigned to one of four activation levels (1-4) based upon the summary score. Level 1 (lowest activation) individuals do not feel in charge of their health and care and may feel disengaged and overwhelmed. Level 2 (lower activation) have some knowledge about their health and condition, but are still struggling and feel that their health is largely out of their control. Level 3 patients (high activation) have basic knowledge about their health and condition and some confidence in their ability to manage their health. Level 4 patients (highest activation) have had some success in managing their health and adopting healthy behaviors but may still struggle during times of stress. Health literacy was assessed using the 3-item Health Literacy Screener(19), with poor health literacy defined as a total score of >10(20). Overall and financial satisfaction was measured using the general and financial satisfaction subscales of the Patient Satisfaction Questionnaire-18(21); scores range from 0-5 with higher scores indicating higher satisfaction. Patient reported health status was assessed using the single question “In general, would you say that your health is excellent, very good, good, fair or poor?” which has been predictive of outcomes in patients with HF(22). Marital status and education level were obtained by questionnaire.
Patient Characteristics
Other patient characteristics were extracted from their medical records, including demographics, comorbidities, and ejection fraction (EF). The Charlson comorbidity index was used to assess comorbidity(23). Resting left ventricular EF was collected from transthoracic echocardiograms performed within six months prior to one month after study enrollment. Preserved EF was defined as ≥50%(24).
Ascertainment of In-Hospital and Post-Discharge Outcomes
In hospital outcomes examined included length of stay, discharge location and mortality. Early post-discharge outcomes examined included 30-day readmission and 30-day mortality. In order to ensure that all participants had the opportunity for at least 30 days of follow-up, participants were followed through August 31, 2015 for all-cause death and readmission. Whether patients were discharged to home, a skilled nursing facility, assisted living facility, or other care arrangement was collected from the medical record. Mortality follow-up was available on all patients. The date of death was determined using death certificates filed in local counties, obituary notices, and electronic files of death certificates obtained from the State of Minnesota Department of Vital and Health Statistics. All readmissions to Mayo Clinic hospitals from the date of discharge to 30 days post-discharge were obtained using local administrative sources. The reason for readmission was categorized based on the principal (first) International Classification of Diseases, 9th revision (ICD-9) billing code.
Statistical Analysis
For each patient enrolled in the study, patient-reported data, patient characteristics, and outcomes were combined together in a single file for data analysis. Missing data were minimal; most variables were complete and all had <1% missing. For descriptive purposes, patient baseline characteristics and outcomes are presented by patient activation level (a 4-level categorical variable). Differences in baseline characteristics across activation levels were compared using generalized linear models for continuous variables and Mantel-Haenszel χ2 for categorical variables. The associations of activation and outcomes were examined using the PAM summary score as a continuous variable. The associations of activation and in-hospital mortality and discharge to nursing home were examined using logistic regression. The association of activation and hospital length of stay was examined using linear regression. Cox proportional hazard regression was used to examine the associations of activation and 30-day outcomes (readmission, mortality). All analyses were performed using Stata Version 13.0 (College Station, Texas).
RESULTS
A total of 375 patients were approached for inclusion in the study and 302 (80.5%) agreed to participate. Patients were elderly, had a high burden of comorbidities, and 47% had preserved EF (Table 1). Almost half (44%) had post-high school education, while 22% did not graduate high school. Most patients (56%) were married, while 24% were widowed, 13% were separated or divorced, and 7% were single/ never married.
Table 1.
