Abstract
A 73-year-old man with type 2 diabetes mellitus and end-stage renal disease was diagnosed with acute myocardial infarction. He required continuous dialysis after percutaneous coronary intervention. Subsequently, multiple nodules were discovered in both lungs for the first time, and Cryptococcus neoformans was isolated from the patient's sputum, blood, bilateral pleural fluid, and cerebrospinal fluid cultures, resulting in a diagnosis of disseminated cryptococcosis. This case represents an invaluable example of disseminated cryptococcosis with rapidly growing lung nodules in a dialysis patient, and illustrates that dialysis causes innate immune disorder and the reactivation of cryptococcosis.
Keywords: disseminated cryptococcosis, hemodialysis, multiple lung nodules, bilateral pulmonary effusion
Introduction
Dialysis patients often experience innate and adaptive immune system disorders (1). Infectious diseases are the second-most common cause of death (after cardiovascular disease) in end-stage renal disease (ESRD) patients. Cardiovascular diseases and infections account for 50% and 20%, respectively, of all deaths in ESRD patients (2). Currently, the number of patients that require dialysis as a result of diabetes mellitus is increasing. The control of infectious diseases is very important for their prognosis. In general, cryptococcosis occurs among human immunodeficiency virus (HIV)-infected patients, solid-organ transplant recipients, and patients who undergo exogenous immunosuppression. Exposure to cryptococcus does not usually lead to overt disease, but inhaled cryptococcus can survive in the alveolar macrophages or granulomas. The activation of cryptococcus in these locations is associated with the host immune status (3). However, disseminated cryptococcosis has also been reported in a few dialysis patients (4-6). We herein report a rare case of disseminated cryptococcosis with rapidly growing lung nodules in an ESRD patient who received dialysis following percutaneous coronary intervention (PCI). This case suggests that dialysis can cause innate immune disorder and the reactivation of cryptococcosis.
Case Report
A 73-year-old man who had been diagnosed with type 2 diabetes mellitus at 35 year of age, who had severe diabetic neuropathy and diabetic-ESRD complained of respiratory distress and sudden chest pain. On the first day of treatment, he visited the emergency room. A physical examination revealed that his body temperature was 35.4°C, his heart rate was 90 beats/min with a regular rhythm; and his blood pressure was 130/77 mmHg. A physical examination revealed coarse crackles on bilateral lung auscultation. The laboratory data showed a WBC count of 8,800/μL with a shift to the left (neutrophils 82%), Hb 10.2 g/dL, blood urea nitrogen (BUN) 82.2 mg/dL, creatinine (Cre) 6.50 mg/dL, HbA1c 5.9%, creatine kinase (CK) 189 IU/L, C-reactive protein (CRP) 8.51 mg/dL, brain-type natriuretic peptide (BNP) 127.4 pg/mL. A chest radiograph revealed perihilar consolidations and air bronchograms (Fig. 1). An electrocardiogram revealed ST-segment elevation and poor R-wave progression in leads V1-V3, and echocardiography revealed apical and ventricular asynergy. The patient was therefore diagnosed with acute myocardial infarction and congestive heart failure. Coronary angiography was performed, revealing severe angiostenosis in the septal branch. PCI was therefore performed. The patient required continuous maintenance dialysis. On the following day, the patient went into cardiorespiratory arrest and cardiopulmonary resuscitation was performed, followed by mechanical ventilation.
Figure 1.

Perihilar consolidation and air bronchograms.
