Abstract
Summary: The clinical studies with intrastriatal transplants of fetal mesencephalic tissue in Parkinson's disease (PD) patients have provided proof-of-principle for the cell replacement strategy in this disorder. The grafted dopaminergic neurons can reinnervate the denervated striatum, restore regulated dopamine (DA) release and movement-related frontal cortical activation, and give rise to significant symptomatic relief. In the most successful cases, patients have been able to withdraw l-dopa treatment after transplantation and resume an independent life. However, there are currently several problems linked to the use of fetal tissue: 1) lack of sufficient amounts of tissue for transplantation in a large number of patients, 2) variability of functional outcome with some patients showing major improvement and others modest if any clinical benefit, and 3) occurrence of troublesome dyskinesias in a significant proportion of patients after transplantation. Thus, neural transplantation is still at an experimental stage in PD. For the development of a clinically useful cell therapy, we need to define better criteria for patient selection and how graft placement should be optimized in each patient. We also need to explore in more detail the importance for functional outcome of the dissection and cellular composition of the graft tissue as well as of immunological mechanisms. Strategies to prevent the development of dyskinesias after grafting have to be developed. Finally, we need to generate large numbers of viable DA neurons in preparations that are standardized and quality controlled. The stem cell technology may provide a virtually unlimited source of DA neurons, but several scientific issues need to be addressed before stem cell-based therapies can be tested in PD patients.
Keywords: Parkinson's disease, transplantation, stem cells, neural grafts, dopamine
INTRODUCTION
Parkinson's disease (PD) is a chronic neurodegenerative disorder characterized by tremor, rigidity, and hypokinesia. The main pathology underlying disease symptoms in PD is a rather selective degeneration of nigrostriatal neurons leading to severe loss of dopamine (DA) in the striatum. The clinical trials with cell therapy in PD patients are based on the idea that restoration of striatal DA transmission by grafted dopaminergic neurons would induce long-lasting clinical improvement, even if the disease is chronic and also affects other brain regions and neuronal systems. In support, a bulk of experimental data from rodents and nonhuman primates have demonstrated that intrastriatally grafted DA neurons, obtained from the fetal ventral mesencephalon, display many of the morphological and functional characteristics of normal DA neurons: they reinnervate the denervated striatum and form synaptic contacts, are spontaneously active and release DA. Successful reinnervation by the grafts is accompanied by significant amelioration of Parkinson-like symptoms in animal models.
Studies with transplantation of human fetal mesencephalic tissue, rich in dopaminergic neurons, to the striatum in PD patients were started in 1987. Since then, clinical cell therapy research in PD has had as its main objectives to explore whether 1) the grafted dopaminergic neurons can survive and form connections in the diseased patient's brain, 2) the patient's brain can integrate and use the grafted neurons, and 3) the grafts can induce measurable clinical improvement. Although the results from these studies seem to provide proof-of-principle for the cell replacement strategy in PD, it is also obvious that further developments are needed if cell-based approaches should become clinically competitive treatments. Major problems with the use of human fetal brain tissue for transplantation purposes are the poor availability and lack of standardization of the cell material, contributing to high variability in the degree of symptomatic relief. Stem cells or their derivatives might be able to solve several of these problems associated with the use of fetal tissue grafts. Stem cells can be defined as immature cells with prolonged self-renewal capacity and, depending on their origin, ability to differentiate into multiple cell types or all cells of the body. From stem cells, it should be possible to produce virtually unlimited numbers of neurons with dopaminergic phenotype in preparations that are standardized and quality controlled.
In this paper, we will review the observations made after transplantation of dopaminergic neurons in PD patients. We will also discuss the scientific advancements that will be needed in experimental and clinical studies for the further development of a cell-based therapy in this disorder. We will argue that a clinically competitive cell replacement therapy for PD will require not only the availability of large numbers of DA neurons, possibly generated from stem cells, but also much better knowledge about which patients should be selected and how the functional outcome should be optimized in each patient's brain.
WHAT HAVE WE LEARNED FROM CLINICAL TRIALS WITH FETAL NEURAL GRAFTS?
Grafts can induce symptomatic relief, but the clinical outcome is variable
An estimated 350 patients with PD have so far received intrastriatal implants of human fetal mesencephalic tissue, rich in postmitotic primary DA neurons. The tissue has been taken from aborted human fetuses, aged 6-9 weeks after conception. Several open-label trials have reported clinical benefit associated with graft survival.1–16 In the most successful cases, patients have been able to withdraw l-dopa treatment during several years after transplantation.10,11,13,17 The magnitude of the overall clinical benefit at 10-24 months postoperatively in three open-label trials11–13 is summarized in Table 1. All patients were grafted bilaterally with tissue from about three to five donors into each putamen. In some cases, tissue was also implanted in the caudate nucleus. According to the unified Parkinson's disease rating scale (UPDRS) motor score during practically defined “off” (i.e., in the morning, at least 12 h after the last dose of antiparkinsonian medication), the overall symptomatic relief at 10-24 months postoperatively was between 30 and 40%. In addition, there was a decrease (by 43–59%) of the average daily time spent in the “off” phase. The mean daily l-dopa requirements were reduced by 16–45%. It is interesting to note that in these three studies, even if the patients showed increased [18F]fluorodopa (FD) uptake in the putamen (by about 60%) using positron emission tomography (PET) indicating graft survival, FD uptake in putamen after transplantation was still only about 50% of the normal mean. This probably explains, at least to some extent, the incomplete functional recovery and indicates that there is room for considerable improvement.
