Abstract
This special interest article provides a historical framework with a contemporary case example that traces the infusion of the science of motor learning into neurorehabilitation practice. The revolution in neuroscience provided the first evidence for learning-dependent neuroplasticity and presaged the role of motor learning as critical for restorative therapies after stroke. The scientific underpinnings of motor learning have continued to evolve from a dominance of cognitive or information processing perspectives to a blend with neural science and contemporary social-cognitive psychological science. Furthermore, advances in the science of behavior change have contributed insights into influences on sustainable and generalizable gains in motor skills and associated behaviors, including physical activity and other recovery-promoting habits. For neurorehabilitation, these insights have tremendous relevance for the therapist–patient interactions and relationships. We describe a principle-based intervention for neurorehabilitation termed the Accelerated Skill Acquisition Program that we developed. This approach emphasizes integration from a broad set of scientific lines of inquiry including the contemporary fields of motor learning, neuroscience, and the psychological science of behavior change. Three overlapping essential elements—skill acquisition, impairment mitigation, and motivational enhancements—are integrated.
Keywords: neuroplasticity, motivation, motor control, motor learning, recovery, self-efficacy, skill acquisition, stroke
INTRODUCTION
Neuroscientific evidence over the past few decades, revealing the inherent plasticity of the brain (neuroplasticity) that allows new learning, adaptation, and compensation at multiple levels of the system from early development well into old age, has had profound implications for rehabilitation and recovery. In fact, this insight has heightened the relevance of the science of motor learning to physical therapist practice. Before the revolution in neuroscience, researchers in the field of motor learning had established a number of behavioral variables important for skill acquisition, chief among them—practice. The science of motor learning itself continues to evolve, providing new insights into the optimization of skill learning and its application to the complex process of neurorehabilitation. Throughout this special interest article, we use the terms skill acquisition and learning, synonymously. Furthermore, we distinguish performance from learning. The learning–performance distinction1,2 has relevance to physical therapy in that the concern is with the achievement of a sustainable or relatively permanent change in the capability for responding (learning) in contrast to a short-lasting temporary change (performance). We now understand that some practice-related techniques such as drills and frequent feedback can have a performance-enhancing effect that boosts performance while available. Similarly, some practice-related interventions may seem to retard or slow performance gains when present, seen, for example when tasks are ordered randomly.3 An assessment of learning and the associated memory processes is not reliable unless it is conducted at some time or context that is removed from the practice period, such as during retention or transfer tests.4–7
The purpose of this special interest article with contemporary exemplar is to (1) provide a historical overview of the integration of motor learning into neurologic physical therapy, (2) emphasize emerging findings in the field of motor learning that involve incorporation of contemporary neuroscience and social-cognitive psychological science, and (3) describe the Accelerated Skill Acquisition Program (ASAP), a patient-centered intervention with elements of skill, capacity, and motivation that support motor learning and is consistent with this new knowledge. Skill in the ASAP refers both to the acquisition of skilled movement and to skills for self-management. The pursuit of skilled movement, rather than merely functional actions, is both relatively demanding and engaging and invokes natural goal-directed advantages. Capacity in the ASAP pertains to impairment mitigation or restoration of physical and physiological capabilities. Motivation in the ASAP encompasses intrinsic motivation associated with satisfaction of fundamental psychological needs, including self-efficacy. With this perspective, we hope to stimulate future programmatic research at the theory and application level.
MOTOR LEARNING AND PHYSICAL THERAPY: A BRIEF HISTORY
Introducing Motor Learning to Physical Therapy: The STEP Conferences
Despite earlier recognition of the importance of practice,8 other techniques concerning recovery and repair of the nervous system prevailed and influenced therapeutic practice well into the 20th century (eg, abnormal reflex and spasticity management, neuromuscular facilitation techniques). Two notable and important professional meetings highlighted the limited integration of the study of motor learning for physical therapy. Both meetings were supported by the Special Therapeutic Exercise Project (STEP) conferences. The first was the opportunity for dialogue between academic scientists and clinicians that was afforded by the first STEP meeting held over 3 weeks in the summer of 1966 at Northwestern University (NU).9 The conference and its proceedings became known as NUSTEP. Motor learning was not a prevalent topic at the meeting. Rather, academic scientists and clinicians were struggling to integrate recent knowledge of basic neurophysiology of human reflex mechanisms into the application of therapeutic exercise.9 However, there were 3 conference articles that dealt with aspects of motor learning; most relevant to this discussion was one written by Cross entitled, Role of practice in perceptual-motor learning10; another by Fischer entitled, Factors affecting motor learning11; and a third by Mathis, entitled Motivation and emotion in learning.12 Unfortunately, these articles were almost entirely ignored by a majority of the physical therapy community,* and except for a few rare instances, they were not integrated into standard curricula in most physical therapy education programs.
Largely ignored, Cross’s observations and insight about practice for motor learning anticipated much of the current evidence regarding the importance of task-specific practice.13 As Cross noted, for practice to affect motor learning, it must have purpose and goal-directedness, “…practice is more than mere repetition, it is repetition with a purpose.”10 Cross went on to distinguish practice from exercise, “Although exercise and practice are often used interchangeably, exercise … refer(s) to repetitious performance of an already learned act with the purpose of modifying in some way one’s physical characteristics (musculature, physical strength or physique).”10 Most surprisingly, Cross’ now 46-year-old writings about practice and motor learning were remarkably prophetic concerning some of the most important advances in motor learning theory: “Performance of any overt or covert act one or more times with a view to fixating or improving the spatial and temporal organization of the same or any other act … changes which occur during practice have some neuroanatomical locus … nature of these changes can be defined only when this locus has been identified.”10 These advances included schema theory for discrete movements,14 the neuropsychological perspective of motor learning,15 the neural correlates of movement representations,16 the importance of consolidation processes,17,18 and even the recent demonstration of motor learning through mental practice alone.19
Twenty-four years after NUSTEP, there was early evidence that behavioral perspectives on motor learning and control were beginning to influence the profession, most notably with the 1987 Movement Science: Foundations for Physical Therapy and Rehabilitation book, edited by Carr, Shepherd, Gordon, Gentile, and Held20 and the special issue of Physical Therapy devoted to movement science that appeared a few years later.21 The group at Teacher’s College Columbia University Movement Science and Education Program was clearly a trailblazer in this area. At the time of the second STEP (II STEP) conference in 1990, Schmidt, a central figure whose research focus was the behavioral basis of motor learning, gave one of the plenary talks entitled Motor Learning Principles for Physical Therapy.22 As an outsider to the physical therapy profession, he confessed that initially he thought the kinds of problems physical therapists were confronted with were analogous to “hardware” problems (eg, muscles, bones, and nerves), and not the kinds of “software” problems that represent the science of mental life and behavior (eg, motor planning, learning, and transfer). This software analogy is reflected today in many popular applications related to neuroplasticity.23
Until the II STEP conference, there was little evidence of communication between academic circles in motor learning and physical therapy with one notable exception previously mentioned—the Teacher’s College group led by Gentile in New York. There was very little content in physical therapy curricula about motor learning or its foundational sciences (ie, psychological science). The tide began to change after II STEP,24 with more cross-fertilization at scientific and professional meetings, and as the academic physical therapy enterprise began to take hold, basic and applied knowledge in motor learning along with other areas of movement science (eg, motor development and exercise science) was integrated and infused into physical therapy curricula.
In 2005, the third of the STEP conferences (III STEP) was held in Salt Lake City, Utah. The theme was linking movement science and intervention. Relative to the 2 proceeding STEP conferences, the program of III STEP reflected a much stronger emphasis on motor learning, neuroplasticity, and motivation.* The interested reader may wish to consult the special issue of Journal of Neurologic Physical Therapy in 2006 for papers from III STEP.25 The fourth STEP conference is planned for July 2016.