Patient Characteristics by Activation Level
| Characteristic | Overall | Highest Activation (n=9) | High Activation (n=121) | Low Activation (n=122) | Lowest Activation (n=50) | P Value |
|---|---|---|---|---|---|---|
| Age, mean (SD), years | 77.3 (12.9) | 74.4 (11.7) | 73.6 (13.2) | 80.7 (11.9) | 78.5 (12.5) | 0.001 |
| Male | 173 (57.3) | 4 (44.4) | 72 (59.5) | 68 (55.7) | 29 (58.0) | 0.59 |
| Non-Hispanic Whites | 279 (92.4) | 8 (88.9) | 108 (89.3) | 116 (95.1) | 47 (94.0) | 0.72 |
| Preserved ejection fraction (≥50%) | 141 (46.8) | 3 (33.3) | 57 (47.1) | 56 (45.9) | 25 (51.0) | 0.53 |
| Comorbidities | ||||||
| Hypertension | 220 (83.3) | 8 (88.9) | 91 (82.7) | 88 (83.8) | 33 (82.5) | 0.87 |
| Diabetes mellitus | 137 (45.4) | 4 (44.4) | 57 (47.1) | 57 (46.7) | 19 (38.0) | 0.40 |
| COPD | 82 (27.2) | 3 (33.3) | 26 (21.5) | 36 (29.5) | 17 (34.0) | 0.13 |
| Prior myocardial infarction | 81 (26.8) | 4 (44.4) | 37 (30.6) | 30 (24.6) | 10 (20.0) | 0.062 |
| Malignancy | 39 (12.9) | 2 (22.2) | 12 (9.9) | 21 (17.2) | 4 (8.0) | 0.91 |
| Peripheral vascular disease | 52 (17.2) | 2 (22.2) | 25 (20.7) | 20 (16.4) | 5 (10.0) | 0.088 |
| Cerebrovascular disease | 59 (19.5) | 0 (0) | 19 (15.7) | 28 (23.0) | 12 (24.0) | 0.052 |
| Depression | 50 (16.6) | 0 (0) | 14 (11.6) | 25 (20.5) | 11 (22.0) | 0.019 |
| Charlson comorbidity index >=3 | 169 (56.0) | 3 (33.3) | 66 (54.5) | 70 (57.4) | 30 (60.0) | 0.24 |
| Overweight/ obese (BMI≥25 kg/m2) | 242 (80.1) | 7 (77.8) | 96 (79.3) | 95 (77.9) | 44 (88.0) | 0.32 |
| Marital Status | 0.78* | |||||
| Married/ living with a partner | 170 (56.3) | 6 (66.7) | 67 (55.4) | 70 (57.4) | 27 (54.0) | |
| Single/ never married | 21 (7.0) | 0 | 10 (8.3) | 5 (4.1) | 6 (12.0) | |
| Separated/ Divorced | 38 (12.7) | 1 (11.1) | 20 (16.5) | 11 (9.0) | 6 (12.0) | |
| Widowed | 72 (24.2) | 2 (22.2) | 24 (19.8) | 36 (29.5) | 11 (22.0) | |
| Fair or poor health status | 219 (72.5) | 5 (55.6) | 86 (71.1) | 88 (72.1) | 40 (80.0) | 0.16 |
| Post-high school education | 134 (44.4) | 7 (77.8) | 61 (50.4) | 50 (41.0) | 16 (32.0) | 0.003 |
| Location prior to admission | <0.001† | |||||
| Home | 250 (82.8) | 9 (100.0) | 112 (92.6) | 92 (75.4) | 37 (74) | |
| Skilled Nursing Facility | 23 (7.6) | 0 | 6 (5.0) | 14 (11.5) | 3 (6) | |
| Assisted Living Facility | 28 (9.3) | 0 | 3 (2.5) | 16 (13.1) | 9 (18) | |
| Other | 1 (0.3) | 0 | 0 | 0 | 1 (2) | |
| Poor health literacy | 85 (28.2) | 0 | 22 (18.2) | 43 (35.5) | 20 (40.0) | <0.001 |
| General patient satisfaction | 3.7 (0.5) | 4.3 (0.6) | 3.8 (0.5) | 3.7 (0.5) | 3.3 (0.5) | <0.001 |
| Financial patient satisfaction | 3.5 (1.1) | 4.4 (0.9) | 3.7 (1.0) | 3.5 (1.0) | 3.0 (1.2) | <0.001 |
Values shown are N(%) unless otherwise indicated. BMI=body mass index; COPD= chronic obstructive pulmonary disease; SD=standard deviation
P value for proportion of patients married/ living with a partner by activation level
P value for proportion of patients living at home by activation level
Patient activation scores ranged from 29-100 (median 53.2, 25th-75th percentile 48.9-55.6). The number (%) of patients in each activation category from highest to lowest was 9 (3.0%), 121 (40.1%), 122 (40.4%), and 50 (16.6%). Patients who were less activated were older, less educated, had worse general and financial satisfaction, and worse health literacy (Table 1). Patients who were less activated also more often had a history of depression.