TABLE 1.
Amount of Graft Tissue and Magnitude of Postoperative Changes of Putaminal fluorodopa Uptake and Motor Function in Five Series of Patients with Idiopathic PD at 10–24 Months after Bilateral Intrastriatal Implantation of Human Fetal Mesencephalic Tissue
| Hauser et al., 199912 (n = 6) | Hagell et al., 199911 (n = 4*) | Brundin et al., 200013 (n = 5) | Freed et al., 200118 (n = 19) | Olanow et al., 200323 (n = 11/12)† | |
|---|---|---|---|---|---|
| Number of VM/putamen | 3–4 | 4.9 | 2.8‡ | 2 | 1/4 |
| Fluorodopa uptake (putamen): | |||||
| Preop§ | 34% | 31% | 31% | 39% | n.r.¶ |
| Postop§ | 55% | 52% | 48% | 55% | n.r.¶ |
| Δ | +61% | +69% | +55% | +40% | n.r.¶ |
| UPDRS motor score in “off” (Δ)‖ | −30% | −30% | −40% | −18% | +3.5%/−0.72% |
| Daily time in “off” phase (Δ) | −43% | −59% | −43% | n.r. | +7.8%/−0.9% |
| Daily l-dopa dose (Δ) | −16% | −37% | −45% | n.r. | −20%/−11% |
Exluding one patient with possible multiple system atrophy.
One- and four-donor groups, respectively.
The graft tissue was treated with the lazaroid tirilazad mesylate.
Mean percentage of fluorodopa uptake compared with the normal mean as measured in healthy volunteers.
Only change in uptake from baseline reported.
As assessed during practically defined “off.”
VM = ventral mesencephalon; Δ = mean postoperative change (percentage) from baseline; Preop = preoperatively; Postop = postoperatively; n.r. = not reported.
The first double-blind, sham surgery-controlled study18 demonstrated a more modest clinical response with 18% reduction of UPDRS motor score in “off” at 12 months after bilateral putaminal grafts (Table 1) but no improvement in the sham-operated group. In patients younger than 60 years, the improvement of UPDRS motor score was 34%. These data are important because they provide the first direct evidence of a specific graft-induced improvement, distinguishable from a placebo effect. In this trial, less tissue was implanted as compared to the open-label trials and, in agreement, the increase of FD uptake was lower (only 40% as compared to 60%). In two patients who died after grafting, the number of dopaminergic neurons in each putamen was only between 7,000 and 40,000,18 which was much lower than that found in two patients in one of the open-label trials19–21 (see below). The low cell number probably occurs because tissue from only two donors was implanted in each putamen (compared with tissue from three to five donors in the open-label trials) and that the tissue was stored in cell culture for up to 4 weeks before implantation. Moreover, no immunosuppressive treatment was given. In agreement, the overall postoperative clinical improvement was smaller compared with what was reported in the other patient series. These findings provide further support for the notion that the number of viable implanted DA neurons is an important factor determining the magnitude of symptomatic relief.22
In a second, sham surgery-controlled, double-blind randomized clinical trial,23 solid pieces of human fetal mesencephalic tissue from one or four donors were implanted in each postcommissural putamen. The transplanted patients were compared with a group of patients subjected to sham surgery. Immunosuppressive treatment with cyclosporine was given for 6 months after surgery and patients were followed for 2 years. The trial failed to meet its primary outcome, i.e., change in UPDRS motor scores at 24 months compared with baseline (Table 1). However, in resemblance with the open-label trials, the patients grafted with tissue from four donors showed progressive improvements up to 6 and 9 months after surgery (but deteriorated thereafter). Putaminal FD-PET uptake was significantly increased in grafted patients at 12 months, as compared with controls and nongrafted striatal areas, and remained largely stable at 2 years after transplantation. The poor clinical outcome in this study could, as discussed in detail below, occur because the patients were more severely disabled at the time of transplantation compared with those in the open-label trials, indicating more extensive degenerative changes. Another possibility is that the short-term immunosuppression had been ineffective in preventing the occurrence of delayed immune reactions causing dysfunctional grafts.
When analyzing the modest results of the two sham surgery-controlled clinical trials, it is of course important to ask whether the symptomatic improvements in the open-label studies may have been attributable to placebo effects or observer bias. There are several arguments against such an interpretation: 1) improvements after unilateral grafts have been predominantly contralateral, and in several patients their most parkinsonian side of the body has switched after transplantation; 2) improvements have occurred gradually, starting after about 3 months and continuing up to 1-2 years after grafting; 3) improvements have also been detectable with objective neurophysiological methods measuring arm and hand movements; 4) some patients have improved to the extent that they have been able to return to work and withdraw l-dopa treatment for several years; 5) improvements have been long-lasting, up to 10 years after transplantation; 6) not only improvements, but also deteriorations have been described in open-label trials; and 7) reported changes in motor function broadly correspond to the degree of graft survival and restoration of movement-related frontal cortical activation.
