Abstract
Context:
Despite rising awareness of the risks associated with sports participation, overuse injuries continue to increase in youth athlete populations. Physeal injuries are one type of overuse injury exclusive to pediatric populations that are often sustained during athletic practice or competition. Overuse physeal injuries are, in theory, preventable; however, little consensus has been reached surrounding the risk factors, prevention, and treatment strategies.
Objective:
This systematic review summarizes the best available evidence concerning overuse physeal injuries in youth and adolescent athletes. It can be used to develop prevention and treatment programs specific to this population.
Data Sources:
PubMed and Academic Search Complete (EBSCOhost) were explored using the keyword physeal injuries from January 1950 through May 2015 to identify 24 studies.
Study Selection:
Original research studies of athletic populations with mechanisms of injury related to sport were chosen.
Study Design:
Systematic review.
Level of Evidence:
Level 3.
Data Extraction:
Data were extracted as available from 24 eligible studies. Study quality was rated using the Oxford Centre for Evidence-based Medicine (OCEBM) guidelines.
Results:
Risk factors for injury include periods of accelerated growth, chronological age, body size, training volume, and previous injury. Injury prevention strategies currently emphasize participation limitations and sport-specific training programs in skeletally immature athletes. The most effective treatment after an overuse physeal injury was an extended period of active rest and joint immobilization when necessary.
Conclusion:
Overuse physeal injuries are multifactorial in nature. Muscular imbalances after accelerated growth periods predispose young athletes to overuse injuries. Modifiable risk factors such as flexibility, strength, and training volume should be regularly monitored to prevent these injuries.
Keywords: physis, physeal injury, overuse, sports injuries, pediatric injuries
An estimated 30 million children in the United States are involved annually in organized sport.1,14 Despite rising awareness of the risks associated with sports participation, overuse injuries continue to increase in youth athlete populations.1,13-16,18,37 Physeal injuries are overuse injuries exclusive to pediatric populations that are most often sustained during athletic practice or competition.9,10,12-14,16-18,20,24,30,34-36,41,45,48,53,58,66,81-83,88 While specific mechanisms of injury are heterogeneous and differ by sport, the physis, as the weakest part of the bone, is a site highly prone to injury in youth athletes.12,13,15,27
Overuse physeal injuries develop in response to excess stress placed on immature bony and soft tissue structures.13-18,24,25,30-34,36,37,40,42,44,48,58,61,62,73 Rapid physical changes combined with repetitive sport-related tasks such as running and overhead throwing are frequently associated with the development of physeal injuries in youth athletes.13,15,20 The gradual nature of this injury progression provides clinicians with multiple opportunities for effective intervention. Overuse physeal injuries are, in theory, preventable. Prevention and treatment strategies should be population specific, taking into account risk factors and clinical impairments observed in youth athletes.15 The purpose of this work was to review the best available evidence concerning recommended prevention and treatment strategies for overuse physeal injuries in clinical practice.
Methods
Literature Review and Article Identification
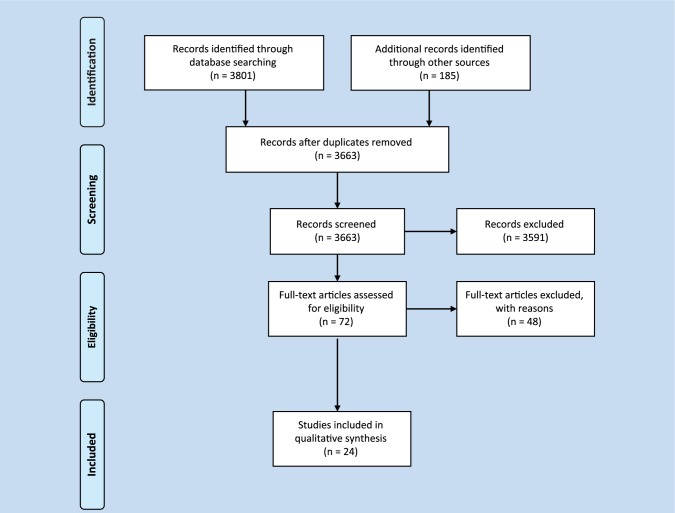
An electronic literature search was performed accessing papers published from January 1950 to May 2015 in the PubMed and all EBSCOhost databases. Search terms included epiphyseal injury, epiphyseal plate injury, pediatric sports injury, and physeal sports injury. Additional searches in the aforementioned databases were performed using the terms Little League shoulder, gymnast wrist, Little League elbow, lower extremity physeal injury, Osgood Schlatter disease, Sever disease, and Sinding-Larsen-Johansson disease as they were the most commonly reported mechanisms of injury during the primary search. Only English-language articles published in peer-reviewed journals with an emphasis on human participants were initially included. Articles were also required to meet level 4 standards or higher based on criteria developed by the Oxford Centre for Evidence-based Medicine (OCEBM). Abstracts and nonpublished works were not included. Based on these search criteria, 3663 articles were located. Using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, studies were selected based on appropriateness of topic and full-text options.60 All clinical commentaries and review articles were omitted. A total of 24 original research studies were included in this systematic review (Figure 1).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)60 flow diagram.
Eligibility Criteria
Article selection was based on repetitive stress as a mechanism of injury in young athletes. Case reports, case series, and cohort studies that described non-sport-related mechanisms of injury, such as falls, were not included in this review. Acute sport-related injuries were also excluded. The scope of this systematic review was limited to overuse physeal injuries sustained during athletic competition.
