Abstract
Objective
As smartphone technology becomes an increasingly important part of youth mental health, there has been little to no examination of how to effectively integrate smartphone-based safety planning with inpatient care. Our study sought to examine whether or not we could effectively integrate smartphone-based safety planning into the discharge process on a child and adolescent inpatient psychiatry unit.
Method
Staff members completed a survey to determine the extent of smartphone ownership in a population of admitted child and adolescent inpatients. In addition to quantifying smartphone ownership, the survey also tracked whether youth would integrate their previously-established safety plan with a specific safety planning application on their smartphone (Be Safe) at the time of discharge.
Results
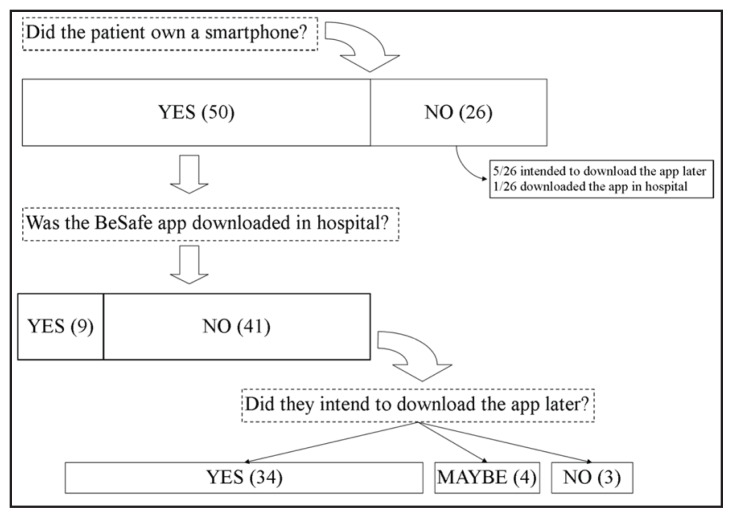
Sixty-six percent (50/76) of discharged youth owned a smartphone, which is consistent with prior reports of high smartphone ownership in adult psychiatric populations. A minority of youth (18%) downloaded the Be Safe app prior to discharge, with most (68%) suggesting they would download the app after discharge. Notably, all patients who downloaded the app prior to discharge were on their first admission to a psychiatric inpatient unit.
Conclusion
Child and adolescent psychiatric inpatients have a clear interest in smartphone-based safety planning. Our results suggest that integrating smartphone-related interventions earlier in an admission might improve access before discharge. This highlights the tension between restricting and incorporating smartphone access for child and adolescent inpatients and may inform future study in this area.
Keywords: smartphones, mobile apps, safety plans, discharge planning, suicide prevention, adolescent
Résumé
Objectif
Comme la technologie du téléphone intelligent devient une partie de plus en plus importante de la santé mentale des adolescents, il y a eu peu ou pas d’examen de la façon d’intégrer efficacement la planification de la sécurité liée au téléphone intelligent aux soins des patients hospitalisés. Notre étude cherchait à examiner si nous pouvions intégrer efficacement la planification de la sécurité liée au téléphone intelligent au processus du congé dans un service psychiatrique pour enfants et adolescents hospitalisés.
Méthode
Les membres du personnel ont répondu à un sondage pour déterminer combien de téléphones intelligents étaient la propriété d’une population d’enfants et d’adolescents hospitalisés. En plus de quantifier la propriété de téléphones intelligents, le sondage demandait aussi si les adolescents ajouteraient à leur plan de sécurité préétabli une application spécifique de planification de sécurité (Be Safe) dans leur téléphone intelligent au moment du congé.
Résultats
Soixante-six pour cent (50/76) des adolescents ayant eu leur congé possédaient un téléphone intelligent, ce qui est conforme aux rapports précédents de propriété élevée de téléphones intelligents dans les populations psychiatriques adultes. Une minorité d’adolescents (18 %) ont téléchargé l’application Be Safe avant d’obtenir leur congé, et la plupart (68 %) ont suggéré qu’ils la téléchargeraient après le congé. À noter, tous les patients qui ont téléchargé l’application avant le congé étaient hospitalisés pour la première fois dans un service psychiatrique.
Conclusion
Les enfants et les adolescents hospitalisés en psychiatrie ont un intérêt évident pour la planification de la sécurité liée au téléphone intelligent. Nos résultats suggèrent que l’intégration précoce des interventions liées au téléphone intelligent durant une hospitalisation peut améliorer l’accès avant le congé. Ceci met en évidence la tension entre la restriction et l’incorporation de l’accès au téléphone intelligent pour les enfants et les adolescents hospitalisés, et peut éclairer une future étude dans ce domaine.