Commonalities Between Motor Learning Research and Physical Therapy Practice
Schmidt22 identified a number of commonalities between motor learning research and physical therapy practice in his II STEP paper, namely:
In a physical therapy session, many different things happen, but one of these is practice.
Patients are engaged in repeated attempts to produce motor behaviors that are beyond their present capabilities (analogous to a person learning to play a musical instrument).
In physical therapy, although the behaviors are not exactly new as they are in other motor learning settings, they can be considered as new in the sense that they are no longer available as a result of an injury that might be peripheral or central (eg, loss of gait from spinal cord or central brain injury.
At least part of the product of participation in physical therapy seems to be the acquisition of the capabilities to use the existing (albeit damaged) motor system.
The patient seems to be learning to use the damaged motor system in a new way to accomplish an environmental goal that may have been achieved earlier—but perhaps in a different way—before the system was damaged.
In this process, the therapist acts as a facilitator-instructor, using many of the same kinds of techniques that have been emphasized (although often under different names) in motor learning, such as providing instructions, physical or verbal guidance, feedback about errors, suggestions for modifications, and encouragement, just as a teacher or coach in other contexts of motor learning would do.
The way that the therapy session is structured, the activities that are to be performed, as well as their order and relative amounts—are all problems that face both the therapist and the traditional instructor in planning their respective sessions.
To a large extent, these observations have been particularly useful in shaping the research and practice agendas around the application of motor learning principles for physical therapy.28–36
NEUROPLASTICITY HEIGHTENS THE IMPORTANCE OF MOTOR LEARNING
It took until the turn of the 21st century before studies began to appear in the literature that examined motor learning in clinical populations.28,37 At about the same time, in 1996 Nudo and colleagues38 published the now seminal paper in the journal Science. In that study, using a primate model of stroke, they demonstrated the capability of the motor cortex to reorganize the digit representation area in response to postinjury motor training, but not as a consequence of spontaneous recovery in the absence of training. More importantly, Nudo and colleagues showed that cortical reorganization of the digit area was the direct result of the food-retrieval practice paradigm used to train the primates after the stroke lesion. In later work, Plautz and colleagues39 further identified that cortical reorganization was dependent on goal-directed, task-specific practice, likely the result of acquisition of a motor skill (ie, motor learning), and not mere repetition of grasping movements from the easiest and largest food wells.
Noted neuroscientist Merzenich said, “The brain is a learning machine” (personal communication, Merzenich M., July 17, 2005). With the advent of new brain imaging technology, it is now well accepted that the learning of motor skills results in adaptive changes in the functional organization of the motor system.40,41 Attempts at skilled movements together with injury-induced plasticity (eg, stroke or head injury) can influence the use of injury-affected musculature and subsequent reorganization of spared neuronal networks.42 Research over the last decade has provided considerable evidence that has advanced knowledge about how to shape plasticity to enhance recovery after injury.43,44
PERSPECTIVES ON SKILL ACQUISITION, SUSTAINABILITY, AND GENERALIZABILITY
There is now sufficient evidence that the acquisition of a new motor skill requires progressive challenge, intensity, problem solving, sufficient motivation, and focused attention, especially in the early stages of learning.2,13,45,46 We also know that skill-based learning involves active participation and requires a certain degree of voluntary neuromotor capability. Most motor skills involve procedural (implicit) memory and knowledge and require little attention once they are learned.47–49
Recently, motivational factors involved in long-term behavioral engagement, including self-efficacy and support for fundamental psychological needs (competence, autonomy support, social-relatedness),50–53 have been examined with respect to their role in motor performance and learning, as reflected in acquisition and retention of novel motor skills in clinical and nonclinical populations.46,54–56 For example, relative to a control group, older women learning a novel balance task who were provided a single statement before beginning indicating that “active people like you, with your experience, usually do very well on this task,” retained learning, balanced longer, and had higher self-efficacy on a delayed test of learning.54 Individuals in inpatient stroke rehabilitation given feedback and encouragement of daily timed gait trials walked significantly faster both at discharge and 3 months later than those not provided with their times and encouragement.56 In another study the impact in individuals with Parkinson disease of learner control or autonomy support over a condition of practice was evaluated. Learner control over which trials to practice a balance task with the aid of a balance pole was contrasted to identical use of the balance pole in a yoked group without choice over use. Those who had choice, relative to the yoked group, demonstrated better balance performance on a retention test.55 These studies demonstrate that motivational factors exert an influence on learning and retention.
In a manner not unlike the effects of exercise that will not be retained unless the exercise is continued, the concept of task-specific practice implies that without ongoing and progressive practice, movement skills will not be advanced.57 Task-specific practice may occur by deliberate and systematic set-aside sessions, or it may be transparently induced by responding to the demands of everyday activities,58 provided that those activities call for use of the more affected extremity. Because development and retention of movement skills over time require ongoing motor behavior, psychological science pertaining to behavior change or support50,59,60 becomes highly relevant to those seeking to produce lasting effects in their clients. As such, another aspect of skill that will be important for sustaining gains and generalizing movement skills into everyday contexts61 is a set of skills related to self-management of those gains and continued use in the natural environment.
INFUSING CONTEMPORARY MOTOR LEARNING INTO NEUROREHABILITATION PRACTICE
In essence, learning underlies the recovery of function and the development of new skills after catastrophic or profound neurologic and other disabling disorders. Creating the conditions that optimize the processes of motor learning and relearning may have been the implicit intent of some rehabilitation and research programs. However, many lack a strong conceptual framework, have been narrow in focus, and have not included critical features to direct, sustain, and generalize effects into life activities and community participation.
The past decade has witnessed an explosion of different therapeutic interventions for stroke rehabilitation, emergent from new insight about the brain–behavior relationship.13,62 Despite the varied intervention options, a significant percentage of individuals are unable to maintain and generalize the gains achieved in therapy to the natural environment after therapy ends.63–65 Although task-oriented training approaches highlight the importance of repetition and task specificity, they sometimes downplay the achievement of skilled movement in the service of functional tasks. Maladaptive or “bad use” may occur when less optimal, unskilled, solutions—ones that rely on compensatory strategies—are used.66–72 This may contribute to incipient declines after therapy ends and gains are not generalized.
The opportunity, therefore, is to integrate the known benefits of intense, challenging, and progressive task practice programs with those that optimize skill, transfer, generalization, and persistence of gains made in therapy to the natural environment. Recently, we suggested an evidence-based solution—one in which the benefits of progressive, task-oriented training could be integrated with patient-centered strategies to facilitate translation of the therapeutic gains into skilled use in the home and community and in which the patient is empowered to incorporate the paretic limb into valued activities.7,73
ACCELERATED SKILL ACQUISITION PROGRAM
We developed an evidence-based intervention, ASAP, that integrates contemporary principles of motor learning.7,68,74,75 The ASAP is a hybrid combination of task-specific and skill-based/impairment-mitigating training with embedded patient-centered motivational enhancements. Targeted task-specific training (skill) emerges as the single most important approach to intervention for the disabling consequences of stroke in mildly to moderately impaired participants.13,62 The fundamental problems that ASAP addresses are conceived as the learning or relearning of motor skills to optimally affect neural plasticity57 as well as skills to self-direct posttraining activities.76 Development of skill is facilitated by the amelioration of impairments (eg, muscle weakness and low self-efficacy) to enhance capacity.69,77,78 Attention to motor learning, motor control (eg, goal-directed whole tasks with natural synergies),2,79 and basic exercise physiology (eg, overload in terms of training load/intensity and speed) principles are very relevant.80 Social-cognitive psychological theories of motivation are applied in this intervention for immediate and particularly longer-term participant motivation. These assume that intrinsic sources of motivation, including perceptions of self-determination (choice, control, collaboration) and self-efficacy (confidence in one’s capabilities), are key contributors of continued choice, effort, and persistence to use paretic limbs, which in turn leads to mitigation of disability and of self-imposed participation restrictions. A note of historical interest, the ASAP intervention draws upon research from motor learning and several overlapping fields of study, and in fact incorporates principles of even more sub-fields of movement science (eg, exercise physiology). As such, we do not consider the ASAP as a motor learning approach, per se.32
CONCEPTUAL FRAMEWORK: INTEGRATION OF SKILL, CAPACITY, AND MOTIVATION
In this section, we outline the conceptual framework for the ASAP and include a case example. A pathway from impairment reduction, to functional capability, to more general use of restored limbs in natural contexts is often implicit but less frequently operationalized in therapeutic practice. This conceptual model derives from the infusion of motor learning, neuroscience, and behavioral science described earlier,2,41,43,51 with the developing evidence base of neurorehabilitation.13,62 Figure 1 illustrates the conceptual framework that skill (motor learning and self-management), capacity (impairment mitigation), and motivation (intrinsic drive) together form the fundamental components for effective incorporation of impaired extremities into life activities. These 3 essential elements result in a set of 8 nonexclusive principles that inform rehabilitation practice. Activities to increase capacity, skills, and motivation are centered around specific tasks of the participant’s choosing. Here, the task is viewed as an important vehicle for the acquisition of skilled movements, a means to promote capacity building, and as a mechanism to foster the development of motivation for meaningful task engagement in the natural setting.