Results
Twenty-four studies were included in this systematic review (Tables 1 and 2).2,4-6,8,21,24,32,33,37-39,44,46,47,49,59,62,63,65,72,73,84,87 Thirty-three percent of studies included descriptions of known physeal injury risk factors while only 8% of studies used those factors to outline effective prevention strategies.6,21,24,32,44,65,72,84 Eighty-eight percent of studies included data describing treatment strategies after an overuse physeal injury.2,5,6,8,21,24,32,33,37,39,46,47,49,59,62,63,65,73,84,87 Review of current evidence suggests that more emphasis has been placed on the treatment of overuse physeal injuries and that further research is needed to establish effective prevention strategies for these diagnoses.
Table 1.
Studies that report lower extremity physeal injuries
| Study | Level of Evidence (OCEBM) | Sample Size | Age Range, y | Injury Site | Sport | Treatment Options |
|---|---|---|---|---|---|---|
| Beovich5 | 3 | 22 | 9-18 | Proximal tibial tubercle | Multiple | Activity modifications (20); active rest (2) |
| de Lucena et al24 | 3 | 954 | 12-15 | Proximal tibial tubercle | Multiple | Stretching program |
| Doral et al32 | 4 | 1 | 16 | Anterior superior iliac spine | Soccer | Surgical intervention |
| Hajdu et al37 | 4 | 7 | 13-16 | Proximal tibial tubercle | Ball games, skiing | Active rest (1); surgical intervention (6) |
| Hussain and Hagroo39 | 3 | 261 | 11-18 | Proximal tibial tubercle | Multiple | Active rest and NSAIDs (237); surgical intervention (24) |
| Kolt and Kirkby44 | 3 | 43 | 11-19 | Multiple sites | Gymnastics | Physical conditioning program |
| Kujala et al46 | 3 | 68 | 9-18 | Proximal tibial tubercle | Multiple | Active rest—3 mo; activity modifications—7 mo |
| Laor et al47 | 4 | 6 | 8-15 | Distal femur, proximal tibia, proximal fibula | Football, basketball, gymnastics, other | Joint immobilization—1-5 wk |
| Liebling et al49 | 4 | 1 | 13 | Distal femur, proximal tibia | Baseball | None |
| Mital et al59 | 3 | 118 | 9-18 | Proximal tibial tubercle | Multiple | Active rest/joint immobilization (104); surgical intervention (14) |
| Nanni et al62 | 4 | 1 | 15 | Proximal tibia | Rugby | Surgical intervention |
| Orava and Virtanen65 | 3 | 185 | 9-26 | Multiple sites | Multiple | Varied |
| Rossi and Dragoni72 | 3 | 203 | 11-18 | Pelvic apophyses | Soccer, gymnastics, fencing, tennis | None |
| Valentino et al87 | 4 | 1 | 13 | Inferior patellar pole | Football | Active rest—5 mo |
NSAIDs, nonsteroidal anti-inflammatory drugs; OCEBM, Oxford Centre for Evidence-based Medicine.
Table 2.
Studies that report upper extremity physeal injuries
| Study | Level of Evidence (OCEBM) | Sample Size | Age Range, y | Injury Site | Sport | Treatment Options |
|---|---|---|---|---|---|---|
| Akgul et al2 | 4 | 1 | 13 | Proximal humerus | Nonathlete | Active rest—4 mo |
| Anton and Podberesky4 | 4 | 1 | 13 | Proximal humerus | Baseball | Active rest, physical therapy |
| Binder et al6 | 3 | 72 | 8-13 | Proximal humerus | Unknown | Joint immobilization—1-4 wk (57); surgical intervention (15) |
| Boyd and Batt8 | 4 | 1 | 15 | Proximal humerus | Badminton | None |
| Carson and Gasser21 | 3 | 23 | 14 | Proximal humerus | Baseball | Active rest—3 mo |
| Drescher et al33 | 4 | 1 | 12 | Proximal humerus | Cricket | Joint immobilization—3 wk; active rest—3 mo |
| Hang et al38 | 3 | 343 | 8-12 | Distal humerus | Baseball | None |
| Kolt and Kirkby44 | 3 | 43 | 11-19 | Multiple sites | Gymnastics | Physical conditioning program |
| Obembe et al63 | 4 | 4 | 11-15 | Proximal humerus | Baseball, tennis | Active rest—3 mo |
| Orava and Virtanen65 | 3 | 185 | 9-26 | Multiple sites | Multiple | Varied |
| Roy et al73 | 4 | 21 | 11-18 | Distal radius | Gymnastics | None |
| Torg et al84 | 4 | 1 | 12 | Proximal humerus | Baseball | None |
Risk factors common to both lower extremity (LE) and upper extremity (UE) physeal injuries include age, physical characteristics, growth patterns, and training volume.13,15,20 While limited evidence was available describing effective prevention strategies in this population, studies did emphasize that youth athletes should engage in minimum periods of active rest after their competition cycles.13,27 Adequate physical training and variation in sport-specific tasks were also encouraged.13,28 Treatment strategies after an overuse physeal injury included varying periods of active rest, and when necessary, immobilization of the affected joint.2,4-6,21,33,37,39,46,47,59,63,87 Gradual return to physical training and conditioning tasks was recommended prior to full return to sport.4,5,44,46
Lower Extremity Injuries
Overuse physeal injuries in the LE typically occur when excess stress is placed across areas with major tendon insertions.7,13 Osgood-Schlatter disease, Sever disease, and Sinding-Larsen-Johansson syndrome are 3 of the most common overuse physeal injuries sustained during childhood.10,53,56 The first 2 syndromes account for a staggering 18% of all pediatric overuse injuries reported in the literature.53
Osgood-Schlatter disease is described as chronic apophysitis of the patellar tendon where it inserts on the tibial tuberosity apophysis. It is typically observed in girls aged 8 to 13 years and boys aged 10 to 15 years (Figure 2).24 The same inflammatory process occurs with Sever disease but at the Achilles tendon insertion into the vertical calcaneal apophysis.65 This condition appears to present more often in young boys between the ages of 8 and 12 years.40 Sinding-Larsen-Johansson syndrome has a similar etiology but develops at the junction of the inferior pole of the patella and the proximal portion of the patellar tendon.87 While this syndrome appears less frequently in the literature than the previous 2, Sinding-Larsen-Johansson syndrome does occur in youth athletes between the ages of 10 and 15 years, limiting their function and participation levels (Table 1).87
Figure 2.