Mots clés: téléphones intelligents, applications mobiles, plans de sécurité, planification du congé, prévention du suicide, adolescent
Introduction
Most mental disorders first emerge in childhood or adolescence (Merikangas et al., 2010). Among adolescents globally, suicide is the third-leading cause of death behind road accidents and human immunodeficiency virus (World Health Organization, 2014b). Although there has been some success at characterizing suicide risk factors in youth, there are large gaps in the literature regarding the efficacy of preventative interventions (Bennett et al., 2015).
Mobile health technologies hold tremendous promise as cost-effective and youth-friendly mental health interventions for this population (Perry, Werner-Seidler, Calear, & Christensen, 2016; Seko, Kidd, Wiljer, & McKenzie, 2014). In the context of suicide prevention, smartphone applications (“apps”) have the potential to aid in risk assessment, provide psycho-education and information on available resources, facilitate adherence to safety plans, and offer access to crisis support and coping tools (Luxton, June, & Chalker, 2015). Adolescent smartphone ownership is dramatically increasing, with recent estimates of 75–84% (Lenhart, 2015; Thinkhouse Ireland, 2014).
The World Health Organization (WHO) recommends mobile devices as an option for providing support and therapy to people at risk of suicide and emphasizes the importance of effective and collaborative communication during transitions of care (e.g. from inpatient to outpatient) (World Health Organization, 2014a). For youth who have been hospitalized for acute suicidality, the transition from an inpatient level of care to a less restrictive environment represents a period of elevated suicide risk (Bridge, Goldstein, & Brent, 2006). Safety planning is considered an integral component of the discharge process, although it has not been specifically evaluated in this population. Nevertheless, there is a growing base of evidence about safety planning in the literature (e.g. safety planning was part of the psychotherapeutic intervention which showed promise in the Treatment of Adolescent Suicide Attempters open trial, safety planning has been shown to be an effective brief intervention for suicidal adults presenting to the emergency department) (Brent et al., 2009; Stanley & Brown, 2012). Based on the WHO recommendations, the process of safety planning during the inpatient to outpatient transition could represent an ideal setting for smartphone-related intervention.
There are at least 3000 mental health apps available today, with diverse functionality ranging from symptom tracking and self-monitoring to appointment reminders and treatment adherence (Aboujaoude, Salame, & Naim, 2015). Unfortunately, the therapeutic potential of these apps remains largely theoretical, as there is a lack of efficacy evidence. There are several small randomized controlled trials (RCTs) of smartphone apps with positive results (e.g. self-monitoring apps have been found superior to retrospective questioning of patients, several cognitive-behavioural therapy apps have shown a significant reduction in depressive symptoms) (Aboujaoude et al., 2015; Donker et al., 2013). Even with increasing research on mobile technology and mental health, the majority of the commercially-available apps have not been evaluated scientifically, underscoring the paucity of evidence (Donker et al., 2013). Unsurprisingly, a review of 27 suicide prevention apps not only found a clear disparity in app quality, but also noted that there was minimal information about how the content was selected or developed (leading the authors to abandon any attempts at determining whether these applications were evidence-based) (Aguirre, McCoy, & Roan, 2013). Similarly, a recent systematic review surveying web-based and mobile suicide prevention interventions in young people commented on the need for empirical evidence after they found only one study which met inclusion criteria (Perry et al., 2016).
Therefore, the role of smartphones in the safety planning process, particularly at the time of transition from an inpatient to outpatient level of care, has yet to be studied. Moreover, no study to date has investigated the prevalence of smartphone ownership in the inpatient child and adolescent psychiatric population. Our study sought to examine the feasibility of incorporating smartphone-based safety planning at the time of discharge from an inpatient to outpatient level of care. Specifically, we sought to understand if youth admitted to inpatient psychiatric units owned smartphones and whether or not they would effectively incorporate their smartphone into a safety planning exercise at discharge. We hoped to inform clinicians on the potential impact of a smartphone-related intervention in this population.
Method
This study involved de-identified data which was originally gathered for inpatient program evaluation purposes. The data was gathered from patients who had been discharged from the child and adolescent psychiatry inpatient unit at London Health Sciences Centre between April 1, 2014 and February 28, 2015. Unit staff (either nurses or child and youth counsellors) were instructed to log several items during the discharge process for admitted inpatients under the age of 18. Questions included: whether patients own a smart phone, whether their safety plan was reviewed, whether their safety plan was incorporated into a safety planning application on their smartphone, and if not, whether patients intended to incorporate their safety plan into their smartphone upon discharge. At this time, youth were provided with more information about the Be Safe application including how to enter their paper-based safety plan into the application.
