Abstract
Problem The hospital based musculoskeletal service in northwest Wales was unable to cope with the demand for referrals from general practitioners. Waiting times were long, duplicate referrals to other departments were common, and general practitioners were reluctant to refer patients with common problems because of the perceived lack of service. Many referrals were made to the inappropriate specialty, especially orthopaedics. At least part of this problem was due to a lack of coordination between the four hospital departments providing musculoskeletal services and the emphasis on district general hospital based rather than community provision.
Design Review over 18 months of impact of the targeted early access to musculoskeletal services (TEAMS) programme on accessibility to musculoskeletal services.
Setting Northwest Wales.
Key measures for improvement Number of patients referred and seen with musculoskeletal problems, waiting times, number of duplicate referrals, and surgery conversion rates in orthopaedic clinics.
Strategies for change Establishing with central clinical triage a common pathway for all musculoskeletal referrals so that patients attend the appropriate department. A back pain pathway led by extended scope physiotherapists was developed, and general practitioners with special interests and extended scope physiotherapists were trained to provide services for patients with uncomplicated musculoskeletal problems in the community.
Effects of change Over 18 months the number of referrals more than doubled. Despite this, waiting times for musculoskeletal services fell; this was noticeable for rheumatology and pain management. Duplicate referrals were abolished. Surgery conversion rates did not, however, change. Questionnaires from the clinics showed a high level of patient satisfaction.
Lessons learnt Integration of hospital services that traditionally have worked in isolation can result in greatly improved access to musculoskeletal services. Community based multidisciplinary clinics run by specially trained general practitioners with special interests and extended scope physiotherapists are an effective way of managing patients with uncomplicated musculoskeletal problems and have been well received by patients and general practitioners. The huge unmet burden of need was reflected by the great increase in musculoskeletal referrals. Other approaches are needed to meet this, including better education of general practitioners and methods for identifying and modifying psychosocial risk factors for chronic pain at an early stage.
Background
Musculoskeletal conditions are a major cause of chronic disability in the United Kingdom and one of the commonest reasons for referral to secondary care. In the 1995 health survey for England, 18% of adults reported some form of moderate or severe disability.1 Musculoskeletal disorders accounted for 34% of these and serious disabilities for 40%. In the 1998 Welsh health survey, 25% of respondents stated that they were being treated for “arthritis.”2 This rose to over 60% in those aged over 85 years. Musculoskeletal conditions accounted for nearly 20% of all general practitioner consultations in 1991-2,3 of which around 5% were referred for a specialist opinion. Because different specialties are involved in managing these patients and waiting times are often long, it can be difficult for general practitioners to know to whom to refer a patient. Consequently, patients are often referred to an inappropriate health professional and referred twice or more for the same problem. Lack of access to appropriate services means that factors that predict chronicity in common disorders such as back pain4 cannot be addressed sufficiently early, thus compounding their social and economic impact.
Outline of context
The North West Wales NHS Trust encompasses the counties of Gwynedd and Anglesey and serves a population of 240 000. This area has one of the highest proportions of elderly people (around 7% aged over 75) in the United Kingdom. Four departments (orthopaedics, rheumatology, pain management, and therapy services) provided secondary care services for musculoskeletal problems. In response to the innovations in care programme for orthopaedics instigated by the Welsh Assembly government, a project group was established in November 2001 consisting of representatives from both the trust and the local health board to assess accessibility to the musculoskeletal services, identify shortfalls, and recommend change. The four departments were managed in different directorates and functioned in isolation. Each department had long waiting times, but there was overlap of effort. The emphasis was on a high tech service in the district general hospital provided by specialists rather than by local services using more holistic providers. Many general practitioners perceived the service to be inadequate for conditions such as back pain and saw little point in referring such patients.
Outline of problem
The key objectives for change were to provide a coordinated service for all patients referred with musculoskeletal problems so that specialists saw those with appropriate problems, to minimise duplicate referrals, to reduce waiting times, and to offer more services locally.
Key outcome measures
Access to musculoskeletal services was assessed for waiting times to the four specialist departments in relation to the number of referrals and number of patients seen. We noted the number of duplicate referrals, and we assessed the rate of conversion from orthopaedic clinics to operating lists as a measure of the appropriateness of orthopaedic referrals.
Process of gathering information
Information was gathered from the hospital based information management system (Isoft). Orthopaedic data did not include accident and trauma patients. Patient satisfaction questionnaires were developed but had not been used routinely before change to the service. These considered access to the service and outcome.
Analysis and interpretation
In March 2002, waiting times to all four departments were long (52 weeks for orthopaedics, pain management, and therapy services, and 36 weeks for rheumatology). The surgical conversion rate in orthopaedic clinics was 37%.
