Abstract
Objective:
Pulmonary hypertension is a serious complication in patients suffering from chronic obstructive pulmonary disease (COPD). The aim of this study is to investigate the effects of atorvastatin in reducing pulmonary arterial pressure in COPD patients.
Methods:
This double-blind, randomized trial was conducted on 42 known cases of COPD with systolic pulmonary arterial pressure of more than 25 mmHg. The patients were randomly assigned into two groups, 21 patients with atorvastatin treatment (40 mg/daily for 6 months) and 21 patients without receiving atorvastatin. All the patients participated voluntarily and provided written informed consent. The trial was registered in the Iranian Registry of Clinical Trials. Pulmonary pressure was also anticipated by Doppler echocardiography with peak pressure gradient of tricuspid regurgitation. Both groups were tested with echocardiography to measure systolic pulmonary pressure at baseline and posttreatment. Statistical analysis includes Chi-square, Student's t-test, and Wilcoxon test. P < 0.05 was considered statistically significant.
Findings:
The mean age was 65.8 ± 11.5 years for atorvastatin group and 63.7 ± 7.6 years for control group (P = 0.45). Baseline and posttreatment mean systolic pulmonary artery pressure (PAP) levels in the atorvastatin group were 48.9 ± 3.3 and 38.4 ± 1.9 mmHg, respectively (P = 0.007). In the control group, mean systolic PAP levels at baseline and 6 months later were 45.6 ± 3.1 and 38.9 ± 2.4 mmHg, respectively (P = 0.073). The patients treated with atorvastatin showed significant decrease in total cholesterol (P = 0.001) and low-density lipoprotein cholesterol (P = 0.008).
Conclusion:
A 40 mg dose of atorvastatin daily for 6 months may have beneficial effects in reducing PAP in patients with COPD. Further studies are necessary to find long-term effects of statins in COPD patients.
KEY WORDS: Atorvastatin, chronic obstructive pulmonary disease, pulmonary artery pressure
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is a major public health problem across the world. It is estimated to be the third cause of death and fifth rank in burden by 2020.[1] Large numbers of patients are frequently hospitalized due to COPD and its complications. COPD patients die from coronary artery disease (CAD), lung cancer, and stroke. Overall, these factors account for 80% of deaths from COPD.[2]
A consequence of COPD, pulmonary hypertension (PH), commonly presents as shortness of breath and fatigue.[3] It is a serious complication among COPD patients that can lead to poor prognosis.[4] PH is caused by an increase in pulmonary vascular resistance and is determined by continuous increase in pulmonary arterial blood pressure, especially mean pulmonary arterial pressure >25 mmHg at rest or 30 mmHg during activity.[5] Several factors are involved in occurrence of PH in patients with COPD including chronic alveolar hypoxia and inflammatory responses.[6] Studies show that in COPD patients, in particular those with PH, survival is reduced in comparison with those without PH.[6] It is unclear to what extent early diagnosis and treatment of PH can contribute to the survival of patients with COPD. Evidently, statins can reduce symptoms and improve quality of life in these patients.[7] There are many treatment options for PH in COPD, but each has its own limitations.[6]
Since inflammation is considered as an underlying cause of COPD associated with PH, anti-inflammatory properties of statins may theoretically play a beneficial role in these patients.[8] Several observational studies and randomized clinical trials have studied the effect of statins on reducing PH.[9,10,11,12,13] Statins have some antiproliferative, antithrombotic, and anti-inflammatory properties that make them an effective option for the treatment of PH.[14] In this study, we preferred to use atorvastatin as a treatment option, because it is well-known and more accessible drug in our country in comparison with other drugs in this class. Due to the effectiveness of 6-month treatment with statins on ability of patients reported by Lee et al.[11] and also chronic inflammation of the airways in COPD patients, effectiveness of statins in the short term will be less reliable. Hence, to observe the more effective impacts, treatment period considers to be 6 months. Given the conflicting results in different observational studies and randomized controlled trials (RCTs), we aimed to study the effects of statins on pulmonary artery pressure (PAP) in patients with COPD.