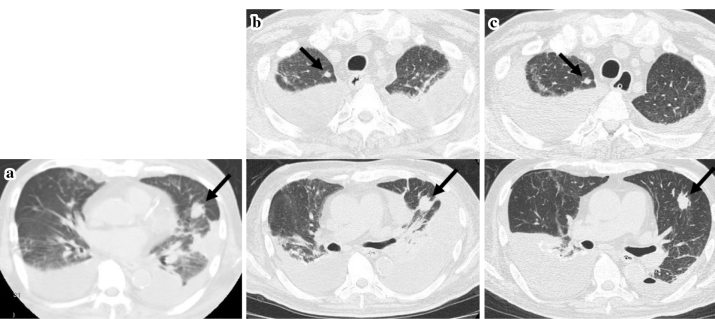
On day 8, ventilator assistance was discontinued. However, the patient produced an increasing volume of sputum, which began to appear purulent. Pseudomonas aeruginosa was identified from a sputum culture, and tazobactam/piperacillin (TAZ/PIPC) (4.5g q12h) was administered. Despite this therapy, the patient's respiratory condition worsened and a chest computed tomography (CT) scan on day 15 revealed bilateral perihilar opacities, pleural effusion, and atelectasis. (Fig. 2). We suspected the development of complications such as microbial substitution, pneumomycosis and thus performed sputum culturing and serum fungal antigen tests. The administration of TAZ/PIPC was changed to meropenem (0.5 g/day). On day 16, the patient's serum tested positive for Cryptococcus antigen. On day 21, cryptococcal bodies were identified in two sets of blood cultures and liposomal amphotericin B (L-AMB) (3 mg/kg/day) was administered. On day 23, cryptococcal bodies were identified in the sputum, cerebrospinal fluid, and bilateral pleural effusion (Fig. 3). The patient was therefore diagnosed with disseminated cryptococcosis. On day 25, brain CT revealed the absence of intracranial hypertension and a brain abscess. The patient was not infected with human immunodeficiency virus (HIV). The administration of L-AMB (3 mg/kg/day) was continued. On day 31, chest CT revealed a solitary nodule in the left lingular segment for the first time, which was suspected to be a pulmonary cryptococcus lesion (Fig. 4a). After several days, all of the sputum, blood, bilateral pleural effusion, and cerebrospinal fluid cultures tested negative. On day 52, chest CT revealed another lung nodule in the right pulmonary apical region. These nodules gradually decreased in size until day 79 (Fig. 4b and c). Although L-AMB was considered effective, the C-reactive protein level remained elevated and the bilateral pleural effusion continuously increased. The patient lost consciousness because of decreased vital capacity with increasing bilateral pleural effusion and was diagnosed with CO2 narcosis. The patient's general condition deteriorated. On day 87, ventricular fibrillation occurred and the patient died. Autopsy was not performed. At a later date, the Cryptococcus isolate was identified and classified as Cryptococcus neoformans var. grubii (serotype A) by a genetic analysis.
Figure 2.
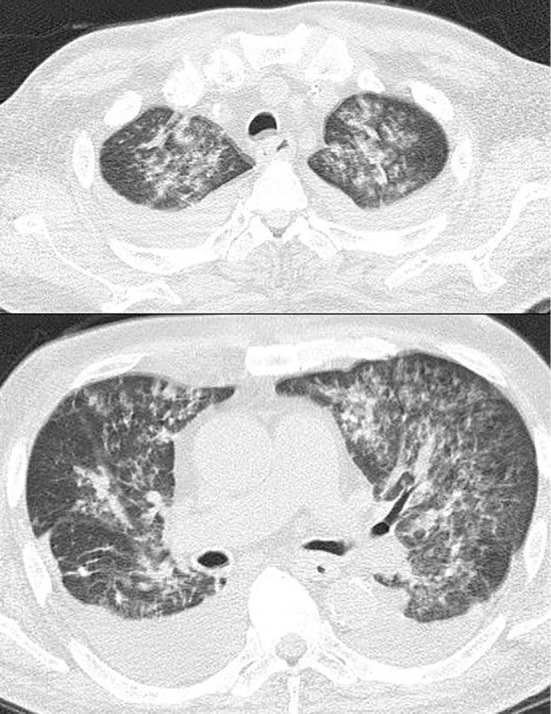
Bilateral perihilar opacities and bilateral pleural effusion.
Figure 3.
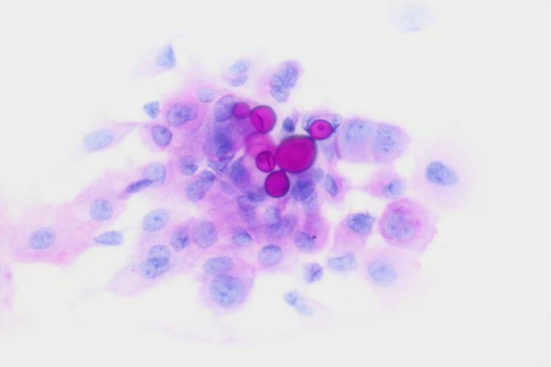
Cryptococcus bodies were identified from the right pleural effusion (PAS).
Figure 4.
A solitary nodule suspected to be a pulmonary cryptococcus lesion in the left lingular segment was revealed by chest computed tomography on day 31. b, c: Another lung nodule in the right pulmonary apical region on day 52. These nodules gradually decreased in size until day 79.
Discussion
Disseminated cryptococcosis is a systemic mycosis that predominantly affects immunocompromised patients. The risk factors for this infection include HIV/acquired immune deficiency syndrome, connective tissue disease, diabetes mellitus, chronic kidney disease, liver cirrhosis, long-term steroid use, exogenous immunosuppression, and solid-organ transplant. C. neoformans and C. gattii are the main causative agents of cryptococcosis. They are commonly associated with pigeon excreta and plant materials. C. neoformans is widespread in the environment, whereas C. gattii is found in many tropical and sub-tropical environments. Almost all cases of cryptococcosis in Japan are caused by C. neoformans (7). Humans likely become infected with Cryptococcus by inhaling fungal basidiospores or encapsulated yeasts. Following inhalation, Cryptococcus localizes to the lungs where it can be phagocytized by the alveolar macrophages. Cryptococcus is surrounded by a polysaccharide capsule that helps the fungus survive in vivo by interfering with phagocytosis. IFN-γ which is secreted from Th1 cells activate macrophages to increase the intracellular killing of Cryptococcus (3). The efficient control of Cryptococcus requires a delicate balance of both Th1- and Th2-type responses (8). More cytokines are needed to control the Th1/Th2 balance and fungal infections, including IL-12, IL-18, IL-13, IL-4, IL-23, IL-17, uPA, IL-10, TGF-β (9). Dialysis and the uremic milieu cause the inability to produce selected cytokines for the immune cells (10).
