Abstract
Background:
Myocardial infarction (MI) is one of the major causes of death and disability worldwide, which can reduces quality of life in patients. Some disabilities are depression and anxiety which delay returning to work. The aim of this study was to evaluate the effect of illness perception focused intervention on quality of life, anxiety, and depression in MI patients.
Materials and Methods:
A randomized controlled trial study of 48 recently hospitalized MI patients was conducted (24 in intervention group and 24 in control group). Intervention group was trained to understand the disease by a mental health counselor in three half-an-hour sessions for three consecutive days. Data were collected from three questionnaires: hospital anxiety and depression scale, the World Health Organization Quality of Life Questionnaire (short form), and Illness Perceptions Questionnaire Brief at admission, 1.5, and 3 months postdischarge. Data were analyzed with ANOVA repeated measure.
Results:
The mean duration of returning to work was 28.7 ± 8.1 days in intervention groups and 46 ± 7.6 days in control group which was statistically significant (P < 0.001). Moreover, anxiety, depression, and illness perceptions score were significantly decreased in intervention groups which were 8.3 ± 3.3, 6.8 ± 3.5, and 36.5 ± 5 in intervention groups and 15.8 ± 2.1(P < 0.001), 17.1 ± 2.3 (P < 0.001), and 41.9 ± 4 (P < 0.001) in control group, respectively. Mean of quality of life subscales scores just physical health subscale showed a significant reduction after 3 months in the control group.
Conclusion:
Training MI patients to understand the disease in three half-an-hour sessions for 3 consecutive days can decrease the duration of returning to work, anxiety and depression, and increase illness perceptions which can make a better outcome.
Keywords: Anxiety, depression, illness perceptions, myocardial infarction, quality of life
INTRODUCTION
Myocardial infarction (MI) is one of the major causes of death and disability worldwide and may be a major catastrophic event leading to sudden death or hemodynamic deterioration.[1] A significant proportion of patients with MI is in working age and returning to work after illness is associated with better quality of life.[2] A large number of patients with acute MI, despite being physically able to work, do not return to work because of some complications such as depression and anxiety leading to changing on lifestyle and decreasing the patients’ health-related quality of life (HRQOL).[3] Myocardial ischemia and the possibility of fatal dysrhythmias increase the level of stress and endangering the adjustment process and future morbidity of discharged patients.[4] In some studies on patients with heart attack have shown that their feeling and attitude to heart disease (illness perception) strongly impact on recovery process.[5]
Counting empirical evidence from a range of disease groups (e.g., cancer, psoriasis, asthma, diabetes, hemophilia, and chronic fatigue syndrome) suggests that illness perception is a key determinant of recovery and may represent a potential target for clinical intervention.[6] The association between these personal illness perceptions and recovery is based on a theory of self-regulation that posits individuals as active problem solvers who, in response to illness and other health threats, develop parallel cognitive and emotional representations of the threat.[7] One prior study (N = 105) investigated the prospective association between illness perception and depression in a group of MI patients and found that changes in beliefs regarding angina and MI over 1 year made near significant contributions (P = 0.06) to the variance in depressive symptomatology on the hospital anxiety and depression scale (HADS).[8] Illness perception may impact on other outcomes including HRQOL, HRQOL is increasingly recognized as a valued outcome in MI patients[9] and is reported to predict cardiac end points.[10] In a study by Yan et al. on 124 patients admitted with the first acute MI were randomized to receive routine care or routine care plus a telephone follow-up intervention, which consist of a predischarge education and three telephone follow-up instructions. At the 6th and the 12th week after discharge, patients in the intervention group had significantly positive perceptions about symptoms of MI and better lifestyle after.[11]
This study was designed to investigate the possible effects of authors developed brief, practical, easily implementable, and bedside illness perception improvement intervention on quality of life, anxiety, and depression in Iranian MI patients.
SUBJECTS AND METHODS
Procedure
These multicenter, parallel groups randomized controlled trial study was done to compare quality of life, anxiety, and depression in patients with MI who discharged from hospital undergone an illness perception improvement intervention (study group) to the routine discharged patients (control group). Inclusion criteria were patients who have chest pain lasts at least 20 min or presence of pathological changes indicative of ischemia in the electrocardiographic waves or increasing in cardiac enzymes (diagnostic criteria of MI). Those with myocardial infarct secondary to bypass surgery or angioplasty, a history of psychiatric disorders (anxiety or depression), treated depression or anxiety, and substance abuse or dependence were not intended to the study.
