Introduction
Erosive pustular dermatosis of the scalp (EPDS) is an uncommon condition that is reported after local injuries including burns, cryotherapy, radiation therapy, photodynamic therapy, skin grafts, and hair transplantation as well as topical medication treatments including retinoids, imiquimod, and 5-fluorouracil.1, 2, 3, 4, 5, 6 We present a case of erosive pustular dermatosis of the scalp developing after contact dermatitis induced by a glued-on hair piece. Although skin trauma, including irritant reactions from topical medications, is documented to precipitate this condition, to the best of our knowledge, contact dermatitis from cosmetic application of hair pieces has not previously been reported as a triggering factor.
Case report
A 58-year-old white woman presented with a pruritic eruption on her scalp, which began after having glued-on hair pieces applied by a hair restoration center. She reported her preceding hair loss as diffuse “thinning,” progressing over years, without flaking, burning, or itching. She was not aware of a similar family history. At the hair restoration center, the process of shaving the central portion of her scalp, applying glue, and attaching a hair piece was repeated 3 times within a 3-month period. A pruritic rash began several days after the application of the first hair piece. Subsequently, 2 more hair pieces were applied despite worsening of the eruption. The final hair piece was then removed and not reapplied. Physical examination found discrete and confluent pink plaques with crusting and excoriations, closely tracking the U-shaped profile of the adhesive portion of the hair piece. The clinical impression was contact dermatitis, and the patient was treated with topical betamethasone dipropionate 0.05% lotion twice a day, resulting in rapid resolution of the rash within 2 weeks. New hair growth was noted, and there were no signs of scarring alopecia. Treatment was discontinued. Approximately a month later, she returned complaining of severe pain and “pimples” on her scalp. Examination found erythema, erosions, crusts, follicular pustules, and alopecia involving the periphery of the eruption. A scalp biopsy found epidermal atrophy, focal erosions, and a mixed inflammatory infiltrate consisting of neutrophils, lymphocytes, and plasma cells (Figs 1 and 2). Fungal stains were negative. Bacterial cultures taken from pustules were also negative. Treatment was given with oral prednisone, 60 mg/d tapering to 10 mg/d over 2 weeks, and topical betamethasone dipropionate 0.05% lotion; however, examination 3 weeks later found worsening of her condition, with increased crusting, pustules, hair loss, and atrophy. Although the most active areas still followed the shape of the adhesive on the hair pieces, there was new involvement centrally and on the posterior neck (Fig 3). Repeat biopsies showed findings similar to those of the initial biopsy. Direct immunofluorescence was negative for immunoglobulin and complement deposition. The corticosteroids were discontinued, and treatment was initiated with topical tacrolimus 0.1% ointment applied twice daily. Monthly follow-up examinations found slow improvement, with decreasing erosions, crusts, pustules, and erythema. After 2 months of tacrolimus treatment, some areas of hair regrowth were noted; however, large areas of alopecia without visible follicular ostia persisted (Fig 4). The patient has continued topical tacrolimus 0.1% ointment once daily and has not experienced a recurrence.
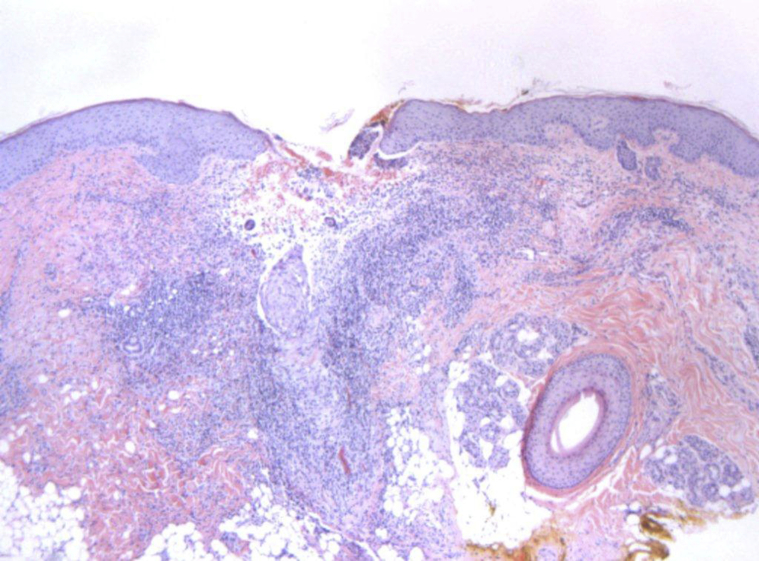
Fig 1.
Erosive pustular dermatosis of the scalp. Epidermal atrophy, focal erosions, and a mixed inflammatory infiltrate are present. (Hematoxylin-eosin stain; original magnification: ×5.)