METHODS
This double-blind, randomized trial was conducted on 42 known cases of COPD with systolic pulmonary arterial pressure of > 25 mmHg, who attended Vali-Asr Hospital, Birjand, East of Iran in 2014. Afterward, each patient was assigned into either of two groups using block randomization method. Twenty-one patients were treated with atorvastatin (40 mg/day) and 21 patients without receiving atorvastatin. The control and atorvastatin groups who completed the study included 18 and 16 patients, respectively. Patients were excluded from the study because of death, refuse to continue treatment, or migration. Patients and the outcome assessor were blind until the study was completed. None of the patients were under specific treatment for PH (e.g., prostanoids, statins, endothelin antagonists, and phosphodiesterase) or under domestic O2 therapy. The methods of this study were reviewed and approved by Birjand University of Medical Sciences Ethics Committee and followed Consort 2010 checklist.[15]
All the patients participated voluntarily after they had been fully informed of the therapies and after they had provided written informed consent. The trial was registered at the Iranian Registry of Clinical Trials with the registration number of IRCT2016042527594N1 where the full-trial protocol is accessible. Inclusion criteria included no previous use of statins, absence of liver disease, and presence of diagnostic criteria for COPD based on the American Thoracic Society (forced expiratory volume 1 s [FEV1] <80% and FEV1/forced vital capacity <70%).[16] The patients would be excluded for the following reasons: discontinuation of statin therapy during the study, having advanced heart disease, the advent of statin therapy complications, and long-term use of systemic corticosteroids. The collected data involved age, sex (male/female), total cholesterol (TC) (mg/dL), triglycerides (TGs) (mg/dL), high-density lipoprotein (HDL) cholesterol (mg/dL), and low-density lipoprotein (LDL) cholesterol (mg/dL).
Echocardiograms were performed in Vali-Asr Hospital by VIVID 10 echocardiography equipment (MEDISON, Korea). Pulmonary pressure was also anticipated by Doppler echocardiography with peak pressure gradient of tricuspid regurgitation. Both groups were tested with echocardiography to measure systolic pulmonary pressure before atorvastatin was taken, and their systolic PAP was recorded at baseline. The case group received 40 mg of statins/day for 6 months (24 weeks) to observe long-term effects[11] whereas the control group received routine treatment for COPD, the usual therapy for airway disease. At the end of the study, the patients were evaluated by echocardiography again. Lipid profile was measured again at the end of 6th month from the study onset.
Statistical analysis was done using SPSS software (Version 16; SPSS Inc., Chicago, IL, USA). Continuous data are expressed as mean (standard deviation [SD]) and categorical data are presented as counts and percentages. Statistical analysis included Chi-square test, independent Student's t-test, and Wilcoxon test. P < 0.05 was considered statistically significant.
RESULTS
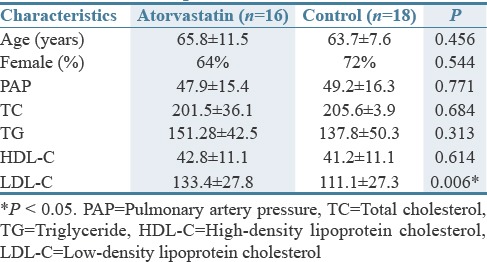
A total of 42 patients were randomized into atorvastatin and control groups. Totally, 64% of the members in the atorvastatin group and 72% of the control group were female. At the baseline, the mean (SD) age was 65.8 ± 11.5 years for atorvastatin group and 63.7 ± 7.6 years for control group. Means of PAP and TC were nonsignificantly lower in atorvastatin group than that in the control group. In contrast, although it was not statistically significant, the mean TG and high-density lipoprotein cholesterol levels were higher in the control than that of treatment group [Table 1].
Table 1.
Baseline clinical and demographic characteristics of the patients
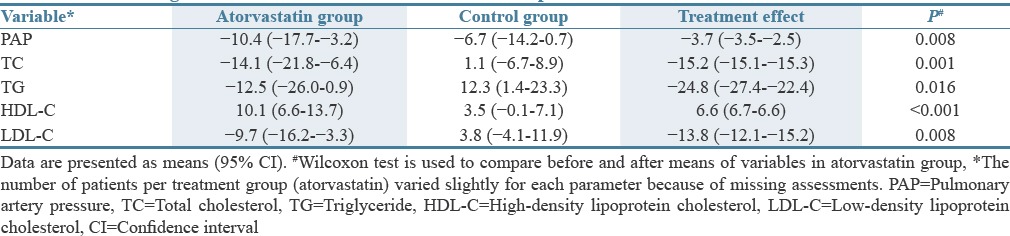
Changes in clinical characteristics of patients are shown in Table 2. The patients treated by atorvastatin showed a significant decrease in the mean PAP (P = 0.008), TC (P = 0.001), TGs (P = 0.016), LDL cholesterol (P < 0.001), and a significant increase in the level of HDL cholesterol (P = 0.008) compared to baseline values. These changes did not differ significantly within the control group after 24 weeks [Table 2].