The Be Safe app allows users to create a digital safety plan, informs them about mental health and addiction resources in the local community (currently customized for 23 regions across Ontario), directs users to the best resources with a decision aid, creates a personal ‘get help’ script to assist users in finding the words to reach out, and empowers them to do so safely (see Figure 1). Since its London pilot in 2014, it has expanded across Ontario and is now available in French and Arabic. The Be Safe development model emphasizes that youth always have a voice in the decision process about the updated needed to keep the tool relevant. Ethics approval was granted by the Health Science Research Ethics Board (HSREB) at Western University. The questionnaire data was aggregated and analyzed using Microsoft Excel 2007. In total, 76 questionnaires were completed during the aforementioned time period, all of which were included in the analysis.
Figure 1.
Screenshots from Be Safe App
Results
Of the 76 patients, 50 reported that they owned a smartphone (see Figure 2). Of the 26 who reported they did not own a smartphone, five patients reported that they still intended to download the Be Safe app later (including one who specified that they owned a tablet). One patient who did not own a smartphone reported downloading the app in hospital. For these six patients who did not own a smartphone yet answered as if they did own one (either downloaded the app in hospital or intended to do so later), we assume that they had access to another person’s smartphone (e.g. a parent’s phone) or a similar smart device such as a tablet computer.
Figure 2.
Flowchart of Results from 76 Questionnaires
Of the 50 patients who owned a smartphone, nine downloaded the Be Safe app in hospital. Of the 41 smartphone owners who did not download in hospital, 34 stated they intended to download the app later, and four additional patients stated they would “maybe” download the app later. Only three out of 50 patients who owned a smartphone reported no interest in downloading the Be Safe app. In total, ten out of 76 patients were able to download the safety planning application on a smartphone prior to discharge. An additional 43 patients expressed an interest in downloading the app after discharge, 38 of whom owned a smartphone.
Fifty-one out of 74 patients were on their first admission to hospital (with two questionnaires providing no response) (see Table 1). Of note, each of the ten patients who downloaded the Be Safe app in hospital was on their first admission. Of the 51 patients for whom this was their first admission, ten downloaded the app, 23 owned a phone and planned to download the app later, one owned a phone and refused to download the app, and 17 did not own a smartphone (although four non-owners intended to download later) (see Table 1). Of the 23 patients for whom this was not their first admission, 15 owned a smartphone and planned to download the app later, one owned a smartphone but did not intend to download Be Safe, and seven did not own a smartphone (although two non-owners intended to download later) (see Table 1).
Table 1.
Comparison of Data amongst Patients on their First Admission versus Repeat Admissions
| First Admission? | Yes = 51 | No = 23 |
| Did patient own a smartphone? | 34 (66.7%) | 16 (69.6%) |
| Downloaded prior to discharge? | 10 (19.6%) | 0 |
| Planned to download postdischarge? | 27 (52.9%)1 | 17 (73.9%)2 |
| Owned phone but refused download | 1 (2.0%) | 1 (4.3%) |
Of these 27, 4 did not own smartphones.
Of these 17, 2 did not own smartphones.
Discussion
This is the first study to report on the prevalence of smartphone ownership in the child and adolescent psychiatry inpatient population. 65.8% of patients in this study reported that they owned a smartphone, which is consistent with reports of youth smartphone ownership in the general population (ranging from 37–84%) (Lenhart, 2015; Thinkhouse Ireland, 2014) . This prevalence is also comparable to reports on smartphone ownership in adult populations: 62.5% (200/320) of adult psychiatric outpatients from four distinct clinics (state-run clinic in Massachusetts, hybrid public-private clinic in Louisiana, country clinic in California, and a private university clinic in Wisconsin) were found to own a smartphone (Torous, Chan, et al., 2014). Notably, smartphone ownership was largest in the subset of adults under 30 (78%) and in the subset of patients surveyed at the university clinic (76.9%) (Torous, Chan, et al., 2014). Similarly, a 2014 report of smartphone ownership in adult psychiatric outpatients at an urban teaching hospital found that 67% owned smartphones (Torous, Friedman, & Keshvan, 2014).
The patients’ interest in adopting the Be Safe app was also encouraging. In total, 71.1% of patients in our study were able to download a safety planning app or were interested in downloading the app after discharge. Of those who owned smartphones, only 6% were opposed to downloading the Be Safe app. These figures demonstrate a high interest in smartphones apps for safety planning, even after acknowledging the possibility of over-estimation (e.g. patients giving socially desirable answers to questions).