Radiograph of a 13-year-old male football player with Osgood-Schlatter disease.
Prevention strategies in the literature emphasize the correction of modifiable risk factors such as deficits in trunk and LE flexibility, which is often attributed to rapid changes in physical growth common during childhood and adolescence.13,15,20,28,87 Programs designed to enhance cardiovascular endurance and correct physical training errors are also recommended to prevent these types of injuries.24,27,44 After an overuse physeal injury in the LE, 50% of studies recommend a 3- to 5-month period of active rest, with complete cessation of sport-specific activities.5,37,39,46,59,65,87 Twenty-one percent of studies suggest activity modifications may be appropriate based on the symptom presentation of the athlete, thereby limiting their total time away from sport.5,46,65 Lower extremity stretching and conditioning programs were also used in 21% of the studies as either a stand-alone treatment or in conjunction with additional strategies.24,44,65 Several studies reported joint immobilization and surgical intervention for long-standing physeal injuries related to overuse; however, these strategies were only employed in severe cases.37,39,47,59,62,65 Irrespective of the treatment strategy used, an athlete should not fully return to sport until symptom resolution has occurred. No studies to date have examined or compared the effectiveness of these treatments in youth athlete populations.75
Upper Extremity Injuries
Overuse physeal injuries in the UE occur due to excess compression or traction forces placed across a joint during sport.13,30 Gymnast wrist, Little League shoulder, and Little League elbow are 3 UE physeal injuries that are highly prevalent and described frequently in the pediatric sports literature.2,4,6,8,21,33,38,44,63,65,73,84 Seventy-nine percent of youth gymnasts report wrist pain during practice or competition, while 32% of youth baseball pitchers report arm pain while throwing.30,51,52
Gymnast wrist occurs in response to the premature closure of the distal radial physis after excessive compression loads during UE weightbearing.18,49 Gymnastics is one of the few sports that repeatedly performs closed-chain weightbearing activities on both their upper and lower extremities.3,11,14,16,17,25,30,31 This injury is typically seen in athletes between the ages of 10 and 14 years (Table 2).30 Little League shoulder has been described in the literature as a widening of the proximal humeral epiphysis or epiphysiolysis (Figure 3). It is most often seen in the dominant shoulder and is thought to occur secondary to the repetitive rotational and traction stresses associated with overhead throwing.2,4,6,9,21,33,63,84 “Little League elbow” is a term often used to describe a variety of physeal and cartilaginous injuries at the pediatric elbow.12,13,15,35,38,42 By definition, Little League elbow is a repetitive traction injury to the medial epicondylar apophysis (Figure 4).35 Diagnoses of Little League shoulder and Little League elbow are most often made after reports of persistent arm pain and loss of function in youth baseball pitchers between the ages of 11 and 15 years (Table 2).21,42,63
Figure 3.

Radiograph of a 14-year-old male baseball player with Little League shoulder.
Figure 4.

Radiograph of a 13-year-old male baseball player with Little League elbow.
Risk factors associated with the development of gymnast wrist include consistent UE loading and timing of growth spurts.29 Studies suggest that participation in repetitive UE weightbearing tasks, especially during periods of rapid physical growth, is directly associated with this highly prevalent, population-specific injury.13,26,29-31 Risk factors related to the development of Little League shoulder and Little League elbow are similar. Excessive game, season, and yearly pitch counts and pitching while fatigued are factors that have been associated with shoulder and elbow dysfunction in youth baseball players.51,52 Pitch type and selection are also important for the health of this population. Youth baseball players who reported throwing breaking pitches such as curveballs or sliders over the course of the season were more at risk to develop shoulder and elbow pain when compared with those who did not.51 Anthropometric measures such as increased height and weight also impacted injury risk but were more significant to the development of elbow pathology than shoulder pathology.52
Despite the lack of epidemiological data concerning gymnast wrist, multiple prevention strategies have been suggested in the literature.26,27,29 The gradual progression and variation of training loads is imperative to limit the volume of compressive forces sustained through the distal radial physis.26,28,29 Studies suggest that coaches and parents should be cognizant of rapid changes in growth, as the athlete is most at risk for overuse physeal injuries during this period.26,28 In an effort to prevent Little League shoulder and Little League elbow, USA Baseball implemented yearly, seasonal, and game pitch count limitations based on an athlete’s age at the time of competition.51,52,64 These recommendations were designed to decrease an athlete’s risk for injury by limiting excessive stress and fatigue during sports participation.50-52
Treatment strategies for all 3 overuse physeal injuries center around an extended period of active rest. After an injury, 50% of studies recommend active rest from sport-specific training to ensure adequate healing and symptom resolution.2,4,21,33,63,65 Recommended periods of active rest range from 4 to 6 weeks for a diagnosis of gymnast wrist or Little League elbow and 3 to 5 months for athletes with Little League shoulder.2,21,29,63,80 In severe cases of Little League elbow, joint immobilization and/or surgical intervention have been employed to ensure optimal functional outcomes.43,66,69 However, an extended period of active rest remains the main treatment of choice for overuse physeal injuries in the UE.
