Abstract
The increase in the prevalence of overweight and obesity in both developed and developing countries is associated with musculoskeletal and other non-communicable diseases. To address this, an accurate measure of body adiposity, bearing in mind several shortcomings of body mass index (BMI), should be used. This study determined the relationship between BMI and body fat (BF)% among adult Nigerians of different ethnic groups residing in an urban setting. Using multistage cluster sampling technique were recruited 1571 subjects (>18 years; male=51.2%) in a cross-sectional study. Body adiposity indices were assessed using BMI and BF%. Using BF%, the result shows that a total number of 156 (9.9%) had low BF% while 291 (18.5%) had very high BF%, while the BMI classifications of body adiposity, 68 (4.3%) were underweight while 271 (17.3%) were obese. There was a strong and positive statistical relationship between BF% and BMI when both were paired without controlling for gender and age (r=0.81, P<0.01). The results show that there is a strong positive association between BMI and BF%, and age and sex are predictors of this association.
Key words: Body mass index, Body fat percentage, Body adiposity indices, Overweight, Obesity, Non-communicable diseases
Introduction
The prevalence of overweight and obesity has been on the increase in many countries irrespective of their economic. Overweight and obesity are usually defined as the abnormal or excessive fat accumulation that may impair health. Globally there are 1.9 billion overweight adults out of which almost 600 million of them are obese.1 In the sub-Saharan African urban population, it has been estimated that 20-50% of the urban population are either overweight or obese2,3 and the World Health Organisation (WHO) projected that by the year 2025, 75% of the global obese population would be in low income countries including sub-Saharan Africa belong.4
There are multiple methods to measure adiposity such as body mass index (BMI), skin-folds calliper measurement, waist circumference (WC), waist to hip ratio (WHR), underwater weighing (densitometry), bio-electrical impedance analysis (BIA), near infrared reactance (NIR), dual-energy X-ray absorptiometry (DEXA), and magnetic resonance imaging (MRI). BMI is relatively easy to calculate, inexpensive, and hence is widely used in the epidemiological studies. However, it does not distinguish between fat and lean body mass. On the other hand, densitometry, DEXA, and MRI provide more accurate measures of obesity but are unsuitable for epidemiological studies since they require specialized equipment and skilled manpower; and they are expensive.5 BIA and NIR are alternative field methods for measuring body fat; they both use portable machines, and their results are reproducible. Both methods have shown good correlation with DEXA, but NIR has several advantages over the BIA. NIR is not subject to variation by ethnicity, consumption of food and beverages, or exercise and it does not require pre-test calibration.
There are an increasing number of studies showing that the correlation between BMI and body fat percentage (BF%) is quite different among populations and there are uncertainty and divergent findings as to whether this relationship is linear or curvilinear. For instance, it was reported that there was no difference in the relationship between BMI and BF% between whites and blacks residing in New York6 while that the relationship between BMI and BF% between the black population residing in Nigeria, Jamaica and the United States is the same.7 Furthermore, a non-linear relationship between American black and white adults and that showed that the non-linear association are not independent of age and gender.8 There is even more uncertainty as to whether the age-dependent change in BF% relationship at a given BMT is affected by gender.9 Furthermore, it has been documented that the relationship between BF% and other anthropometric measures depends on ethnicity, age and gender.10-12
The availability of a valid index of body composition is important for health professionals so that persons at risk for developing obesity-related diseases can be successfully screened.13 Percentage body fat is strongly associated with risk of chronic diseases such as hypertension, dyslipidaemia, diabetes mellitus and coronary heart disease.14 BMI, WC, waist-hip ratio and skin fold thickness have been used extensively to measure body fatness in epidemiological and clinical studies. BMI has been used to determine overweight and obesity because it is simple, inexpensive and non-invasive. It is a surrogate measure of body fatness since it measures excess weight rather than excess body fat. However, these techniques do not accurately and precisely characterize persons by body compositions (percentage body fat or muscle mass).15