Table 2.
Mean change in baseline clinical characteristics of the patients from baseline to week 24
DISCUSSION
In the present study, a 40 mg daily dose of atorvastatin significantly reduced PAP in patients with COPD. Statins are drugs that have recently become more prevalent. In addition, there has been a special attention in pleiotropic effects of statins in recent years.[17] One of the applications recently considered for statins related to patients with primary or secondary PH. The beneficial effects of statins on pulmonary arterial pressure in animals have been shown recently.[18]
However, the results of the first randomized clinical trial about the impact of statins on PH were not very promising.[19] Carlin et al.'s study on animal models concerning the influence of pharmaceutical forms of statins on PAP showed that some form of statins such as fluvastatin can be effective in reducing PAP. Thus, they suggested that some forms of statins may be more effective in reducing PAP than others.[20] A study on the effects of atorvastatin at a dose of 10 mg daily for 6 months on 220 patients with PH or chronic thromboembolic PH in China showed that statins had no significant effect on PAP.[21] Another study on the impact of statins on the PAP showed that prescribing simvastatin ranged between 20 and 80 mg/daily can reduce right ventricular systolic pressure and lead to improvement in 6-min walking test.[12] The authors emphasized on the safety of simvastatin in patients with PH and stated that the rate of disease progression appeared to be attenuated. A study conducted by Zeng et al. also demonstrated that simvastatin treatment beginning at 20 mg/daily for 2 months, then increasing to 40 mg/daily for another 4 months, decreased PAP in patients with PH.[21]
On the other hand, in a clinical trial in those treated with simvastatin 80 mg daily for 6 months, the short-term effect of simvastatin showed a reduction in right ventricular pressure. However, this effect did not sustain after 6 months.[19]
PH is a common complication of COPD characterized by reduced life expectancy, poor prognosis, and high health-care costs.[22] In recent years, a new theory holds that the main contributor to PH is endothelial dysfunction and inflammatory mechanisms.[23] Statins can be useful given their anti-inflammatory, antioxidant, and antithrombogenic properties and the improvement they incur in endothelial cell function in patients with PH, which is caused by COPD.[24] A few studies have been performed on the effects of statins in reducing PAP in patients with COPD. In an RCT study by Lee et al.[11] on the effects of statins on PAP in patients with COPD, it was found that 40 mg/day pravastatin for 6 months can be significantly effective in reducing PAP and improving physical abilities. Nonetheless, Moosavi et al. showed that atorvastatin's effect was not statistically significant in reducing pulmonary arterial systolic pressure in patients with COPD and recommended further study concerning the relation between PAP and atorvastatin.[4] The effects of statins in reducing PAP in different studies appear to depend largely on the dose used. It is believed that when the atorvastatin dose increases from 40 to 80 mg, its anti-inflammatory effects appear.[25] We found a beneficial effect of atorvastatin at a dose of 40 mg on pulmonary arterial pressure. This may be the minimum effective dose to reduce pulmonary arterial pressure in patients with COPD.
Another beneficial effect in relation to the use of atorvastatin included decreased LDL level and increased HDL level. All these benefits without significant side effects were observed in our patients. Moreover, the beneficial effects of statins on blood lipid profile are well known. The beneficial effects of statins on blood lipid profile in patients with COPD is important since CAD in patients with COPD is more prevalent and it is the second most common cause of death in these patients after respiratory failure.[26] A series of studies and a meta-analysis of articles related to the effects of statins in patients with COPD showed that statins were associated with a significant reduction in myocardial infarction risk.[27] During 6-month follow-up, the major side effects that forced us to discontinue atorvastatin were not observed.
A dose of 40 mg of atorvastatin/day for 6 months may have beneficial effects in reducing PAP and improving blood lipid profile in patients with COPD. Further studies are needed to overcome the limitations of the present study and to find long-term effects of statins on PAPs in COPD patients.