Discussion
Physeal injuries represent approximately 15% of all pediatric sports injuries.13 The physis, as the weakest physiologic structure of the bone in a young athlete, is particularly susceptible to overuse injuries.9,10,12-20,24,29,34-36,41,45,48,53,58,66,81-83,88 As participation in youth sports continues to increase, clinicians should know the risk factors, prevention strategies, and treatment options associated with overuse physeal injuries.9,10,13,15,16,35,82,83
Risk Factors
Risk factors associated with participation in youth sports have been reported; however, none have examined injury risk with respect to physeal injuries.15 Physeal injuries are exclusive to skeletally immature individuals, suggesting that modifiable and nonmodifiable risk factors are specific to this population.15,20,24,25,36,44,57,75
Nonmodifiable risk factors for overuse injuries can include timing of accelerated growth spurts, chronological age, body size, and history of previous injury.15,27,29 Previous injury is the strongest predictor for the development of future injuries.15,20,70,86 Studies show that athletes with a prior injury were at a much greater risk to sustain an injury when compared with a previously healthy cohort.86 Modifiable risk factors such as flexibility, strength, training volume, and coaching styles also impact overall injury risk in youth and adolescent athletes. Multiple studies suggest that excessive training loads often lead to physical fatigue in youth athletes.13,15,41 Continued participation in sport once fatigued can damage an athlete’s physical development, thereby illustrating the importance of responsible coaching, especially during the early years of sport.15,27,29,41
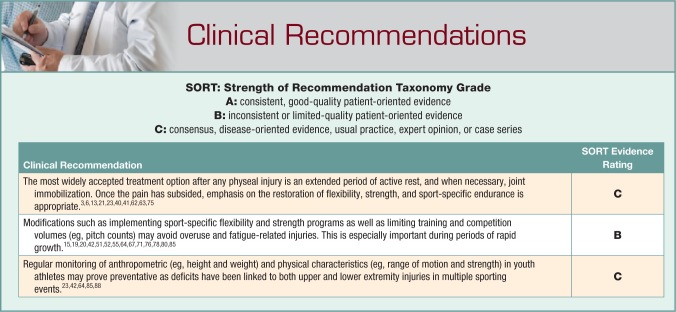
Prevention and Treatment Strategies
Injury prevention strategies for youth and adolescent athletes focus on limiting time spent participating in sport as well as encouraging 2 to 3 months of scheduled rest away from training and competition.27,68 This is designed to mediate the effects of repetitive risk-prone activities on physically maturing bodies. Pitch count regulations, which are enforced by the governing bodies in youth baseball, are one notable attempt at preventing upper extremity overuse injuries at the policy level.51,52,76,79 Multiple studies have also recommended that clinicians monitor known risk factors such as anthropometric (eg, height and weight) and physical characteristics (eg, range of motion and strength) as youth athletes mature over time.24,26,27,77,85 Multiple programs designed to improve flexibility, strength, and balance deficits have protective effects against injuries in this population.15,19,54,55,67,78
The most widely accepted treatment strategy after any physeal injury is an extended period of active rest.3,6,13,21,23,40,42,62,63,75 Recommended durations of active rest vary from 4 to 6 weeks to 3 to 5 months depending on diagnosis, sport, and severity of symptoms.20,21,42 During this time, strategies can include field position changes to limit throwing in the cases of Little League shoulder and Little League elbow or no running for a specified period of time in athletes with Osgood-Schlatter disease, Sinding-Larsen-Johansson syndrome, or Sever disease. In most cases, nonsymptomatic activities such as hitting a baseball or footwork drills in soccer can be continued, allowing young athletes to continue training without prolonging their recovery by reaggravating the affected joint.
During a period of active rest, conservative measures such as physical therapy may be beneficial. Once the pain has subsided, the necessary flexibility, strength, and neuromuscular control required to participate safely in sport can be restored.2-4,8,14,16-19,21,22,25,29,31,33,43,44,63,74,80 Progressive strength training programs, lasting approximately 6 to 8 weeks, can augment return to throwing or running programs when appropriate.42 The rehabilitation programs in the literature were vague and lacked return-to-sport criteria.42,80 Future research should focus on the development of age- and injury-specific return-to-sport progressions designed to provide clinicians with evidence-based guidelines to return their athletes safely back to sport.
Limitations
The main limitation of this systematic review was the lack of experimental and epidemiological data concerning overuse injuries in youth sports. Review studies typically described pediatric sports injuries in general terms with little respect to injury type. The current evidence surrounding risk factors, prevention, and treatment strategies for overuse injuries in youth sports was primarily limited to review studies and level 3 and 4 publications. The paucity of high-quality evidence combined with strict inclusion criteria appeared to impact the study selection process. A variety of search terms were used; however, a disproportionate number of studies featured Little League shoulder as the diagnosis. This selection bias toward overuse physeal injuries in the UE may have influenced the generalizability of the clinical recommendations made in this systematic review.