Excessive body fat deposit in the body can be measured using WC, WHR, BAI, BMI and DEXA. DEXA is a direct method of measuring body adiposity but it is expensive and cannot be used in epidemiological studies because of the time and financial implications. The WHO recommends the use of BMI for assessment and measurement of body adiposity. However, BMI, as compared to weight and height, is just an index of weight excess, rather than body fatness compositions16 and does not differentiate between excess fat, muscle, or bone mass, nor does it provide any indications for the distribution of fat among individuals.17 The inability of BMI to accurately detect and estimate body fat led to the call for new ways of assessing and measuring body fat that would be easy, cheap and be able to use in resource limited areas as well as epidemiological studies. BIA has been shown to measure body fat accurately in both resource limited areas and epidemiological studies. It is based on the principle that lean tissue, which contains large amount of water and electrolytes, is a good electrical conductor and fat, which is anhydrous, is a poor conductor. Studies have been carried out on the use of BIA to assess body compositions: children,18 Anglo Celtic population,19 Nigerian tribes20 and clinical settings.21 Despite the popularity of BIA in estimating body composition, there appear to be different levels of agreement between different BIA models and other reference methods.22
It was recently reported that 21% of the world deaths related to non-communicable diseases in individuals between the ages of 30 and 70 to be from Africa.23 This can be reduced if an accurate measurement of body fat is available. Most epidemiological studies use BMI as the method of estimation for overweight and obesity. There is a need to compare BMI to other field methods because of its limitations; and a field method, such as BIA, may be more appropriate because it distinguishes between fat and lean body mass. There is a need to assess the relationship between BMI and BF% by gauging the strength of the correlation, testing hypotheses concerning, for example, the functional form of the relationship, and using the fitted model for prediction. This study was carried out to determine the relationship between BMI and BF% as measured by TANITA BIA 549-plus among Nigerian adults of diverse ethnic affiliations in urban settings. This study also examined the nature of the relationship (i.e. whether it is linear or curvilinear), and the effects of age and gender on this relationship.
Materials and Methods
Participants and design
This was a cross-sectional survey design of a household-based sample of adults 18 years and older using a multi-stage cluster sampling technique to recruit subjects. The research setting was the Alimosho local government area of Lagos State, Nigeria, with a population of 1,277,714.24 There are 11 political wards in Alimosho local government. Using the WHO25 guidelines for conducting community surveys, five out of eleven political wards into which Alimosho area is divided were randomly chosen and three census enumeration areas (EAs) were randomly selected in each of the five chosen political wards. Permissions and ethical clearances were obtained from the University of the Western Cape Research Ethics Committee (12/9/15) and Lagos State University Health Research and Ethics Committee (LREC/10/06/261). Informed written consent was provided by the participants after the details of the study were thoroughly explained. Confidentiality and anonymity were ensured and results of each of the subjects were presented to them. Participants with high blood pressure and BMI were advised to seek medical interventions. Houses with odd numbers were selected for participation in the study. Subjects within the age range of 18 years and older in each of the houses with odd numbers were recruited for this study. Therefore, a total of 1571 adults consented to participate in the study. Data with regards to non-communicable diseases were collected with the WHO STEPS instrument.26 The WHO STEPS instrument is a standardized method of collecting, analysing and disseminating data in WHO member countries for non-communicable diseases.
Measurements
Physical measurements taken included height, weight, hip and WC, and body composition. Body composition measurement was carried out using Tanita BC-549 plus Ironman body composition monitor (Tanita BC-549 plus, Tanita Corp, Illinois, USA) by asking subjects with minimal clothing and dry feet to step on the measuring platform after the subject gender, age and height might were entered/keyed into the machine. Guest mode was used throughout the period of this study since it allows the researcher to programme the unit for a one-time use without resetting a Personal data number. Every participant was instructed not to step on the measuring platform until 0.0 was displayed. The participant was asked to step onto the measurement platform within about 30 seconds after 0.0 appeared. After the measurement was taken, readings were automatically displayed in this order: body weight, BF%, body water and muscle mass, physique rating, basal metabolic rate (BMR), metabolic age, bone mass and visceral fat rating. Readings were recorded for each subject.