The median (25th-75th percentile) hospital length of stay was 4 (3-7) days. In total, 7 (2.3%) patients died in the hospital, while the remainder were discharged home (n=217, 73.6%), to assisted living facilities (n=6, 2.0%), skilled nursing facilities (n=70, 23.7%), or to other care arrangements (n=2, 0.7%). The 30-day readmission rate was 21.7%. The most common reasons for readmission were HF (32.8% of readmissions) and respiratory failure (7.8%). The 30-day mortality rate was 7.0%. Of those that died within 30 days of hospital discharge, 10 (47.6%) died in the hospital, 4 (19.0%) died at home, 5 (23.8%) in skilled nursing facilities, 1 (4.8%) in inpatient hospice, and 1 (4.8%) in an assisted living facility. In total, 12 (57.1%) saw palliative care in consultation in the two months prior to death and 6 (28.6%) enrolled in hospice.
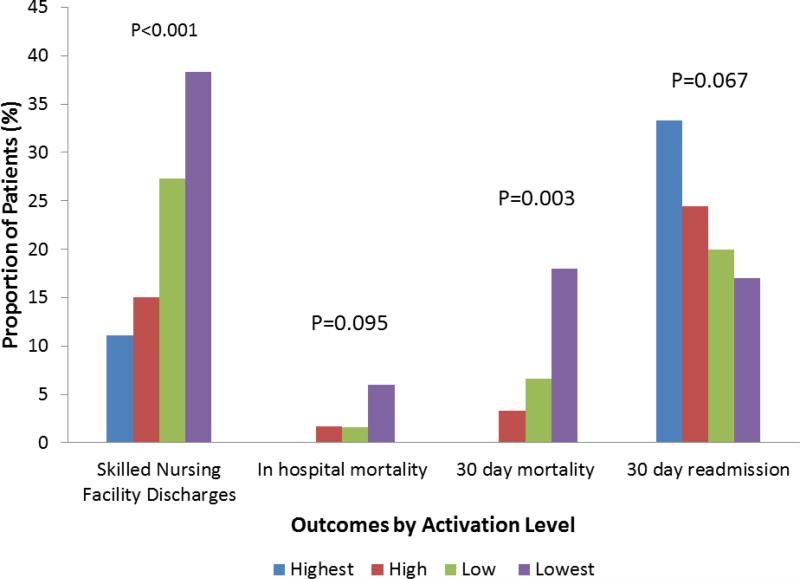
The associations of patient activation and in-hospital and early post-discharge outcomes are shown in Table 2 and Figure 1. There was a stepwise increase in the proportion of patients who discharged to skilled nursing facilities with decreasing activation (p <0.001). Even when patients who were residents of skilled nursing facilities on admission where excluded, the proportion of new nursing home discharges still increased with decreasing activation (11.1%, 12.3%, 23.4%, and 32.6%, for those with highest to lowest activation, respectively, p <0.001). The odds of requiring a skilled nursing facility at hospital discharge was 3.6 (95% CI 1.7-7.8) for patients with the lowest activation and 2.2 (1.2-4.1) for patients with low activation compared with patients with the highest two levels of activation. The odds of discharge to a skilled nursing facility increased 10% with each 1-point decrease in PAM (OR 1.10, 95% CI 1.05-1.15, p<0.001). The association persisted after adjusting for age and comorbidity (OR 1.08, 95% CI 1.03-1.14, p<0.001).
Table 2.
In-Hospital and Post-Hospital Outcomes by Activation Level
| Characteristic | Highest Activation | High Activation | Low Activation | Lowest Activation | P Value |
|---|---|---|---|---|---|
| Hospital Length of Stay, days, median (25th, 75th percentile) | 3 (2.5, 8.5) | 4 (3, 7.5) | 4 (3, 7) | 5 (3, 8) | 0.92 |
| In Hospital Mortality, % | 0 | 2 (1.7) | 2 (1.6) | 3 (6.0) | 0.095 |
| Discharge To: | <0.001 | ||||
| Home | 8 (88.9) | 99 (82.5) | 81 (66.9) | 29 (61.7) | |
| Skilled Nursing Facility | 1 (11.1) | 18 (15.0) | 33 (27.3) | 18 (38.3) | |
| Assisted Living Facility | 0 | 2 (1.7) | 4 (3.3) | 0 | |
| Other | 0 | 1 (0.8) | 3 (2.5) | 0 | |
| 30-day Mortality | 0 | 4 (3.3) | 8 (6.6) | 9 (18.0) | 0.003 |
| 30-day Readmission | 3 (33.3) | 29 (24.4) | 24 (20.0) | 8 (17.0) | 0.067 |
| 30-day Readmission Accounting for Out-of-Hospital Death* | 3 (33.3) | 29 (24.4) | 28 (23.3) | 12 (25.5) | 0.88 |
Values shown are N(%) unless otherwise noted.
