Abstract
Cervical cancer is a major cause of death in adult women. However, many women do not undergo cervical cancer screening for the following reasons: fear, shame, physical limitations, cultural or religious considerations and lack of access to health care services. Self-collected vaginal smears maybe an alternative means of including more women in cervical cancer screening programs. The objective of this systematic review was to evaluate the acceptability of vaginal smear self-collection for cervical cancer screening. We selected articles from PubMed, the Cochrane Library and Embase that were published between January 1995 and April 2016. Studies written in English, French, Italian, Portuguese or Spanish that involved women between 18 and 69 years of age who had engaged in sexual intercourse were included in this review. The review was performed in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement. Nineteen studies were ultimately evaluated in this review. Most of the included studies (n=17) demonstrated that the self-collection method exhibited outstanding acceptability among women with respect to cervical cancer screening, and only two studies indicated that self-collection exhibited low acceptability among women in this context. The acceptability of self-collection was determined subjectively (without standardized questionnaires) in 10 studies (53%) and via structured and validated questionnaires in the remaining studies. The results of our review suggest that the self-collection method is well-accepted and may therefore encourage greater participation in cervical cancer screening programs. However, additional studies are required to verify these results.
Keywords: Cervical Cancer, Vaginal Smear Self-Collection, Cancer Screening, Method Acceptance, Systematic Review
INTRODUCTION
Screening for cancer of the cervix has intensified in recent decades, enabling the identification of precursor lesions and cancer at earlier disease stages, thereby increasing patient survival. However, many patients still die from this disease 1, which is the most common cancer affecting women after non-melanoma skin cancer, breast cancer and colorectal cancer 1. Cervical cancer is also the fourth-leading cause of malignancy-related death among women in Brazil 2. Therefore, additional means of screening for this disease, which remains a great public health concern, are needed.
The collection of cervix-vaginal cytology samples by health care professionals is generally an effective tool for performing cervical cancer screening. However, many women do not undergo this test for the following reasons: fear, embarrassment, functional or physical limitations, cultural or religious reasons and even lack of access to health services 3,4. In general, women living in rural areas or on the outskirts of large cities have lower education levels and are of lower social and economic statuses than their counterparts in urban areas. Additionally, these women are more likely to have their first sexual intercourse prematurely and often have more sexual partners and more children than other women. Consequently, clinicians have less opportunities to implement preventative health measures among these populations 5.
The vaginal smear self-collection method was created to provide women with access to cervical cancer screening, as patients can perform smear collections themselves and then forward their smears to the appropriate facility for further analysis 5-7. Thus, this method has the potential to increase participation in cervical cancer screening and to facilitate the incorporation of populations living on the outskirts of major centers, including prisoners, into screening programs. However, cultural and psychological factors (fear or fear of self-manipulation) may limit the effectiveness of this method. Our systematic review aimed to assess the acceptability of the self-collection method among women.
METHODS
We conducted a systematic review of studies regarding the acceptability of using the vaginal self-collection method for cervical cancer screening among women. This study was conducted in accordance with the recommendations established by PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 8.