Statistical analysis
Descriptive statistics of mean, median and standard deviation were used for normally distributed data while and interquartile range was used for not normally distributed data. Earlier on, the participants were grouped into three age categories (<39, 40-59 and >60) as well as into male and female based on their gender. Differences between the means were determined using Kruskal-Wallis test. Spearman rho correlation coefficient (r) was used to calculate the relationship between BMI and BF% in relation to age and gender. Multiple regression analysis was carried out to determine the effects of gender and age on the relationship between BMI and BF% using BF% as dependent variable and BMI and gender as independent variables. Body adiposity was categorized into underweight (BMI<18.5), normal weight (BMI=18.5-24.9), overweight (BMI=25-29.9) and obese (BMI>30). For BF% categorisation, Tanita 549-plus manufacturer guide for interpreting BF% result was used using the minimum age for this study as shown in Table 1.27 IBM SPSS Statistical package version 22 was used in analysing the data. Level of significance was set at 0.05.
Table 1.
Interpreting the body fat percentage result
| Gender | Age | - (low) | 0 (normal) | + (high) | ++ (very high) |
|---|---|---|---|---|---|
| Female | 20-39 | <21.0 | 21.0-32.9 | 33.0-38.9 | ≥39.0 |
| 40-59 | <23.0 | 23.0-33.9 | 34.0-39.9 | ≥40.0 | |
| 60-79 | <24.0 | 24.0-35.9 | 36.0-41.9 | ≥42.0 | |
| Male | 20-39 | <8.0 | 8.0-19.9 | 20.0-24.9 | ≥25.0 |
| 40-59 | <11.0 | 11.0-21.9 | 22.0-27.9 | ≥28.0 | |
| 60-79 | <13.0 | 13.0-24.9 | 25.0-29.9 | ≥30.0 |
Based on NIH/WHO guidelines for body mass index and Based on Gallagher et al.27
Results
A total of 1571 individuals participated in this study of which 51.2% (805) were females while 48.2% (706) were males. Table 2 summarises the participants’ age, BF% and BMI.
Table 2.
Physical characteristics of the subjects.
| Male (n=805) |
Female (n=766) |
Total (n=1571) |
P value | |
|---|---|---|---|---|
| Age (years) | 34.37±11.13 | 36.4±12.11 | 35.36±11.66 | 0.000 |
| Height (m) | 170.36±7.52 | 160.31±6.67 | 165.46±8.71 | 0.000 |
| Weight (kg) | 67.82±12.39 | 69.40±15.61 | 68.59±14.07 | 0.000 |
| Body fat, % | 17.47±7.81 | 32.95±15.66 | 25.01±14.51 | 0.000 |
| Body mass index, kg/m2 | 23.38±4.16 | 27.03±5.95 | 25.16±5.43 | 0.000 |
P values are given for comparison between male and female. Data are expressed a mean±SD.
Analysis of prevalence of body adiposity using BF% shows that a total number of 156 (9.9%) had low BF% while 291 (18.5%) had very high BF%. Regarding the BMI classification of body adiposity, 68 (4.3%) were underweight while 271 (17.3%) were obese as shown in Table 3.
Table 3.
Prevalence of body adiposity using body fat and body mass index.
| Classification (BF%) | No. | % | Classification (BMI) | No. | % |
|---|---|---|---|---|---|
| Low | 156 | 9.9 | Underweight | 68 | 4.3 |
| Normal | 798 | 50.8 | Normal | 838 | 53.3 |
| High | 323 | 20.6 | Overweight | 394 | 25.1 |
| Very high | 291 | 18.6 | Obese | 271 | 17.3 |
BF, body fat; BMI, body mass index.
Relationship between body fat percentage and body mass index
There was a strong and positive statistical relationship between BF% and BMI when both were paired without controlling for gender and age (r=.81, P<0.01). A positive and strong correlation between BF% and BMI in males (r=0.83, P<0.01) and females (r=0.89, P<0.01) was found using Spearman rho rank since the variables were not normally distributed.
Differences between body fat percentage and body mass index means
Differences between the means for the whole sample and between male and female were determined using Kruskal-Wallis test. In the whole sample, there were statistical significant differences between the categories of a BF%. In addition, there were statistical significant differences between male and female in the categories of a BF% was found. These are summarised in Table 4 below. To examine the effect of gender and age on the relationship between BF% and BMI, the P-value of the regression model is 0.001 which shows that the model is a good fit. The adjusted R2 is 81.9% which shows that 81.9% of the variance of BF% can be explained by age, gender and weight. The linear regression model/equation as follows:
Table 4.