Intervention group was educated to better understand of disease process by a resident of psychiatry and a clinical psychologist, who were trained under the supervision of a cardiologist. Intervention was done in three half-an-hour individual and interactive sessions in 3 consecutive days at the bedside of patients, and the control group do not receive any special educational program (the current method in the hospital). Training sessions started the day after cardiac stabilization and completing the questionnaires. In the first session, the patients requested to explain their beliefs regarding the causes of MI and wrong beliefs were described and modified by trainers. The second session implemented to checking the current lifestyle and education regarding healthy lifestyle of patient with MI, and the last session was about the signs of a recovery period, changing the lifestyle to preventing from recurrence of MI, importance of using prescribed drugs regularly, and the role of the partner in the process of recovery.
Quality of life, anxiety, and depression were measured as the base at the 1st–3rd days of admission to hospital, and then 1.5 and 3 months after intervention.
Participants
Participants were recruited between August and December 2014 from Chamran, Alzahra, and Khorshid hospitals in Isfahan and ShahidBeheshti and Milad Hospitals in Kashan and SeyedAlshohada hospital in Aram in Iran. All patients who were hospitalized for a definite MI diagnosed by a cardiologist at this time framework were eligible for participation.
Sixty-five patients were contacted, 17 patients declined to participate and 48 cases included in the study and allocated with a simple random sampling method in two groups of intervention and control (24 cases in each group). The study received ethics approval from the relevant Institutional Review Committees, and all participants gave written informed consent.
Instruments
Hospital anxiety and depression scale
This short questionnaire evaluates the anxiety and depression in medically ill patients by to removing the physical symptoms and focusing on psychological symptoms. Anxiety and Depression scale consists of 14 items and two subscales of anxiety and depression. Each item is a set of 4-point calibration, and a score of 8 or greater on one or both of the subscales indicates the presence of a depressive or anxiety disorder. Completion of the questionnaire takes only a few minutes. The developers aimed to discard all ambiguous somatic symptoms such as dizziness and lethargy and instead comprised the depression subscale around the psychopathology of anhedonia and the anxiety subscale based on the cognitive symptoms of anxiety. The HADS has been found to perform reliably in psychiatric, nonpsychiatric, and well populations as a screening tool;[12] however, its use as a diagnostic instrument for research may be inappropriate.[13] In a study in Iranian patients, the Iranian version of the HADS was found to be acceptable to almost all patients (99%). Cronbach's alpha coefficient (to test reliability) has been found to be 0.78 for the anxiety subscale and 0.86 for the depression subscale, respectively.[14]
The World Health Organization Quality of Life Questionnaire (short form)
The questionnaire included 26 questions on a Likert scale of 1–5 different aspects of the person's quality of life. One question measures the total sense of person to own life and other questions measure the feeling and behavior in the last 2 weeks such as (1) the field of health and physical health (physical activity, substance dependence and complementary medicines, mobility, pain and discomfort, sleep, rest, and ability to work); (2) psychological (feelings toward body appearance, positive and negative emotions, learning, thinking, memory, concentration, confidence, and personality traits spirit); (3) social relationships (personal relationships, social support, and sexual activity); (4) the social environment (financial resources, liberty and physical security, access to health and social care, home environment, opportunities, access to information, and the opportunity to participate in social activities) and physical environment (pollution, and transportation). The psychometric properties of these instruments have been confirmed as acceptable in most of these populations.[15,16,17] The psychometric properties of the Persian version were done by Nejat et al. intraclass correlation and Cronbach's alpha values were achieved more than 0.70 in all areas, but in the sphere of social relations was 0.55.[18]
Illness Perceptions Questionnaire Brief
A short form of Illness Perceptions Questionnaire Brief was used to basic evaluate and follow-up of illness perception score. The questionnaire consists of 9 subscales. Five subscales measur cognitive reaction to disease including perceptions of the consequences, disease duration, self-control, controlled by treatment, and cognitive symptoms. Two subscales measure anxiety about illness and emotions. One subscale measures capability to understand the condition and cause direction which is an open question. This questionnaire has been reported as a reliable and valid instrument to measure the illness perception in various conditions.[19]
Data analysis
Analysis was done using descriptive statistics such as mean and standard deviation and analytical statistics such as ANOVA repeated measure by SPSS 20 software. P < 0.05 considered as meaningful
RESULTS
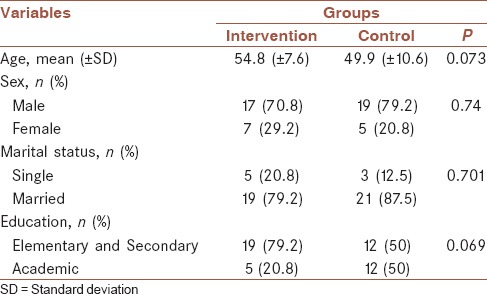
The mean age of the patients in the intervention group (17 males, 7 females) was 54.8 ± 7.6 years and in control group (19 males, 5 females) was 49.9 ± 10.6 years. Table 1 shows a comparison of demographic findings of two groups.