The lack of high-quality, patient-oriented research in younger athlete populations and the absence of research on physeal injuries pose notable gaps in the literature. These gaps include minimal data establishing the incidence, prevalence, and severity of overuse injuries in youth athletes, especially with respect to physeal involvement.52,64 No original research studies have clearly defined physeal injuries at this time. Also, little is known about the effects of population-specific risk factors, like growth-related changes and training volume, on the development of injuries in skeletally immature individuals. Future studies should establish a clear definition of physeal injuries in sport and determine the mechanisms and risk factors associated with their development. This will provide the foundation for more effective prevention and treatment strategies at the policy level, including the paradigm-shifting concept of scheduled periods of rest from sport.
Conclusion
Overuse physeal injuries are multifactorial in nature.55 Periods of accelerated growth, chronological age, skeletal maturity, and history of previous injury can predispose young athletes to repetitive stress injuries.55 Modifiable risk factors such as flexibility, strength, and training volume should be regularly monitored in an effort to limit risk-prone activities and prevent injuries when possible.15,20,24,25,36,44,75,86
The most effective treatment strategy after overuse physeal injuries is an extended period of active rest. After symptom resolution, athletes should restore function through improvements in flexibility, strength, and neuromuscular control.2-4,8,14,16-18,20-22,25,30,31,33,43,44,74,80 Progressive strength training programs should include gradual return to throwing or running programs when appropriate.42 Return-to-sport timelines typically range from 4 to 6 weeks in most cases but can extend to 3 to 5 months when symptoms persist.21,42,47
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Adirim TA, Cheng TL. Overview of injuries in the young athlete. Sports Med. 2003;33:75-81. [DOI] [PubMed] [Google Scholar]
- 2. Akgul S, Dilicikik U, Kanbur NO, Kaya D, Donmez G, Doral MN. Proximal humeral physeal widening: little leaguer’s shoulder or a variation of normal development? Turk J Pediatr. 2011;53:711-714. [PubMed] [Google Scholar]
- 3. Albanese SA, Palmer AK, Kerr DR, Carpenter CW, Lisi D, Levinsohn EM. Wrist pain and distal growth plate closure of the radius in gymnasts. J Pediatr Orthop. 1989;9:23-28. [DOI] [PubMed] [Google Scholar]
- 4. Anton C, Podberesky DJ. Little League shoulder: a growth plate injury. Pediatr Radiol. 2010;40(suppl 1):S54. [DOI] [PubMed] [Google Scholar]
- 5. Beovich RF. Osgood-Schlatter’s disease: a review of the literature and an Australian series. Aust J Sci Med Sport. 1988;20:11-13. [Google Scholar]
- 6. Binder H, Schurz M, Aldrian S, Fialka C, Vecsei V. Physeal injuries of the proximal humerus: long-term results in seventy two patients. Int Orthop. 2011;35:1497-1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bloom OJ, Mackler L, Barbee J. Clinical inquiries. What is the best treatment for Osgood-Schlatter disease? J Fam Pract. 2004;53:153-156. [PubMed] [Google Scholar]
- 8. Boyd KT, Batt ME. Stress fracture of the proximal humeral epiphysis in an elite junior badminton player. Br J Sports Med. 1997;31:252-253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Brooks MA, Schiff MA, Rivara FP. Identifying previous sports injury among high school athletes. Clin Pediatr (Phila). 2009;48:548-550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bruns W, Maffulli N. Lower limb injuries in children in sports. Clin Sports Med. 2000;19:637-662. [DOI] [PubMed] [Google Scholar]
- 11. Butler TA, Yingling VR. The effects of delayed puberty on the growth plate. J Pediatr Orthop. 2013;33:99-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Caine D, Caine C, Maffulli N. Incidence and distribution of pediatric sport-related injuries. Clin J Sport Med. 2006;16:500-513. [DOI] [PubMed] [Google Scholar]
- 13. Caine D, DiFiori J, Maffulli N. Physeal injuries in children’s and youth sports: reasons for concern? Br J Sports Med. 2006;40:749-760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Caine D, Lewis R, O’Connor P, Howe W, Bass S. Does gymnastics training inhibit growth of females? Clin J Sport Med. 2001;11:260-270. [DOI] [PubMed] [Google Scholar]
- 15. Caine D, Maffulli N, Caine C. Epidemiology of injury in child and adolescent sports: injury rates, risk factors, and prevention. Clin Sports Med. 2008;27:19-50. [DOI] [PubMed] [Google Scholar]