Patients who experienced out-of-hospital death were assumed to be readmitted on the day of death
Figure. Outcomes by Patient Activation.
The proportion of patients experiencing each health outcome by patient activation level is shown. P values are for trend across activation levels.
A stepwise increase in 30-day mortality with decreasing activation was also observed. None of the patients who died within 30 days of hospitalization were in the highest activation level, and 81% were in the lowest two activation levels. The risk of 30-day mortality was 6.4 (95% CI 2.1-23.7) for patients with the lowest activation and 2.2 (95% CI 0.70-8.3) for patients with low activation compared to patients with the highest two levels of activation. The risk of death increased 10% with each 1-point decrease in PAM (HR 1.10, 95% CI 1.03-1.17, p=0.003). The association persisted after adjusting for age and comorbidity (HR 1.09, 95% CI 1.03-1.16, p=0.006). As only 7 patients died during their index hospitalization, the association between activation and in-hospital mortality did not reach statistical significance (OR per 1-point decrease in PAM 1.10, 95% CI 0.98-1.24, p=0.095).
The association between patient activation and 30-day readmission was not statistically significant (HR per 1 point decrease in PAM 0.97, 95% CI 0.95-1.01, p=0.067), but there was a stepwise increase in 30-day readmission rates in patients with higher activation. However, this was because patients with low activation often died before they could be readmitted. When we assumed that patients who died within 30 days would have been readmitted on the day of death, the 30-day readmission rate was similar across activation levels (33.3%, 24.4%, 23.3%, 25.5% for those from highest to lowest activation, respectively). No significant association between patient activation and length of stay was observed (β=0.06, 95% CI -0.10-0.11, p=0.92).
DISCUSSION
We chose to focus on evaluating the association between patient activation and in-hospital and early post-discharge outcomes, as this is a period of enhanced risk in patients with HF(4) where intervention might be beneficial. Among community patients hospitalized with ADHF, low activation was common, particularly in patients who were older; less educated and with poor health literacy. Lower activation was associated with worse patient satisfaction, increased need for skilled nursing facility care at hospital discharge, and higher 30-day mortality. Patient activation did not differ by comorbidity burden, health status, or EF, and was not predictive of 30-day readmission.
Activation in patients hospitalized with ADHF is lower than has been previously measured in a general ambulatory population(8, 11) and in patients hospitalized in a general medical ward(10). For example, in a large outpatient primary care population, four out of five patients were in the highest two levels of activation, compared with only two out of five in our study. Patients with chronic disease tend to be less activated(9, 25), though the proportion of patients at the highest activation level in this study (3.0%) was less than has been reported in ambulatory populations. This could reflect that we are capturing a high-risk population, and they may feel a lack of control over their health while in the hospital and over their condition given their acute decompensation.
Similar to others, we found that activation was higher in patients who were younger(25, 26), more educated(10, 25, 26), and in those with better health literacy(10). Previous HF literature demonstrates that health literacy is associated with enhanced HF knowledge and better self-care(27, 28), and our results suggest that these patients also have higher activation. The association of activation with age is intriguing but may reflect that older adults with HF frequently have concomitant geriatric syndromes, such as impaired cognition and limitations in functional mobility(29, 30) that can make self-care and disease management more challenging. Several prior studies have noted that patients who are less activated are more likely to have depression(10, 25), consistent with our findings. Symptoms associated with depression such as anhedonia, difficulty concentrating, and insomnia can make it more difficult for patients to feel confident in engaging in their healthcare decisions and management. Unlike prior studies(18, 25, 26, 31), we found no association between activation and health status. However, it is important to note that the health status of patients in this study was quite poor, and could explain the variation in our findings compared with prior reports.
Patient Activation and Outcomes
In this study, lower activation was associated with higher 30-day mortality, and patients at the lowest activation level had a more than 6-fold increased risk of death within 30-days of hospital discharge compared with patients in the highest two activation levels. To the best of our knowledge, this is the first study to find an association between patient activation and mortality. However, other measures of self-care such as medication adherence have been associated with risk of death in patients with chronic conditions including HF(32, 33). The PAM is easy to administer, and could represent a simple way to identify patients at increased risk for death in the early post-discharge period. Notably, half of patients who died within 30 days of hospital discharge saw palliative care specialists in consultation prior to death and one-quarter enrolled in hospice, likely indicating that clinicians recognized that the patients were approaching the end-of-life. However, other patients also suffered unanticipated deaths, and measuring activation during hospitalization may be another trigger for providers to discuss goals of care with patients. It is important to recognize that low activation may not cause death, but rather, patients with HF who are nearing the end-of-life may be less activated and feel less control over their health.