Grafts can reinnervate striatum, release dopamine, and become integrated in patient's brain
Human fetal mesencephalic DA neurons survive transplantation into the brain of PD patients. Significant increases of FD uptake in the grafted striatum have been observed in several studies,1,3,4,6–8,10–16,18,23 and in one patient, uptake was normalized after transplantation.10,17 FD-PET has also demonstrated that the grafts can survive despite an ongoing disease process and continuous antiparkinsonian drug treatment.17 Histopathological analyses have confirmed survival of the dopaminergic grafts and demonstrated their ability to reinnervate the striatum.19–21 In two transplanted patients, between 80,000 and 135,000 dopaminergic neurons had survived on each side, with neurite outgrowth from the grafted neurons extending up to approximately 7 mm within the putamen. Between 24 and 78% of the postcommissural putamen were reinnervated, and electron microscopy revealed synaptic connections between graft and host.
The grafts can also restore regulated release of DA in the striatum. Thus, in one patient who was transplanted unilaterally in the putamen and showed major clinical improvement, FD uptake in the grafted putamen was normal at 10 years postoperatively.17 The uptake in the nongrafted putamen was only about 10% of normal level. Dopamine release, quantified using [11C]raclopride and PET,17 was normal in the grafted putamen both under basal conditions and after amphetamine administration. In contrast, the release in the contralateral, nongrafted putamen was very low. It seems highly likely that the efficient restoration of DA release in large parts of the grafted putamen underlies this patient's major clinical improvement.
Finally, the fetal DA neuron grafts can become functionally integrated into neural circuitries in the PD patient's brain. In the intact brain, substantia nigra DA neurons are important regulators of corticostriatal neurotransmission. Deficient striatal dopaminergic function as a consequence of the loss of substantia nigra neurons in PD leads to an increased threshold for activation of the striatopallidothalamic output pathway. This causes impairment of the movement-related activation of frontal motor cortical areas, which is believed to underlie parkinsonian akinesia.24 Piccini and coworkers25 analyzed movement-related cortical activation, using PET and regional cerebral blood flow measurements, in four PD patients grafted bilaterally in the caudate and putamen. Postoperatively, there was a gradual restoration of the movement-related activation of frontal motor cortical areas that paralleled the time course of clinical improvement. These findings indicate that successful grafts in patients with PD, by improving striatal dopaminergic neurotransmission, can restore movement-related cortical activation, which probably is necessary to induce substantial clinical improvement.
Grafts can give rise to troublesome dyskinesias
The most debated complication from current clinical transplantation protocols for PD is the occurrence of postoperative graft-induced dyskinesias (GIDs).26 Freed et al.18 reported that 15% of their grafted patients developed severe postoperative dyskinesias in the “off” phase. Hagell et al.27 found that 8 of 14 PD patients grafted in Lund displayed postoperative “off”-phase dyskinesias that were mild and caused no distress or disability. In the remaining six patients, dyskinesias were of moderate severity and in one patient constituted a clinical therapeutic problem. In the study of Olanow et al.,23 56.5% of the grafted patients developed postoperative “off”-phase dyskinesias, which consisted of stereotypic, rhythmic movements in the lower extremities. Dyskinesia severity appeared to be generally mild, as judged by mean scores of 3.2 and 2.7 of a possible maximum score of 28 in the one- and four-donor group, respectively (no significant difference between groups), but were disabling and required surgery in three cases.
The one or more mechanisms underlying GIDs are obscure.26 The first attempt to explain GIDs postulated excess DA as a result of continued fiber outgrowth from the grafts.18 However, several lines of evidence speak against this hypothesis. First, there is a lack of correlation between the magnitude of GIDs and that of the antiparkinsonian graft response.23,27 Second, GIDs and antiparkinsonian effect displayed different temporal developments after transplantation.18,23,27 For example, in three bilaterally grafted patients reported by Hagell et al.,27 dyskinesias reached their maximum at 24-48 months after transplantation, whereas the antiparkinsonian response developed during the first 12 months. Third, the occurrence of GIDs has not been associated with high postoperative striatal FD uptake or to the most pronounced graft-induced increases in striatal FD uptake.23,27 When comparing regional putaminal FD uptake in dyskinetic and nondyskinetic grafted patients, Ma et al.28 found evidence of an imbalance between the dopaminergic innervation in the ventral and dorsal putamen in the dyskinetic cases. However, Olanow et al.23 reported no differences in either regional or global levels of striatal FD uptake between patients with and without GIDs. Finally, from a phenomenological point of view, GIDs have differed from l-dopa-induced “on”-phase dyskinesias and instead been reminiscent of biphasic dyskinesias,23,26,28 which could suggest intermediate (not excess) DA levels.
HOW SHALL CELL THERAPY BE DEVELOPED IN PARKINSON′S DISEASE?