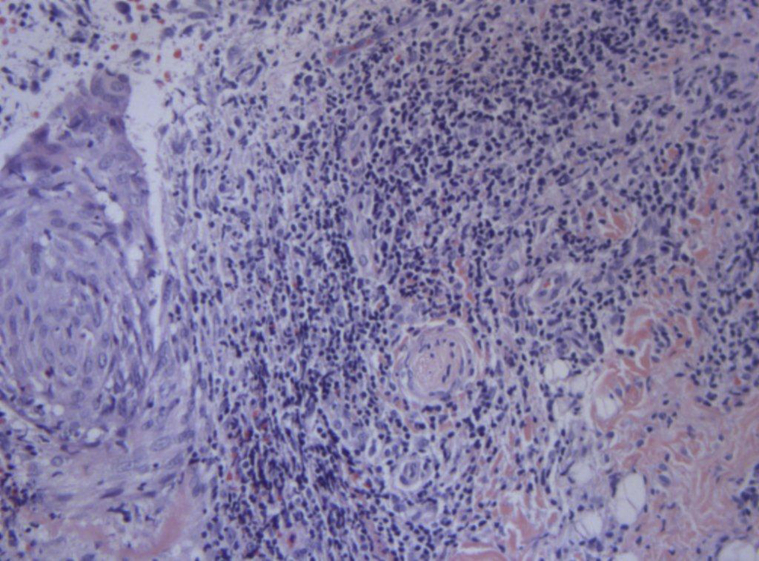
Fig 2.
Erosive pustular dermatosis of the scalp. A mixed inflammatory infiltrate is present. (Hematoxylin-eosin stain; original magnification: ×20.)
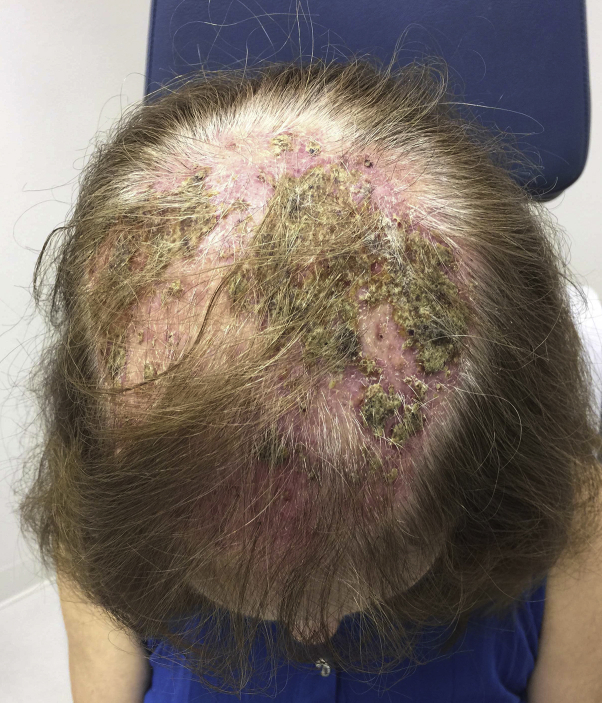
Fig 3.
Erosive pustular dermatosis of the scalp. Erythema, erosions, crusts, pustules, and early alopecia.
Fig 4.
Six month follow-up. Central hair regrowth and scarring alopecia in the areas of initial contact dermatitis.
Discussion
EPDS is a chronic inflammatory disease, with pustules, erosions, and crusting of the scalp, leading to scarring alopecia. Scalp trauma is described as a trigger factor, but autoimmune disorders including rheumatoid arthritis, autoimmune hepatitis, Hashimoto thyroiditis, and Takayasu aortitis are also reported.7 The differential diagnosis includes bacterial or fungal infection, irritated solar keratoses, squamous cell carcinoma, pustular psoriasis, Brunsting-Perry cicatricial pemphigoid, lupus erythematosus, pemphigus foliaceus, lichen planus, folliculitis decalvans, and other scarring alopecias. Reported treatments for EPDS include topical high-potency corticosteroids, retinoids, calcipotriol, dapsone, and topical tacrolimus.8, 9 Photodynamic therapy is effective in some patients but has induced the disease in others.4, 9
To the best of our knowledge, we report the first case of EPDS after treatment for contact dermatitis unrelated to irritation from topical medications. The diagnosis of contact dermatitis was supported by the temporal association with adhesive, a clinically consistent pruritic eruption following the adhesive pattern, and response to corticosteroid treatment. It would be interesting to know the components of the adhesive; however, its ingredients could not be obtained. The differentiation of EPDS from a chronic contact dermatitis was based on the observation that the new lesions started about a month after resolution of the initial contact dermatitis and lasted for several months without further application of adhesives or hair pieces. Retreatment with corticosteroids did not improve the condition, also supporting the diagnosis of an eruption separate from the initial contact dermatitis. Histologic findings in EPDS are nonspecific but typically show epidermal atrophy, focal erosions, and an upper dermal mixed inflammatory infiltrate. The findings are suggestive but not specific, so the diagnosis is usually made by excluding other conditions.10 The clinical features and course, negative cultures, ineffectiveness of antibiotics, negative direct immunofluorescence, and histologic findings that were not specific for the other conditions in the differential diagnosis were sufficient to diagnose the eruption as EPDS.