Figure 1.
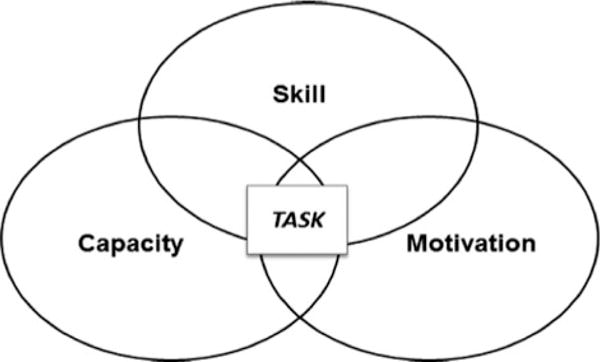
Conceptual framework for the Accelerated Skill Acquisition Program. Activities to increase capacity, skill, and motivation were centered around meaningful tasks of the participant’s choosing.
PRINCIPLES OF ASAP AND CASE EXAMPLE
The principles of the ASAP are provided in Table 1 along with implementation examples. The following case example illustrates the manner in which the principles unfold in one participant’s 30-session therapy intervention. This case involved rehabilitation for a paretic upper extremity after stroke and was part of the Interdisciplinary Comprehensive Arm Rehabilitation Evaluation (ICARE) phase III, randomized controlled trial (www.ClinicalTrials.gov Identifier: NCT00871715).7 ICARE was developed to compare the effectiveness for paretic arm recovery of the investigational intervention, ASAP, with a dose-matched usual care group. It was designed with a relatively high dose of therapy in large part to ensure a reasonable test of the intervention, with the intervention dependent on sufficient practice for skill acquisition and generalizability beyond the clinic setting (ie, 30 1-hour visits distributed over 10 weeks delivered in the outpatient setting).
Table 1.
ASAP Principles and Implementation Examples
| ASAP Principle | Implementation Examples | |
|---|---|---|
| 1. | Ensure challenging and meaningful practice39,80,81 | Demonstrate the challenge threshold (the performance threshold above which movement breaks down and is unsuccessful, and below which the task can be accomplished relatively successfully) Focus on skillful performance of important activity to the participant |
| 2. | Address important (interfering) changeable impairments69,77,78 | Focus on mitigating a particular area of weakness (eg, wrist), pain, or interference with progress |
| 3. | Enhance motor capacity through overload and specificity80,82 | Practice at a clearly intense level Provide task repetitions to physical limits |
| 4. | Preserve natural goal-directedness in movement organization2,81,83 | Perform the natural task, practiced with natural coordination demands |
| 5. | Avoid artificial task breakdowns when possible2,84,85 | When feasible, practice the whole task in its functional entirety Break down the functional task when key to pinpointing or addressing the problem area |
| 6. | Ensure active patient/participant involvement and opportunities for self-direction59,60,76 | Encourage participant activity/response involving problem solving or task construction/determination |
| 7. | Balance immediate and future needs50,60,86 | Participant problem solving (problem identification, solution generation, education, and action plan discussions focused on future, action plan extrapolations of session activities for home practice/recovery); focus is on knowledge and choices for the future |
| 8. | Drive task-specific self-confidence high through performance accomplishments46,51,56,87, | Assess the participant’s task self-efficacy Demonstrate progress through clear measurement (timed performance, counts, repetitions, increased weight, etc.) Celebrate or attend to success |
Abbreviation: ASAP, Accelerated Skill Acquisition Program.
Description of the Participant
Mr H is a 60-year-old right-hand dominant man with hypertension who sustained a right basal ganglia hemorrhagic stroke resulting in left-sided weakness. Medical history reveals a lack of adherence with antihypertensive medication. He received inpatient rehabilitation services for 9 days and was randomized to the ASAP intervention within 24 days after stroke. Mr H reported previously being a house painter but was unemployed and living with his wife and her aging parents. His left upper extremity motor deficits included limitations in shoulder elevation, reach and grasping of objects, grasp-release, and dexterity. His upper extremity motor Fugl-Meyer score at the time of randomization was 43/66.
Introduction to the Case Tables
The following tables illustrate the conceptual framework and clinical application of the ASAP used with Mr H. Training descriptions are grouped chronologically, starting with the first session of orientation to the ASAP (Table 2), then early (Table 3), middle (Table 4), and late (Table 5) therapy sessions. Each table is divided into the following 4 sections: a session description, identification of task performance with examples of dialogue occurring within the hour-long session between the therapist and Mr H, corresponding principles of the ASAP addressed in the session, and finally descriptions of specific elements from the conceptual model that are targeted during training (skill, motivation, capacity) along with specific comments, which highlight aspects of the content of the session. The exchange between Mr H (bolded and italicized) and the therapist (italicized) is a critical component of the task training. The elements/comments section supplies the environmental context and explanation of the dialogue used to support autonomous behavior. A description of each of the 4 table sections with specific content details follows.
Table 2.
Orientation to ASAP Principles
| Session description | Partnership Agreement was signed by T and P. It describes the importance of participation and sharing ideas for challenging task practice, mitt orientation, and outside-of-session action planning |
| Identification of 6 meaningful tasks (2 each from dexterity, bimanual, strength categories) for session practice/performance. Tasks identified: tying shoes, turning pages, opening a water bottle, ironing a shirt, using a weed-eater, using a paint brush | |
| Selection of the priority task: P: “I want to be able to use a paintbrush to paint a wall with my affected hand.” | |
| P rated self-efficacy for priority task performance (1, “not confident at all I can complete the task”). | |
| P attempted performance of the priority task | |
| P/T collaborated on identifying the problem with task performance | |
| Task performance and dialogue | T: “Would you like to give [your priority task] a try with this brush?” |
| [TASK PERFORMANCE: Sitting at a table, the participant was unable to grasp a paintbrush from the table top.] | |
| T: “What do you think is difficult about picking up the brush?” | |
| P: “I can’t open my hand, … unable to raise my shoulder enough, … can’t seem to keep my hand flat on the table.” | |
| [TASK PERFORMANCE: P was still unable to pick up the brush.] | |
| T: “Would a different position be better?” | |
| P: “I could stand.” | |
| T: “What do you think is difficult about picking up the brush in this position?” | |
| P: “I can’t raise my arm.” | |
| T: “What would you like to work on?” | |
| P: “Raising my arm.” | |
| Elements/comments | A skill focus and motivational enhancements (for collaboration and choice) are reflected in therapist/participant dialogue |
| P was limited in manual dexterity and strength for functional grasp of the brush | |
| T and coach determined the challenge threshold (for raising the arm) to enhance motor capacity | |
| P was encouraged to problem solve as the therapist assumed the role of a “coach” | |
| Principles emphasized: 1, 2, 4, and 6 |
Abbreviations: ASAP, Accelerated Skill Acquisition Program; P, participant; T, therapist.