The limitations of the present study were lack of large sample size, lack of direct measurement of the systolic and diastolic PA pressures, and also the lack of precise care on drug use by patients.
AUTHORS' CONTRIBUTION
Anahita Arian, Sayyed Gholamreza Mortazavi Moghadam and Toba Kazemi contributed on idea, design, sample collection, patient management and writing the manuscript. Morteza Hajihosseini contributed on analyzing and writing first draft. All authors read and approved the manuscript.
FINANCIAL SUPPORT AND SPONSORSHIP
Funding support for this project was provided by the Research Committee of Birjand University of Medical Sciences.
CONFLICTS OF INTEREST
There are no conflicts of interest.
ACKNOWLEDGMENTS
This article was derived from the thesis of internal medicine assistant student Mrs. Anahita Arian. Authors are grateful to all cooperation and funding support for this project.
REFERENCES
- 1.Vestbo J, Hurd SS, Agustí AG, Jones PW, Vogelmeier C, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187:347–65. doi: 10.1164/rccm.201204-0596PP. [DOI] [PubMed] [Google Scholar]
- 2.Maclay JD, McAllister DA, Macnee W. Cardiovascular risk in chronic obstructive pulmonary disease. Respirology. 2007;12:634–41. doi: 10.1111/j.1440-1843.2007.01136.x. [DOI] [PubMed] [Google Scholar]
- 3.Sun XG, Hansen JE, Oudiz RJ, Wasserman K. Exercise pathophysiology in patients with primary pulmonary hypertension. Circulation. 2001;104:429–35. doi: 10.1161/hc2901.093198. [DOI] [PubMed] [Google Scholar]
- 4.Moosavi SA, Raji H, Faghankhani M, Yazdani R, Esmaeili M. Evaluation of the effects of atorvastatin on the treatment of secondary pulmonary hypertension due to chronic obstructive pulmonary diseases: A randomized controlled trial. Iran Red Crescent Med J. 2013;15:649–54. doi: 10.5812/ircmj.8267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McGoon M, Gutterman D, Steen V, Barst R, McCrory DC, Fortin TA, et al. Screening, early detection, and diagnosis of pulmonary arterial hypertension: ACCP evidence-based clinical practice guidelines. Chest. 2004;126(1 Suppl):14S–34S. doi: 10.1378/chest.126.1_suppl.14S. [DOI] [PubMed] [Google Scholar]
- 6.Minai OA, Chaouat A, Adnot S. Pulmonary hypertension in COPD: Epidemiology, significance, and management: Pulmonary vascular disease: The global perspective. Chest. 2010;137(6 Suppl):39S–51S. doi: 10.1378/chest.10-0087. [DOI] [PubMed] [Google Scholar]
- 7.McLaughlin VV, Presberg KW, Doyle RL, Abman SH, McCrory DC, Fortin T, et al. Prognosis of pulmonary arterial hypertension: ACCP evidence-based clinical practice guidelines. Chest. 2004;126(1 Suppl):78S–92S. doi: 10.1378/chest.126.1_suppl.78S. [DOI] [PubMed] [Google Scholar]
- 8.Jain MK, Ridker PM. Anti-inflammatory effects of statins: Clinical evidence and basic mechanisms. Nat Rev Drug Discov. 2005;4:977–87. doi: 10.1038/nrd1901. [DOI] [PubMed] [Google Scholar]
- 9.Barreto AC, Maeda NY, Soares RP, Cícero C, Lopes AA. Rosuvastatin and vascular dysfunction markers in pulmonary arterial hypertension: A placebo-controlled study. Braz J Med Biol Res. 2008;41:657–63. doi: 10.1590/s0100-879x2008000800003. [DOI] [PubMed] [Google Scholar]
- 10.Kawut SM, Bagiella E, Lederer DJ, Shimbo D, Horn EM, Roberts KE, et al. Randomized clinical trial of aspirin and simvastatin for pulmonary arterial hypertension: ASA-STAT. Circulation. 2011;123:2985–93. doi: 10.1161/CIRCULATIONAHA.110.015693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee TM, Chen CC, Shen HN, Chang NC. Effects of pravastatin on functional capacity in patients with chronic obstructive pulmonary disease and pulmonary hypertension. Clin Sci (Lond) 2009;116:497–505. doi: 10.1042/CS20080241. [DOI] [PubMed] [Google Scholar]