Graft efficacy has to be increased and variability reduced
The clinical trials with fetal mesencephalic grafts in PD patients have provided proof-of-principle that cell replacement can restore function in the parkinsonian brain. However, a clinically competitive cell therapy has to provide advantages over current, rather effective treatments for alleviation of motor symptoms in PD patients. Cell-based approaches should give rise to long-lasting, major improvements of mobility and suppression of dyskinesias without the need for further therapeutic interventions. Alternatively, the cells should improve symptoms that are largely resistant to current treatments, such as balance problems and cognitive disturbances. So far, the improvements after intrastriatal transplantation of fetal DA neurons in patients18,23,29 have not exceeded those found with subthalamic deep brain stimulation,30 and there is no convincing evidence that drug-resistant symptoms are reversed by these grafts.29
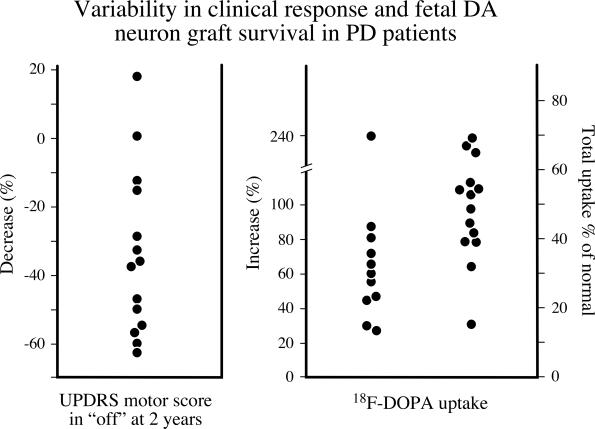
The most important question raised by the clinical transplantation trials performed so far is why the functional outcome has been so variable. This variability is not only seen between different trials and centers, but also within groups of PD patients transplanted at the same center. Among the patients operated in Lund, some have shown major improvement, with 40–60% decrease in UPDRS motor score in “off” at 1-2 years after transplantation, whereas others have exhibited little or no benefit (FIG. 1, left panel). Transplant-induced increases in FD uptake have also been highly variable (FIG. 1, right panel), which suggests that the magnitude of survival and growth of the grafted DA neurons are important factors in determining the functional outcome in patients. The results obtained in the Lund program indicate that good clinical recovery (>30% reduction in UPDRS motor score) is obtained only in patients with at least 40–50% increase in putaminal FD uptake in the grafted putamen. Small transplants, poorly surviving transplants, or poor DA fiber outgrowth (less than about 40% increase in overall FD uptake in the grafted putamen) have generally been associated with limited functional improvement. From the autopsy cases reported by Kordower et al.,20,21 it seems that a good clinical response is associated with survival of at least 100,000 tyrosine hydroxylase (TH)-positive, presumed dopaminergic neurons in the putamen, and reinnervation of about one-third to one-half of the putaminal volume. This level of graft survival and TH-positive fiber outgrowth may correspond to a recovery of putaminal FD uptake to about 50% of normal.
FIG. 1.
Data compiled from 14 of the PD patients operated in Lund, showing the change in UPDRS motor score in individual patients at 2 years after transplantation (expressed as percentage relative to the preoperative value; left panel), and the increase in FD-PET uptake in the putamen at this postoperative time point (right panel). The FD-PET values are expressed both as the increase in percentage of preoperative value (values shown at left), or as the absolute value expressed as percentage of normal age-matched controls.
From available data, it thus seems clear that good graft survival and reinnervation of the denervated striatum, reflected in a marked increase in FD uptake at the graft site, is a necessary prerequisite for a good clinical response. It is equally clear, however, that the magnitude of increase in FD uptake in the grafted putamen does not always match the level of graft-induced functional improvement. This means that even in patients that show a marked increase in FD uptake, the transplantation-induced improvement in motor function, i.e., in UPDRS motor score, is quite variable.
These observations indicate that variability in DA neuron survival and axonal outgrowth alone cannot explain the variable functional outcome, but that other factors are also likely to play an important role. Available experimental and clinical data highlight four such factors, each of which may be critical for determining the functional efficacy of intrastriatal VM grafts. These four factors are as follows: 1) patient selection, i.e., the nature and extent of the pathological processes underlying the parkinsonian symptoms in the individual patient; 2) graft placement, which determines the area(s) of the denervated forebrain that will become reinnervated by the grafted DA neurons; 3) composition of the graft with respect to different subtypes of DA neurons as well as other types of neuronal and non-neuronal elements; and 4) delayed and slowly developing immunological response associated with the immunogenicity of allogeneic transplants in the brain, which may compromise long-term DA neuron survival and function.
Patient selection.