Second, we found that activation was strongly associated with nursing home placement. Post-acute care use is common after an acute hospitalization, and represents a substantial burden to the healthcare system(34). The need for nursing home care is frequent in patients hospitalized with ADHF; in the Get with the Guidelines program, 24.1% of patients were discharged to a nursing home after hospitalization(35), which is similar to the 23.7% we observed. Some of these patients only need acute rehabilitation rather than long-term care, and an intervention to improve activation targeting patients discharged to skilled nursing facilities may be of interest to explore in future studies.
We found no association between patient activation and 30-day readmission. This is in contrast to prior studies demonstrating that patients with higher activation are less likely to be hospitalized(9) and rehospitalized(10). There are potential reasons why our findings vary from prior reports. As previously noted, the health status of patients in this study is worse than in prior studies; patients in this study were plagued with a high symptom and disease burden. While activation may help to avoid readmissions that could have been prevented by improved medication adherence and disease management, many of the readmissions may have been unavoidable, regardless of activation level.
Finally, we found no association between patient activation and in-hospital mortality or length of stay. However, the in-hospital mortality rate in patients with HF is only 3.3%(36), which is similar to the 2.3% in our study, and as such we were limited in our ability to detect a difference in this relatively rare outcome.
Prior work has suggested that patient activation changes over time(11) and can be modified. Interventions to improve activation have had some success. One trial reported that patients randomized to participate in a weekly workshop, covering topics such as dealing with frustration, effective communication techniques, nutrition, and exercise, had greater improvements in activation over six weeks compared with a control group(12). A trial of a nurse-led intervention in 84 patients with HF found that patients randomized to the intervention had increased activation and fewer hospitalizations than the control arm(13). This study now demonstrates that lower activation is associated with the need for skilled nursing facility care and 30-day mortality in patients hospitalized with ADHF. Further work is needed to understand if patient activation can increase in response to intervention in this high-risk population and, if so, whether improvement in activation translates into better health outcomes.
Strengths and Limitations
There are limitations that should be acknowledged to aid in interpretation of these data. First, we were limited in our ability to evaluate the associations of activation and infrequent outcomes, such as in-hospital mortality, and these findings should be replicated in larger patient populations. Second, this study was performed in a single community, and associations may vary in other geographic areas. However, it should be acknowledged that the characteristics of the local population are similar to the state of Minnesota and the Upper Midwest United States(37). Third, if readmission occurred to a non-Mayo hospital, it was not captured. However, the 30-day readmission rate in this study (22%) is very similar to the national 30-day readmission rate for HF (22.7%), making it unlikely that we missed a large number of readmissions. Conversely, there are several notable strengths. To the best of our knowledge, this is the first study to investigate the associations of activation and outcomes in patients with hospitalized with ADHF. We were able to assess activation and several other key constructs such as patient satisfaction and health literacy in a group of high-risk patients with HF.
Conclusions
Most patients hospitalized with ADHF have low activation, and therefore lack the skills, confidence, and motivation to manage their own health. Those with lower activation are less satisfied with their care, more often require skilled care at hospital discharge, and have higher 30-day mortality. Future studies are needed to understand whether interventions can improve patient activation in this high-risk population.
ACKNOWLEDGMENTS
We thank William Lehman, Annette McNallan RN, and Ellen Koepsell RN for their help with patient identification, recruitment, and data collection for the study.
Source of Funding: This study was supported by a grant from the National Institutes of Health (K23 HL116643, PI: Shannon M. Dunlay).
ABBREVIATIONS
- ADHF
acute decompensated heart failure
- EF
ejection fraction
- HF
heart failure
- PAM
patient activation measure
Footnotes
Conflicts of Interest
The authors have no conflicts of interest.