- 12.Kao PN. Simvastatin treatment of pulmonary hypertension: An observational case series. Chest. 2005;127:1446–52. doi: 10.1378/chest.127.4.1446. [DOI] [PubMed] [Google Scholar]
- 13.Girgis R. Statin therapy in pulmonary hypertension. PVRI Rev. 2009;1:199. [Google Scholar]
- 14.Anand V, Garg S, Duval S, Thenappan T. A systematic review and meta-analysis of trials using statins in pulmonary arterial hypertension. Pulm Circ. 2016;6:295–301. doi: 10.1086/687304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMC Med. 2010;8:1. doi: 10.4103/0976-500X.72352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Celli BR, MacNee W. ATS/ERS Task Force. Standards for the diagnosis and treatment of patients with COPD: A summary of the ATS/ERS position paper. Eur Respir J. 2004;23:932–46. doi: 10.1183/09031936.04.00014304. [DOI] [PubMed] [Google Scholar]
- 17.Liao JK, Laufs U. Pleiotropic effects of statins. Annu Rev Pharmacol Toxicol. 2005;45:89–118. doi: 10.1146/annurev.pharmtox.45.120403.095748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nishimura T, Vaszar LT, Faul JL, Zhao G, Berry GJ, Shi L, et al. Simvastatin rescues rats from fatal pulmonary hypertension by inducing apoptosis of neointimal smooth muscle cells. Circulation. 2003;108:1640–5. doi: 10.1161/01.CIR.0000087592.47401.37. [DOI] [PubMed] [Google Scholar]
- 19.Wilkins MR, Ali O, Bradlow W, Wharton J, Taegtmeyer A, Rhodes CJ, et al. Simvastatin as a treatment for pulmonary hypertension trial. Am J Respir Crit Care Med. 2010;181:1106–13. doi: 10.1164/rccm.2009111-699OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carlin CM, Celnik DF, Pak O, Wadsworth R, Peacock AJ, Welsh DJ. Low-dose fluvastatin reverses the hypoxic pulmonary adventitial fibroblast phenotype in experimental pulmonary hypertension. Am J Respir Cell Mol Biol. 2012;47:140–8. doi: 10.1165/rcmb.2011-0411OC. [DOI] [PubMed] [Google Scholar]
- 21.Zeng WJ, Xiong CM, Zhao L, Shan GL, Liu ZH, Xue F, et al. Atorvastatin in pulmonary arterial hypertension (APATH) study. Eur Respir J. 2012;40:67–74. doi: 10.1183/09031936.00149011. [DOI] [PubMed] [Google Scholar]
- 22.Barbera J, Peinado V, Santos S. Pulmonary hypertension in chronic obstructive pulmonary disease. Eur Respir J. 2003;21:892–905. doi: 10.1183/09031936.03.00115402. [DOI] [PubMed] [Google Scholar]
- 23.Barberà JA, Blanco I. Pulmonary hypertension in patients with chronic obstructive pulmonary disease: Advances in pathophysiology and management. Drugs. 2009;69:1153–71. doi: 10.2165/00003495-200969090-00002. [DOI] [PubMed] [Google Scholar]
- 24.Shujaat A, Bajwa AA, Cury JD. Pulmonary hypertension secondary to COPD. Pulm Med. 2012;2012:203952. doi: 10.1155/2012/203952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tello A, Marín F, Roldán V, García-Herola A, Lorenzo S, Climent VE, et al. Effect of maximum dose of atorvastatin on inflammation, thrombogenesis and fibrinolysis in high-risk patients with ischemic heart disease. Rev Esp Cardiol. 2005;58:934–40. [PubMed] [Google Scholar]
- 26.Mannino DM, Thorn D, Swensen A, Holguin F. Prevalence and outcomes of diabetes, hypertension and cardiovascular disease in COPD. Eur Respir J. 2008;32:962–9. doi: 10.1183/09031936.00012408. [DOI] [PubMed] [Google Scholar]
- 27.Cao C, Wu Y, Xu Z, Lv D, Zhang C, Lai T, et al. The effect of statins on chronic obstructive pulmonary disease exacerbation and mortality: A systematic review and meta-analysis of observational research. Sci Rep. 2015;5:16461. doi: 10.1038/srep16461. [DOI] [PMC free article] [PubMed] [Google Scholar]