Table 1.
Comparison of demographic variables in two groups
The mean duration of returning to work was 28.7 ± 8.1 days in intervention groups and 46 ± 7.6 days in control group that this difference was statistically significant (P < 0.001).
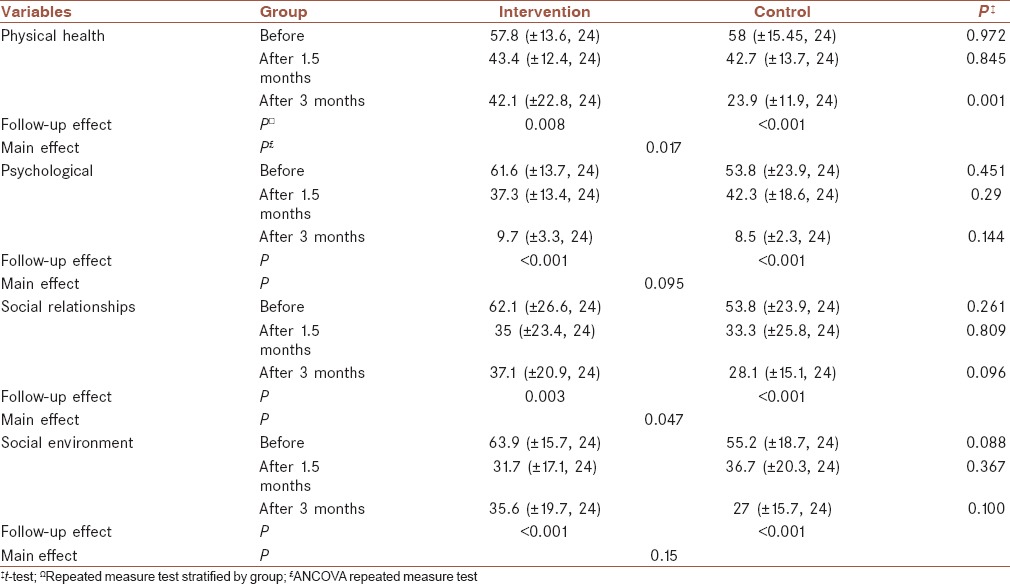
Table 2 shows quality of life subscales scores before and over 3 months follow-up after intervention.
Table 2.
Comparison of quality of life subscales scores over 3-month follow-up after intervention
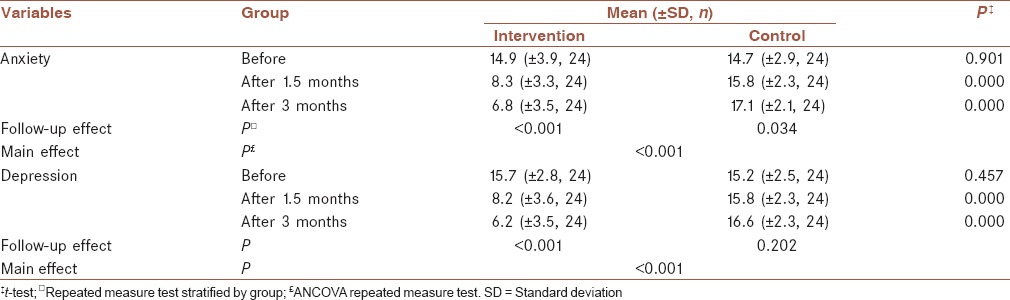
Mean of anxiety and depression score was significantly decreased in intervention groups compared to control group after 1.5 and 3 months [Table 3].
Table 3.
Comparison of anxiety and depression scores over 3-month follow-up after intervention
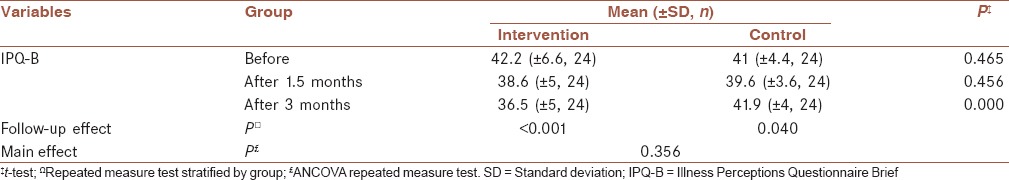
Mean of illness perceptions score was significantly decreased in intervention groups compared to control group after 3 months [Table 4].