Usually, the inhalation of Cryptococcus causes focal pneumonitis, and the infection is generally detected as single or multiple pulmonary nodules (11,12). In immunosuppressed patients, focal infection worsens and can cause life-threatening respiratory failure, fungemia, and meningoencephalitis. Disseminated cryptococcosis most frequently infects the lung and central nervous system but can also infect the skin, prostate, and bones. The diagnostic tools that can be used to detect cryptococcosis include histology, fungal cultures, the serum cryptococcal antigen test, and radiography. Disseminated cryptococcosis is defined by either: 1) positive cultures of clinical samples taken from at least two different sites or 2) a positive blood culture (13). Dissemination to extrapulmonary sites is associated with acute respiratory failure and a high rate of mortality (14). In the present case, diabetes mellitus, uremia, hemodialysis, and mechanical ventilation were considered to be risk factors for the dissemination and activation of cryptococcosis, because they are closely related to disorders of both the innate and adaptive immune systems (15-17). Furthermore, the patient lived in a Buddhist temple that had garden with pigeons; thus it was considered that he could have been infected with Cryptococcus before admission. We thought he was not infected with human t-cell leukemia virus type 1 (HTLV-1), because of absence of atypical cells in his peripheral blood, splenohepatomegaly and skin symptoms (18).
Although cases of cryptococcosis have been reported in immunocompetent patients, cryptococcal pleurisy is rare (19,20). In the present case, multiple nodules were detected in both lungs, and cryptococcal bodies were identified in blood and bilateral pulmonary effusion cultures. In the present case, Cryptococcus was therefore thought to have been disseminated through both the airway and the bloodstream.
Induction therapy for disseminated cryptococcosis in non-HIV patients includes amphotericin B, flucytosine, and L-AMB (21). Flucytosine may cause drug-induced anemia; thus, flucytosine was not administered to our patient because of his chronic renal anemia. On day 21, we initiated the administration of L-AMB, which was effective in shrinking the nodules and clearing the patient's cultures. However, on day 31, we found that the pulmonary nodules had grown during treatment. This paradoxical reaction is similar that observed in mycobacterial infection and is considered to be related to a state of relative immunosuppression mediated by a shift in T-helper cell responses to the Th2 phenotype. It can be reversed by antimicrobial therapy (22). There is a previously reported case in which an HIV-seronegative patient with Cryptococcus neoformans meningitis developed a severe inflammatory reaction during treatment (23). To the best of our knowledge, the growth of lung nodules has not previously been reported as a paradoxical reaction. However, we did not find any pathological or bacteriological evidence to suggest that his pulmonary nodules were pulmonary lesions of cryptococcus. This therapy did not entirely ameliorate the patient's inflammation or pulmonary effusion. It is possible that this patient had recurring silent aspiration and pneumonia. It is thought that the patient's ventricular fibrillation, which was caused by cardiac ischemia, was associated with hypovolemia and severe arteriosclerosis.
Disseminated cryptococcosis generally reflects immunosuppression and is rarely found in immunocompetent patients. In dialysis patients, growing pulmonary nodules can suggest disseminated cryptococcosis; thus, appropriate testing and therapy should be immediately initiated.
The authors state that they have no Conflict of Interest (COI).
Acknowledgement
We wish to thank Dr. Atsushi Yoshida from Department of Infection Control and Clinical Laboratory of Medicine, Dokkyo Medical University for performing the genetic analysis which was used to classify and identify Cryptococcus.