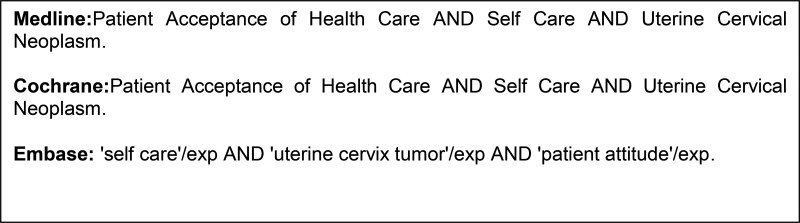
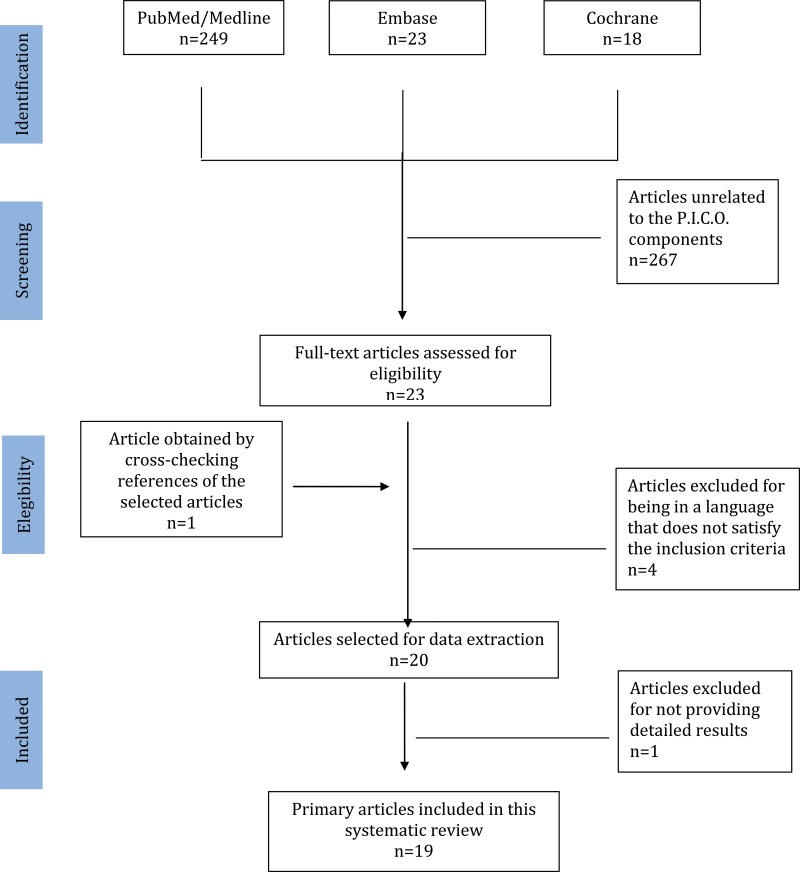
We consulted Medline, the Cochrane Library and Embase to identify relevant studies published from January 1995 (first report) to April 2016. We did not impose any restrictions regarding publication dates. We searched for texts published in English, French, Italian, Spanish and Portuguese. We used search keywords that were in accordance with our selected P.I.C.O. ("patient", "intervention", "control" and "outcome"), and the specific search strategies utilized for electronic databases are summarized in Figure 1. The process of manuscript retrieval is described in Figure 2. Publications listed in the references sections of retrieved articles were also retrieved. Studies involving women over 18 years of age who had engaged in sexual intercourse (P) and submitted to the self-collection of vaginal smears (I) were included in this review. The control group was conventional smears (C). The outcome was the acceptability of the self-collection of vaginal smears for assessing uterine neoplasm in the cervix (O). Retrospective studies or studies for which we did not have access to the full text were excluded. The study selection process and the evaluations of the titles and abstracts obtained through the above searches were conducted in an unbiased manner in strict accordance with the inclusion and exclusion criteria of this study by two researchers (NDSFB and NPCL) skilled in the preparation of systematic reviews. The original articles were subsequently critically evaluated to decide whether they should be included in the review. Meta-analysis was not performed due to variability regarding the methods used for assessing self-collection method acceptability. A third reviewer (JMSJ) was consulted when there was disagreement regarding the selection of studies among the researchers. The information obtained from the selected studies was entered into a table including information regarding the names of the authors, the years of publication, the study designs, the numbers of patients, the ages of the patients, the index test (self-collection) and the reference test (conventional collection).
Databases and search strategies.
The algorithm used for this systematic review.
RESULTS
A total of 290 studies were initially retrieved; 267 of these studies were excluded by applying the aforementioned exclusion criteria. After the references of the selected articles were cross-checked, we included another manuscript. After reading and analyzing articles, we excluded four manuscripts for being in a language that does not satisfy the inclusion criteria. We excluded additional manuscripts because the studies described did not provide detailed results. Thus, 19 manuscripts were ultimately included in this review. The information obtained from the selected studies was entered into a table including information on author names, the publication year, country, study design, the numbers of participants, the ages of the patients, acceptability and the method used (Table 1).
Table 1.