Table 3.
Early Training Visits
| Session description | Assess pre/post vital signs, pain |
| Debriefing of preceding Action Plan (“Find a challenging task involving personal hygiene or grooming, or dressing [self-care]. See how many times you can do it before you can no longer accomplish it to your liking. At the next session, be prepared to report back on the task(s) you chose and how many times you can do it right now.”): | |
| T: “Well, how was your weekend? Tell me what you did?” | |
| P: “I practiced buttoning my shirt and turning pages in my Bible. But I could not button the smaller buttons on my cuff and collar.” | |
| Determination of tasks and sequence of activities for the session’s practice: | |
| T: “That is great that you tried to do the smaller buttons. So what would you like to do today?” | |
| P: “Practice buttoning shirt and turning pages in the Bible.” | |
| P chose an activity sequence for the session: hold paintbrush, button/unbutton shirt for time, turn one page at a time in the Bible until fatigue | |
| P reported self-efficacy for the priority task: 3/10 | |
| Task performance and dialogue | T: “What movement in your shoulder is important in painting a wall?” |
| P: “Being able to hold my arm up while painting with the brush.” | |
| [TASK PERFORMANCE: P demonstrated shoulder flexion with compensatory movements of shoulder hiking and trunk lean.] | |
| T: “So how could we make this difficult?” | |
| P: “See how far I can raise my arm in standing.” | |
| [TASK PERFORMANCE: T gave verbal cues for strategies to reduce compensatory movements. P practiced raising arm to shoulder level, demonstrating proper shoulder stabilization and trunk control. First trial, raised arm successfully 5 times; rested, repeated multiple trials. Increased number of successful attempts in one trial to 10 times.] | |
| T: “How could we make this harder?” | |
| P: “See how long I could hold my arm at shoulder level?” | |
| T: “Yes, that is a really good strategy to increase strength.” | |
| [TASK PERFORMANCE: P raised arm, held at shoulder level for 10 s, rested, repeated movement, and progressed to maximum hold time of 30 s by the 5th trial.] | |
| T: “Is this getting easier? Do you think you are ready to make the task harder?” | |
| P: “Yes, what if I hold something and raise my arm?” | |
| T: “OK, what do you want to hold?” | |
| P: “I think I could lift this 1-lb weight, at least to start out with, and then I could try more weight.” | |
| Elements/comments | P demonstrated elements of skill and motivation for self-direction in response to the Action Plan activities |
| T questions facilitated problem solving without controlling language to support intrinsic motivation | |
| P identified lynchpin impairments of shoulder strength and fine motor control (through buttoning tasks) to improve capacity to paint a wall | |
| P and T celebrated the P’s increased confidence with raising the affected limb. Positive feedback provided to enhance self-efficacy | |
| Principles emphasized: 1–6 and 8 |
Abbreviations: ASAP, Accelerated Skill Acquisition Program; P, participant; T, therapist.
Table 4.
Middle Training Visits
| Session description | Debriefing of preceding Action Plan (“Practice doing each of the three tasks you chose for outside-of-training practice (preparing/eating food, personal hygiene/grooming/dressing, and housework/home maintenance) and assess in what ways you are making progress.”): |
| T: “How did you do with your Action Plan? Did you discover or try any new activities since we last met? Are you noticing any changes with activities you tried earlier?” | |
| P: “I have been ironing daily and noticed that I can maneuver the shirts better and can pump the steam button faster with my thumb. I can now hold large pliers in my weaker hand—I am happy that I did not have to ask my wife to help me! I also worked with the weed eater for around 90 min. I think I only took about 4 breaks that were about 2–3 min. Shoulder was kind of sore the next day though, so I rested my arm.” | |
| Determination of tasks and sequence of activities for the session’s practice: hammering nails in 2×4 board, painting a wall with a brush, refilling mechanical pencil with lead, digging holes for plant with hand shovel, preparing wall for painting by sanding | |
| P: “I think sanding will be a good way to increase strength and endurance in my arm.” | |
| Self-efficacy rating for the priority task: 7/10 | |
| Task performance and dialogue | T: “How long do you think you can sand the wall?” |
| P: “I am not sure, maybe a minute. But after sanding the wall, I want to use the screwdriver to put back the 3 screws in the wall and place back the soap holder.” | |
| [TASK PERFORMANCE: P sanded wall 6 ft high (head level), and suggested timing the activity to provide a measure of accomplishment.] | |
| T: “That is really nice because you are directing the progression of the activity.” | |
| [TASK PERFORMANCE: Over 3 trial attempts, P was able to increase time spent sanding wall without rest. He focused on speed of unscrewing and screwing 3 screws. Improved speed and reduced time to complete task from 3 min 12 sec to 2 min 5 sec over 3 trial attempts.] | |
| P: “Do you have any tape so I can tape around the door frame and molding? However, I think I can use my left hand [weaker hand] to trim the corners and ceiling without using the tape.” | |
| T: “Wow, you can trim without tape?” Unbelievable! How should we set up the challenge for this task?” | |
| P: “Measure the distance I am able to paint the top of the wall without touching the ceiling.” | |
| [TASK PERFORMANCE: P carried a 6-ft ladder to the wall, held the paint can/brush in the affected hand, and climbed the ladder. | |
| P was able to increase accuracy of trim job from 61 inches to 143 inches without touching the ceiling.] | |
| P: “Let’s try to paint the baseboards to make it harder.” | |
| T: “That is great! You just figured out how to increase the intensity of the task.” | |
| [TASK PERFORMANCE: P was able to trim the wall next to baseboard for a distance of 12 inches using the affected arm.] | |
| P: “I think I can do better. I am going to have to come up with a new strategy to paint the baseboards.” | |
| T: “Your painting skills are fantastic, what do you think?” | |
| P: “Pretty good, I may be able to get a job painting. It is an advantage to be able to paint with both hands.” | |
| Elements/comments | Self-direction, problem solving, and intensity of training initiated by the participant; the therapist was supportive of the participant’s choices, building self-efficacy, and support for autonomy |
| P initiated progression of the task and T supported autonomy by getting the paint tape and “going with the flow.” T remained in the background and allowed time for the P to identify, choose, and direct challenges for himself | |
| T was enthusiastic and celebrated the P’s efforts and ideas | |
| P/T celebrated the success of the activity | |
| All principles (1–8) and all elements of ASAP represented in the P/T exchange: intrinsic motivation, capacity building, and skill development |
Abbreviations: ASAP, Accelerated Skill Acquisition Program; P, participant; T, therapist.
Table 5.