REFERENCES
- 1.Gerber Y, Weston SA, Redfield MM, Chamberlain AM, Manemann SM, Jiang R, et al. A contemporary appraisal of the heart failure epidemic in Olmsted County, Minnesota, 2000 to 2010. JAMA Int Med. 2015;175(6):996–1004. doi: 10.1001/jamainternmed.2015.0924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roger VL, Weston SA, Redfield MM, Hellermann-Homan JP, Killian J, Yawn BP, et al. Trends in heart failure incidence and survival in a community-based population. JAMA. 2004;292(3):344–50. doi: 10.1001/jama.292.3.344. [DOI] [PubMed] [Google Scholar]
- 3.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation. 2015;133(4):e38–e360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 4.Dharmarajan K, Hsieh AF, Kulkarni VT, Lin Z, Ross JS, Horwitz LI, et al. Trajectories of risk after hospitalization for heart failure, acute myocardial infarction, or pneumonia: retrospective cohort study. BMJ. 2015;350:h411. doi: 10.1136/bmj.h411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. New Engl J Med. 2009;360(14):1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 6.Artinian NT, Magnan M, Sloan M, Lange MP. Self-care behaviors among patients with heart failure. Heart Lung. 2002;31(3):161–72. doi: 10.1067/mhl.2002.123672. [DOI] [PubMed] [Google Scholar]
- 7.Riegel B, Vaughan Dickson V, Goldberg LR, Deatrick JA. Factors associated with the development of expertise in heart failure self-care. Nurs Res. 2007;56(4):235–43. doi: 10.1097/01.NNR.0000280615.75447.f7. [DOI] [PubMed] [Google Scholar]
- 8.Greene J, Hibbard JH. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J Gen Intern Med. 2012;27(5):520–6. doi: 10.1007/s11606-011-1931-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Remmers C, Hibbard J, Mosen DM, Wagenfield M, Hoye RE, Jones C. Is patient activation associated with future health outcomes and healthcare utilization among patients with diabetes? J Ambul Care Manage. 2009;32(4):320–7. doi: 10.1097/JAC.0b013e3181ba6e77. [DOI] [PubMed] [Google Scholar]
- 10.Mitchell SE, Gardiner PM, Sadikova E, Martin JM, Jack BW, Hibbard JH, et al. Patient activation and 30-day post-discharge hospital utilization. J Gen Intern Med. 2014;29(2):349–55. doi: 10.1007/s11606-013-2647-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Greene J, Hibbard JH, Sacks R, Overton V, Parrotta CD. When patient activation levels change, health outcomes and costs change, too. Health Affairs. 2015;34(3):431–7. doi: 10.1377/hlthaff.2014.0452. [DOI] [PubMed] [Google Scholar]
- 12.Hibbard JH, Mahoney ER, Stock R, Tusler M. Do increases in patient activation result in improved self-management behaviors? Health Serv Res. 2007;42(4):1443–63. doi: 10.1111/j.1475-6773.2006.00669.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shively MJ, Gardetto NJ, Kodiath MF, Kelly A, Smith TL, Stepnowsky C, et al. Effect of patient activation on self-management in patients with heart failure. J Cardiovasc Nurs. 2013;28(1):20–34. doi: 10.1097/JCN.0b013e318239f9f9. [DOI] [PubMed] [Google Scholar]
- 14.Rocca WA, Yawn BP, St Sauver JL, Grossardt BR, Melton LJ., 3rd History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proceed. 2012;87(12):1202–13. doi: 10.1016/j.mayocp.2012.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bursi F, Weston SA, Redfield MM, Jacobsen SJ, Pakhomov S, Nkomo VT, et al. Systolic and diastolic heart failure in the community. JAMA. 2006;296(18):2209–16. doi: 10.1001/jama.296.18.2209. [DOI] [PubMed] [Google Scholar]
- 16.Pakhomov S, Weston SA, Jacobsen SJ, Chute CG, Meverden R, Roger VL. Electronic medical records for clinical research: application to the identification of heart failure. Am J Manag Care. 2007;13(6 Part 1):281–8. [PubMed] [Google Scholar]
- 17.Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res. 2005;40(6 Pt 1):1918–30. doi: 10.1111/j.1475-6773.2005.00438.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39(4 Pt 1):1005–26. doi: 10.1111/j.1475-6773.2004.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36(8):588–94. [PubMed] [Google Scholar]
- 20.Peterson PN, Shetterly SM, Clarke CL, Bekelman DB, Chan PS, Allen LA, et al. Health literacy and outcomes among patients with heart failure. JAMA. 2011;305(16):1695–701. doi: 10.1001/jama.2011.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marshall GN, Hays RD. The Patient Satisfaction Questionnaire Short Form (PSQ-18) RAND Corporation; Santa Monica, CA: 1994. http://www.rand.org/pubs/papers/P7865.html. [Google Scholar]