Strategy for change
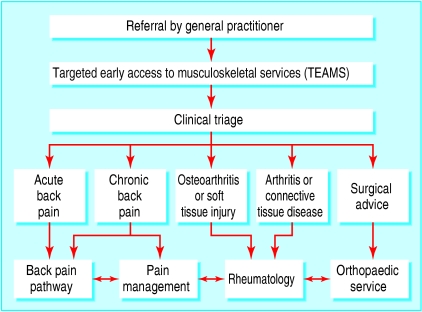
The four departments were integrated by establishing the targeted early access to musculoskeletal services (TEAMS) programme, which incorporated a common pathway for all referrals for musculoskeletal problems combined with a central clinical triage of patients to the appropriate clinical service based on information in a generic referral letter (fig 1). A senior manager was allocated to the services, and a full time coordinator was appointed to oversee the referral process and to set up the service on the patient information management system to code and track patients through the system. New services included a back pain pathway led by extended scope physiotherapists, and three community based musculoskeletal clinics run by general practitioners with special interests5 and extended scope physiotherapists for patients with uncomplicated musculoskeletal problems. Workshops were held for general practitioners throughout the assessment period, providing an opportunity for their input into the process and development of referral guidelines. These and the referral letter proforma were made available on the trust's website.
Fig 1.
Flow diagram showing clinical triage of patients referred to targeted early access to musculoskeletal services
Effects of change
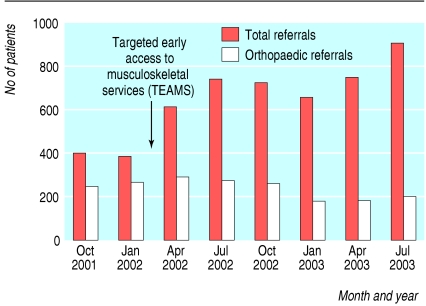
After the introduction of the targeted early access to musculoskeletal services in April 2002, there was a major increase (116%) in the total number of referrals for musculoskeletal problems (fig 2). In contrast, the number of orthopaedic referrals was slightly reduced. Despite the increased numbers of patients seen, waiting times fell. This was particularly noticeable for pain management and rheumatology and patients referred with back pain (fig 3). Excluding hand clinics, where there continued to be a backlog of referrals, waiting times for orthopaedics also fell. This was also reflected in the number of outpatients waiting for an orthopaedic appointment for more than four months, which totalled 823 in August 2002, peaked at 1026 in February 2003, and progressively fell to 607 in September 2003. The surgery conversion rate remained unchanged (37% in both April 2002 and September 2003), but duplicate referrals were all but eliminated. The community musculoskeletal clinics were well received by general practitioners, and the short waiting time of four to six weeks put them in demand. Patients were generally seen on a one-off basis; less than 10% were referred on or followed up. Patient satisfaction questionnaires showed that 88% of patients rated the service as excellent or good, and 75% were completely satisfied with the service provided.
Fig 2.
Effect of targeted early access to musculoskeletal services programme on numbers of musculoskeletal referrals to secondary care services, in total and to orthopaedics
Fig 3.
Waiting times (weeks) for pain management, rheumatology, and orthopaedics (excluding hand referrals) and for patients with back pain since introduction of targeted early access to musculoskeletal services programme
Key learning points
Integration of hospital services can improve access to musculoskeletal services
Multidisciplinary clinics run by general practitioners with special interests and extended scope physiotherapists can effectively manage patients with uncomplicated musculoskeletal problems
In many patients, musculoskeletal pain does not have a specific treatable cause, and in the traditional hospital model there is no service for these people
The targeted early access to musculoskeletal services model applies to any district general hospital, resulting in improved access to musculoskeletal services
Lessons learnt and next steps
Since the introduction of the targeted early access to musculoskeletal services, a large proportion of the increased burden of referrals has fallen on physiotherapy services. It is apparent, however, that many referrals to physiotherapy are inappropriate. We are therefore establishing a programme run by general practitioners with special interests and extended scope physiotherapists to educate general practitioners about the role of physiotherapy in the management of musculoskeletal problems. We are also introducing methods for identifying those patients with non-specific musculoskeletal pain that is unlikely to respond to biological interventions and developing self management interventions based on modifying health beliefs and behaviours. We are also establishing clinical pathways for common hand conditions, such as carpal tunnel syndrome, to help remove the backlog of patients waiting to be seen in the orthopaedic clinics.
Contributors: PJM was the lead writer of this paper; he is guarantor. The other authors are members of the Targeted Early Access to Musculoskeletal Services Project Group and contributed to the design of the programme, its implementation and monitoring, and the preparation of this report.
Funding: Innovations in care programme for orthopaedics, Welsh Assembly government, and North Wales NHS Trust.
Competing interests: None declared.
References
- 1.Joint Health Surveys Unit. Health survey for England 1995. Vol 1: findings. London: Stationery Office, 1997.
- 2.Welsh Office. Better health better Wales: a consultation paper. Cardiff: Welsh Office, 1998.
- 3.McCormick A, Fleming D, Charlton J. Morbidity statistics from general practice. Fourth national study 1991-1992. London: HMSO, 1995.
- 4.Burton AK, Tillotson KM, Main CJ, Hollis S. Psychosocial predictors of outcome in acute and subacute low back trouble. Spine 1995;20: 722-8. [DOI] [PubMed] [Google Scholar]
- 5.Department of Health and Royal College of General Practitioners. Implementing a scheme for general practitioners with special interests. London: DoH, 2002.