Late Training Visits
| Session description | Debriefing of preceding Action Plan (“Test yourself on all the tasks you have chosen for outside-of-training practice over the past weeks since the beginning of your ASAP training and assess your confidence for doing all these tasks under the most demanding of circumstances. Assess your confidence in being able to manage your strengthening, skill development, and community participation needs in the future.”): |
| T: “What do you feel are your accomplishments? Do you think you have improved?” | |
| P: “I am so excited, for the first time I tried to carry 2 full garbage cans to the road and I did it! I helped my father-in-law get dressed, tied his shoes for him. I tried to shoot hoops using the backboard as the external target—was able to shoot and get 3 baskets out of 7 attempts. Moved farther away from the hoop to make it harder. Did yard work, like to paint and do yard work.” | |
| P: “I went bowling with my wife and was able to lift a 6-lb bowling ball and played 2 games. My shoulder was sore so I took a hot shower and did some stretching exercises, feels better.” | |
| Determination of tasks and sequence of activities for the session’s practice: painting wall/baseboards, dribbling basketball, carrying 2 bags of groceries | |
| Self-efficacy rating for the priority task: 10/10 | |
| Task performance and dialogue | T: “What do you want to do today?” |
| P: “Finish the paint job.” | |
| [TASK PERFORMANCE: Finished trimming the baseboards and painting the wall. Cleaned-up workspace. Endurance measured for progress-—40 min recorded for activity task completion, with 1 break for 1.30 min. The participant reports fatigue after painting.] | |
| P: “I know if I can paint with my affected hand, I will be able to work. Being able to paint with my left hand is a real confidence builder.” | |
| T: “You have done a terrific job. Thanks so much for all your hard work.” | |
| P: “I feel better and better, shoulder feels looser.” | |
| Elements/comments | P demonstrated self-management and health protective behavior |
| P directed the session and T supported the autonomous behavior by limiting questions and dialogue with the participant. T was a “coach” during the sessions with the P | |
| Task-oriented training integrated with self-direction, self-regulation, and self-efficacy produced behavioral changes in the P, with indications of transfer to real-world activities | |
| P and T celebrated the accomplishments to drive self-confidence higher | |
| Principles 1–8 incorporated |
Abbreviations: ASAP, Accelerated Skill Acquisition Program; P, participant; T, therapist.
Table Section 1: Session Description
Several key components are demonstrated within the session descriptions that support the application of ASAP principles: determining the point at which the functional movement breaks down (challenge threshold), identifying the functional impairments that interfere with efficient movement, establishing the level of intensity of task practice during the session, and considering activity and task progressions. A typical session included a debriefing of the Action Plan, whereby the participant discussed his or her discoveries made while attempting functional activities in the home and community environment followed by opportunities for the participant to become in volved in the planning of the order of tasks to be practiced during that session.
Table Section 2: Task Performance and Dialogue
A Socratic-like approach, wherein the therapist asked Mr H guiding questions about his performance and explored challenges, was effective in eliciting his active participation in problem solving and learning how to increase the intensity of the chosen tasks for the session. More importantly, the collaborative communication shifts the balance of power from the therapist to Mr H by offering choice, respect, and recognition of the participant’s opinion. The reader may refer to this category in Table 2 to see the flow of the conversation in relationship to task practice and the intent behind the therapist’s questions.
Table Section 3: Elements and Comments
This category describes the integration of information from the previously described headings to facilitate an understanding of the relationship of discussion with the participant and adhering to the principles of the study to promote behavioral changes and motor learning. Numbered principles emphasized in these sessions are selected from the 8 principles in Table 1.
Table 2: Orientation Session
In the orientation session, Mr H received an introduction to the ASAP where the concepts of collaboration, problem solving, and challenging task practice were defined in a written document called the Partnership Agreement and subsequently signed by the therapist and Mr H. A mitt that may be worn on the less-affected hand was issued to him along with written safety precautions on using the mitt outside of training practice. Of note, Mr H wore the mitt only briefly outside of his therapy sessions. Mr H practiced putting the mitt on and off to ensure there would be no difficulties encountered in the home environment. Next, he identified 2 meaningful and challenging tasks to accomplish in the dexterity, bimanual, and strengthening categories for a total of 6 tasks. The priority task was selected from one of the 6 tasks to measure progress over many sessions. A Likert scale quantified self-efficacy for the priority task, where a 1 represents “not confident at all” and a 10 is “very confident.” An initial measurement of self-efficacy for the priority task, “I want to be able to use a paintbrush to paint a wall with my weaker hand” produced a score of “1.” Mr H and his therapist engaged in self-reflection and developed mutual respect to create the paradigm shift from a prescriptive approach toward treatment to a more collabo rative approach. Therefore, the mission for the therapist was to build a therapeutic relationship by not only providing the treatment environment to promote behavioral changes but also supporting the emotional and social adjustments that occur after experiencing a life-changing event.
Table 3: Early Session
After the orientation session, each subsequent visit started with a debriefing of the previous session’s Action Plan. The therapist identified and supported Mr H’s attempt at a challenging task (buttoning small buttons) and working at his challenge threshold—“that is great that you tried to do the smaller buttons.” Session activities emerged from the home practice of the previous night with direction from Mr H as to what he wanted to address that day. By asking Mr H to identify his capacity limitations (“What movement in your shoulder is important in painting the wall?”), she facilitated his problem solving and led the discussion in such a way to allow him to identify and choose how he would like to address the important (interfering) and changeable impairment (Principle 2). Questions such as “How could we make it harder?” allowed Mr H to direct himself as to how the task could be modified to work at his challenge threshold, enhancing his motor capacity through overload and specificity (Principle 3). Simply asking Mr H “Do you think you are ready to make the task harder?” actively engaged his involvement and supported his self-direction of the therapy period (Principle 6). Action Plans to facilitate continued practice outside of the session were purposely phrased to support self-direction and assessment. Mr H was asked to choose the activity—“Find a challenging task involving (specified area) to practice”—which helps to ensure challenging and meaningful practice (Principle 1). Instead of the therapist prescribing the number of repetitions of a task (eg, 2 sets of 10 repetitions 3 times per day), the duration of the practice is to be directed by Mr H (“How many times can you do it before no longer accomplishing it to your liking?”).
Table 4: Middle Session
In this example of a typical middle period training session, the therapist’s question “Are you noticing any changes with activities you tried earlier?” allowed her to evaluate how Mr H was improving in the self-assessment of his skills and capacity (“I can maneuver the shirts better and can pump the [iron’s] steam button faster”). Without prompting, Mr H stated: “I think sanding will be a good way to increase strength in my arm,” more evidence suggesting he was improving in his ability to self-assess and self-direct his own activities. The therapist reflects back to Mr H when he makes choices that support a specific principle: “That’s great! You just figured out how to increase the intensity of the task.” She supported self-efficacy by being enthusiastic about his accomplishments (“Your painting skills are fantastic!),” but also made sure she asked for his perspective (“What do you think?”).
Table 5: Late Session
These final sessions illustrated Mr H’s perspective on the improvements he made functionally, with his self-efficacy (“Being able to paint with my left hand is a real confidence builder”), his skills in identifying his skills/capacity (“… was able to make 3 out of 7 attempts of shooting hoops”), and self-management (“I went bowling with my wife … my shoulder was sore, so I took a hot shower and did some stretching exercises”). He was also able to resume his role as a caregiver for his father-in-law and expressed his confidence in returning to work. The therapist reduced her guiding questions/dialogue, supporting Mr H’s autonomous behavior. Action Plans shifted toward Mr H identifying ways he would continue to manage his strengthening, skill development, and community participation after therapy ended.
SUMMARY AND DISCUSSION
This perspective with a contemporary case example traces the evolution in neurorehabilitation practice that accompanied changes in scientific foundations, beginning with behavioral perspectives on motor learning, first introduced to physical therapy and highlighted over several decades by the STEP Conferences. The revolution in neuroscience then provided the first evidence for experience- and learning-dependent cortical reorganization and the importance of skill acquisition for restorative therapies after stroke. Today, social-cognitive interventions and behavior change perspectives influence the extent to which motor learning can be optimized in the near and longer term. We developed the ASAP, principle-based intervention for neurorehabilitation, which emphasizes integration from a broad set of scientific lines of inquiry, including the contemporary fields of motor learning, neuroscience, and the psychological science of behavior change, and includes 3 overlapping essential elements including skill, capacity, and motivation. Further refinement and testing of the ASAP, and in varying populations and permutations, in well-conceived and sound clinical research is encouraged.88,89
The ICARE trial is currently underway at this writing. It is our expectation that the ASAP principles would apply across a diverse spectrum of disabling conditions to rehabilitation interventions for a number of different clinical populations and are not unique to the case example of upper-extremity function in neurological conditions. Compared with most protocol-driven approaches, the principle-based approach of the ASAP was undertaken to provide for a more flexible and customizable intervention including innovative technologies for participants of varying clinical needs, severity levels, and personal preferences for therapeutic goals. The identification of multiple principles guiding dynamic clinical decisions means that in any given moment, some principles will be emphasized whereas others may be downplayed. However, it is usually the case that therapeutic actions can satisfy one or more principles without contradicting others. It is expected that all of the principles will be supported over the course of a therapy session and especially over a multisession episode of care. The ability to take advantage of frequently occurring “teachable moments” is one strength of a principle-driven approach. Conversely, this abstraction and flexibility can be challenging for inexperienced clinicians but exciting to those seeking new challenges in their practice and high-quality interactions with their clients.