- 16. Caine D, Roy S, Singer KM, Broekhoff J. Stress changes of the distal radial growth plate. A radiographic survey and review of the literature. Am J Sports Med. 1992;20:290-298. [DOI] [PubMed] [Google Scholar]
- 17. Caine DB, Bass S, Daly R. Does elite competition inhibit growth and delay maturation in some gymnasts? Quite possibly. Pediatr Exerc Sci. 2003;15:360-372. [Google Scholar]
- 18. Caine DH, Howe W, Ross W, Bergman R. Does repetitive physical loading inhibit radial growth in female gymnasts. Clin J Sports Med. 1997;7:302-308. [DOI] [PubMed] [Google Scholar]
- 19. Caine DJ, Golightly YM. Osteoarthritis as an outcome of paediatric sport: an epidemiological perspective. Br J Sports Med. 2011;45:298-303. [DOI] [PubMed] [Google Scholar]
- 20. Caine DJ, Maffulli N. Epidemiology of children’s individual sports injuries. An important area of medicine and sport science research. Med Sport Sci. 2005;48:1-7. [DOI] [PubMed] [Google Scholar]
- 21. Carson WG, Jr, Gasser SI. Little Leaguer’s shoulder. A report of 23 cases. Am J Sports Med. 1998;26:575-580. [DOI] [PubMed] [Google Scholar]
- 22. Carter SR, Aldridge MJ, Fitzgerald R, Davies AM. Stress changes of the wrist in adolescent gymnasts. Br J Radiol. 1988;61:109-112. [DOI] [PubMed] [Google Scholar]
- 23. Cohen E, Sala DA. Rehabilitation of pediatric musculoskeletal sport-related injuries: a review of the literature. Eur J Phys Rehabil Med. 2010;46:133-145. [PubMed] [Google Scholar]
- 24. de Lucena GL, dos Santos Gomes C, Guerra RO. Prevalence and associated factors of Osgood-Schlatter syndrome in a population-based sample of Brazilian adolescents. Am J Sports Med. 2011;39:415-420. [DOI] [PubMed] [Google Scholar]
- 25. De Smet L, Claessens A, Lefevre J, Beunen G. Gymnast wrist: an epidemiologic survey of ulnar variance and stress changes of the radial physis in elite female gymnasts. Am J Sports Med. 1994;22:846-850. [DOI] [PubMed] [Google Scholar]
- 26. DiFiori JP. Overuse injury and the young athlete: the case of chronic wrist pain in gymnasts. Curr Sports Med Rep. 2006;5:165-167. [DOI] [PubMed] [Google Scholar]
- 27. DiFiori JP, Benjamin HJ, Brenner J, et al. Overuse injuries and burnout in youth sports: a position statement from the American Medical Society for Sports Medicine. Clin J Sport Med. 2014;24:3-20. [DOI] [PubMed] [Google Scholar]
- 28. DiFiori JP, Benjamin HJ, Brenner JS, et al. Overuse injuries and burnout in youth sports: a position statement from the American Medical Society for Sports Medicine. Br J Sports Med. 2014;48:287-288. [DOI] [PubMed] [Google Scholar]
- 29. DiFiori JP, Caine DJ, Malina RM. Wrist pain, distal radial physeal injury, and ulnar variance in the young gymnast. Am J Sports Med. 2006;34:840-849. [DOI] [PubMed] [Google Scholar]
- 30. DiFiori JP, Puffer JC, Aish B, Dorey F. Wrist pain, distal radial physeal injury, and ulnar variance in young gymnasts: does a relationship exist? Am J Sports Med. 2002;30:879-885. [DOI] [PubMed] [Google Scholar]
- 31. DiFiori JP, Puffer JC, Mandelbaum BR, Dorey F. Distal radial growth plate injury and positive ulnar variance in nonelite gymnasts. Am J Sports Med. 1997;25:763-768. [DOI] [PubMed] [Google Scholar]
- 32. Doral MN, Aydog ST, Tetik O, Atay OA, Turhan E, Demirel HA. Multiple osteochondroses and avulsion fracture of anterior superior iliac spine in a soccer player. Br J Sports Med. 2005;39:e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Drescher WR, Falliner A, Zantop T, Oehlert K, Petersen W, Hassenpflug J. Little league shoulder syndrome in an adolescent cricket player. Br J Sports Med. 2004;38:E14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Eastwood DM, de Gheldere A, Bijlsma P. Physeal injuries in children. Surgery. 2014;32:1-8. [Google Scholar]
- 35. Frush TJ, Lindenfeld TN. Peri-epiphyseal and overuse injuries in adolescent athletes. Sports Health. 2009;1:201-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Gottschalk AW, Andrish JT. Epidemiology of sports injury in pediatric athletes. Sports Med Arthrosc. 2011;19:2-6. [DOI] [PubMed] [Google Scholar]
- 37. Hajdu S, Kaltenecker G, Schwendenwein E, Vecsei V. Apophyseal injuries of the proximal tibial tubercle. Int Orthop. 2000;24:279-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hang DW, Chao CM, Hang YS. A clinical and roentgenographic study of Little League elbow. Am J Sports Med. 2004;32:79-84. [DOI] [PubMed] [Google Scholar]
- 39. Hussain AH, Hagroo GA. Osgood-Schlatter disease. Sports Exerc Inj. 1996;2:202-206. [Google Scholar]
- 40. Kennedy JG, Knowles B, Dolan M, Bohne W. Foot and ankle injuries in the adolescent runner. Curr Opin Pediatr. 2005;17:34-42. [DOI] [PubMed] [Google Scholar]
- 41. Kerssemakers SP, Fotiadou AN, de Jonge MC, Karantanas AH, Maas M. Sport injuries in the paediatric and adolescent patient: a growing problem. Pediatr Radiol. 2009;39:471-484. [DOI] [PubMed] [Google Scholar]