Studies included in the systematic review.
| Authors and publication year | Country | Age (years) | Type | Number of participants | Acceptability | Method used | |
|---|---|---|---|---|---|---|---|
| 1) | Szarewski et al. (9) | United Kingdom | 21 – 65 | Transversal | 28 | Low | Questionnaire |
| 2) | Mitchell et al. (10) | Uganda | 30 – 65 | Transversal | 300 | High | Subjective |
| 3) | Szarewski et al. (11) | United Kingdom | 29 – 65 | Randomized | 3000 | High | Questionnaire |
| 4) | Ortiz et al. (12) | USA | 18 – 34 | Case-control | 100 | High | Questionnaire |
| 5) | Cerigo et al. (13) | Canada | 18 – 69 | Case-control | 93 | High | Subjective |
| 6) | Quincy et al. (14) | Nicaragua | 25 – 60 | Case-control | 250 | High | Subjective |
| 7) | Fielder et al. (15) | USA | 18 – 69 | Randomized | 483 | High | Subjective |
| 8) | Penaranda et al. (16) | Mexico | 30 – 65 | Transversal | 21 | High | Subjective |
| 9) | Sultana et al. (17) | Australia | 30 – 69 | Randomized | 8000 | High | Questionnaire |
| 10) | Vanderpool et al. (18) | USA | 30 – 64 | Transversal | 31 | High | Subjective |
| 11) | Racey et al. (19) | Canada | 30 – 70 | Randomized | 818 | High | Questionnaire |
| 12) | Penaranda et al. (20) | Mexico | 30 – 65 | Transversal | 110 | High | Subjective |
| 13) | Sultana et al. (21) | Australia | 30 – 69 | Transversal | 35 | High | Subjective |
| 14) | Crofts et al. (22) | Cameroon | 30 – 65 | Transversal | 450 | High | Questionnaire |
| 15) | Fargnoli et al. (23) | Switzerland | 24 – 67 | Transversal | 125 | Low | Subjective |
| 16) | Sultana et al. (24) | Australia | 30 – 69 | Transversal | 1521 | High | Questionnaire |
| 17) | Dareng et al. (25) | Nigeria | 18 – 69 | Transversal | 600 | High | Questionnaire |
| 18) | Boggan et al. (26) | Haiti | 25 – 65 | Case-control | 1845 | High | Subjective |
| 19) | Wong et al. (27) | China | 35 – 65 | Randomized | 392 | High | Questionnaire |
A total of 18,202 participants were included in this study 9-27. Only two studies (10.5%) demonstrated that the self-collection method exhibited low acceptability among women 9,23. The acceptability of the self-collection method among women was determined subjectively (without standardized questionnaires) in ten studies (52.6%) 10,13-16,18,20-21,23,26 and via structured and valid questionnaires in the remaining studies. Only five studies were randomized. These results are summarized in Table 1.
The women enrolled in the two studies demonstrating that the self-collection method exhibited low acceptability preferred to continue undergoing screenings performed by health care professionals because they were afraid of not performing the sampling properly or were concerned about experiencing some discomfort during the procedure 9,23. Additionally, some women questioned the validity of self-collected smear results and wondered about the possibility of medical appointments being replaced with self-collection procedures 23. The participants enrolled in these studies, particularly women over 50 years of age, also reported that the explanations regarding how to perform self-collection were confusing and inadequate 9,23.
Among the 17 manuscripts demonstrating that the self-collection method exhibited high acceptability among women, nine performed only subjective evaluations 10,13-16,18,20-21,26, whereas the remaining eight studies used standardized and validated questionnaires.
The following main points were addressed across these questionnaires: 1) the psychosocial aspects of self-collection, such as shame; 2) the feasibility of self-collection, such as perormance reliability; 3) the practicality of self-collection; 4) the desire to perform self-collection again 11-12; 5) characteristics related to life style and reproductive considerations, which were determined using self-administered questionnaires 11,17; 6) the acceptability of self-collection compared with traditional sample collection 17,19,22; 7) the likelihood of recommending self-collection to a family member or friend 24,25-27; 8) the grade of discomfort associated with self-collection, determined using a 5-point Likert scale 27; 9) participants’ knowledge regarding HPV and cervical cancer 11-12; 10) media handling, which was addressed using simple questions, such as "Was the procedure uncomfortable?" or ”Were you embarrassed?" 17,24; and 11) participants’ assessments of the instructions that they were provided 12,22. Thus, the studies were heterogeneous with respect to the information collected by the different types of questionnaires used therein. However, most of the studies indicated that the self-collection method possessed the following advantages over the conventional screening method: easier and faster implementation and lower costs 9-15, 22-25. Prior detailed explanations regarding the method played a fundamental role in the opinions of the participants regarding the method and their acceptance of the method 9,23.