Supplementary Material
Footnotes
Video Abstract available (See Video, Supplemental Digital Content 1, http://links.lww.com/JNPT/A71) for more insights from the authors.
Supplemental digital content is available for this article. Direct URL citation appears in the printed text and is provided in the HTML and PDF versions of this article on the journal’s Web site (www.jnpt.org).
The authors declare no conflict of interest.
The authors and our colleagues who received our entry-level education in physical therapy in the late 1960s and early 1970s used the NUSTEP Proceedings as a textbook for therapeutic exercise and patient management. An informal survey suggested that many of the articles, including the three commented on here pertaining to motor learning, simply were not assigned as required course readings. By implication, this suggests that content pertaining to motor learning was not thought to be particularly relevant for the development of therapeutic exercise programs. In hindsight, this was unfortunate and likely stalled research progress in this area.
References
- 1.Tolman EC. Purposive Behavior in Animals and Man. NY: Century; 1932. [Google Scholar]
- 2.Schmidt RA, Lee TD. Motor Control and Learning: A Behavioral Emphasis. 5th. Champaign, IL: Human Kinetics; 2011. [Google Scholar]
- 3.Schmidt RA, Bjork R. New conceptualizations of practice: common principles in three paradigms suggest new concepts for training. Psychol Sci. 1992;3(4):207–217. [Google Scholar]
- 4.Russell D, Newell K. On No-KR tests in motor learning, retention and transfer. Hum Movement Sci. 2007;26(1):155–173. doi: 10.1016/j.humov.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 5.Kantak SS, Winstein CJ. Learning-performance distinction and memory processes for motor skills: a focused review and perspective. Behav Brain Res. 2012;228(1):219–231. doi: 10.1016/j.bbr.2011.11.028. [DOI] [PubMed] [Google Scholar]
- 6.Winstein CJ, Pohl PS, Lewthwaite R. Effects of physical guidance and knowledge of results on motor learning: support for the guidance hypothesis. Res Q Exerc Sport. 1994;65(4):316–323. doi: 10.1080/02701367.1994.10607635. [DOI] [PubMed] [Google Scholar]
- 7.Winstein CJ, Wolf SL, Dromerick AW, et al. Interdisciplinary Comprehensive Arm Rehabilitation Evaluation (ICARE): a randomized controlled trial protocol. BMC Neurol. 2013;13:5. doi: 10.1186/1471-2377-13-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Franz S, Scheetz ME, Wilson AA. The possibility of recovery of motor function in long-standing hemiplegia. JAMA. 1915;65:2150–2154. [Google Scholar]
- 9.Northwestern University (Evanston IMS) An Exploratory and Analytical Survey of Therapeutic Exercise; Proceedings Northwestern University Special Therapeutic Exercise Project, NUSTEP, July 25, 1966 to August 19, 1966, Northwestern University Medical School, Chicago, Ill. Vol. 46. Baltimore, MD: Williams & Wilkins, Co; 1967. [Google Scholar]
- 10.Cross KD. Role of practice in perceptual-motor learning. Am J Phys Med. 1967;46(1):487–510. [PubMed] [Google Scholar]
- 11.Fischer E. Factors affecting motor learning. Am J Phys Med. 1967;46(1):511–519. [PubMed] [Google Scholar]
- 12.Mathis BC. Motivation and emotion in learning. Am J Phys Med. 1967;46(1):468–479. [PubMed] [Google Scholar]
- 13.Winstein C, Wolf S. Task-oriented training to promote upper extremity recovery. In: Stein J, Harvey R, Macko R, Winstein C, Zorowitz R, editors. Stroke Recovery and Rehabilitation. NY: Demos Medical; 2008. pp. 267–290. [Google Scholar]
- 14.Schmidt RA. Motor schema theory after 27 years: reflections and implications for a new theory. Res Q Exerc Sport. 2003;74(4):366–375. doi: 10.1080/02701367.2003.10609106. [DOI] [PubMed] [Google Scholar]
- 15.Willingham DB. A neuropsychological theory of motor skill learning. Psychol Rev. 1998;105(3):558–584. doi: 10.1037/0033-295x.105.3.558. [DOI] [PubMed] [Google Scholar]
- 16.Karni A, Meyer G, Jezzard P, Adams MM, Turner R, Ungerleider LG. Functional MRI evidence for adult motor cortex plasticity during motor skill learning. Nature. 1995;377(6545):155–158. doi: 10.1038/377155a0. [DOI] [PubMed] [Google Scholar]
- 17.Muellbacher W, Ziemann U, Wissel J, et al. Early consolidation in human primary motor cortex. Nature. 2002;415(6872):640–644. doi: 10.1038/nature712. [DOI] [PubMed] [Google Scholar]
- 18.Kantak SS, Sullivan KJ, Fisher BE, Knowlton BJ, Winstein CJ. Neural substrates of motor memory consolidation depend on practice structure. Nat Neurosci. 2010;13:923–925. doi: 10.1038/nn.2596. [DOI] [PubMed] [Google Scholar]
- 19.Stefan K. Formation of a motor memory by action observation. J Neurosci. 2005;25(41):9339–9346. doi: 10.1523/JNEUROSCI.2282-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carr JH, Shepherd RB. Movement Science: Foundations for Physical Therapy in Rehabilitation. Aspen Publishers; 1987. [Google Scholar]
- 21.Winstein C, Knecht HG. Movement science and its relevance to physical therapy. Phys Ther. 1990;70(12):759–762. doi: 10.1093/ptj/70.12.759. [DOI] [PubMed] [Google Scholar]
- 22.Schmidt RA. Motor learning principles for physical therapy. In: Lister M, editor. Contemporary Management of Motor Control Problems: Proceedings of the II Step Conference. Alexandria, VA: Foundation for Physical Therapy; 1991. pp. 49–63. [Google Scholar]
- 23.Merzenich DM. Soft-Wired: How the New Science of Brain Plasticity Can Change Your Life. San Francisco, CA: Parnassus Publishing, LLC; 2013. [Google Scholar]
- 24.McEwen IR. “STEPS” in practice. Phys Ther. 2004;84(7):606–607. [PubMed] [Google Scholar]
- 25.Gill-Body K, Deutsch JE. Editor’s note: Integrating IIISTEP into practice, education and research. J Neurol Phys Ther. 2006;30(3):97–98. [Google Scholar]
- 26.Kleim JA. III STEP: a basic scientist perspective. Phys Ther. 2006;86(5):614–617. [PubMed] [Google Scholar]
- 27.Callahan J, Parlman K, Beninato M, Townsend E. Perspective: Impact of the IIISTEP conference on clinical practice. J Neurol Phys Ther. 2006;30(3):157–166. doi: 10.1097/01.npt.0000281953.71064.44. [DOI] [PubMed] [Google Scholar]
- 28.Winstein CJ, Merians AS, Sullivan KJ. Motor learning after unilateral brain damage. Neuropsychologia. 1999;37:975–987. doi: 10.1016/s0028-3932(98)00145-6. [DOI] [PubMed] [Google Scholar]
- 29.Lin C, Sullivan K, Wu A, Kantak SS, Winstein C. Effect of task practice order on motor skill learning in adults with Parkinson’s disease: a pilot study. Phys Ther. 2007;87(9):1120–1131. doi: 10.2522/ptj.20060228. [DOI] [PubMed] [Google Scholar]
- 30.Boyd LA, Winstein CJ. Impact of explicit information on implicit motor-sequence learning following middle cerebral artery stroke. Phys Ther. 2003;83(11):976–989. [PubMed] [Google Scholar]
