Abstract
Objectives: We examined associations of physical intimate partner violence (PIPV) with selected mental health disorders using a nationally representative sample of emergency department (ED) discharges corresponding to men and women (18–64 years) from the 2010 Nationwide Emergency Department Sample.
Methods: PIPV was determined using International Classification of Disease, 9th Revision, Clinical Modification (ICD-9-CM) external cause of injury code E967.3 (battering by spouse or partner). ICD-9-CM clinical classification of discharge diagnoses was used to identify mental health disorders. Multivariable logistic regression models were constructed to estimate adjusted odds ratios (ORadj) and their 95% confidence intervals (CIs).
Results: PIPV prevalence was estimated at 0.36 per 1000 ED discharges. The strongest correlates of PIPV were alcohol-related (ORadj = 3.02, 95% CI: 2.62–3.50), adjustment (ORadj = 2.37, 95% CI: 1.56–3.58), intentional self-harm (ORadj = 1.41, 95% CI: 1.05–1.89), anxiety (ORadj = 1.23, 95% CI: 1.07–1.40), drug-related (ORadj = 1.22, 95% CI: 1.01–1.47), and mood (ORadj = 1.16, 95% CI: 1.04–1.31) disorders. PIPV's association with alcohol-related disorders was stronger among women (ORadj = 3.22, 95% CI: 2.79–3.72) versus men (ORadj = 1.98, 95% CI: 1.42–2.77). Similarly, drug-related disorders were stronger correlates of PIPV among women (ORadj = 1.32, 95% CI: 1.09–1.60) versus men (ORadj = 0.59, 95% CI: 0.31–1.16).
Conclusions: In EDs, PIPV was linked to several mental health disorders, with women experiencing comorbid PIPV and substance use more frequently than men.
Keywords: : intimate partner violence, mental health, emergency department, surveillance
Introduction
Intimate partner violence (IPV) is a pattern of assaultive and coercive behaviors in intimate relationships1–3 and an issue of public health importance. The Centers for Disease Control and Prevention defines IPV as “physical violence, sexual violence, threats of physical/sexual violence, and psychological/emotional abuse perpetrated by a current or former spouse, common-law spouse, nonmarital dating partners, or boyfriends/girlfriends of the same or opposite sex.”4,5 Previous studies have linked IPV to a wide range of adverse health consequences, including injury,3,6–8 chronic pain,9,10 gastrointestinal disorders,11–13 sexually transmitted diseases,14–17 disability,18,19 poor pregnancy outcomes,20 substance abuse,21–23 depression,24,25 post-traumatic stress disorder (PTSD),26,27 and death.28
Clearly, a gender gap exists in susceptibility to violence in general and IPV in particular, with most national surveys suggesting higher IPV rates in women versus men.3,29,30
Based on the National Violence against Women Survey conducted through telephone interviews of 8000 women and 8000 men, nearly 25% of women and 7.6% of men disclosed rape and/or physical assault by a current or former spouse, cohabiting partner, or date at least once during their lifetime.29 In addition, 1.5% of women (representing 1.5 million women) and 0.9% of men (representing 834,732 men) said that they were raped and/or physically assaulted by a partner in the previous 12 months.29 Finally, nearly 5% of women and 0.6% of men reported being stalked by an intimate partner during their lifetime. In addition, 0.5% of women (representing 503,485 women) and 0.2% of men (representing 185,496 men) were stalked by an intimate partner in the past year.29
Although both sexes are involved in IPV and experience IPV-related health outcomes,31,32 researchers have traditionally focused on physical and nonphysical forms of violence perpetrated by a male partner against a female victim.1,33 In the general population, lifetime prevalence of IPV against women has been estimated at 22%,3,34–36 with physical violence affecting 17%–34% and nonphysical violence affecting 12%–35% of women.37–39 Among women identified in primary care or emergency departments (EDs), 37%–50% reported lifetime physical violence and 36%–72% lifetime nonphysical violence, with 10%–18% reporting physical violence and 28%–44% reporting nonphysical violence in the past year.40–44 Women with a history of IPV were shown to utilize healthcare services (including primary care and EDs) for injuries and physical and mental health problems nearly twice as often as women with no history of IPV,37,45,46 highlighting opportunities for IPV screening by healthcare providers. The Centers for Disease Control and Prevention estimates annual IPV-related costs among women at $5.8 billion (with $4.0 billion in healthcare costs).45,47 Based on the Medical Expenditure Panel Survey and the National Violence Against Women Survey, it is estimated that $2.4 billion in medical costs are attributable to physical assault and $1.6 million in medical costs are attributable to rape against women by an intimate partner.37,48
Routine screening for identification and treatment of IPV by healthcare providers can potentially reduce the burden of IPV and its associated health problems on individuals, families, the healthcare system, and society as a whole.40 According to the US Preventive Services Task Force (USPSTF), high-quality evidence supporting IPV screening in primary care and EDs as a safe and effective strategy for the prevention of IPV and its associated health outcomes remains inconclusive40,49 with recently conducted intervention trials yielding inconsistent findings.50–77 While the USPSTF and other organizations have recommended screening of reproductive aged women for IPV in various healthcare settings,31 the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) requires all EDs to have policies and procedures in place for IPV screening and patients who disclose IPV can be treated or referred to services, which address healthcare needs associated with IPV.45
Despite the JCAHO mandate, less than half of US EDs report having policies and procedures in place for IPV screening, and even fewer EDs regularly ask about mental health problems in women identified as IPV victims.40,45,78 A bidirectional association31 has been previously suggested between IPV history and costly mental health problems45 such as symptoms of depression,79–81 PTSD,82,83 suicidality,84–86 and substance abuse.87–89 In a recent study of women enrolled in the Group Health Cooperative, IPV exposure was specifically linked to excessive utilization of mental health services.11,37 Comorbid mental health problems can adversely impact the success of IPV interventions and often present at EDs rather than specialized centers while being underdiagnosed by ED healthcare providers.45
Successful screening interventions require a better understanding of what mental health symptoms and diagnoses are frequently encountered in patients with a history of IPV, for the purpose of referral to on-site and off-site services. Although a growing body of the literature has evaluated mental health outcomes of IPV in both sexes,38,90–95 previous studies were predominantly focused on women and little is known about sex-specific mental health outcomes of IPV. Limited evidence suggests that men and women respond differently to IPV exposure and that IPV-related mental healthcare needs may be sex specific.1,96 To our knowledge, no published studies have examined overall and sex-specific utilization of healthcare services linking physical IPV (PIPV) to mental health diagnoses, using a nationally representative sample of ED discharges.
The purpose of this population-based cross-sectional study is to examine these relationships among male and female adult patients, 18–64 years of age, whose medical records were included in the 2010 Healthcare Cost and Utilization Project's (HCUP) Nationwide Emergency Department Sample (NEDS). The study aims to identify whether there are sex differences in patterns of PIPV-related mental health problems in the ED setting.
Materials and Methods
Study design and setting
Sponsored by the Agency for Healthcare Research and Quality, the HCUP consists of publicly available databases and software tools created as a federal-state-industry partnership to support decision-making. NEDS is the largest all-payer ED database in the United States, yielding national and regional estimates of hospital-based ED visits, with data on ∼30 million discharges representing ∼130 million ED visits each year. Since 2006, the NEDSs were selected from the American Hospital Association community, nonrehabilitation hospitals participating in the State Inpatient Databases (patients initially seen in the ED and then admitted to the same hospital), and State Emergency Department Databases (ED treat-and-release visits or transfers to another hospital) and include information on geographic, hospital, and patient characteristics, as well as the nature of the visits.