DISCUSSION
Cervical cancer remains a public health challenge 1-5. The results of this review indicate that vaginal smear selfcollection is a well-accepted method that may increase participation in cervical cancer screening 10-22,24-27. However, no standardized questionnaire for evaluating the acceptability of this method exists 10-22,24-27, and better explanations regarding the performance of this method are necessary to improve patient participation in cancer screening 9,23.
Low acceptability of the method among women, which was noted in two studies, was mainly attributed to participant insecurity regarding appropriate sample handling 9,23. The women enrolled in these two studies reported having difficulty understanding the tested approach due to a lack of knowledge regarding their own bodies (their anatomy) 9,23. Participants also expressed concern regarding the possibility that medical appointments could be replaced by vaginal smear self-collection procedures 23. These findings indicate that health education is important with respect to the acceptance of new technologies and treatments 28-29.
The studies demonstrating that the self-collection method exhibited high acceptability among women noted that the ease and rapidity of the self-collection method provide women with greater autonomy with respect to collecting vaginal material, thereby increasing participation in screening programs and complementing the classical methods utilized by health care professionals 21-22,24-27, particularly among populations with difficulty accessing health care facilities, to ultimately facilitate increases in the rate of early cervical cancer diagnosis. The review also noted that the guidelines and explanations pertaining to the performance of the procedure played an important role in increasing patient confidence in and acceptance of the method 9,23. Therefore, the introduction of self-collection should be preceded by community education regarding both the method and the female genitourinary tract.
Several studies used subjective questions regarding the self-collection method, whereas others used complex questionnaires encompassing questions regarding the psychological impact of the self-collection method 9,23, making it difficult to compare the studies, a weakness of this analysis. In addition, the numbers of participants involved in the included studies varied, ranging from <30 participants to >1,000 participants 9-27. Moreover, only five studies included in this review were randomized, indicating that additional randomized studies that feature long follow-up periods and include participants who have received prior education regarding the self-collection method are necessary.
The findings of this systematic review indicate that vaginal smear self-collection is a well-accepted method that may increase participation in cervical cancer screening. However, barriers exist with respect to the use of the self-collection procedure among women who are uncomfortable performing the procedure or uncertain regarding the validity of its results. Thus, additional randomized, prospective and long-term follow-up studies regarding the acceptability of the vaginal smear method are needed.
AUTHOR CONTRIBUTIONS
Braz NS was responsible for the design, revision, analysis and manuscript writing. Lorenzi NP was responsible for the design, revision, analysis and manuscript writing. Sorpreso IC was responsible for the design and revision of the manuscript. Aguiar LM was responsible for the design and revision of the manuscript. Baracat EC was responsible for the design, revision, analysis and manuscript writing. Soares-Júnior JM was responsible for the design, revision, analysis and manuscript writing.
Footnotes
No potential conflict of interest was reported.
REFERENCES
- 1.Tranberg M, Larsen MB, Mikkelsen EM, Svanholm H, Andersen B. Impact of opportunistic testing in a systematic cervical cancer screening program: a nationwide registry study. BMC Public Health. 2015;15:681. doi: 10.1186/s12889-015-2039-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.INCA http://www2.inca.gov.br/wps/wcm/connect/tiposdecancer/site/home/colo_utero/definicao Acesso em 05 de maio de 2016.