Differences between body fat% and body mass index means.
Total group=BF%=0.583×BMI+0.456×gender+ 0.152×age.
Females=BF%=0.756×BMI+0.177×age+constant
Males=BF%=0.708×BMI+0.235×age+constant
Effects of age and gender on the relationship between body fat percentage and body mass index
Table 5 below shows that age and gender are significant predictors of the relationship between BF% and BMI. But gender contributes more effects on the relationship.
Table 5.
Effects of age and gender on the relationship between body fat% and body mass index.
| SEE | B | P value | |
|---|---|---|---|
| Intercept | 0.641 | <0.001 | |
| BMI | 0.25 | 5.83 | <0.001 |
| Age | 0.11 | 1.52 | <0.001 |
| Gender | 2.60 | 4.56 | <0.001 |
| R2 | 0.819 |
BMI, body mass index.
Relationships between body fat percentage and body mass index using age groups
There were statistical significant relationships between BMI and BF% in all the three age groups with r=0.767 (P<0.01) for <39 years age group, r=0.812 (P<0.01) for 40-59 years age group and r=0.871 (P<0.01) for>60 years age group as shown in Table 6 and Figure 1.
Table 6.
Relationships between body mass index and body fat%.
| Age Group | No. | r | P value |
|---|---|---|---|
| <39 | 1077 | 0.767 | 0.000 |
| 40-59 | 426 | 0.812 | 0.000 |
| >60 | 65 | 0.871 | 0.000 |
Scatter plot shows a strong positive correlation between BI and BF%. Though curvilinear relationship developed with increasing BMI, it shows that the correlation is still linear. Test of linearity with the use of polynomial regression shows a significant quadratic component.
Figure 1.
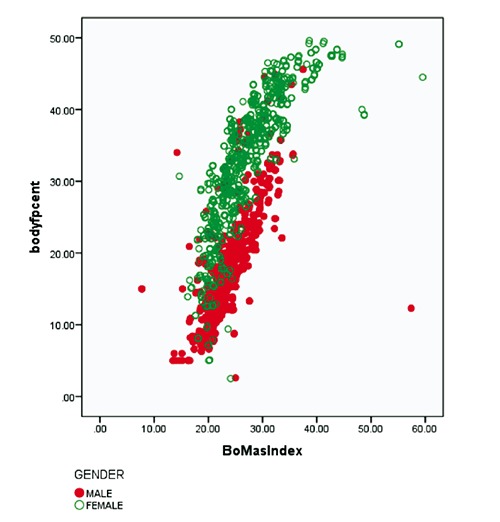
Linear correlation between body mass index and body fat percentage.
Discussion
This study aimed to investigate the relationship between BMI and BF%. A strong and positive relationship between BMI and BF% was found. This relationship was examined using age and gender as independent variables. The results of our study show that the strength of the relationship between BF% and BMI increases with advancing age when looked at relationship in different age groups. This can be literarily explained that the older one becomes the more/higher the BF% one possesses. This is in line with the previous studies carried out in different population.6,28 Few of the reasons that can be adduced for this include protein-energy malnutrition29 and disuse muscle atrophy which might arise from inactivity or lack of inadequate physical activity.30 Findings indicate that in hypothetical cases of 23 kg/m2 BMIs for men and women, there is an increase in BF% of approximately 1.0-1.1 and 0.7-1.0% per decade, respectively.6 The findings of this study are similar to that of a study among three different black populations of African origin.7 Other researchers have also reported that BMI strongly correlates with BF% estimated by bioelectrical impedance in a group of South Asian adults from Sri Lanka.31 There are divergent opinions regarding whether the relationship between BF% and BMI is linear or curvilinear. Earlier on, a curvilinear relationship has been reported between BF% and BMI among health conscious Sri Lankan adults31 despite the fact that 94% of their subjects had BMI values <30 kg/m2 and in UK adults7 with BMI values <35 kgm2. However, our study shows a linear relationship. The curvilinear relationship is usually seen in samples with higher BMI of >35 kg/m2 which have been reported in the literatures.9,32 However, 95.86% of our total sample had BMI of <35 kg/m2. This is in line with previous study where there was a significant linear correlation between BF% and BMI in both black and white women.6
The multiple regression analysis shows that age and gender have significant effects on the relationship between BF% and BMI. Previous studies have also documented that age and gender had significant effects on the relationship between BF% and BMI and that the relationship was even stronger with gender.7,33 The clinicians and public health scientists should always take into account the effects of age and gender when the use of BMI in predicting BF% arises. It was also observed from our study that the strength of the relationship between BF% and BMI increased with increase in age. This could be due to the replacement of lean muscle mass with fat as ageing sets in so as to compensate for the BMI at an older age.