For the latest available time period (January 1 to December 31, 2010), NEDS data were compiled from 961 hospitals located in 28 participating states (AZ, CA, CT, FL, GA, HI, IA, IL, IN, KS, KY, MA, MD, MN, MO, NC, NE, NJ, NV, NY, OH, RI, SC, SD, TN, UT, VT, and WI), representing a 20% stratified sample of US EDs. Stratification was based on five characteristics as follows: geographic region (Northeast, Midwest, South, and West), trauma center designation (trauma level I, II, III, and nontrauma), hospital urban–rural location (large metropolitan, small metropolitan, micropolitan, and nonurban residual), teaching status (teaching and nonteaching), and ownership (public, for-profit, and not-for-profit). The database includes clinical and resource information during ED visits, encompassing demographic information, admissions, injuries, diagnoses (up to 15), payment source, total hospital charges for inpatient stays of ED visits that result in admission, procedures categorized according to the International Classification of Disease, 9th Revision, Clinical Modification (ICD-9-CM), and the Current Procedural Terminology, as well as death in ED, if present.
Selection of participants
ED discharges corresponding to adult patients, between 18 and 64 years of age, who sought healthcare at EDs for various reasons, including injuries, were selected from the 2010 HCUP NEDS. Accordingly, the study sample consists of 81,386,155 weighted discharges (with a mean ± standard error age of 39.5 ± 0.06 years for men and 37.6 ± 0.07 years for women). After identifying PIPV cases, a 10% simple random sample of the non-IPV group was selected as a control group due to computational limitations. A second 10% simple random sample was also selected to confirm the results.
Measures
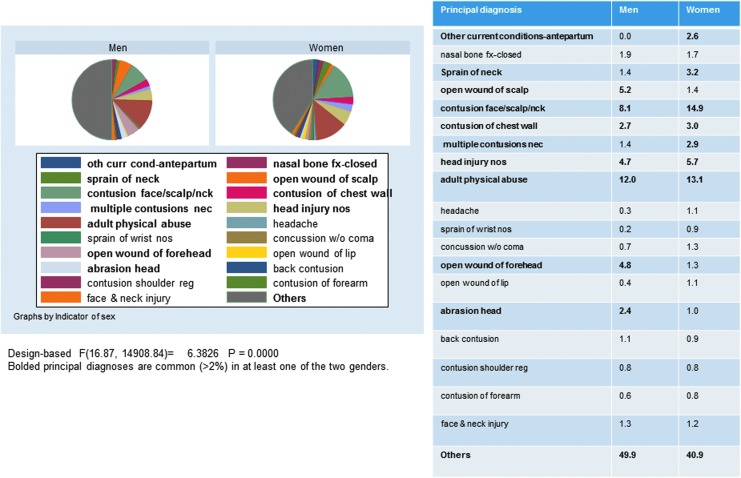
ED discharges with an ICD-9-CM external cause of injury code (ECODE1–ECODE4) of E967.3 (battering by spouse or partner) were identified as a PIPV discharge since the patient had experienced PIPV. Due to the multitude of IPV screening tools, a gold standard for diagnosing PIPV in an ED setting is yet to be identified, limiting our ability to assess the sensitivity and specificity of ICD-9-CM codes in the context of PIPV. Furthermore, ICD-9-CM clinical classification category codes (DXCCS1–DXCCS15) were used to identify ED discharges whereby the patient had been diagnosed with the following mental health problems: (1) 650 adjustment disorders; (2) 651 anxiety disorders; (3) 652 attention-deficit, conduct, and disruptive behavior disorders; (4) 655 disorders usually diagnosed in infancy, childhood, or adolescence, including pervasive development disorders, tic disorders, and elimination disorders; (5) 656 impulse control disorders, not elsewhere classified; (6) 657 mood disorders; (7) 658 personality disorders; (8) 659 schizophrenia and other psychotic disorders; (9) 660 alcohol-related disorders; (10) 661 drug-related disorders; (11) 662 intentional self-harm/suicide and intentional self-inflicted injury; (12) 670 miscellaneous disorders, including eating disorders, mental disorders in pregnancy, dissociative disorders, factitious disorders, sleep disorders, and somatoform disorders. Each mental health problem was examined as a separate dichotomous outcome and all mental health problems were combined as one dichotomous outcome. Hospital and patient characteristics were included as covariates in the models. Hospitals were characterized by region, urban or rural location, trauma center designation, teaching status, and ownership/control, and patients were characterized by gender, age in years (18–24, 25–29, 30–34, 35–39, 40–44, 45–49, 50–54, 55–59, and 60–64), and household socioeconomic status in quartiles as denoted by the patient's zip code. In addition, the principal diagnosis was ranked among PIPV cases, and the most common 19 diagnoses with a 20th category labelled as “Others” were presented and compared between men and women in terms of relative proportion. Based on Figure 1, the most common principal diagnoses among men (aside from the “Others” category) were “adult physical abuse” (12.0%), followed by “contusion of face/scalp/neck” (8.1%), and “open wound of the scalp” (5.2%), with similar proportions obtained for “head injury” (4.7%) and “open wound of forehead” (4.8%). Among women, “contusion of face/scalp/neck” (14.9%) was more prevalent than “adult physical abuse” (13.1%), which was followed by “head injury” (5.7%). The following ICD-9-CM codes were identified as the most prevalent primary diagnoses classified in the “Others” category: “Cervicalgia” [7231] (1.79%), “Sprain of shoulder or arm not otherwise specified” [8409] (1.41%), “Sprain of hand not otherwise specified” [84210] (1.60%), “Concussion with coma not otherwise specified” [8505] (1.33%), “Concussion not otherwise specified” [8509] (1.29%), “Open wound of hand” [8820] (1.18%), “Abrasion NEC” [9190] (1.33%), “Contusion of abdominal wall” [9222] (1.29%), “Contusion of hands” [92320] (1.75%), “Contusion not otherwise specified” [9249] (1.22%), and “Adult sexual abuse” [99583] (1.60%). The distribution of principal diagnoses differed markedly by gender (p < 0.001, design-based F-test).
FIG. 1.
Distribution of principal diagnoses (19 most common overall) by sex; NEDS 2010. NEDS, Nationwide Emergency Department Sample. Color images available online at www.liebertpub.com/jwh
Statistical analyses
All statistical analyses were conducted using STATA version 14 (STATA Corp, College Station, TX). Summary statistics included prevalence proportions of PIPV and mental disorders, accounting for sampling design complexity, as well as weighted totals. Prevalence of PIPV was estimated overall and within strata of hospital- and patient-level categorical variables. Among IPV cases, men and women were compared in terms of principal diagnosis proportionate distribution. Comparisons between categorical variables were done using design-based F-tests. Moreover, we examined differences in the prevalence of specific and overall mental health diagnoses by PIPV status. Those analyses were conducted on the entire sample of eligible discharges (18–64 years, Weighted N = 81,386,155). Using PIPV cases and the 10% sample of controls from the non-IPV subgroup, multivariable logistic regression models were constructed to examine PIPV as a predictor of mental health diagnoses, adjusting for potential confounders. Finally, using the same 10% subsample of controls and the full sample of PIPV cases, we performed sex-specific analyses to evaluate whether observed associations differed according to sex, while examining interaction effects. A second 10% sample of non-PIPV controls (Control B) was also selected and the results were contrasted with those of the first 10% subsample (Control A). All analyses were performed taking into account the single-stage cluster sampling design, through STATA's svy commands. Two-sided statistical tests were conducted at an alpha level of 0.05.