- 3.Allgar VL, Neal RD. Delays in the diagnosis of six cancers: analysis of data from the National Survey of NHS Patients: Cancer. Br J Cancer. 2005;92((11)):1959–70. doi: 10.1038/sj.bjc.6602587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Emery JD, Walter FM, Gray V, Sinclair C, Howting D, Bulsara M, et al. Diagnosing cancer in the bush: a mixed-methods study of symptom appraisal and help-seeking behaviour in people with cancer from rural Western Australia. Fam Pract. 2013;30((3)):294–301. doi: 10.1093/fampra/cms087. [DOI] [PubMed] [Google Scholar]
- 5.Broquet C, Triboullier D, Untiet S, Schafer S, Petignat P, Vassilakos P. Acceptability of self-collected vaginal samples for HPV testing in an urban and rural population of Madagascar. Afr Health Sci. 2015;15((3)):755–61. doi: 10.4314/ahs.v15i3.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stanczuk G, Baxter G, Currie H, Lawrence J, Cuschieri K, Wilson A, et al. Clinical validation of hrHPV testing on vaginal and urine self-samples in primary cervical screening (cross-sectional results from the Papillomavirus Dumfries and Galloway-PaVDaG study) BMJ Open. 2016;6((4)):e010660. doi: 10.1136/bmjopen-2015-010660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jun JK, Lim MC, Hwang SH, Shin HY, Hwang NR, Kim YJ, et al. Comparison of DRY and WET vaginal swabs with cervical specimens in Roche Cobas 4800 HPV and Abbott Real Time High Risk HPV tests. J ClinVirol. 2016;79:80–4. doi: 10.1016/j.jcv.2016.04.012. [DOI] [PubMed] [Google Scholar]
- 8.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Szarewski A, Cadman L, Ashdown-Barr L, Waller J. Exploring the acceptability of two self-sampling devices for human papillomavirus testing in the cervical screening context: a qualitative study of Muslim women in London. J Med Screen. 2009;16((4)):193–8. doi: 10.1258/jms.2009.009069. [DOI] [PubMed] [Google Scholar]
- 10.Mitchell S, Ogilvie G, Steinberg M, Sekikubo M, Biryabarema C, Money D. Assessing women’s willingness to collect their own cervical samples for HPV testing as part of the ASPIRE cervical cancer screening project in Uganda. Int J Gynaecol Obstet. 2011;114((2)):111–5. doi: 10.1016/j.ijgo.2011.01.028. [DOI] [PubMed] [Google Scholar]
- 11.Szarewski A, Cadman L, Mesher D, Austin J, Ashdown-Barr L, Edwards R, et al. HPV self-sampling as an alternative strategy in non-attenders for cervical screening - a randomised controlled trial. Br J Cancer. 2011;104((6)):915–20. doi: 10.1038/bjc.2011.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ortiz AP, Alejandro N, Pérez CM, Otero Y, Soto-Salgado M, Palefsky JM, et al. Acceptability of cervical and anal HPV self-sampling in a sample of Hispanic women in Puerto Rico. P R Health Sci J. 2012;31((4)):205–12. [PMC free article] [PubMed] [Google Scholar]
- 13.Cerigo H, Coutlée F, Franco EL, Brassard P. Dry self-sampling versus provider-sampling of cervicovaginal specimens for human papillomavirus detection in the Inuit population of Nunavik, Quebec. J Med Screen. 2012;19((1)):42–8. doi: 10.1258/jms.2012.012011. [DOI] [PubMed] [Google Scholar]
- 14.Quincy BL, Turbow DJ, Dabinett LN. Acceptability of self-collected human papillomavirus specimens as a primary screen for cervical cancer. J Obstet Gynaecol. 2012;32((1)):87–91. doi: 10.3109/01443615.2011.625456. [DOI] [PubMed] [Google Scholar]
- 15.Fielder RL, Carey KB, Carey MP. Acceptability of sexually transmitted infection testing using self-collected vaginal swabs among college women. J Am Coll Health. 2013;61((1)):46–53. doi: 10.1080/07448481.2012.750610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Penaranda E, Molokwu J, Hernandez I, Salaiz R, Nguyen N, Byrd T, et al. Attitudes toward self-sampling for cervical cancer screening among primary care attendees living on the US-Mexico border. South Med J. 2014;107((7)):426–32. doi: 10.14423/SMJ.0000000000000132. [DOI] [PubMed] [Google Scholar]