- 42. Klingele KE, Kocher MS. Little league elbow: valgus overload injury in the paediatric athlete. Sports Med. 2002;32:1005-1015. [DOI] [PubMed] [Google Scholar]
- 43. Kocher MS, Waters PM, Micheli LJ. Upper extremity injuries in the paediatric athlete. Sports Med. 2000;30:117-135. [DOI] [PubMed] [Google Scholar]
- 44. Kolt GS, Kirkby RJ. Epidemiology of injury in elite and subelite female gymnasts: a comparison of retrospective and prospective findings. Br J Sports Med. 1999;33:312-318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Krueger-Franke M, Siebert CH, Pfoerringer W. Sports-related epiphyseal injuries of the lower extremity. An epidemiologic study. J Sports Med Phys Fitness. 1992;32:106-111. [PubMed] [Google Scholar]
- 46. Kujala UM, Kvist M, Heinonen O. Osgood-Schlatter’s disease in adolescent athletes: retrospective study of incidence and duration. Am J Sports Med. 1985;13:236-241. [DOI] [PubMed] [Google Scholar]
- 47. Laor T, Wall EJ, Vu LP. Physeal widening in the knee due to stress injury in child athletes. AJR Am J Roentgenol. 2006;186:1260-1264. [DOI] [PubMed] [Google Scholar]
- 48. LeVeau BF, Bernhardt DB. Developmental biomechanics. Effect of forces on the growth, development, and maintenance of the human body. Phys Ther. 1984;64:1874-1882. [DOI] [PubMed] [Google Scholar]
- 49. Liebling MS, Berdon WE, Ruzal-Shapiro C, Levin TL, Roye D, Jr, Wilkinson R. Gymnast’s wrist (pseudorickets growth plate abnormality) in adolescent athletes: findings on plain films and MR imaging. AJR Am J Roentgenol. 1995;164:157-159. [DOI] [PubMed] [Google Scholar]
- 50. Lyman S, Fleisig GS. Baseball injuries. Med Sport Sci. 2005;49:9-30. [DOI] [PubMed] [Google Scholar]
- 51. Lyman S, Fleisig GS, Andrews JR, Osinski ED. Effect of pitch type, pitch count, and pitching mechanics on risk of elbow and shoulder pain in youth baseball pitchers. Am J Sports Med. 2002;30:463-468. [DOI] [PubMed] [Google Scholar]
- 52. Lyman S, Fleisig GS, Waterbor JW, et al. Longitudinal study of elbow and shoulder pain in youth baseball pitchers. Med Sci Sports Exerc. 2001;33:1803-1810. [DOI] [PubMed] [Google Scholar]
- 53. Maffulli N, Bruns W. Injuries in young athletes. Eur J Pediatr. 2000;159:59-63. [DOI] [PubMed] [Google Scholar]
- 54. Maffulli N, Longo UG, Gougoulias N, Caine D, Denaro V. Sport injuries: a review of outcomes. Br Med Bull. 2011;97:47-80. [DOI] [PubMed] [Google Scholar]
- 55. Maffulli N, Longo UG, Gougoulias N, Loppini M, Denaro V. Long-term health outcomes of youth sports injuries. Br J Sports Med. 2010;44:21-25. [DOI] [PubMed] [Google Scholar]
- 56. Maffulli N, Longo UG, Spiezia F, Denaro V. Sports injuries in young athletes: long-term outcome and prevention strategies. Phys Sportsmed. 2010;38:29-34. [DOI] [PubMed] [Google Scholar]
- 57. McHugh MP, Tyler TF, Tetro DT, Mullaney MJ, Nicholas SJ. Risk factors for noncontact ankle sprains in high school athletes: the role of hip strength and balance ability. Am J Sports Med. 2006;34:464-470. [DOI] [PubMed] [Google Scholar]
- 58. Mirtz TA, Chandler JP, Eyers CM. The effects of physical activity on the epiphyseal growth plates: a review of the literature on normal physiology and clinical implications. J Clin Med Res. 2011;3:1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Mital MA, Matza RA, Cohen J. The so-called unresolved Osgood-Schlatter lesion: a concept based on fifteen surgically treated lesions. J Bone Joint Surg Am. 1980;62:732-739. [PubMed] [Google Scholar]
- 60. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336-341. [DOI] [PubMed] [Google Scholar]
- 61. Murray DW, Wilson-MacDonald J, Morscher E, Rahn BA, Kaslin M. Bone growth and remodeling after fracture. J Bone Joint Surg Br. 1996;78:42-50. [PubMed] [Google Scholar]
- 62. Nanni M, Butt S, Mansour R, Muthukumar T, Cassar-Pullicino VN, Roberts A. Stress-induced Salter-Harris I growth plate injury of the proximal tibia: first report. Skeletal Radiol. 2005;34:405-410. [DOI] [PubMed] [Google Scholar]
- 63. Obembe OO, Gaskin CM, Taffoni MJ, Anderson MW. Little Leaguer’s shoulder (proximal humeral epiphysiolysis): MRI findings in four boys. Pediatr Radiol. 2007;37:885-889. [DOI] [PubMed] [Google Scholar]
- 64. Olsen SJ, Fleisig GS, Dun S, Loftice J, Andrews JR. Risk factors for shoulder and elbow injuries in adolescent baseball pitchers. Am J Sports Med. 2006;34:905-912. [DOI] [PubMed] [Google Scholar]
- 65. Orava S, Virtanen K. Osteochondroses in athletes. Br J Sports Med. 1982;16:161-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Patel DR, Nelson TL. Sports injuries in adolescents. Med Clin North Am. 2000;84:983-1007. [DOI] [PubMed] [Google Scholar]