Results
The overall prevalence of PIPV in the study sample was estimated to be 36 per 100,000 (unweighted n = 6342) ED discharges. Furthermore, variations in PIPV prevalence were observed according to US hospital region, patient sex, and age (p < 0.0001), but not according to hospital urban–rural location, trauma center designation, teaching status, ownership, or household socioeconomic status. The estimated PIPV prevalence was higher among female (57 per 100,000) versus male (6 per 100,000) patients; also, PIPV prevalence was highest among patients 25–34 years of age and in the Western region of the United States (Table 1).
Table 1.
Prevalence of Physical Intimate Partner Violence by Hospital and Patient Characteristics: National Emergency Department Surveillance System, 2010
| PIPV | |||||
|---|---|---|---|---|---|
| Per 1000 | SEM | Na | p | n (%) | |
| US hospital region | ≤0.0001 | ||||
| Northeast | 0.33 | 0.027 | 15824906 | 3319673 (18.43) | |
| Midwest | 0.44 | 0.040 | 19263930 | 3780021 (20.98) | |
| South | 0.25 | 0.010 | 32447377 | 7921059 (43.97) | |
| West | 0.50 | 0.41 | 13849942 | 2995563 (16.63) | |
| Urban–rural location of hospital | 0.05 | ||||
| Urban | 0.36 | 0.02 | 65033243 | 14650341 (81.97) | |
| Rural | 0.34 | 0.028 | 15712682 | 3222578 (18.03) | |
| Trauma center designation | 0.07 | ||||
| I | 0.32 | 0.050 | 8183904 | 1,773,540 (9.84) | |
| II | 0.31 | 0.047 | 6725408 | 1,403,132 (7.79) | |
| III | 0.40 | 0.070 | 6028840 | 903,716 (5.02) | |
| IV | 0.34 | 0.017 | 51798076 | 12,227,040 (67.87) | |
| Unknown | 0.48 | 0.062 | 8650724 | 1,708,888 (9.49) | |
| Teaching status | 0.07 | ||||
| Teaching | 0.36 | 0.026 | 33000946 | 6891422 (38.25) | |
| Nonteaching | 0.36 | 0.019 | 48385209 | 11124894 (61.75) | |
| Hospital ownership | 0.08 | ||||
| Public | 0.36 | 0.048 | 5006202 | 1443595 (8.01) | |
| For-profit | 0.27 | 0.029 | 6766859 | 2108070 (11.70) | |
| Not-for-profit | 0.32 | 0.033 | 12131169 | 2966645 (16.47) | |
| Unknown | 0.37 | 0.02 | 57481926 | 11498006 (63.82) | |
| Patient sex | ≤0.0001 | ||||
| Male | 0.059 | 0.0048 | 34976225 | 7707160 (42.78) | |
| Female | 0.57 | 0.025 | 46403852 | 10307844 (57.22) | |
| Patient age | ≤0.0001 | ||||
| 18–24 | 0.36 | 0.022 | 15752761 | 3479906 (19.54) | |
| 25–29 | 0.51 | 0.026 | 10728068 | 2374613 (13.33) | |
| 30–34 | 0.51 | 0.027 | 9252674.4 | 2054059 (11.53) | |
| 35–39 | 0.46 | 0.026 | 8287384.9 | 1844129 (10.35) | |
| 40–44 | 0.39 | 0.021 | 8279463.2 | 1840578 (10.33) | |
| 45–49 | 0.33 | 0.018 | 8804093.6 | 1949154 (10.94) | |
| 50–54 | 0.22 | 0.015 | 8160947 | 1802042 (10.12) | |
| 55–59 | 0.13 | 0.010 | 6603734.8 | 1454022 (8.16) | |
| 60–64 | 0.087 | 0.0069 | 4584215.5 | 1011418 (5.68) | |
| Household socioeconomic status | 0.1 | ||||
| Quartile 1 | 0.37 | 0.024 | 27604238 | 6064435 (34.54) | |
| Quartile 2 | 0.36 | 0.017 | 22100992 | 4872582 (27.75) | |
| Quartile 3 | 0.36 | 0.024 | 16898112 | 3790665 (21.59) | |
| Quartile 4 | 0.30 | 0.025 | 12713731 | 2831135 (16.12) | |
| Total | 0.36 | 0.015 | 81386155 | 17558817 (100.00) | |
Weighted sample size; weighted number of PIPV cases in 2010 NEDS, n = 28,970.
NEDS, Nationwide Emergency Department Sample; PIPV, physical intimate partner violence; SEM, standard error of the mean.
Overall, PIPV was positively and significantly associated with the presence of any mental health diagnosis, either before (odds ratio [OR] = 1.19, 95% confidence interval [CI]: 1.09–1.32) or after (OR = 1.35, 95% CI: 1.23–1.48) adjustment for confounders. However, the magnitude and direction of the association differed according to the specific mental health disorder. In multivariable models, the strongest positive associations pertained to alcohol-related (OR = 3.02, 95% CI: 2.62–3.50) and adjustment (OR = 2.37, 95% CI: 1.56–3.58) disorders, followed by intentional self-harm, suicide, and intentional self-inflicted injury (OR = 1.41, 95% CI: 1.05–1.89), anxiety disorders (OR = 1.23, 95% CI: 1.07–1.40), drug-related disorders (OR = 1.22, 95% CI: 1.01–1.47), and mood disorders (OR = 1.16, 95% CI: 1.04–1.31). By contrast, PIPV was not significantly associated with disorders usually diagnosed in infancy, childhood, or adolescence, attention-deficit, conduct, and disruptive behavior disorders or personality disorders. Interestingly, a significant but negative association was noted between PIPV and schizophrenia and other psychotic disorders (OR = 0.49, 95% CI: 0.35–0.71) (Table 2).
Table 2.