- 17.Sultana F, English DR, Simpson JA, Brotherton JM, Drennan K, Mullins R, et al. Rationale and design of the iPap trial: a randomized controlled trial of home-based HPV self-sampling for improving participation in cervical screening by never- and under-screened women in Australia. BMC Cancer. 2014;14:207. doi: 10.1186/1471-2407-14-207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vanderpool RC, Jones MG, Stradtman LR, Smith JS, Crosby RA. Self-collecting a cervico-vaginal specimen for cervical cancer screening: an exploratory study of acceptability among medically underserved women in rural Appalachia. Gynecol Oncol. 2014;132((Suppl 1)):S21–5. doi: 10.1016/j.ygyno.2013.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Racey CS, Gesink DC, Burchell AN, Trivers S, Wong T, Rebbapragada A. Randomized Intervention of Self-Collected Sampling for Human Papillomavirus Testing in Under-Screened Rural Women: Uptake of Screening and Acceptability. J Womens Health. 2016;25((5)):489–97. doi: 10.1089/jwh.2015.5348. [DOI] [PubMed] [Google Scholar]
- 20.Penaranda E, Molokwu J, Flores S, Byrd T, Brown L, Shokar N. Women’s Attitudes Toward Cervicovaginal Self-Sampling for High-Risk HPV Infection on the US-Mexico Border. J Low Genit Tract Dis. 2015;19((4)):323–8. doi: 10.1097/LGT.0000000000000134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sultana F, Mullins R, Murphy M, English DR, Simpson JA, Drennan KT, et al. Women’s views on human papillomavirus self-sampling: focus groups to assess acceptability, invitation letters and a test kit in the Australian setting. Sex Health. 2015;12((4)):279–86. doi: 10.1071/SH14236. [DOI] [PubMed] [Google Scholar]
- 22.Crofts V, Flahault E, Tebeu PM, Untiet S, Fosso GK, Boulvain M, et al. Education efforts may contribute to wider acceptance of human papillomavirus self-sampling. Int J WomensHealth. 2015;7:149–54. doi: 10.2147/IJWH.S56307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fargnoli V, Petignat P, Burton-Jeangros C. To what extent will women accept HPV self-sampling for cervical cancer screening? A qualitative study conducted in Switzerland. Int J Womens Health. 2015;7:883–8. doi: 10.2147/IJWH.S90772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sultana F, Mullins R, English DR, Simpson JA, Drennan KT, Heley S, et al. Women’s experience with home-based self-sampling for human papillomavirus testing. BMC Cancer. 2015;15:849. doi: 10.1186/s12885-015-1804-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dareng EO, Jedy-Agba E, Bamisaye P, Isa Modibbo F, Oyeneyin LO, Adewole AS, et al. Influence of Spirituality and Modesty on Acceptance of Self-Sampling forCervical Cancer Screening. PLoS One. 2015;10((11)):e0141679. doi: 10.1371/journal.pone.0141679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Boggan JC, Walmer DK, Henderson G, Chakhtoura N, McCarthy SH, Beauvais HJ, et al. Vaginal Self-Sampling for Human Papillomavirus Infection as a Primary Cervical Cancer Screening Tool in a Haitian Population. Sex Transm Dis. 2015;42((11)):655–9. doi: 10.1097/OLQ.0000000000000345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wong EL, Chan PK, Chor JS, Cheung AW, Huang F, Wong SY. Evaluation of the Impact of Human Papillomavirus DNA Self-sampling on the Uptake of Cervical Cancer Screening. Cancer Nurs. 2016;39((1)):E1–E11. doi: 10.1097/NCC.0000000000000241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sorpreso IC, Vieira LH, Haidar MA, Nunes MG, Baracat EC, Soares JM. Multidisciplinary approach during menopausal transition and postmenopause in Brazilian women. Clin Exp Obstet Gynecol. 2010;37((4)):283–6. [PubMed] [Google Scholar]
- 29.Esposito Sorpreso IC, Laprano Vieira LH, Longoni Calió C, Abi Haidar M, Baracat EC, Soares JM., Jr Health education intervention in early and late postmenopausal Brazilian women. Climacteric. 2012;15((6)):573–80. doi: 10.3109/13697137.2011.635915. [DOI] [PubMed] [Google Scholar]