References
- 1.Sharif MR, Chitsazian Z, Moosavian M, et al. . Immune disorders in hemodialysis patients. Iran J Kidney Dis 9: 84-96, 2015. [PubMed] [Google Scholar]
- 2.Kato S, Chmielewski M, Honda H, et al. . Aspects of immune dysfunction in end-stage renal disease. Clin J Am Soc Nephrol 3: 1526-1533, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DeLeon-Rodriguez CM, Casadevall A. Cryptococcus neoformans: tripping on acid in the phagolysosome. Front Microbiol 7: 164, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tuon FF, Morales HMP, Penteado-Filho SR, da-Silva MM, de Quadros I, El Hamoui A. Central venous catheter-related bloodstream infection and Cryptococcus neoformans. Braz J Infect Dis 13: 317-318, 2009. [DOI] [PubMed] [Google Scholar]
- 5.Smith JW, Arnold WC. Cryptococcal peritonitis in patients on peritoneal dialysis. Am J Kidney Dis 11: 430-433, 1988. [DOI] [PubMed] [Google Scholar]
- 6.Richard B, Adrian W, Stuart G, Particia B, David W, Campbell M. Disseminated Cryptococcus in a patient receiving chronic haemodialysis. Postgrad Med J 61: 745-747, 1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harris J, Lochhart S, Chiller T. Cryptococcus gatti: where do we go from here? Med Mycol 50: 113-129, 2012. [DOI] [PubMed] [Google Scholar]
- 8.Lindell DM, Ballinger MN, McDonald RA, Toews GB, Huffinagle GB. Diversity of the T-cell response to pulmonary Cryptococcus neoformans infection. Infect Immun 74: 4538-4548, 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coelho C, Bocca AL, Casadevall A. The intracellular life of Cryptococcus neoformans. Annu Rev Pathol 9: 219-238, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mansouri L, Paulsson JM, Moshfegh A, Jacobson SH, Lundahl J. Leukocyte proliferation and immune modulator production in patients with chronic kidney disease. Plos One 8: e73141, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kishi K, Homma S, Kurosaki A, Kohno T, Motoi N, Yoshimura K. Clinical features and high-resolution CT findings of pulmonary cryptococcosis in non-AIDS patients. Respir Med 100: 807-812, 2006. [DOI] [PubMed] [Google Scholar]
- 12.Yu JQ, Tang KJ, Xu BL, Xie CM, Light RW. Pulmonary cryptococcosis in non-AIDS patients. Braz J infect Dis 16: 531-539, 2012. [DOI] [PubMed] [Google Scholar]
- 13.Chuang YM, Ho YC, Chang HT, Yu CJ, Yang PC, Hsueh PR. Disseminated cryptococcosis in HIV-uninfected patients. Eur J Clin Microbiol. Infect Dis 27: 307-310, 2008. [DOI] [PubMed] [Google Scholar]
- 14.Vilchez RA, Linden P, Lacomis J, Costello P, Fung J, Kusne S. Acute respiratory failure associated with pulmonary cryptococcosis in non-aids patients. Chest 119: 1865-1869, 2001. [DOI] [PubMed] [Google Scholar]
- 15.Darras-Joly C, Chevret S, Wolff M, et al. . Cryptococcus neoformans infection in France: epidemiologic features of and ealy prognostic parameters for 76 patients who were infected with human immunodeficiency virus. Clin Infect Dis 23: 369-376, 1996. [DOI] [PubMed] [Google Scholar]
- 16.Kohno S, Kakeya H, Izumikawa K, et al. . Clinical features of pulmonary Cryptococcus in non-HIV patients in Japan. J Infect Chemother 21: 23-30, 2015. [DOI] [PubMed] [Google Scholar]
- 17.Hauser AB, Stinghen AE, Kato S, et al. . Characteristics and causes of immune dysfunction related to uremia and dialysis. Perit Dial Int 28 (Suppl 3): S183-S187, 2008. [PubMed] [Google Scholar]
- 18.Debourgogne A, Iriart X, Blanchet D, et al. . Characteristics and specificities of Cryptococcus infections in French Guiana, 1998-2008. Med Mycol 49: 864-871, 2011. [DOI] [PubMed] [Google Scholar]
- 19.Chechani V, Kamholz SL. Pulmonary manifestations of disseminated cryptococcosis in patients with AIDS. Chest 98: 1060-1066, 1990. [DOI] [PubMed] [Google Scholar]
- 20.Izumikawa K, Zhao Y, Motoshima K, et al. . A case of pulmonary cryptococcosis followed by pleuritic in an apparently immunocompetent patient during fluconazole treatment. Med Mycol 46: 595-599, 2008. [DOI] [PubMed] [Google Scholar]
- 21.Perfect JR, Dismukes WE, Dromer F, et al. . Clinical practice guidelines for the management of cryptococccal disease; 2010 update by the infectious diseases society of America. Clin Infect Dis 50: 291-322, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schluger NW, Rom WN. The host immune response to tuberculosis. Am J Respir Crit Care Med 157(3 Pt 1): 679-691, 1998. [DOI] [PubMed] [Google Scholar]
- 23.Einsiedel L, Goldon DL, Dyer JR. Paradoxical inflammatory reaction during treatment of Cryptococcus neoformans var. gatti meningitis in an HIV-seronegative woman. Clin Infect Dis 39: e78-e82, 2004. [DOI] [PubMed] [Google Scholar]