Physical Intimate Partner Violence As a Predictor of Selected Mental Health Disorders Before and After Adjustment for Hospital and Patient Characteristics: National Emergency Department Surveillance System, 2010
| % (SEM) | OR (95% CI) | |||
|---|---|---|---|---|
| Non-PIPV | PIPV | Unadjusted | Adjusted | |
| Adjustment disorders | 0.21 (0.013) | 0.47 (0.11) | 2.28 (1.50–3.49) | 2.37 (1.56–3.58) |
| Anxiety disorders | 4.05 (0.078) | 5.32 (0.37) | 1.32 (1.16–1.51) | 1.23 (1.07–1.40) |
| Attention-deficit, conduct, and disruptive behavior disorders | 0.35 (0.013) | 0.25 (0.074) | 0.73 (0.42–1.29) | 0.85 (0.48–1.52) |
| Disorders usually diagnosed in infancy, childhood, or adolescence, including pervasive development disorders, tic disorders, and elimination disorders | 0.059 (0.0019) | 0.014 (0.014) | 0.24 (0.03–1.68) | 0.41 (0.059–2.88) |
| Impulse control disorders, not elsewhere classified | 0.036 (0.0028) | — | — | — |
| Mood disorders | 6.38 (0.15) | 7.57 (0.47) | 1.19 (1.06–1.35) | 1.16 (1.04–1.31) |
| Personality disorders | 0.28 (0.017) | 0.19 (0.057) | 0.68 (0.38–1.21) | 0.59 (0.33–1.11) |
| Schizophrenia and other psychotic disorders | 1.41 (0.044) | 0.57 (0.10) | 0.39 (0.28–0.56) | 0.49 (0.35–0.71) |
| Alcohol-related disorders | 3.65 (0.079) | 5.88 (0.40) | 1.65 (1.43–1.89) | 3.02 (2.62–3.50) |
| Drug-related disorders | 3.03 (0.069) | 2.99 (0.28) | 0.98 (0.81–1.17) | 1.22 (1.01–1.47) |
| Intentional self-harm/suicide and intentional self-inflicted injury | 0.81 (0.027) | 0.98 (0.14) | 1.19 (0.89–1.59) | 1.41 (1.05–1.89) |
| Miscellaneous disorders, including eating disorders, mental disorders in pregnancy, dissociative disorders, factitious disorders, sleep disorders, and somatoform disorders | 0.38 (0.0091) | 0.41 (0.077) | 1.11 (0.78–1.59) | 0.79 (0.56–1.14) |
| Overall | 15.0 (0.22) | 17.5 (0.73) | 1.19 (1.09–1.32) | 1.35 (1.23–1.48) |
CI, confidence interval; OR, odds ratio.
Finally, we examined interactions between PIPV and sex in relation to the selected mental health disorders (Table 3). With the exception of alcohol- and drug-related disorders, there were no significant interactions whereby the magnitude or direction of associations between PIPV and mental health disorders differed between men and women. For alcohol-related disorders, the association with PIPV was stronger among women (adjusted OR = 3.22, 95% CI: 2.79–3.72) compared to men (adjusted OR = 1.98, 95% CI: 1.42–2.77). Similarly, drug-related disorders were significantly related to PIPV among women (adjusted OR = 1.32, 95% CI: 1.09–1.60) but not among men (adjusted OR = 0.59, 95% CI: 0.31–1.16). Results using Control B (10% sample) of the non-PIPV subgroup resulted in virtually identical estimates of OR for PIPV versus mental health outcomes as in the Control A (10% sample) in all multiple logistic regression models.
Table 3.
Physical Intimate Partner Violence As a Predictor of Mental Health Disorders Before and After Adjustment for Hospital and Patient Characteristics, Overall and According to Sex: National Emergency Department Surveillance System, 2010
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Overall | ||||
| Male | 1.26 | 0.98–1.62 | 1.26 | 0.97–1.63 |
| Female | 1.32 | 1.20–1.45 | 1.38 | 1.26–1.51 |
| Sex × PIPV | p = 0.33 | |||
| Adjustment disorders | ||||
| Male | 3.37 | 0.88–12.83 | 3.50 | 1.00–12.27 |
| Female | 2.31 | 1.52–3.53 | 2.29 | 1.50–3.50 |
| Sex × PIPV | p = 0.51 | |||
| Anxiety disorders | ||||
| Male | 1.06 | 0.66–1.72 | 1.07 | 0.66–1.73 |
| Female | 1.21 | 1.05–1.38 | 1.25 | 1.09–1.43 |
| Sex × PIPV | p = 0.57 | |||
| Attention-deficit, conduct, and disruptive behavior disorders | ||||
| Male | 0.73 | 0.17–3.20 | 0.56 | 0.82–3.89 |
| Female | 0.89 | 0.49–1.65 | 0.89 | 0.49–1.65 |
| Sex × PIPV | p = 0.66 | |||
| Disorders usually diagnosed in infancy, childhood, or adolescence, including pervasive development disorders, tic disorders, and elimination disorders | ||||
| Male | 1.98 | 0.28–13.83 | 2.02 | 0.29–14.14 |
| Female | — | — | — | — |
| Sex × PIPV | — | |||
| Impulse control disorders, not elsewhere classified | ||||
| Male | — | — | — | — |
| Female | — | — | — | — |
| Sex × PIPV | — | |||
| Mood disorders | ||||
| Male | 0.99 | 0.64–1.54 | 1.02 | 0.65–1.58 |
| Female | 1.11 | 0.99–1.26 | 1.19 | 1.05–1.34 |
| Sex × PIPV | p = 0.55 | |||
| Personality disorders | ||||
| Male | — | — | — | — |
| Female | 0.74 | 0.41–1.32 | 0.65 | 0.35–1.18 |
| Sex × PIPV | — | |||
| Schizophrenia and other psychotic disorders | ||||
| Male | 0.54 | 0.22–1.32 | 0.53 | 0.22–1.29 |
| Female | 0.51 | 0.35–0.75 | 0.52 | 0.35–0.77 |
| Sex × PIPV | p = 0.83 | |||
| Alcohol-related disorders | ||||
| Male | 1.94 | 1.42–2.66 | 1.98 | 1.42–2.77 |
| Female | 3.13 | 2.72–3.63 | 3.22 | 2.79–3.72 |
| Sex × PIPV | p = 0.002 | |||
| Drug-related disorders | ||||
| Male | 0.66 | 0.35–1.23 | 0.59 | 0.31–1.16 |
| Female | 1.40 | 1.17–1.69 | 1.32 | 1.09–1.60 |
| Sex × PIPV | p = 0.02 | |||
| Intentional self-harm/suicide and intentional self-inflicted injury | ||||
| Male | 1.37 | 0.55–3.42 | 1.42 | 0.57–3.52 |
| Female | 1.48 | 1.09–1.98 | 1.41 | 1.04–1.90 |
| Sex × PIPV | p = 0.99 | |||
| Miscellaneous disorders, including eating disorders, mental disorders in pregnancy, dissociative disorders, factitious disorders, sleep disorders, and somatoform disorders | ||||
| Male | — | — | — | — |
| Female | 0.87 | 0.61–1.25 | 0.81 | 0.57–1.17 |
| Sex × PIPV | — | |||
Discussion
To the best of our knowledge, this is the first population-based cross-sectional study to examine sex-specific associations between PIPV and mental health diagnoses, using a nationally representative sample of ED discharges. Our results suggested that PIPV was positively associated with specific diagnoses, namely, alcohol-related, adjustment, intentional self-harm, suicide, intentional self-inflicted injury, anxiety, and drug-related and mood disorders, and negatively associated with schizophrenia and other psychotic disorders. In addition, alcohol-related and drug-related disorders were more strongly associated with PIPV among women than among men.