The cell replacement strategy in PD is based on the assumption that restoration of DA neurotransmission in restricted areas of the forebrain is sufficient to reverse, or significantly ameliorate, motor symptoms in patients. Although the degeneration of the nigrostriatal DA neuron system is generally viewed as the common unifying defect in idiopathic PD, it is clear from autopsy studies that clinically diagnosed PD patients display a range of other neuropathological changes that are variable in extent and may involve other brainstem and cortical areas as well. Thus, Lewy bodies and α-synuclein-positive inclusions and dystrophic neurites vary markedly in extent and location from patient to patient.31 Moreover, widespread cortical changes, including amyloid plaques, neurofibrillary tangles, and cell loss, are frequently observed, also in patients without clinically diagnosed dementia.32 This variability is also seen in the extent to which other neurotransmitter systems, such as noradrenergic, serotonergic, and enkephalin-containing neurons, are affected.33
Some of these changes may reflect the progressive nature of the disease, such that areas outside the nigrostriatal system may become more severely involved as the disease progresses. If so, intrastriatal DA neuron transplants would be expected to be more efficacious during early stages of PD, i.e., at stages when the pathological changes are likely to be confined mostly to the nigrostriatal DA system. More extensive degeneration may, at least in part, explain why the overall improvement seen in the Olanow et al.23 trial was so poor. As judged by the doses of antiparkinsonian medication taken by the patients at the time of surgery, these patients are likely to have had overall more advanced disease than, for example, the patients in the Lund program (mean daily l-dopa equivalent dose 1363.3 vs 932.5 mg, respectively). Furthermore, when Olanow and coworkers23 analyzed their less severely disabled patients, they observed a significant improvement difference compared to sham-operated patients at 2 years. Freed et al.18 have reported that transplant-induced recovery was significantly better in younger patients. In the older patient group (>60 years of age), the reduction in UPDRS motor score seen after transplantation was significantly correlated to the magnitude of the response to l-dopa medication as assessed preoperatively.
In experiments in rodents, Sortwell et al.34 have shown that the survival and growth of fetal mesencephalic DA neurons are much reduced (by about 75%) in aged recipients, and that the functional effect of identical transplants is less in older animals. Previous studies have also demonstrated that the DA-denervated striatum exerts a stimulatory effect on the survival and growth of grafted dopaminergic neurons.35–37 Consistent with these in vivo data, Carvey et al.38 observed that the striatum-derived neurotrophic activity, as assessed on DA neurons in culture, is increased after removal of the DA afferents, and that the level declines with age.39 The factor, or factors, involved have so far not been identified, but several growth factors with neurotrophic activity on DA neurons are known to be present in the adult striatum. Two of them, BDNF and GDNF, have indeed been shown to be expressed at increased levels in the DA-denervated striatum. This denervation-induced increase of neurotrophic factor production is significantly reduced in aged animals.40–42 Based on these animal experimental data, it seems likely that the availability of diffusible growth-promoting factors, such as BDNF and GDNF, may play an important role in the regulation of graft survival and function also in PD patients.
Available clinical and experimental data thus point to both age and disease severity as important factors in determining functional efficacy and hence also in explaining the variable outcome of intrastriatal fetal mesencephalic transplants. Moreover, the impact of these two factors may be additive: advancing age is likely to affect, above all, the ability of the denervated striatum to sustain survival and growth of the transplanted DA neurons. Increased disease severity, on the other hand, will affect the ability of the host brain to respond to otherwise fully functional DA neuron grafts. From what we know today, it seems likely that DA neuron transplants will be optimally effective, and hence therapeutically valuable, only in moderately advanced PD patients exhibiting a good and reliable response to l-dopa medication in combination with symptomatology and PET image, which suggest nigrostriatal dysfunction as the leading cause of disability.
Graft placement.
In the clinical trials performed so far, the fetal mesencephalic grafts have—with few exceptions—been placed in the putamen, and in some cases only in the posterior putamen. The outgrowing axons can be estimated to extend 2–3 mm from the site of implantation, which means that the action of the transplanted DA neurons will be limited to a relatively restricted area surrounding each cell deposit. We have previously estimated that about one-third of the grafted putamen will be reached by the graft-derived DA innervation from three to four implantation sites. Remaining parts of the putamen, as well as other striatal areas, are not reinnervated. The reasons for selecting the putamen as the primary transplantation target are that this region exhibits the most marked reductions in DA content, and that it is the part of the striatal complex that is physiologically most closely linked to motor control. However, the loss of DA is quite widespread and also involves other parts of the basal ganglia and limbic forebrain, as well as areas of the cerebral cortex. In most of these regions the mean reductions, as measured biochemically in postmortem brain samples from PD patients, is in the range of 50–90% (see33).
The extent to which DA projections to areas outside the putamen are involved (e.g., caudate nucleus, nucleus accumbens, and frontal cortex) varies from patient to patient and may also be reflected in the severity and range of symptoms exhibited by the individual patient. Based on these considerations, it seems likely that the placement of the dopaminergic transplants has to be tailored to each patient. The way to approach this, we believe, is to perform high-resolution PET scans before surgery to identify the areas, or subregions, where FD uptake is most severely reduced. Such data will be useful not only as a rational basis for selecting optimal transplantation sites for each patient, but they will also help in establishing a correct diagnosis and linking specific symptoms to the pattern of striatal DA dysfunction.