- 31.Boyd LA, Winstein CJ. Providing explicit information disrupts implicit motor learning after basal ganglia stroke. Learn Mem. 2004;11(4):388–396. doi: 10.1101/lm.80104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chan DY, Chan CC, Au DK. Motor relearning programme for stroke patients: a randomized controlled trial. Clin Rehabil. 2006;20(3):191–200. doi: 10.1191/0269215506cr930oa. [DOI] [PubMed] [Google Scholar]
- 33.Ezekiel HJ, Lehto NK, Marley TL, Wishart LR, Lee TD. Application of motor learning principles: the physiotherapy client as a problem-solver. III: Augmented feedback. Physiother Can. 2001;53(1):33–39. [Google Scholar]
- 34.Wishart LR, Lee TD, Ezekiel HJ, Marley TL, Lehto NK. Application of motor learning principles: the physiotherapy client as a problem-solver. 1. Concepts. Physiother Can. 2000;52(3):229–232. [Google Scholar]
- 35.Kitago T, Krakauer JW. Motor learning principles for neurorehabilitation. In: Barnes MP, Good DC, editors. Handbook of Clinical Neurology. Vol. 110. Elsevier B.V.; [DOI] [PubMed] [Google Scholar]
- 36.Lang CE, MacDonald JR, Reisman DS, et al. Observation of amounts of movement practice provided during stroke rehabilitation. Arch Phys Med Rehabil. 2009;90(10):1692–1698. doi: 10.1016/j.apmr.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hanlon RE. Motor learning following unilateral stroke. Arch Phys Med Rehabil. 1996;77:811–815. doi: 10.1016/s0003-9993(96)90262-2. [DOI] [PubMed] [Google Scholar]
- 38.Nudo RJ, Wise BM, SiFuentes F, Milliken GW. Neural substrates for the effects of rehabilitative training on motor recovery after ischemic infarct. Science. 1996;272(5269):1791–1794. doi: 10.1126/science.272.5269.1791. [DOI] [PubMed] [Google Scholar]
- 39.Plautz EJ, Milliken GW, Nudo RJ. Effects of repetitive motor training on movement representations in adult squirrel monkeys: role of use versus learning. Neurobiol Learn Mem. 2000;74(1):27–55. doi: 10.1006/nlme.1999.3934. [DOI] [PubMed] [Google Scholar]
- 40.Karni A, Meyer G, Jezzard P, Adams MM, Turner R, Ungerleider LG. Functional MRI evidence for adult motor cortex plasticity during motor skill learning. Nature. 1995;377(14):155–158. doi: 10.1038/377155a0. [DOI] [PubMed] [Google Scholar]
- 41.Askim T, Indredavik B, Vangberg T, Haberg A. Motor network changes associated with successful motor skill relearning after acute ischemic stroke: a longitudinal functional magnetic resonance imaging study. Neurorehabil Neural Repair. 2009;23(3):295–304. doi: 10.1177/1545968308322840. [DOI] [PubMed] [Google Scholar]
- 42.Nudo RJ. Functional and structural plasticity in motor cortex: implications for stroke recovery. Phys Med Rehabil Clin N Am. 2003 Feb;14(1 Suppl):S57–S76. doi: 10.1016/s1047-9651(02)00054-2. [DOI] [PubMed] [Google Scholar]
- 43.Dancause N, Nudo RJ. Shaping plasticity to enhance recovery after injury. Prog Brain Res. 2011;192:273–295. doi: 10.1016/B978-0-444-53355-5.00015-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tennant KA, Adkins DL, Scalco MD, et al. Skill learning induced plasticity of motor cortical representations is time and age-dependent. Neurobiol Learn Mem. 2012;98:291–302. doi: 10.1016/j.nlm.2012.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kleim JA. Neural Plasticity: Foundations for Neurorehabilitation. TANAS Publishing; 2012. [Google Scholar]
- 46.Lewthwaite R, Wulf G. Motor learning through a motivational lens. In: Hodges NJ, Williams AM, editors. Skill Acquisition in Sport. 2nd. Routledge; 2012. [Google Scholar]
- 47.Goh H-T, Sullivan KJ, Gordon J, Wulf G, Winstein C. Dual-task practice enhances motor learning: a preliminary investigation. Exp Brain Res. 2012;222(3):201–210. doi: 10.1007/s00221-012-3206-5. [DOI] [PubMed] [Google Scholar]
- 48.Knowlton BJ, Mangels JA, Squire LR. A neostriatal habit learning system in humans. Science. 1996;273(5280):1399–1402. doi: 10.1126/science.273.5280.1399. [DOI] [PubMed] [Google Scholar]
- 49.Reber PJ, Squire LR. Encapsulation of implicit and explicit memory in sequence learning. J Cogn Neurosci. 1998;10(2):248–263. doi: 10.1162/089892998562681. [DOI] [PubMed] [Google Scholar]
- 50.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 51.Bandura A. Self-Efficacy: The Exercise of Control. NY: Freeman; 1997. [Google Scholar]
- 52.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55(1):68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- 53.Deci EL, Ryan RM. The “what” and “why” of goal pursuits: human needs and the self-determination of behavior. Psychological Inquiry. 2000;11:227–268. [Google Scholar]
- 54.Wulf G, Chiviacowsky S, Lewthwaite R. Altering mindset can enhance motor learning in older adults. Psychol Aging. 2012;27(1):14–21. doi: 10.1037/a0025718. [DOI] [PubMed] [Google Scholar]
- 55.Chiviacowsky S, Wulf G, Lewthwaite R, Campos T. Motor learning benefits of self-controlled practice in persons with Parkinson’s disease. Gait Posture. 2012;35(4):601–605. doi: 10.1016/j.gaitpost.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 56.Dobkin BH, Plummer-D’Amato P, Elashoff R, Lee J. International randomized clinical trial: Stroke inpatient rehabilitation with reinforcement of walking speed (SIRROWS), improves outcomes. Neurorehab Neural Repair. 2010;24(3):235–242. doi: 10.1177/1545968309357558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kleim JA, Markham JA, Vijj K, Freese JL, Ballard DH, Greenough WT. Motor learning induces astrycytic hypertrophy in the cerebellar cortex. Behav Brain Res. 2007;178:244–249. doi: 10.1016/j.bbr.2006.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Schweighofer N, Han CE, Wolf SL, Arbib MA, Winstein CJ. A functional threshold for long-term use of hand and arm function can be determined: predictions from a computational model and supporting data from the Extremity Constraint-Induced Therapy Evaluation (EXCITE) trial. Phys Ther. 2009;89(12):1327–1336. doi: 10.2522/ptj.20080402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Williams GC, McGregor HA, Zeldman A, Freedman ZR, Deci EL. Testing a self-determination theory process model for promoting glycemic control through diabetes self-management. Health Psychol. 2004;23(1):58–66. doi: 10.1037/0278-6133.23.1.58. [DOI] [PubMed] [Google Scholar]
- 60.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002;288(19):2469–2475. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 61.Hellstrom K, Lindmark B, Wahlberg B, Fugl-Meyer AR. Self-efficacy in relation to impairments and activities of daily living disability in elderly patients with stroke: a prospective investigation. J Rehabil Med. 2003;35(5):202–207. doi: 10.1080/16501970310000836. [DOI] [PubMed] [Google Scholar]
- 62.Timmermans AA, Spooren AI, Kingma H, Seelen HA. Influence of task-oriented training content on skilled arm-hand performance in stroke: a systematic review. Neurorehabil Neural Repair. 2010;24(9):858–870. doi: 10.1177/1545968310368963. [DOI] [PubMed] [Google Scholar]