Our results should be interpreted with caution and in light of several limitations that arise from the use of deidentified databases. First, little data could be gleaned from HCUP NEDS regarding clinical presentation and since our study included only ED patients, physicians may not have been aware of relevant patient experiences, due to the urgency of events. This may explain the paucity of secondary diagnostic codes available for each patient. Furthermore, race was not included as a data element in the HCUP NEDS, precluding the evaluation of racial disparities in PIPV. Second, the HCUP NEDS database consists of discharge records whereby multiple observations may be attributed to an individual patient. Given the nature of PIPV, the likelihood of repeat ED visits for each individual patient may be substantial, but cannot be ascertained in HCUP NEDS. Third, the cross-sectional design precludes examination of temporal or causal relationships between PIPV and various mental health problems. Fourth, the quality and completeness of HCUP NEDS data depend on existing medical records, which may result in misclassification and residual confounding biases. Of note, PIPV is typically underreported by patients and under identified by healthcare providers, suggesting a high false negative rate and underestimation of PIPV prevalence.97 More importantly, patients experiencing IPV were identified based on ICD-9-CM codes, which do not take into account psychological forms of violence that often co-occur with physical and sexual forms of violence based on the CDC definition, especially among patients diagnosed with mental health disorders. Accordingly, IPV prevalence estimates are substantially lower in the NEDS population compared to estimates from general and clinical population surveys. For instance, previously conducted surveys in ED settings have estimated 2%–7% annual prevalence rates of IPV.98 Similar validity issues are encountered with respect to PIPV and mental health disorders based on ICD-9-CM, whereby date of diagnosis is unknown in NEDS. In addition, the hypothesized relationship between PIPV and mental health disorders may be confounded by patient and hospital characteristics that were not assessed in the HCUP NEDS. Nevertheless, administrative databases are ideal for providing a large patient sample with sufficient power to detect uncommon occurrences, including mental health diagnoses.
PIPV is a significant public health concern that has been linked to increased risk of a variety of mental health problems, including depression,24,81,99,100 alcohol abuse,101,102 substance use,102 suicidality,103 and PTSD.104 Although the majority of PIPV research has focused primarily on women,105 it was found that men also experience mental health problems associated with PIPV.103,106 It is estimated that more than half of PIPV events are not reported to the police,107 suggesting the need for intervention efforts aimed outside the realm of law enforcement. Healthcare providers, particularly those working within ED settings, can serve as an important point of contact for victims of PIPV. Although PIPV is common among patients presenting to EDs,108,109 screening and identification for PIPV by healthcare providers are low.109
Considering that intervention for mental health problems related to PIPV may reduce the risk of revictimization,110 it is important for healthcare providers to appropriately address these issues in addition to screening for PIPV among both men and women seeking healthcare in EDs. Furthermore, despite consistent findings suggesting an association between PIPV and mental health problems, few studies81 have examined the relationship between PIPV and diagnosed mental disorders. Specific mental health diagnoses may be important clues in identifying individuals at an increased risk of PIPV victimization or perpetration.
Previous research suggested sex differences in mental health problems related to PIPV, consistent with our study findings. Among victims of PIPV presenting to EDs, women tend to report more symptoms related to depression,96 PTSD, substance abuse, and alcohol use102 and men report symptoms related to depression,96,103 PTSD, and suicidality.103 Two study findings necessitate further elucidation. First, the inverse relationship between PIPV and psychoses may be explained by PIPV underreporting or absence of a partner in ED patients diagnosed with these mental health disorders. Second, in line with the concept that PIPV is a public health issue that cuts across all layers of society, PIPV prevalence did not differ significantly according to household socioeconomic status although it was linked to other hospital and patient characteristics.
Conclusions
In summary, PIPV in ED settings may be linked to a wide range of mental health disorders, with women experiencing comorbid PIPV and substance use disorders more frequently than men. Increased awareness of the connection between PIPV and mental health conditions may lead to better referrals or coordination of care. These sex-specific associations should be used to guide PIPV interventions in ED settings. More studies are needed to elucidate sex differences in the hypothesized relationships between IPV and mental health diagnoses in various healthcare settings.
Acknowledgments
This study was supported, in part, by the NIA/NIH/IRP in collaboration with Johns Hopkins University School of Medicine. The authors thank Ms. Nicolle Mode for her critical review of the article.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Rhodes KV, Houry D, Cerulli C, Straus H, Kaslow NJ, McNutt LA. Intimate partner violence and comorbid mental health conditions among urban male patients. Ann Fam Med 2009;7:47–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saltzman LE, Green YT, Marks JS, Thacker SB. Violence against women as a public health issue: Comments from the CDC. Am J Prev Med 2000;19:325–329 [DOI] [PubMed] [Google Scholar]
- 3.Tjaden PT, Thoennes N. Prevalence, incidence, and consequences of violence against women: Findings from the National Violence against Women Survey. In: Prevention, National Institute of Justice & Centers for Disease Control and Prevention, ed. Washington, DC, 1998 [Google Scholar]
- 4.Chang JC, Cluss PA, Ranieri L, et al. . Health care interventions for intimate partner violence: What women want. Womens Health Issues 2005;15:21–30 [DOI] [PubMed] [Google Scholar]
- 5.Saltzman LE, Fanslow JL, McMahon PM, Shelley GA. Intimate partner violence surveillance: Uniform definitions and recommended data elements, version 1.0. In: National Center for Injury Prevention and Control CfDCaP, ed. Atlanta, GA, 1999 [Google Scholar]
- 6.St Ivany A, Schminkey D. Intimate partner violence and traumatic brain injury: State of the science and next steps. Fam Community Health 2016;39:129–137 [DOI] [PubMed] [Google Scholar]
- 7.Walton-Moss BJ, Manganello J, Frye V, Campbell JC. Risk factors for intimate partner violence and associated injury among urban women. J Community Health 2005;30:377–389 [DOI] [PubMed] [Google Scholar]
- 8.Wu V, Huff H, Bhandari M. Pattern of physical injury associated with intimate partner violence in women presenting to the emergency department: A systematic review and meta-analysis. Trauma Violence Abuse 2010;11:71–82 [DOI] [PubMed] [Google Scholar]
- 9.Tiwari A, Fong DY, Chan CH, Ho PC. Factors mediating the relationship between intimate partner violence and chronic pain in Chinese women. J Interpers Violence 2013;28:1067–1087 [DOI] [PubMed] [Google Scholar]