There are animal experimental data in support of this approach. Previous studies, in both rodents and monkeys, have shown that transplants placed in different subregions of the striatal complex will influence different aspects of sensorimotor behavior in the 6-hydroxydopamine (6-OHDA) animal model of PD. Thus, grafts placed in the ventrolateral sector of the striatum in rats, or in the putamen in monkeys, improve paw use and sensorimotor-orienting responses; grafts placed in the dorsocentral part of the striatum in rats, or in the caudate nucleus in monkeys, influence motor asymmetry and posture; and grafts placed in the accumbens area will affect various aspects of locomotor activity in rats.43–46
The striatum and associated limbic and cortical forebrain areas are known to be functionally heterogeneous. As a consequence, the effect of DA denervation on sensorimotor behavior is directly dependent on which area, or areas, are affected.47 Although the nigrostriatal DA system is most severely degenerated in PD, there is clearly a variable involvement of the mesocorticolimbic DA system as well. This raises the question whether grafts limited to the caudate nucleus and putamen are sufficient in all cases. Experiments in rats with 6-OHDA-induced lesions have shown that the magnitude of functional recovery induced by intrastriatal transplants is greater in partially lesioned animals in which the limbic and cortical projections are spared, and that the effect of identical transplants is less in animals with complete lesions of the entire mesotelencephalic DA projection system.36 Thus, the spared portions of the DA projection system innervating nonstriatal areas may be necessary for the intrastriatal grafts to exert their optimal functional effect. The implication of this observation is that patients with more widespread DA neuron cell loss, in which the disease has progressed to also involve nonstriatal areas, may be less suitable candidates for intrastriatal dopaminergic transplants.
Composition and preparation of the graft tissue.
There has so far been no attempt to standardize the way cell transplantation is carried out at different centers. Almost all aspects of tissue procurement and handling vary from one center to another: the dissection of the fetal brain material, the age of the donor fetuses, the length and type of storage after dissection, the way the tissue is dissociated before implantation (into pieces or crude cell suspensions), and the composition of the medium used for storage and/or injection. As a result, the composition of the cell material used for transplantation is likely to vary significantly. In the Freed et al.18 trial, the tissue was cultured for up to 4 weeks before grafting, and in some cases a growth factor cocktail was used. The tissue was implanted as nondissociated solid tissue strands. In the Olanow et al.23 trial, tissue was stored in so-called hibernation medium at 4°C for up to 2 days, and the grafts were implanted as solid pieces. In the Lund program, we have in most cases used nonstored tissue (implanted within about 5–6 h after dissection), and the tissue has been dissociated into a crude cell suspension before injection.
The use of solid grafts is partly justified because it makes it possible to also use tissue from somewhat older aborted fetuses. However, solid tissue grafts are likely to be more immunogenic. Experiments with intracerebral allografts in rodents have shown that the blood capillaries that develop in grafts composed of solid tissue pieces are almost entirely of donor origin and will express high levels of major histocompatibility class I for weeks or months after transplantation, whereas the capillaries in suspension grafts are mostly of host origin.48,49 The disadvantage of using long-term stored or cultured tissue is that its cellular composition is likely to change significantly over time in culture. Cultured fetal mesencephalic DA neurons, moreover, survive less well after transplantation and show more limited fiber outgrowth than freshly dissociated DA neuroblasts.50
One aspect of graft tissue composition that deserves more attention relates to the fact that the ventral mesencephalon contains two distinct DA neuron subtypes: the so-called A9 neurons of the substantia nigra and the A10 neurons of the ventral tegmental area (VTA). Experiments in rodents51,52 suggest that the axons reinnervating the striatum are derived from grafted neurons of the A9 subtype (which is the one normally innervating the caudate nucleus and putamen). The mesencephalic transplants contain a mixture of both subtypes but the fiber outgrowth from the A10 neurons seems to be confined to the graft itself and is thus unlikely to exert any major functional effect. There are good reasons to believe, therefore, that the functional impact of intrastriatal fetal mesencephalic grafts is predominantly mediated by the A9 neuron subtype. Unfortunately, we do not yet have access to any reliable markers that allow us to safely distinguish A9 from A10 neurons. One potentially useful marker is the retinoic acid-generating dehydrogenase enzyme AHD2, which is preferentially expressed by the DA neurons located in the substantia nigra pars compacta. However, because only a subfraction of the nigral DA neurons express this enzyme, it does not provide a sufficiently reliable tool to identify all nigral neurons in the graft.52 It is clear that the relative proportion of A9 and A10 cells in the graft preparations may differ depending on the dissection, preparation, and storage of the tissue before grafting. There are some indications from the work of Isacson and colleagues52,53 that A9 neurons are more vulnerable and that they survive less well after transplantation, at least when taken from somewhat older donors. There is an obvious risk, therefore, that prolonged storage or cell culture may lead to preferential loss of the A9 subtype. This is important to keep in mind when evaluating the outcome of cell transplants in PD patients: the total number of surviving DA neurons in the graft does not tell us how many of these are fully functional A9 neurons with projections extending into the host striatum. Mesencephalic tissue transplanted as solid pieces may be less favorable than cell suspensions in this regard: the number of surviving DA neurons (A9 and A10 combined) required to induce a measurable functional effect in the 6-OHDA PD model (≥50% reduction in amphetamine-induced turning behavior) has been estimated to be about twofold higher in solid grafts as compared to cell suspension grafts.52
Immunological mechanisms.