Conclusions
The results of our study demonstrate that there is a strong relationship between BMI and BF% measured by BIA which is influenced mostly by gender and to a lesser extent by age among adult Nigerians. Also, there is linear relationship between BMI and BF% in our study. This implies that as BMI increases there is a corresponding increase in the BF% of our participants. Therefore, our findings support that age and gender should be considered when interpreting BMI in a cross sectional studies and trials like ours that are clinically oriented. Either BMI or BF% can be used to access level of adiposity among the study sample but this should be done with caution as this study did not look into which between BMI and BF% is better in predicting cardiovascular diseases.
Acknowledgements
The authors are indebted to all those who participated in the study. We are grateful for the valuable advice on statistical analyis from Dr Siake Lougue of the Department of Statistics and Population Studies at the University of the Western Cape.
References
- 1.WHO. Factsheet No 311- Obesity and overweight. Geneva. 2015. Available from: http://www.who.int/mediacentre/factsheets/fs311/en/index.html [Google Scholar]
- 2.Kamadjeu RM, Edwards R, Atanga JS, et al. Anthropometry measures and prevalence of obesity in the urban adult population of Cameroon: an update from the Cameroon Burden of Diabetes Baseline Survey. BMC Public Health 2006;6:228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sodjinou R, Agueh V, Fayomi B, Delisle H. Obesity and cardiometabolic risk factors in urban adults of Benin: relationship with socio-economic status, urbanisation, and lifestyle patterns. BMC Public Health 2008;8:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO Preventing chronic diseases: a vital investment: WHO global report. Geneva, Switzerland: WHO; 2005. [Google Scholar]
- 5.Jennings CL, Micklesfield LK, Lambert MI, et al. Comparison of body fatness measurements by near-infrared reactance and dual-energy Xray absorptiometry in normal-weight and obese black and white women. Br J Nutr 2010;103:1065-9. [DOI] [PubMed] [Google Scholar]
- 6.Gallagher D, Visser M, Sepulveda D, et al. How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups? Am J Epidemiol 1996;143: 228-39. [DOI] [PubMed] [Google Scholar]
- 7.Luke A, Durazo-Arvizzu R, Rotimi C, et al. Relation between body mass index and body fat in black population samples from Nigeria, Jamaica and the United States. Am J Epidemiol 1997;145:620-8. [DOI] [PubMed] [Google Scholar]
- 8.Jackson AS, Stanforth PR, Gagnon J, et al. The effect of sex, age and race on estimating percentage body fat from body mass index: The Heritage Family Study. Int J Obes Relat Metab Disord 2002;26:789-96. [DOI] [PubMed] [Google Scholar]
- 9.Meeuwsen S, Horgan GW, Elia M. The relationship between BMI and percent body fat, measured by bioelectrical impedance, in a large adult sample is curvilinear and influenced by age and sex. Clin Nutr 2010;29:560-6. [DOI] [PubMed] [Google Scholar]
- 10.Womersley J, Durnin JVGA. A comparison of the skinfold method with extent of overweight and various weight-height relationships in the assessment of obesity. Br J Nutr 1977;38:271-84. [DOI] [PubMed] [Google Scholar]
- 11.Deurenberg-Yap M, Schmidt G, van Staveren WA, et al. Body fat measurement among Singaporean Chinese, Malays and Indians: a comparative study using a four compartment model and different two-compartment models. Br J Nutr 2001;85: 491-8. [DOI] [PubMed] [Google Scholar]
- 12.Lopes DCF, Silvestre MPC, Silva MR, et al. Evaluation of body fat composition in Brazilian women by anthropometry, bioimpedance and dual energy x-ray absorptiometry. Alim Nutr Braz J Food Nutr 2013:24:259-65. [Google Scholar]