- 10.Wuest J, Ford-Gilboe M, Merritt-Gray M, et al. . Pathways of chronic pain in survivors of intimate partner violence. J Womens Health (Larchmt) 2010;19:1665–1674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bonomi AE, Anderson ML, Reid RJ, Rivara FP, Carrell D, Thompson RS. Medical and psychosocial diagnoses in women with a history of intimate partner violence. Arch Intern Med 2009;169:1692–1697 [DOI] [PubMed] [Google Scholar]
- 12.Campbell JC. Health consequences of intimate partner violence. Lancet 2002;359:1331–1336 [DOI] [PubMed] [Google Scholar]
- 13.Wong J, Mellor D. Intimate partner violence and women's health and wellbeing: Impacts, risk factors and responses. Contemp Nurse 2014;46:170–179 [DOI] [PubMed] [Google Scholar]
- 14.Dude A. Intimate partner violence and increased lifetime risk of sexually transmitted infection among women in Ukraine. Stud Fam Plann 2007;38:89–100 [DOI] [PubMed] [Google Scholar]
- 15.Hess KL, Javanbakht M, Brown JM, Weiss RE, Hsu P, Gorbach PM. Intimate partner violence and sexually transmitted infections among young adult women. Sex Transm Dis 2012;39:366–371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Renzetti CM. Identified intimate partner violence (IPV) as a risk for women in contracting HIV/AIDS and other sexually transmitted disease. Violence Against Women 2013;19:811–813 [DOI] [PubMed] [Google Scholar]
- 17.Spiwak R, Afifi TO, Halli S, Garcia-Moreno C, Sareen J. The relationship between physical intimate partner violence and sexually transmitted infection among women in India and the United States. J Interpers Violence 2013;28:2770–2791 [DOI] [PubMed] [Google Scholar]
- 18.Breiding MJ, Armour BS. The association between disability and intimate partner violence in the United States. Ann Epidemiol 2015;25:455–457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hahn JW, McCormick MC, Silverman JG, Robinson EB, Koenen KC. Examining the impact of disability status on intimate partner violence victimization in a population sample. J Interpers Violence 2014;29:3063–3085 [DOI] [PubMed] [Google Scholar]
- 20.Sarkar NN. The impact of intimate partner violence on women's reproductive health and pregnancy outcome. J Obstet Gynaecol 2008;28:266–271 [DOI] [PubMed] [Google Scholar]
- 21.Brackley MH, Williams GB, Wei CC. Substance abuse interface with intimate partner violence: What treatment programs need to know. Nurs Clin North Am 2010;45:581–589, vi [DOI] [PubMed] [Google Scholar]
- 22.Fals-Stewart W, Kennedy C. Addressing intimate partner violence in substance-abuse treatment. J Subst Abuse Treat 2005;29:5–17 [DOI] [PubMed] [Google Scholar]
- 23.Gonzalez-Guarda RM, Florom-Smith AL, Thomas T. A syndemic model of substance abuse, intimate partner violence, HIV infection, and mental health among Hispanics. Public Health Nurs 2011;28:366–378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beydoun HA, Beydoun MA, Kaufman JS, Lo B, Zonderman AB. Intimate partner violence against adult women and its association with major depressive disorder, depressive symptoms and postpartum depression: A systematic review and meta-analysis. Soc Sci Med 2012;75:959–975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Daniels K. Intimate partner violence & depression: A deadly comorbidity. J Psychosoc Nurs Ment Health Serv 2005;43:44–51 [DOI] [PubMed] [Google Scholar]
- 26.Chan CH, Tiwari A, Fong DY, Ho PC. Post-traumatic stress disorder among Chinese women survivors of intimate partner violence: A review of the literature. Int J Nurs Stud 2010;47:918–925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Woods SJ. Intimate partner violence and post-traumatic stress disorder symptoms in women: What we know and need to know. J Interpers Violence 2005;20:394–402 [DOI] [PubMed] [Google Scholar]
- 28.Abrahams N, Jewkes R, Martin LJ, Mathews S, Vetten L, Lombard C. Mortality of women from intimate partner violence in South Africa: A national epidemiological study. Violence Vict 2009;24:546–556 [DOI] [PubMed] [Google Scholar]
- 29.Tjaden P, Thoennes N. Extent, nature, and consequences of intimate partner violence. In: Prevention, National Institute of Justice & Centers for Disease Control and Prevention, ed. 2000 [Google Scholar]
- 30.Rennison C, Welchans S. Intimate partner violence. In: NCJ 178247, ed. Washington, DC, 2000 [Google Scholar]
- 31.Choo EK, Benz M, Rybarczyk M, et al. . The intersecting roles of violence, gender, and substance use in the emergency department: A research agenda. Acad Emerg Med 2014;21:1447–1452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hackenberg EA, Sallinen V, Koljonen V, Handolin L. Severe intimate partner violence affecting both young and elderly patients of both sexes. Eur J Trauma Emerg Surg 2016. [In Press] [DOI] [PubMed] [Google Scholar]
- 33.Wathen CN, Jamieson E, Wilson M, et al. . Risk indicators to identify intimate partner violence in the emergency department. Open Med 2007;1:e113–e122 [PMC free article] [PubMed] [Google Scholar]
- 34.Rhodes KV, Kothari CL, Dichter M, Cerulli C, Wiley J, Marcus S. Intimate partner violence identification and response: Time for a change in strategy. J Gen Intern Med 2011;26:894–899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bachman R, Saltzman LE. Violence against women: Estimates from the redesigned study. In: US Department of Justice Bureau of Justice Statistics, ed. Vol Bureau of Justice Statistics Publication No. 154–348. Washington, DC, 1995 [Google Scholar]
- 36.Catalano SM. Criminal victimization, 2004. Data from the National Crime Victimization Survey. In: Bureau of Justice Statistics Office of Justice Programs, US Department of Justice, ed. Washington, DC, 2005 [Google Scholar]
- 37.Bonomi AE, Anderson ML, Rivara FP, Thompson RS. Health care utilization and costs associated with physical and nonphysical-only intimate partner violence. Health Serv Res 2009;44:1052–1067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Coker AL, Davis KE, Arias I, et al. . Physical and mental health effects of intimate partner violence for men and women. Am J Prev Med 2002;23:260–268 [DOI] [PubMed] [Google Scholar]
- 39.Thompson RS, Bonomi AE, Anderson M, et al. . Intimate partner violence: Prevalence, types, and chronicity in adult women. Am J Prev Med 2006;30:447–457 [DOI] [PubMed] [Google Scholar]
- 40.Gillum TL, Sun CJ, Woods AB. Can a health clinic-based intervention increase safety in abused women? Results from a pilot study. J Womens Health (Larchmt) 2009;18:1259–1264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bauer HM, Rodriguez MA, Perez-Stable EJ. Prevalence and determinants of intimate partner abuse among public hospital primary care patients. J Gen Intern Med 2000;15:811–817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dearwater SR, Coben JH, Campbell JC, et al. . Prevalence of intimate partner abuse in women treated at community hospital emergency departments. JAMA 1998;280:433–438 [DOI] [PubMed] [Google Scholar]
- 43.Kramer A, Lorenzon D, Mueller G. Prevalence of intimate partner violence and health implications for women using emergency departments and primary care clinics. Womens Health Issues 2004;14:19–29 [DOI] [PubMed] [Google Scholar]
- 44.Peralta RL, Fleming MF. Screening for intimate partner violence in a primary care setting: The validity of “feeling safe at home” and prevalence results. J Am Board Fam Pract 2003;16:525–532 [DOI] [PubMed] [Google Scholar]
- 45.Houry D, Kemball RS, Click LA, Kaslow NJ. Development of a brief mental health screen for intimate partner violence victims in the emergency department. Acad Emerg Med 2007;14:202–209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Arias I, Corso P. Average cost per person victimized by an intimate partner of the opposite gender: A comparison of men and women. Violence Vict 2005;20:379–391 [PubMed] [Google Scholar]