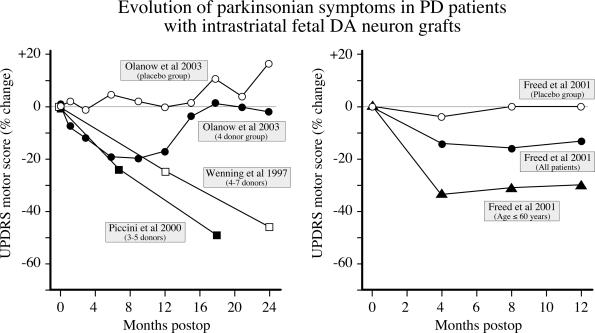
The time course of functional changes in the two sham surgery-controlled studies is clearly different from that observed in the Lund program. In both studies, as illustrated in Figure 2, an initial improvement in UPDRS motor score was observed during the first 4–6 months after transplantation, but was not sustained beyond 6 months. In the Freed et al.18 study, the improvement seen in the younger patient group leveled off at this time point, whereas in the Olanow et al.23 study, the UPDRS scores gradually returned toward preoperative values. In the Lund series,10,25 many of the transplanted patients have shown continued improvement between 6 and 12 months, and in some patients also during the second year after grafting. Interestingly, the magnitude of symptomatic relief seen in the Freed et al.18 and Olanow et al.23 trials over the first 4-6 months matches fairly well the improvement seen in the Lund patients over this time period (FIG. 2). However, although the Lund patients continued to improve over the subsequent 12–18 months, the patients in the Freed and Olanow studies did not.
FIG. 2.
Time course of symptomatic improvement in the patients reported in the Olanow et al.23 study (left panel) and the Freed et al.18 study (right panel), compared with the changes observed in two groups of PD patients transplanted in Lund.10,25 The magnitude of symptomatic improvement seen over the first 4-6 months in the two placebo-controlled studies matches fairly well the improvement seen in the Lund patients over this time period. However, whereas the Lund patients continued to improve over the subsequent 12-18 months, the patients in the Olanow and Freed studies did not. As discussed in the text, this difference may be readily explained by the differences in immunosuppressive treatments used: in the Olanow et al. trial, the immunosuppression was limited to cyclosporine only for the first 6 months, and no immunosuppression at all was used in the Freed at al. trial. The Lund patients were given triple immunosuppressive regimen for at least 12 months.
This major discrepancy in the clinical evolution after transplantation could be explained by the difference in the immunosuppressive treatments used: in the two sham surgery-controlled trials, the immunosuppression was kept at a minimum, i.e., no immunosuppression at all in the Freed et al.18 trial, and only a low-dose cyclosporine regimen in the Olanow et al.23 study. In contrast, a well monitored triple drug immunosuppressive regimen, with high doses initially, was maintained for at least 12 months in the Lund patients. Interestingly, in the Olanow et al.23 trial, the cyclosporine treatment was stopped after 6 months, and the functional improvement ceased to increase soon thereafter. It is conceivable, therefore, that the failure of the transplants to give rise to further clinical benefits in the two sham surgery-controlled trials is caused, at least in part, by the development of a delayed immunological response to the allogeneic graft tissue, the impact of which became apparent during the second half of the year after transplantation.
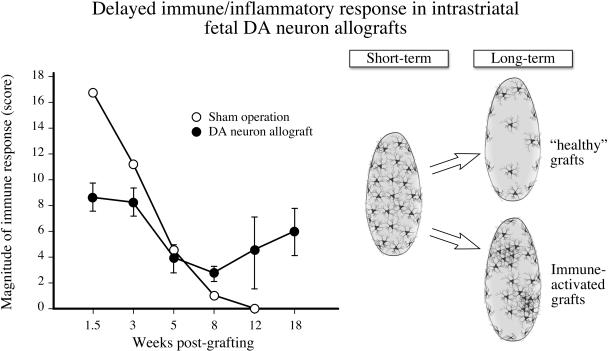
Earlier animal experimental studies have shown that intracerebral allogeneic transplants that differ immunologically on both major and minor histocompatibility antigens will induce an acute inflammatory response, accompanied by an upregulation of both class I and class II antigens in the donor cells. This response subsides over the first 6-8 weeks, but in cases where the recipient animal is immunized against the donor tissue the immune response may rebound, leading to a long-lasting inflammatory response coupled to macrophage and microglial activation at the graft site (FIG. 3). Hudson et al.54 and Shinoda et al.55,56 have shown that this delayed inflammatory response may be detrimental to both survival and function of intrastriatal DA neuron transplants. In such chronic immune-activated transplants, the DA neurons may survive in a compromised state for a long time, with patches of activated microglia–macrophages and increased expression of class II antigens (FIG. 3, immune-activated grafts). Interestingly, this is a picture similar to that observed in the two cases that have come to autopsy in the Olanow et al.23 trial. As pointed out above, solid tissue allografts, as used in this trial, are likely to be more immunogenic because the blood capillaries in such grafts to a large extent are donor-derived and induced to express high levels of donor class I antigens.48,49 For this reason, they may be particularly prone to developing the delayed inflammatory response. The immune reaction against the implanted cells will also depend on the extent of tissue damage or bleeding at the implantation site(s), and it is further enhanced when the transplantation is made in stages, with an interval of several weeks.57 Long-term immunosuppressive treatment is therefore essential to allow the transplanted DA neurons to develop their full functional potential, particularly when the transplantation is performed bilaterally with an interval of several weeks, or multiple needle penetrations are used.