Our clinical experience of patients being enthusiastic about using this app has also been reflected in the national usage statistics. As of June 2016, there have been over 7,100 downloads of Be Safe. On average, users viewed 5.78 screens in each session for a total of 2:09 minutes. The most popular section was the safety plan component (10,816 screen views) followed by resources (8,008 screen views) and the decision aid (7,353 screen views). 85.5% of users accessed the app on an Apple device (9,853 sessions) and 4.6% on Android (532 sessions). Unfortunately, ascertaining these usage parameters for the specific population in our study was beyond its scope, so this remains an area for further study.
Our results echo a growing literature on the interest in specific apps targeting the adolescent population and those with suicidal ideation. For example, the MYPLAN app (designed to help those at risk of suicide) has been downloaded 8000 times and both users and clinicians have provided positive feedback (Larsen, Frandsen, & Erlangsen, 2016). The “CopeSmart” app (designed for mood monitoring and provision of coping skills) was identified as either very useful or somewhat useful by 79% of adolescent females (Kenny, Dooley, Fitzgerald, & Kenny, 2015). A recent qualitative study of adolescents, parents, and clinicians found that all parties endorsed the use of a personalized smartphone app to improve accessibility and portability of a patient’s safety plan (Kennard et al., 2015).
It is important to note that only ten out of 76 patients actually downloaded the app prior to discharge. Although 43 patients expressed intent to download Be Safe after discharge, they might not have done so. One question raised by these results is whether waiting to download the app until the moment of discharge limits the opportunity for staff to facilitate the adoption of a smartphone app. To our knowledge, there are no reports in the literature on the prevalence of phone restrictions on psychiatric inpatient units. However, in our setting, smartphones have not been permitted due to smartphone camera functions and the ward privacy policy. Allowing youth access to their smartphones while an inpatient could permit the development of familiarity with an app during the admission and it would concurrently give staff the ability to confirm that interested patients were able to download the app. Generally, the issue of technology on inpatient units is relatively understudied and there can be tension between access to potentially-therapeutic technology and privacy-related restrictions.
Limitations
Despite its unique contribution to the literature, our study only captured a portion of all discharged patients as the survey was not mandatory for all discharged inpatients. It is important to note that our ward restrictions on smartphone use limited the opportunity to download the app prior to discharge. Therefore, the proportion that did download the app in this study is not representative of those that would have downloaded the app in hospital if there were no restrictions in place. In addition, the lack of identifying data made it possible for a patient to appear twice in the data set if they were admitted more than once during the study. The data was gathered indirectly from program staff, which introduces a potential source of error or bias. The inability to confirm whether a patient had downloaded the app after saying they would do so was an additional limitation, as patients or parents may have answered in a way they thought would be pleasing to staff. Lastly, because only descriptive statistics were used, the observations should only be considered hypothesis-generating.
Conclusion
Smartphone-based apps could play a role in safety planning when children and adolescents are being discharged from an inpatient unit to an outpatient level of care. A high percentage of youth not only own smartphones but also have an interest in using apps for this purpose. If these apps prove to be effective interventions for youth, our results suggest that there might be an earlier role for smartphones apps during the admission in order to ensure access before discharge. In the future, prospective studies of smartphone app users will help determine whether these tools can be effective in preventing suicide.
Acknowledgements/Conflicts of Interest
Dr. Gregory and Dr. Sukhera have no perceived or actual conflicts of interest to report. Melissa Taylor-Gates has received funding support from partners across Ontario to support mindyourmind and development of the Be Safe app. Be Safe was created by a team of youth, mindyourmind, the Centre for Addiction and Mental Health, and other partners in the Systems Improvement through Service Collaboratives initiative in London, Ontario and surrounding area to improve access to and coordination of mental health and addictions services for children, youth and families in April 2014. Since July 2015, it had expanded to 23 regions across Ontario.