- 47.Centers for Disease Control and Prevention. Costs of intimate partner violence against women in the United States. In: U.S. Department of Health & Human Services, ed. Atlanta, GA, 2003 [Google Scholar]
- 48.Max W, Rice DP, Finkelstein E, Bardwell RA, Leadbetter S. The economic toll of intimate partner violence against women in the United States. Violence Vict 2004;19:259–272 [DOI] [PubMed] [Google Scholar]
- 49.USPTF. Screening for family and intimate partner violence. Screening: Family violence. Available at: www.ahrq.gov/downloads/pub/prevent/pdfser/famviolser.pdf Accessed August2, 2016
- 50.Stevens J, Scribano PV, Marshall J, Nadkarni R, Hayes J, Kelleher KJ. A trial of telephone support services to prevent further intimate partner violence. Violence Against Women 2015;21:1528–1547 [DOI] [PubMed] [Google Scholar]
- 51.Saftlas AF, Harland KK, Wallis AB, Cavanaugh J, Dickey P, Peek-Asa C. Motivational interviewing and intimate partner violence: A randomized trial. Ann Epidemiol 2014;24:144–150 [DOI] [PubMed] [Google Scholar]
- 52.Graham-Bermann SA, Miller-Graff LE, Howell KH, Grogan-Kaylor A. An efficacy trial of an intervention program for children exposed to intimate partner violence. Child Psychiatry Hum Dev 2015;46:928–939 [DOI] [PubMed] [Google Scholar]
- 53.Graham-Bermann SA, Miller-Graff L. Community-based intervention for women exposed to intimate partner violence: A randomized control trial. J Fam Psychol 2015;29:537–547 [DOI] [PubMed] [Google Scholar]
- 54.Wall KM, Sullivan PS, Kleinbaum D, Stephenson R. Actor-partner effects associated with experiencing intimate partner violence or coercion among male couples enrolled in an HIV prevention trial. BMC Public Health 2014;14:209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Stadler J, Delany-Moretlwe S, Palanee T, Rees H. Hidden harms: Women's narratives of intimate partner violence in a microbicide trial, South Africa. Soc Sci Med 2014;110:49–55 [DOI] [PubMed] [Google Scholar]
- 56.Rhodes KV, Rodgers M, Sommers M, Hanlon A, Crits-Christoph P. The Social Health Intervention Project (SHIP): Protocol for a randomized controlled clinical trial assessing the effectiveness of a brief motivational intervention for problem drinking and intimate partner violence in an urban emergency department. BMC Emerg Med 2014;14:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hossain M, Zimmerman C, Kiss L, et al. . Working with men to prevent intimate partner violence in a conflict-affected setting: A pilot cluster randomized controlled trial in rural Cote d'Ivoire. BMC Public Health 2014;14:339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Falb KL, Diaz-Olavarrieta C, Campos PA, et al. . Evaluating a health care provider delivered intervention to reduce intimate partner violence and mitigate associated health risks: Study protocol for a randomized controlled trial in Mexico City. BMC Public Health 2014;14:772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mejdoubi J, van den Heijkant SC, van Leerdam FJ, Heymans MW, Hirasing RA, Crijnen AA. Effect of nurse home visits vs. usual care on reducing intimate partner violence in young high-risk pregnant women: A randomized controlled trial. PloS One 2013;8:e78185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kacanek D, Bostrom A, Montgomery ET, et al. . Intimate partner violence and condom and diaphragm nonadherence among women in an HIV prevention trial in southern Africa. J Acquir Immune Defic Syndr 2013;64:400–408 [DOI] [PubMed] [Google Scholar]
- 61.Jones DL, Kashy D, Villar-Loubet OM, Cook R, Weiss SM. The impact of substance use, sexual trauma, and intimate partner violence on sexual risk intervention outcomes in couples: A randomized trial. Ann Behav Med 2013;45:318–328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hegarty KL, O'Doherty LJ, Chondros P, et al. . Effect of type and severity of intimate partner violence on women's health and service use: Findings from a primary care trial of women afraid of their partners. J Interpers Violence 2013;28:273–294 [DOI] [PubMed] [Google Scholar]
- 63.Hegarty K, O'Doherty L, Taft A, et al. . Screening and counselling in the primary care setting for women who have experienced intimate partner violence (WEAVE): A cluster randomised controlled trial. Lancet 2013;382:249–258 [DOI] [PubMed] [Google Scholar]
- 64.Graham-Bermann SA, Miller LE. Intervention to reduce traumatic stress following intimate partner violence: An efficacy trial of the Moms' Empowerment Program (MEP). Psychodyn Psychiatry 2013;41:329–349 [DOI] [PubMed] [Google Scholar]
- 65.Catallo C, Jack SM, Ciliska D, Macmillan HL. Mixing a grounded theory approach with a randomized controlled trial related to intimate partner violence: What challenges arise for mixed methods research? Nurs Res Pract 2013;2013:798213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Taft AJ, Small R, Humphreys C, et al. . Enhanced maternal and child health nurse care for women experiencing intimate partner/family violence: Protocol for MOVE, a cluster randomised trial of screening and referral in primary health care. BMC Public Health 2012;12:811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Stein ML, Miller AK. Distress resulting from perceivers' own intimate partner violence experiences predicts culpability attributions toward a battered woman on trial for killing her abuser: A path model. J Interpers Violence 2012;27:2527–2544 [DOI] [PubMed] [Google Scholar]
- 68.Carlson CE, Chen J, Chang M, et al. . Reducing intimate and paying partner violence against women who exchange sex in Mongolia: Results from a randomized clinical trial. J Interpers Violence 2012;27:1911–1931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Taft AJ, Small R, Hegarty KL, Watson LF, Gold L, Lumley JA. Mothers' AdvocateS In the Community (MOSAIC)—Non-professional mentor support to reduce intimate partner violence and depression in mothers: A cluster randomised trial in primary care. BMC Public Health 2011;11:178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Humphreys J, Tsoh JY, Kohn MA, Gerbert B. Increasing discussions of intimate partner violence in prenatal care using Video Doctor plus Provider Cueing: A randomized, controlled trial. Womens Health Issues 2011;21:136–144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Cohen JA, Mannarino AP, Iyengar S. Community treatment of posttraumatic stress disorder for children exposed to intimate partner violence: A randomized controlled trial. Arch Pediatr Adolesc Med 2011;165:16–21 [DOI] [PubMed] [Google Scholar]
- 72.Tiwari A, Fong DY, Yuen KH, et al. . Effect of an advocacy intervention on mental health in Chinese women survivors of intimate partner violence: A randomized controlled trial. JAMA 2010;304:536–543 [DOI] [PubMed] [Google Scholar]
- 73.Taylor CA. Randomised controlled trial: Early childhood home visits to high-risk families may reduce maternally perpetrated intimate partner violence. Evid Based Med 2010;15:42–43 [DOI] [PubMed] [Google Scholar]
- 74.Koziol-McLain J, Garrett N, Fanslow J, et al. . A randomized controlled trial of a brief emergency department intimate partner violence screening intervention. Ann Emerg Med 2010;56:413–423.e1 [DOI] [PubMed] [Google Scholar]
- 75.Kiely M, El-Mohandes AA, El-Khorazaty MN, Blake SM, Gantz MG. An integrated intervention to reduce intimate partner violence in pregnancy: A randomized controlled trial. Obstet Gynecol 2010;115(2 Pt 1):273–283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kataoka Y, Yaju Y, Eto H, Horiuchi S. Self-administered questionnaire versus interview as a screening method for intimate partner violence in the prenatal setting in Japan: A randomised controlled trial. BMC Pregnancy Childbirth 2010;10:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bair-Merritt MH, Jennings JM, Chen R, et al. . Reducing maternal intimate partner violence after the birth of a child: A randomized controlled trial of the Hawaii Healthy Start Home Visitation Program. Arch Pediatr Adolesc Med 2010;164:16–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Krasnoff M, Moscati R. Domestic violence screening and referral can be effective. Ann Emerg Med 2002;40:485–492 [DOI] [PubMed] [Google Scholar]