- 13.Wellens RI, Roche AF, Khamis HJ, et al. Relationships between body mass index and body composition. Obes Res 1996;4:35-44. [DOI] [PubMed] [Google Scholar]
- 14.Dentali F, Sharma AM, Douketis JD. Management of hypertension in overweight and obese patients: a practical guide for clinicians. Curr Hypertens Rep 2005;7:330-6. [DOI] [PubMed] [Google Scholar]
- 15.Dagenais GR, Yi Q, Mann JF, et al. Prognostic impact of body weight and abdominal obesity in women and men with cardiovascular disease. Am Heart J 2005;149:54-60. [DOI] [PubMed] [Google Scholar]
- 16.Wang C, Hou XH, Zhang ML, et al. Comparison of body mass index with body fat percentage in the evaluation of obesity in Chinese. Biomed Environ Sci 2010;23:173-9. [DOI] [PubMed] [Google Scholar]
- 17.Daniels SR. The use of BMI in the clinical setting. Paediatrics 2009;124:S35-41. [DOI] [PubMed] [Google Scholar]
- 18.Pecoraro P, Guida B, Caroli M, et al. Body mass index and skin fold thickness versus bioimpedance analysis: fat mass prediction in children. Acta Diabetol 2003;40:S278-81. [DOI] [PubMed] [Google Scholar]
- 19.Wattanapenpaiboon N, Lukito W, Strauss BJ, et al. Agreement of skinfold measurement and bioelectrical impedance analysis (BIA) methods with dual energy X-ray absorptiometry (DEXA) in estimating total body fat in Anglo-Celtic Australians. Int J Obes Relat Metab Disord 1998;22:854-60. [DOI] [PubMed] [Google Scholar]
- 20.Azinge EC, Mabayoje M, Ward LC. Body proportions in three Nigerian tribes. Acta Diabetol 2003;40:S317-9. [DOI] [PubMed] [Google Scholar]
- 21.Buchholz AC, Bartok C, Schoeller DA. The validity of bioelectrical impedance models in clinical populations. Nutr Clin Pract 2004;19:433-46. [DOI] [PubMed] [Google Scholar]
- 22.Dehghan M, Merchant AT. Is bioelectrical impedance accurate for use in large epidemiological studies? Nutr J 2008;7:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gulland A. Most countries will fail to meet targets on non-communicable diseases, says WHO. BMJ 2015;350:h331. [DOI] [PubMed] [Google Scholar]
- 24.Nigeria Population Commission (NPC). Report of the 2006 National Census Exercise. Published in National Population Commission Bulletin, Abuja, Nigeria; 2007. [Google Scholar]
- 25.Sethi D, Habibula S, McGee K, et al. Guidelines for conducting community surveys on injuries and violence. Geneva: World Health Organisation; 2004. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organisation. STEPwise approach to surveillance (STEPS), 2008. Available from: http://www.who.intl/chp/steps/en [Google Scholar]
- 27.Gallagher D, Heymsfield SB, Heo M, et al. Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr 2000;72:691-701. [DOI] [PubMed] [Google Scholar]
- 28.Mills TC. Predicting body fat using data on the BMI. J Stat Educ 2005;13:1-12. [Google Scholar]
- 29.World Health Organization. Global strategy on diet, physical activity and health: obesity and overweight. Available from: http://www.who.int/mediacentre/factsheets/fs311/en/ [Google Scholar]
- 30.Evans WJ. Exercise, nutrition and aging. J Nutr 1992;122:796-801. [DOI] [PubMed] [Google Scholar]
- 31.Bortz WM., 2nd Disuse and aging. JAMA 1982;248:1203-8. [PubMed] [Google Scholar]
- 32.Jackson AS, Pollock ML, Ward A. Generalized equations for predicting body density of women. Med Sci Sports Exerc 1980;12:175-81. [PubMed] [Google Scholar]
- 33.Ranasinghe C, Gamage P, Katulanda P, et al. Relationship between body mass index (BMI) and body fat percentage, estimated by bioelectrical impedance, in a group of Sri Lankan adults: a cross sectional study. BMC Public Health 2013;13:797. [DOI] [PMC free article] [PubMed] [Google Scholar]