References
- Aboujaoude E, Salame W, Naim L. Telemental health: A status update. World Psychiatry: Official Journal of the World Psychiatric Association (WPA) 2015;14(2):223–230. doi: 10.1002/wps.20218. http://doi.org/10.1002/wps.20218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aguirre RTP, McCoy MK, Roan M. Development guidelines from a study of suicide prevention mobile applications (Apps) Journal of Technology in Human Services. 2013;31(February 2014):269–293. http://doi.org/10.1080/15228835.2013.814750. [Google Scholar]
- Bennett K, Rhodes AE, Duda S, Cheung AH, Manassis K, Links P, …Szatmari P. A youth suicide prevention plan for Canada: A systematic review of reviews. Canadian Journal of Psychiatry Revue Canadienne de Psychiatrie. 2015;60(6):245–257. doi: 10.1177/070674371506000603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent D, Greenhill L, Compton S, Emslie G, Walkup J, Vitiello B, …Turner JB. The Treatment of Adolescent Suicide Attempters (TASA) study: Predictors of suicidal events in an open treatment trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48(10):987–996. doi: 10.1097/CHI.0b013e3181b5dbe4. http://doi.org/10.1097/CHI.0b013e3181b5dbe4.The. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bridge JA, Goldstein TR, Brent DA. Adolescent suicide and suicidal behavior. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2006;47(3–4):372–394. doi: 10.1111/j.1469-7610.2006.01615.x. http://doi.org/10.1111/j.1469-7610.2006.01615.x. [DOI] [PubMed] [Google Scholar]
- Donker T, Petrie K, Proudfoot J, Clarke J, Birch MR, Christensen H. Smartphones for smarter delivery of mental health programs: A systematic review. Journal of Medical Internet Research. 2013;15(11):e247. doi: 10.2196/jmir.2791. http://doi.org/10.2196/jmir.2791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennard BD, Biernesser C, Wolfe KL, Foxwell AA, Craddock Lee SJ, Rial KV, Brent DA. Developing a brief suicide prevention intervention and mobile phone application: A qualitative report. Journal of Technology in Human Services. 2015;33(4):345–357. doi: 10.1080/15228835.2015.1106384. http://doi.org/10.1080/15228835.2015.1106384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny R, Dooley B, Fitzgerald A, Kenny R. Feasibility of “CopeSmart ”: A telemental health app for adolescents. Journal of Medical Internet Research. 2015;2(3e22):1–10. doi: 10.2196/mental.4370. http://doi.org/10.2196/mental.4370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen JLS, Frandsen H, Erlangsen A. MYPLAN – A mobile phone application for supporting people at risk of suicide. Crisis-the Journal of Crisis Intervention and Suicide Prevention. 2016 doi: 10.1027/0227-5910/a000371. http://doi.org/10.1027/0227-5910/a000371. [DOI] [PubMed] [Google Scholar]
- Lenhart A. Teens, Social Media and Technology Overview 2015. 2015. Retrieved March 22, 2016, from http://www.pewinternet.org/files/2015/04/PI_TeensandTech_Update2015_0409151.pdf.
- Luxton DD, June JD, Chalker SA. Mobile health technologies for suicide prevention: feature review and recommendations for use in clinical care. Current Treatment Options in Psychiatry. 2015:349–362. http://doi.org/10.1007/s40501-015-0057-2. [Google Scholar]
- Merikangas KR, He J-P, Burstein M, Swanson SA, Avenevoli S, Cui L, Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A) Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. http://doi.org/10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry Y, Werner-Seidler A, Calear AL, Christensen H. Web-based and mobile suicide prevention interventions for young people: A systematic review. Journal of the Canadian Academy of Child and Adolescent Psychiatry. 2016;25(2):73–79. [PMC free article] [PubMed] [Google Scholar]
- Seko Y, Kidd S, Wiljer D, McKenzie K. Youth mental health interventions via mobile phones: A scoping review. Cyberpsychology, Behavior and Social Networking. 2014;17(9):591–602. doi: 10.1089/cyber.2014.0078. http://doi.org/10.1089/cyber.2014.0078. [DOI] [PubMed] [Google Scholar]
- Stanley B, Brown GK. Safety planning intervention: A brief intervention to mitigate suicide risk. Cognitive and Behavioral Practice. 2012;19(2):256–264. http://doi.org/10.1016/j.cbpra.2011.01.001. [Google Scholar]
- Thinkhouse Ireland. Irish Mobile Youth Report 2014. 2014 http://doi.org/10.1121/1.3508834. [Google Scholar]
- Torous J, Chan SR, Yee-Marie Tan S, Behrens J, Mathew I, Conrad EJ, Keshavan M. Patient smartphone ownership and interest in mobile apps to monitor symptoms of mental health conditions: A survey in four geographically distinct psychiatric clinics. JMIR Mental Health. 2014;1(1):e5. doi: 10.2196/mental.4004. http://doi.org/10.2196/mental.4004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torous J, Friedman R, Keshvan M. Smartphone ownership and interest in mobile applications to monitor symptoms of mental health conditions. Journal of Medical Internet Research. 2014;16(1):1–8. doi: 10.2196/mhealth.2994. http://doi.org/10.2196/mhealth.2994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Preventing suicide: A global imperative. Geneva, Switzerland: World Health Organization; 2014a. http://doi.org/10.1002/9780470774120. [Google Scholar]
- World Health Organization. WHO | Adolescent health. 2014b. Retrieved March 22, 2016, from http://www.who.int/topics/adolescent_health/en/