- 22.Chamberlain AM, Manemann SM, Dunlay SM, Spertus JA, Moser DK, Berardi C, et al. Self-rated health predicts healthcare utilization in heart failure. JAHA. 2014;3(3):e000931. doi: 10.1161/JAHA.114.000931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 24.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr., Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62(16):e147–239. doi: 10.1016/j.jacc.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 25.Bos-Touwen I, Schuurmans M, Monninkhof EM, Korpershoek Y, Spruit-Bentvelzen L, Ertugrulvan der Graaf I, et al. Patient and disease characteristics associated with activation for self-management in patients with diabetes, chronic obstructive pulmonary disease, chronic heart failure and chronic renal disease: a cross-sectional survey study. PloS One. 2015;10(5):e0126400. doi: 10.1371/journal.pone.0126400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nijman J, Hendriks M, Brabers A, de Jong J, Rademakers J. Patient activation and health literacy as predictors of health information use in a general sample of Dutch health care consumers. J Health Commun. 2014;19(8):955–69. doi: 10.1080/10810730.2013.837561. [DOI] [PubMed] [Google Scholar]
- 27.Chen AM, Yehle KS, Albert NM, Ferraro KF, Mason HL, Murawski MM, et al. Health Literacy Influences Heart Failure Knowledge Attainment but Not Self-Efficacy for Self-Care or Adherence to Self-Care over Time. Nurs Res Pract. 2013;2013:353290. doi: 10.1155/2013/353290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen AM, Yehle KS, Plake KS, Murawski MM, Mason HL. Health literacy and self-care of patients with heart failure. J Cardiovasc Nurs. 2011;26(6):446–51. doi: 10.1097/JCN.0b013e31820598d4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dunlay SM, Manemann SM, Chamberlain AM, Cheville AL, Jiang R, Weston SA, et al. Activities of daily living and outcomes in heart failure. Circ Heart Fail. 2015;8(2):261–7. doi: 10.1161/CIRCHEARTFAILURE.114.001542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Murad K, Goff DC, Jr., Morgan TM, Burke GL, Bartz TM, Kizer JR, et al. Burden of Comorbidities and Functional and Cognitive Impairments in Elderly Patients at the Initial Diagnosis of Heart Failure and Their Impact on Total Mortality: The Cardiovascular Health Study. JACC Heart Fail. 2015;3(7):542–50. doi: 10.1016/j.jchf.2015.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Skolasky RL, Green AF, Scharfstein D, Boult C, Reider L, Wegener ST. Psychometric properties of the patient activation measure among multimorbid older adults. Health Serv Res. 2011;46(2):457–78. doi: 10.1111/j.1475-6773.2010.01210.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Granger BB, Swedberg K, Ekman I, Granger CB, Olofsson B, McMurray JJ, et al. Adherence to candesartan and placebo and outcomes in chronic heart failure in the CHARM programme: double-blind, randomised, controlled clinical trial. Lancet. 2005;366(9502):2005–11. doi: 10.1016/S0140-6736(05)67760-4. [DOI] [PubMed] [Google Scholar]
- 33.Bailey JE, Wan JY, Tang J, Ghani MA, Cushman WC. Antihypertensive medication adherence, ambulatory visits, and risk of stroke and death. J Gen Intern Med. 2010;25(6):495–503. doi: 10.1007/s11606-009-1240-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mechanic R. Post-acute care--the next frontier for controlling Medicare spending. New Engl J Med. 2014;370(8):692–4. doi: 10.1056/NEJMp1315607. [DOI] [PubMed] [Google Scholar]
- 35.Allen LA, Hernandez AF, Peterson ED, Curtis LH, Dai D, Masoudi FA, et al. Discharge to a skilled nursing facility and subsequent clinical outcomes among older patients hospitalized for heart failure. Circ Heart Fail. 2011;4(3):293–300. doi: 10.1161/CIRCHEARTFAILURE.110.959171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen J, Dharmarajan K, Wang Y, Krumholz HM. National trends in heart failure hospital stay rates, 2001 to 2009. J Am Coll Cardiol. 2013;61(10):1078–88. doi: 10.1016/j.jacc.2012.11.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ, 3rd, Rocca WA. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proceed. 2012;87(2):151–60. doi: 10.1016/j.mayocp.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]