Table 4.
Illness Perceptions Questionnaire Brief score over 3-month follow-up after intervention
DISCUSSION
This clinical trial developed and tested an illness perception intervention in MI patients. Forty-eight patients with a recent MI had been included in this trial in two equal groups of intervention and control.
Setting the patients on educating the patients to planning exercise schedules, modifying wrong beliefs, changing lifestyle, and a date to return to work into an action plan, together with reinforcing controllable causal attributions were the main component of the intervention in this study. Emphasizing on the nature of atherosclerosis and muscle damage, modifying wrong beliefs, and explaining that heart disease is a chronic condition and need to change lifestyle were the another components of our intervention.
The intervention significantly improved the speed of return to work, physical health, depression and anxiety, and illness perception after 3 months compared to the control group. In other studies, it was found that increasing illness perception can lower patient anxiety and depression and improved patients’ information regarding MI. In these studies, it was indicated that patients who received the intervention felt more prepared to leave the hospital and reported higher intentions to attend rehabilitation classes than the control group. They reported greater increases in exercise and fewer calls to the general practitioner or hospital relating to their heart condition which could obtain by the following patients in our study.[20,21,22]
In terms of illness perceptions, the intervention increased patients’ feeling of coherence about their condition, and this remained over the course of the 3-month follow-up. The intervention also significantly strengthened patients’ causal attributions for the heart attack to high cholesterol and lack of exercise in comparison to the control group. These changes in coherence and causal attributions gave the patients a coherent illness model on which to base their recovery and modifiable causal attributions and made them to have more physical health score and lowered anxiety and depression.
Regarding quality of life as shown in Table 2, if the physical health score in intervention group is better on follow-up, the quality of life scores decreased in both intervention and control groups in all domains during 3 month follow-up in comparison to the base scores. This finding shows that MI as a catastrophic accident has a serious side effect on all aspects of the life of affected patients and returning to pre-MI situation needs more time and rehabilitations.
Causal attributions to internal and controllable factors have been linked to faster return to work and improving depression and anxiety about the disease and changed lifestyle.[20] In a previous research, attributions to fate and luck predicted poor prognosis and lowered functioning in 12 years following of a group of MI patients.[21]
Previous studies showed illness perceptions are well recognized as a target for treatment,[22] and illness perception interventions have shown promising results for patients with acute[23] and chronic conditions.[24]
It is useful to consider why, in contrast to the previous trials, control perceptions were not changed. One possible reason is that the patient education about their disease is not performed routinely in hospitals which were studied and this fact is due to the high patient load in these centers and not having a systematized program of education after MI. Moreover, heart disease has been believed as disaster event in Iran, which can influence patient's lifestyle more than the other diseases.
The causal attributions have been explained much more than hereditary factors which may reflect a greater understanding of the cause of the patient's condition that could reduce anxiety associated with not knowing what caused the event. Having a solid causal framework could also increase the match between illness perceptions and the need for treatment and lifestyle modification. While a positive family history cannot be changed, recognizing a high genetic risk may make the patient more motivated to reduce other risk factors that are modifiable, such as high cholesterol, through exercise, diet, and medication.[25]
In this study, the intervention was very brief, but it had some positive outcomes. This demonstrates that a brief education regarding illness perception for the MI patient can improve their understanding of the MI and lessen their anxiety and depression about the condition and improves them to return to work faster. Moreover, our study was based on bedside intervention which can have more influence on the patient's illness perception, also the length of intervention classes in our study was half-an-hour for 3 consecutive days. However, in other studies, the method of intervention was different that lead to have a less positive influence on the illness perceptions. Yan et al. used telephone follow-up intervention,[11] Broadbent et al. used one half-hour patient-and-spouse session,[24] and Williams et al. studied on type D personality.[25] Moreover, increasing illness perception could be more cost benefits due to decreasing the rehospitalization, mortality, and increase objective health outcomes by preparing them to return to work faster.[26]
Recent studies in primary care highlight the importance of patients’ beliefs and emotional responses to their illness as being important in influencing their satisfaction with the consultation, reassurance following negative medical testing, and future health-care use. Recent research shows illness perceptions to have associations with a number of outcomes in chronic illness including self-management behaviors and quality of life. As yet, however, few interventions have been developed designed to change illness perceptions and improve illness outcomes.[27]
Illness perceptions influence the way, in which patients cope and their self-management of the illness. Illness perceptions can be assessed quite easily and directly, they inform health-care providers about the psychosocial responses of patients toward their illness, they are responsive to change in the clinical encounter or through self-management intervention training. Exploring patient's illness perceptions, therefore, is a crucial component of good clinical care.[28]
Limitation
First, patients were selected from different hospitals in Isfahan and Kashan cities, so the results of the study may have limited generalizability. Second, further research should extend the follow-up period to assess the long-term outcomes of the intervention.