- 63.Takebayashi T, Koyama T, Amano S, et al. A 6-month follow-up after constraint-induced movement therapy with and without transfer package for patients with hemiparesis after stroke: a pilot quasi-randomized controlled trial. Clin Rehabil. 2013;27(5):418–426. doi: 10.1177/0269215512460779. [DOI] [PubMed] [Google Scholar]
- 64.Hidaka Y, Han C, Wolf S, Winstein C, Schweighofer N. Use it and improve it or lose it: interactions between arm function and use in humans post-stroke. PLoS Comput Biol. 2012;8(2):e1002343. doi: 10.1371/journal.pcbi.1002343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Patterson KK, Gage WH, Brooks D, Black SE, McIlroy WE. Changes in gait symmetry and velocity after stroke: a cross-sectional study from weeks to years after stroke. Neurorehabil Neural Repair. 2010;24(9):783–790. doi: 10.1177/1545968310372091. [DOI] [PubMed] [Google Scholar]
- 66.Michielsen ME, Selles RW, Stam HJ, Ribbers GM, Bussmann JB. Quantifying nonuse in chronic stroke patients: a study into paretic, nonparetic, and bimanual upper-limb use in daily life. Arch Phys Med Rehabil. 2012;93(11):1975–1981. doi: 10.1016/j.apmr.2012.03.016. [DOI] [PubMed] [Google Scholar]
- 67.Shaikh T, Goussev V, Feldman AG, Levin MF. Arm-trunk coordination for beyond-the-reach movements in adults with stroke. Neurorehabil Neural Repair. 2013 doi: 10.1177/1545968313510973. [DOI] [PubMed] [Google Scholar]
- 68.Lum PS, Mulroy S, Amdur RL, Requejo P, Prilutsky BI, Dromerick AW. Gains in upper extremity function after stroke via recovery or compensation: potential differential effects on amount of real-world limb use. Top Stroke Rehabil. 2009;16(4):237–253. doi: 10.1310/tsr1604-237. [DOI] [PubMed] [Google Scholar]
- 69.Corti M, McGuirk TE, Wu SS, Patten C. Differential effects of power training versus functional task practice on compensation and restoration of arm function after stroke. Neurorehabil Neural Repair. 2012;26(7):842–854. doi: 10.1177/1545968311433426. [DOI] [PubMed] [Google Scholar]
- 70.Tan C, Tretriluxana J, Pitsch E, Runnarong N, Winstein CJ. Anticipatory planning of functional reach-to-grasp: a pilot study. Neurorehabil Neural Repair. 2012;26(8):957–967. doi: 10.1177/1545968312437938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kitago T, Liang J, Huang VS, et al. Improvement after constraint-induced movement therapy: recovery of normal motor control or task-specific compensation? Neurorehabil and Neural Repair. 2012;27(2):99–109. doi: 10.1177/1545968312452631. [DOI] [PubMed] [Google Scholar]
- 72.Levin M, Kleim JA, Wolf S. Point of view: enhancing interdisciplinary perspectives. What do motor recovery and compensation mean in patients following stroke? Nuerorehabil Neural Repair. doi: 10.1177/1545968308328727. [DOI] [PubMed] [Google Scholar]
- 73.Wade E, Winstein CJ. Virtual reality and robotics for stroke rehabilitation: where do we go from here? Top Stroke Rehabil. 2011;18(6):685–700. doi: 10.1310/tsr1806-685. [DOI] [PubMed] [Google Scholar]
- 74.James GA, Lu ZL, VanMeter JW, Sathian K, Hu XP, Butler AJ. Changes in resting state effective connectivity in the motor network following rehabilitation of upper extremity poststroke paresis. Top Stroke Rehabil. 2009;16(4):270–281. doi: 10.1310/tsr1604-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tretriluxana J, Runnarong N, Tretriluxana S, Prayoonwiwat N, Vachalathiti R, Winstein C. Feasibility investigation of the Accelerated Skill Acquisition Program (ASAP): insights into reach-to-grasp coordination of individuals with postacute stroke. Top Stroke Rehabil. 2013;20(2):151–160. doi: 10.1310/tsr2002-151. [DOI] [PubMed] [Google Scholar]
- 76.Sabini RC, Dijkers MP, Raghavan P. Stroke survivors talk while doing: development of a therapeutic framework for continued rehabilitation of hand function post stroke. J Hand Ther. 2013;26(2):124–130. doi: 10.1016/j.jht.2012.08.002. quiz 131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Platz T, van Kaick S, Moller L, Freund S, Winter T, Kim IH. Impairment-oriented training and adaptive motor cortex reorganisation after stroke: a fTMS study. J Neurol. 2005;252(11):1363–1371. doi: 10.1007/s00415-005-0868-y. [DOI] [PubMed] [Google Scholar]
- 78.Thielman GT, Dean CM, Gentile AM. Rehabilitation of reaching after stroke: task-related training versus progressive resistive exercise. Arch Phys Med Rehabil. 2004;85(10):1613–1618. doi: 10.1016/j.apmr.2004.01.028. [DOI] [PubMed] [Google Scholar]
- 79.Wu C, Trombly CA, Lin K, Tickle-Degnen L. A kinematic study of contextual effects on reaching performance in persons with and without stroke: influences of object availability. Arch Phys Med Rehabil. 2000;81(1):95–101. doi: 10.1016/s0003-9993(00)90228-4. [DOI] [PubMed] [Google Scholar]
- 80.Panarese A, Colombo R, Sterpi I, Pisano F, Micera S. Tracking motor improvement at the subtask level during robot-aided neurorehabilitation of stroke patients. Neurorehabil Neural Repair. 2012 doi: 10.1177/1545968311431966. [DOI] [PubMed] [Google Scholar]
- 81.Kleim J, Jones T. Principles of experience-dependent neural plasticity: implications for rehabilitation after brain damage. J Speech Lang Hear Res. 2008;51(1):S225–S239. doi: 10.1044/1092-4388(2008/018). [DOI] [PubMed] [Google Scholar]
- 82.Butefisch C, Hummelsheim H, Denzler P, Mauritz KH. Repetitive training of isolated movements improves the outcome of motor rehabilitation of the centrally paretic hand. J Neurol Sci. 1995;130(1):59–68. doi: 10.1016/0022-510x(95)00003-k. [DOI] [PubMed] [Google Scholar]
- 83.Wulf G, Prinz W. Directing attention to movement effects enhances learning: a review. Psychon Bull Rev. 2001;8(4):648–660. doi: 10.3758/bf03196201. [DOI] [PubMed] [Google Scholar]
- 84.Mane A, Adams JA, Donchin E. Adaptive and part-whole training in the acquisition of a complex perceptual-motor skill. Acta Psychol (Amst) 1989;71:179–196. [Google Scholar]
- 85.Schmidt R, Young DE. Transfer of movement control in motor skill learning. In: Cormier SM, Hagman JD, editors. Transfer of Learning. Orlando, FL: Academic Press Inc; 1987. pp. 47–79. [Google Scholar]
- 86.Lee TD, Wishart LR. Motor learning conundrums (and possible solutions) Quest. 2005;57:67–78. [Google Scholar]
- 87.Holladay CL, Quinones MA. Practice variability and transfer of training: the role of self-efficacy generality. J Appl Psychol. 2003;88(6):1094–1103. doi: 10.1037/0021-9010.88.6.1094. [DOI] [PubMed] [Google Scholar]
- 88.Hart T, Bagiella E. Design and implementation of clinical trials in rehabilitation research. Arch Phys Med Rehabil. 2012;93(8 Suppl):S117–S126. doi: 10.1016/j.apmr.2011.11.039. [DOI] [PubMed] [Google Scholar]
- 89.Dobkin BH. Progressive staging of pilot studies to improve Phase III trials for motor interventions. Neurorehabil Neural Repair. 2009;23(3):197–206. doi: 10.1177/1545968309331863. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