EPDS should be considered in any patient with a chronic inflammatory response, delayed healing, or recurrence of eruption after treatment for contact dermatitis. The pathogenesis of EPDS is unclear. Cultures are usually negative, and laboratory and histopathologic evaluations are not diagnostic. Because autoimmune disorders are described in association with some cases of EPDS, it has been suggested that trauma to the skin might cause auto-antibody production acting against skin structures that results in a secondary inflammatory reaction.7 This finding may underlie the observation that during our patient's peak severity, EPDS lesions extended beyond the initial area of contact dermatitis, involving the central scalp and posterior neck. Interestingly, the resultant scarring alopecia was within the initial contact dermatitis areas. Contact dermatitis should be added to the list of causative injuries that may induce EPDS, and dermatologists should be aware of this to avoid misdiagnosis.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Al-Benna S., Johnson K., Perkins W., O'Boyle C. Erosive pustular dermatosis: new description of a possible cause of the non-healing burn wound. J Burns. 2014;40(4):636–640. doi: 10.1016/j.burns.2013.08.042. [DOI] [PubMed] [Google Scholar]
- 2.Rongioletti F., Delmonte S., Rossi M.E., Strani G.F., Rebora A. Erosive pustular dermatosis of the scalp following cryotherapy and topical tretinoin for actinic keratosis. Clin Exp Dermatol. 1999;24(6):499–500. doi: 10.1046/j.1365-2230.1999.00546.x. [DOI] [PubMed] [Google Scholar]
- 3.Trueb R.M., Krasovec M. Erosive pustular dermatosis of the scalp following radiation therapy for solar keratosis. Br J Dermatol. 1999;141:763–765. doi: 10.1046/j.1365-2133.1999.03138.x. [DOI] [PubMed] [Google Scholar]
- 4.Guarneri C., Vaccaro M. Erosive pustular dermatosis of the scalp following methylaminolaevulinate photodynamic therapy. J Am Acad Dermatol. 2009;60(3):521–522. doi: 10.1016/j.jaad.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 5.Martin F.J., Herrera A., Rios J.J., Moreno J.C., Camacho F. Erosive pustular dermatosis of the scalp after skin grafting. Dermatol Surg. 2001;27(8):766–767. doi: 10.1046/j.1524-4725.2001.00212.x. [DOI] [PubMed] [Google Scholar]
- 6.Shahmoradi Z., Abtahi-Naeini B., Pourazizi M. Erosive pustular dermatosis of the scalp following hair transplantation. Adv Biomed Res. 2014;3:176. doi: 10.4103/2277-9175.139412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yamamoto T., Furuse Y. Erosive pustular dermatosis of the scalp in association with rheumatoid arthritis. Int J Dermatol. 1995;34:148. doi: 10.1111/j.1365-4362.1995.tb03605.x. [DOI] [PubMed] [Google Scholar]
- 8.Tardio N.B., Daly T.J. Erosive pustular dermatosis and associated alopecia successfully treated with topical tacrolimus. J Am Acad Dermatol. 2011;65(3):93–94. doi: 10.1016/j.jaad.2011.05.008. [DOI] [PubMed] [Google Scholar]
- 9.Meyer T., Lopez-Navarro N., Herrera-Acosta E., Jose A., Herrera E. Erosive pustular dermatosis of the scalp: A successful treatment with photodynamic therapy. Photodermatol Photoimmunol Photomed. 2010;26:44–45. doi: 10.1111/j.1600-0781.2009.00478.x. [DOI] [PubMed] [Google Scholar]
- 10.Bolduc C., Sperling L.C., Shapiro J. Primary cicatricial alopecia: Other lymphocytic primary cicatricial alopecias and neutrophilic and mixed primary cicatricial alopecias. J Am Acad Dermatol. 2016;75(6):1101–1117. doi: 10.1016/j.jaad.2015.01.056. [DOI] [PubMed] [Google Scholar]