- 79.Godoy-Ruiz P, Toner B, Mason R, Vidal C, McKenzie K. Intimate partner violence and depression among Latin American women in Toronto. J Immigr Minor Health 2015;17:1771–1780 [DOI] [PubMed] [Google Scholar]
- 80.Flanagan JC, Gordon KC, Moore TM, Stuart GL. Women's stress, depression, and relationship adjustment profiles as they relate to intimate partner violence and mental health during pregnancy and postpartum. Psychol Violence 2015;5:66–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ouellet-Morin I, Fisher HL, York-Smith M, Fincham-Campbell S, Moffitt TE, Arseneault L. Intimate partner violence and new-onset depression: A longitudinal study of women's childhood and adult histories of abuse. Depress Anxiety 2015;32:316–324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gerber MR, Fried LE, Pineles SL, Shipherd JC, Bernstein CA. Posttraumatic stress disorder and intimate partner violence in a women's headache center. Women Health 2012;52:454–471 [DOI] [PubMed] [Google Scholar]
- 83.Hellmuth JC, Jaquier V, Young-Wolff K, Sullivan TP. Posttraumatic stress disorder symptom clusters, alcohol misuse, and women's use of intimate partner violence. J Trauma Stress 2013;26:451–458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Devries KM, Mak JY, Bacchus LJ, et al. . Intimate partner violence and incident depressive symptoms and suicide attempts: A systematic review of longitudinal studies. PLoS Med 2013;10:e1001439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Guillen AI, Panadero S, Rivas E, Vazquez JJ. Suicide attempts and stressful life events among female victims of intimate partner violence living in poverty in Nicaragua. Scand J Psychol 2015;56:349–356 [DOI] [PubMed] [Google Scholar]
- 86.Pico-Alfonso MA, Garcia-Linares MI, Celda-Navarro N, Blasco-Ros C, Echeburua E, Martinez M. The impact of physical, psychological, and sexual intimate male partner violence on women's mental health: Depressive symptoms, posttraumatic stress disorder, state anxiety, and suicide. J Womens Health 2006;15:599–611 [DOI] [PubMed] [Google Scholar]
- 87.Mason R, Du Mont J. Advancing our knowledge of the complexity and management of intimate partner violence and co-occurring mental health and substance abuse problems in women. F1000Prime Rep 2015;7:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Stover CS, Spink A. Affective awareness in parenting of fathers with co-occurring substance abuse and intimate partner violence. Adv Dual Diagn 2012;5:74–85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Evans DD, Shapiro SE. Intimate partner violence, depression, and substance abuse in women presenting to emergency departments for care. Adv Emerg Nurs J 2011;33:109–113 [DOI] [PubMed] [Google Scholar]
- 90.Ansara DL, Hindin MJ. Psychosocial consequences of intimate partner violence for women and men in Canada. J Interpers Violence 2011;26:1628–1645 [DOI] [PubMed] [Google Scholar]
- 91.Bhattacherjee S. Intimate partner violence affects men as well as women. BMJ 2014;348:g3771. [DOI] [PubMed] [Google Scholar]
- 92.Costa D, Hatzidimitriadou E, Ioannidi-Kapolou E, et al. . Intimate partner violence and health-related quality of life in European men and women: Findings from the DOVE study. Qual Life Res 2015;24:463–471 [DOI] [PubMed] [Google Scholar]
- 93.Costa D, Soares J, Lindert J, et al. . Intimate partner violence: A study in men and women from six European countries. Int J Public Health 2015;60:467–478 [DOI] [PubMed] [Google Scholar]
- 94.Cunradi CB. Intimate partner violence among hispanic men and women: The role of drinking, neighborhood disorder, and acculturation-related factors. Violence Vict 2009;24:83–97 [DOI] [PubMed] [Google Scholar]
- 95.Hamberger LK, Guse C. Typology of reactions to intimate partner violence among men and women arrested for partner violence. Violence Vict 2005;20:303–317 [DOI] [PubMed] [Google Scholar]
- 96.Lipsky S, Caetano R, Field CA, Bazargan S. The role of alcohol use and depression in intimate partner violence among black and Hispanic patients in an urban emergency department. Am J Drug Alcohol Abuse 2005;31:225–242 [PubMed] [Google Scholar]
- 97.Schafer SD, Drach LL, Hedberg K, Kohn MA. Using diagnostic codes to screen for intimate partner violence in Oregon emergency departments and hospitals. Public Health Rep 2008;123:628–635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Nelson HD, Nygren P, McInerney Y, Klein J, Force USPST. Screening women and elderly adults for family and intimate partner violence: A review of the evidence for the U. S. Preventive Services Task Force. Ann Intern Med 2004;140:387–396 [DOI] [PubMed] [Google Scholar]
- 99.Adams AE, Bybee D, Tolman RM, Sullivan CM, Kennedy AC. Does job stability mediate the relationship between intimate partner violence and mental health among low-income women? Am J Orthopsychiatry 2013;83:600–608 [DOI] [PubMed] [Google Scholar]
- 100.Craparo G, Gori A, Petruccelli I, Cannella V, Simonelli C. Intimate partner violence: Relationships between alexithymia, depression, attachment styles, and coping strategies of battered women. J Sex Med 2014;11:1484–1494 [DOI] [PubMed] [Google Scholar]
- 101.Breiding MJ, Black MC, Ryan GW. Chronic disease and health risk behaviors associated with intimate partner violence −18 US states/territories, 2005. Ann Epidemiol 2008;18:538–544 [DOI] [PubMed] [Google Scholar]
- 102.Hankin A, Smith LS, Daugherty J, Houry D. Correlation between intimate partner violence victimization and risk of substance abuse and depression among African-American women in an urban emergency department. West J Emerg Med 2010;11:252–256 [PMC free article] [PubMed] [Google Scholar]
- 103.Rhodes K, Houry D, Cerulli C, Straus H, Kaslow N, McNutt L. Intimate partner violence and comorbid mental health conditions among urban male patients. Ann Fam Med 2009;7:47–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Weiss NH, Dixon-Gordon KL, Duke AA, Sullivan TP. The underlying role of posttraumatic stress disorder symptoms in the association between intimate partner violence and deliberate self-harm among African American women. Compr Psychiatry 2015;59:8–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Golding JM. Intimate partner violence as a risk factor for mental disorders: A meta-analysis. J Fam Violence 1999;14:99–132 [Google Scholar]
- 106.Hines DA, Douglas EM. Symptoms of posttraumatic stress disorder in men who sustain intimate partner violence: A study of helpseeking and community samples. Psychol Men Masc 2011;12:112–127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wolf ME, Ly U, Hobart MA, Kernic MA. Barriers to seeking police help for intimate partner violence. J Fam Violence 2003;18:121–129 [Google Scholar]
- 108.Choo EK, Houry DE. Managing intimate partner violence in the emergency department. Ann Emerg Med 2015;65:447–451.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Daugherty JD, Houry DE. Intimate partner violence screening in the emergency department. J Postgrad Med 2008;54:301–305 [DOI] [PubMed] [Google Scholar]
- 110.Iverson KM, Gradus JL, Resick PA, Suvak MK, Smith KF, Monson CM. Cognitive-behavioral therapy for PTSD and depression symptoms reduces risk for future intimate partner violence among interpersonal trauma survivors. J Consult Clin Psychol 2011;79:193–202 [DOI] [PMC free article] [PubMed] [Google Scholar]