- 67. Paterno MV, Taylor-Haas JA, Myer GD, Hewett TE. Prevention of overuse sports injuries in the young athlete. Orthop Clin North Am. 2013;44:553-564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Petty DH, Andrews JR, Fleisig GS, Cain EL. Ulnar collateral ligament reconstruction in high school baseball players: clinical results and injury risk factors. Am J Sports Med. 2004;32:1158-1164. [DOI] [PubMed] [Google Scholar]
- 69. Rauck RC, LaMont LE, Doyle SM. Pediatric upper extremity stress injuries. Curr Opin Pediatr. 2013;25:40-45. [DOI] [PubMed] [Google Scholar]
- 70. Rauh MJ, Koepsell TD, Rivara FP, Margherita AJ, Rice SG. Epidemiology of musculoskeletal injuries among high school cross-country runners. Am J Epidemiol. 2006;163:151-159. [DOI] [PubMed] [Google Scholar]
- 71. Ray TR. Youth baseball injuries: recognition, treatment, and prevention. Curr Sports Med Rep. 2010;9:294-298. [DOI] [PubMed] [Google Scholar]
- 72. Rossi F, Dragoni S. Acute avulsion fractures of the pelvis in adolescent competitive athletes: prevalence, location and sports distribution of 203 cases collected. Skeletal Radiol. 2001;30:127-131. [DOI] [PubMed] [Google Scholar]
- 73. Roy S, Caine D, Singer KM. Stress changes of the distal radial epiphysis in young gymnasts. A report of twenty-one cases and a review of the literature. Am J Sports Med. 1985;13:301-308. [DOI] [PubMed] [Google Scholar]
- 74. Sabick MB, Kim YK, Torry MR, Keirns MA, Hawkins RJ. Biomechanics of the shoulder in youth baseball pitchers: implications for the development of proximal humeral epiphysiolysis and humeral retrotorsion. Am J Sports Med. 2005;33:1716-1722. [DOI] [PubMed] [Google Scholar]
- 75. Scharfbillig RW, Jones S, Scutter SD. Sever’s disease: what does the literature really tell us? J Am Podiatr Med Assoc. 2008;98:212-223. [DOI] [PubMed] [Google Scholar]
- 76. Severini GC, Cacchio A, Campana V, Milano G. Prevention strategies of shoulder injuries. In: Doral MN, Karlsson J. eds. Sports Injuries: Prevention, Diagnosis, Treatment and Rehabilitation. New York, NY: Springer; 2015:279-290. [Google Scholar]
- 77. Shanley E, Kissenberth MJ, Thigpen CA, et al. Preseason shoulder range of motion screening as a predictor of injury among youth and adolescent baseball pitchers. J Shoulder Elbow Surg. 2015;24:1005-1013. [DOI] [PubMed] [Google Scholar]
- 78. Shanley EB, Bailey L, Rauh MJ, et al. Influence of a prevention program on arm injury risk: an RCT in adolescent pitchers. Orthop J Sports Med. 2014;2(7 suppl 2):2325967114S00089. [Google Scholar]
- 79. Shanley E, Rauh MJ, Michener LA, Ellenbecker TS, Garrison JC, Thigpen CA. Shoulder range of motion measures as risk factors for shoulder and elbow injuries in high school softball and baseball players. Am J Sports Med. 2011;39:1997-2006. [DOI] [PubMed] [Google Scholar]
- 80. Shanley E, Thigpen CA. Throwing injuries in the adolescent athlete. Int J Sports Phys Ther. 2013;8:630-640. [PMC free article] [PubMed] [Google Scholar]
- 81. Sharma P, Luscombe KL, Maffulli N. Sports injuries in children. Trauma. 2003;5:245-259. [Google Scholar]
- 82. Stracciolini A, Casciano R, Levey Friedman H, Meehan WP, 3rd, Micheli LJ. Pediatric sports injuries: an age comparison of children versus adolescents. Am J Sports Med. 2013;41:1922-1929. [DOI] [PubMed] [Google Scholar]
- 83. Stracciolini A, Casciano R, Levey Friedman H, Stein CJ, Meehan WP, 3rd, Micheli LJ. Pediatric sports injuries: a comparison of males versus females. Am J Sports Med. 2014;42:965-972. [DOI] [PubMed] [Google Scholar]
- 84. Torg JS, Pollack H, Sweterlitsch P. The effect of competitive pitching on the shoulders and elbows of preadolescent baseball players. Pediatrics. 1972;49:267-272. [PubMed] [Google Scholar]
- 85. Trakis JE, McHugh MP, Caracciolo PA, Busciacco L, Mullaney M, Nicholas SJ. Muscle strength and range of motion in adolescent pitchers with throwing-related pain: implications for injury prevention. Am J Sports Med. 2008;36:2173-2178. [DOI] [PubMed] [Google Scholar]
- 86. Tyler TF, McHugh MP, Mirabella MR, Mullaney MJ, Nicholas SJ. Risk factors for noncontact ankle sprains in high school football players: the role of previous ankle sprains and body mass index. Am J Sports Med. 2006;34:471-475. [DOI] [PubMed] [Google Scholar]
- 87. Valentino M, Quiligotti C, Ruggirello M. Sinding-Larsen-Johansson syndrome: a case report. J Ultrasound. 2012;15:127-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Vandervliet EJ, Vanhoenacker FM, Snoeckx A, Gielen JL, Van Dyck P, Parizel PM. Sports-related acute and chronic avulsion injuries in children and adolescents with special emphasis on tennis. Br J Sports Med. 2007;41:827-831. [DOI] [PMC free article] [PubMed] [Google Scholar]