CONCLUSION
Training MI patients to understand the disease in three half-an-hour sessions for 3 consecutive days can decrease the duration of returning to work, anxiety and depression, and increase illness perceptions which can make a better outcome. However, our results showed that the quality of life of patients has not been affected as much as other studied variable which needs long-term follow-up. In other words, decreasing the rate of anxiety and depression in MI patients may lead to increase the quality of life which needs to be followed up for several months or years.
Financial support and sponsorship
The study was supported by Isfahan University of Medical Science, Isfahan, Iran.
Conflicts of interest
There are no conflicts of interest.
AUTHORS’ CONTRIBUTION
RBS: contributed in the conception of the work, design of the work, conducting the study and agreed for all aspects of the work.
MM: contributed in the data collection, drafting and revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work.
GhRKh: Contributed in the conception of the work, study design, conducting the study, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work.
MRM: Contributed in the study design, Data analysis, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work.
EP: Contributed in the data collection, drafting and revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work.
Acknowledgments
We gratefully acknowledge the dedicated efforts of the investigators, coordinators, and volunteer patients, who participated in this study.
REFERENCES
- 1.Mathers C, Vos T, Stevenson C. The Burden of Disease and Injury in Australia. Canberra, Australian Capital Territory: Australian Institute of Health and Welfare. 1999 [Google Scholar]
- 2.Antman EM. ST-elevation myocardial infarction: Management. In: Libby P, Bonow RO, Mann DL, Zipes DP, editors. Braunwald s Heart Disease: A Text of Cardiovascular Medicine. 8th ed. Philadelphia: Saunders, Elsevier; 2008. pp. 1233–99. [Google Scholar]
- 3.Rudisch B, Nemeroff CB. Epidemiology of comorbid coronary artery disease and depression. Biol Psychiatry. 2003;54:227–40. doi: 10.1016/s0006-3223(03)00587-0. [DOI] [PubMed] [Google Scholar]
- 4.Frasure-Smith N, Lespérance F, Juneau M, Talajic M, Bourassa MG. Gender, depression, and one-year prognosis after myocardial infarction. Psychosom Med. 1999;61:26–37. doi: 10.1097/00006842-199901000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Wearden AJ. Illness perception interventions for heart attack patients and their spouses: Invited commentary. J Psychosom Res. 2009;67:25–7. doi: 10.1016/j.jpsychores.2009.01.018. [DOI] [PubMed] [Google Scholar]
- 6.French DP, Cooper A, Weinman J. Illness perceptions predict attendance at cardiac rehabilitation following acute myocardial infarction: A systematic review with meta-analysis. J Psychosom Res. 2006;61:757–67. doi: 10.1016/j.jpsychores.2006.07.029. [DOI] [PubMed] [Google Scholar]
- 7.Leventhal H, Nerenz DR, Steele DS. Illness representations and coping with health threats. In: Baum A, Taylor SE, Singer JE, editors. Handbook of Psychology and Health. Hillsdale, NJ: Erlbaum; 1984. pp. 219–52. [Google Scholar]
- 8.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 9.Haas DC. Depression and disability in coronary patients: Time to focus on quality of life as an end point. Heart. 2006;92:8–10. doi: 10.1136/hrt.2005.066035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yan J, You LM, He JG, Wang JF, Chen L, Liu BL, et al. Illness perception among Chinese patients with acute myocardial infarction. Patient Educ Couns. 2011;85:398–405. doi: 10.1016/j.pec.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 11.Yan J, You LM, Liu BL, Jin SY, Zhou JJ, Lin CX, et al. The effect of a telephone follow-up intervention on illness perception and lifestyle after myocardial infarction in China: A randomized controlled trial. Int J Nurs Stud. 2014;51:844–55. doi: 10.1016/j.ijnurstu.2013.10.011. [DOI] [PubMed] [Google Scholar]
- 12.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the hospital anxiety and depression scale. An updated literature review. J Psychosom Res. 2002;52:69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 13.Silverstone PH. Poor efficacy of the hospital anxiety and depression scale in the diagnosis of major depressive disorder in both medical and psychiatric patients. J Psychosom Res. 1994;38:441–50. doi: 10.1016/0022-3999(94)90105-8. [DOI] [PubMed] [Google Scholar]
- 14.Montazeri A, Vahdaninia M, Ebrahimi M, Jarvandi S. The hospital anxiety and depression scale (HADS): Translation and validation study of the Iranian version. Health Qual Life Outcomes. 2003;1:14. doi: 10.1186/1477-7525-1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bonomi AE, Patrick DL, Bushnell DM, Martin M. Validation of the United States’ version of the World Health Organization Quality of Life (WHOQOL) instrument. J Clin Epidemiol. 2000;53:1–12. doi: 10.1016/s0895-4356(99)00123-7. [DOI] [PubMed] [Google Scholar]
- 16.Skevington SM. Measuring quality of life in Britain: Introducing the WHOQOL-100. J Psychosom Res. 1999;47:449–59. doi: 10.1016/s0022-3999(99)00051-3. [DOI] [PubMed] [Google Scholar]
- 17.Skevington SM. Advancing cross-cultural research on quality of life: Observations drawn from the WHOQOL development. World Health Organization Quality of Life Assessment. Qual Life Res. 2002;11:135–44. doi: 10.1023/a:1015013312456. [DOI] [PubMed] [Google Scholar]
- 18.Nejat S, Montazeri A, Holakouie Naieni K, Mohammad K, Majdzadeh SR. The World Health Organization Quality of Life questionnaire: Translation and validation study of the Iranian version. J Sch Public Health Inst Public Health Res. 2006;4:1–12. [Google Scholar]
- 19.Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60:631–7. doi: 10.1016/j.jpsychores.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 20.Foster NE, Bishop A, Thomas E, Main C, Horne R, Weinman J, et al. Illness perceptions of low back pain patients in primary care: What are they, do they change and are they associated with outcome? Pain. 2008;136:177–87. doi: 10.1016/j.pain.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 21.Broadbent E, Ellis CJ, Thomas J, Gamble G, Petrie KJ. Further development of an illness perception intervention for myocardial infarction patients: A randomized controlled trial. J Psychosom Res. 2009;67:17–23. doi: 10.1016/j.jpsychores.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 22.Botha-Scheepers S, Riyazi N, Kroon HM, Scharloo M, Houwing-Duistermaat JJ, Slagboom E, et al. Activity limitations in the lower extremities in patients with osteoarthritis: The modifying effects of illness perceptions and mental health. Osteoarthritis Cartilage. 2006;14:1104–10. doi: 10.1016/j.joca.2006.04.011. [DOI] [PubMed] [Google Scholar]
- 23.Weinman J, Petrie K, Sharpe N, Walker S. Causal attributions in patients and spouses following first-time myocardial infarction and subsequent lifestyle changes. Br J Health Psychol. 2000;5:263–73. [Google Scholar]
- 24.Broadbent E, Ellis CJ, Thomas J, Gamble G, Petrie KJ. Can an illness perception intervention reduce illness anxiety in spouses of myocardial infarction patients? A randomized controlled trial. J Psychosom Res. 2009;67:11–5. doi: 10.1016/j.jpsychores.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 25.Williams L, O’Connor RC, Grubb NR, O’Carroll RE. Type D personality and illness perceptions in myocardial infarction patients. J Psychosom Res. 2011;70:141–4. doi: 10.1016/j.jpsychores.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 26.Foxwell R, Morley C, Frizelle D. Illness perceptions, mood and quality of life: A systematic review of coronary heart disease patients. J Psychosom Res. 2013;75:211–22. doi: 10.1016/j.jpsychores.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 27.Petrie KJ, Jago LA, Devcich DA. The role of illness perceptions in patients with medical conditions. Curr Opin Psychiatry. 2007;20:163–7. doi: 10.1097/YCO.0b013e328014a871. [DOI] [PubMed] [Google Scholar]
- 28.Kaptein AA, Klok T, Moss-Morris R, Brand PL. Illness perceptions: Impact on self-management and control in asthma. Curr Opin Allergy Clin Immunol. 2010;10:194–9. doi: 10.1097/ACI.0b013e32833950c1. [DOI] [PubMed] [Google Scholar]