FIG. 3.
Time course of the host immune response to intrastriatal allogeneic grafts, as seen in experiments in nonimmunosuppressed rats. The initial immune response subsides over the first 5-8 weeks but shows a gradual, variable reappearance at 12-18 weeks after grafting. This delayed immune/inflammatory response is observed as a variable activation of host microglia. In immune-activated grafts, there is an increased number of activated microglia, as well as an increased number of major histocompatibility complex class I- and class II-expressing cells (not shown). DA neuron survival is compromised in such immune-activated transplants.56 Data compiled from Shinoda et al.55,56
Techniques for generation of standardized DA neurons in large numbers have to be developed
It is unlikely that transplantation of human fetal mesencephalic tissue will become routine treatment for PD because of problems with tissue availability and standardization of the grafts, leading to much variation in functional outcome. Most probably, fetal mesencephalic grafts will continue to be the golden standard in cell therapy research for PD, and to make more progress it will be necessary to perform additional open-label trials where small groups of patients are operated to explore specific scientific issues. Other sources of cells, such as xenogeneic mesencephalic DA neurons,58 have been considered. However, the clinical trials using intrastriatal transplantation of porcine fetal mesencephalic tissue in patients with PD59,60 have not provided any evidence of graft survival or unequivocal clinical benefits. The main interest is now focused on the production of DA neurons from stem cells in culture and subsequent transplantation.
Stem and progenitor cell technology has the potential to provide virtually unlimited numbers of defined and standardized cells for transplantation in PD patients. Hypothetically, DA neurons could be generated from four different sources of stem cells: embryonic stem cells from the fertilized egg, neural stem cells from the fetal or adult brain, or stem cells in other tissues such as bone marrow. However, the neurons generated from stem cells have to work at least as well as primary DA neurons in fetal mesencephalic grafts. One advantage of stem cells might be the possibility for controlled genetic modification that, hypothetically, could be used to increase survival, migration, and function of their progeny. Based on results obtained with fetal transplants in animals and patients, a set of requirements can be identified that probably have to be fulfilled also by stem cell-derived cells to induce marked clinical improvement: 1) the cells should release DA in a regulated manner and exhibit the molecular, morphological, and electrophysiological properties of substantia nigra neurons53; 2) the cells must be able to reverse motor deficits in animal models resembling the symptoms in patients; 3) the yield of cells should allow for 100,000 or more grafted DA neurons to survive long-term in each human putamen22; 4) the grafted DA neurons should re-establish a dense terminal network throughout large areas of the striatum; and 5) the grafts have to become functionally integrated into host neural circuitries.25
Neurons with a dopaminergic phenotype surviving transplantation in animal models have been generated in culture from mouse and monkey embryonic stem cells and from neural stem or progenitor cells derived from the fetal rodent and human brain.61 Currently, there is little evidence that DA neurons for grafting can be made from adult neural stem cells or from stem cells derived from other tissues. In most cases, it is unclear whether the stem cell-derived cells after transplantation to animal models can substantially reinnervate the striatum, restore DA release, and markedly improve deficits resembling the PD patient's symptoms. The most promising results so far have been obtained using mouse embryonic stem cells.62,63 Large numbers of DA neurons can also be generated when the embryonic stem cells are of human origin, which probably is necessary for a clinical application.
It should be emphasized that, before any clinical application, the risk for teratoma from embryonic stem cells has to be carefully evaluated. Strategies to prevent this serious adverse effect should be developed. Direct implantation of mouse embryonic stem cells into the rat striatum caused teratomas in 20% of the animals,62 but the risk seems to be reduced if the cells are predifferentiated in vitro. Importantly, embryonic stem cells are probably more prone to generating tumors when implanted into the same species from which they were derived.64 Thus, absence of tumors after implantation of human embryonic stem cells or their derivatives in rodents does not exclude their occurrence in the human brain.
Strategies to avoid dyskinesias have to be developed
New animal models in rodents and nonhuman primates are needed to reveal the pathophysiological mechanisms of GIDs.65 Observations in patients and experimental animals suggest several possible mechanisms that may contribute to the development of GIDs.26 One possibility is that failure of the grafts to restore a precise distribution of dopaminergic synaptic contacts on host neurons could result in abnormal gating of corticostriatal inputs, causing abnormal striatal signaling and synaptic plasticity. An alternative possibility, supported by the FD-PET data of Ma et al.,28 is that GIDs might be induced by small grafts that give rise to islands of dopaminergic reinnervation, surrounded by supersensitive, denervated striatal areas. It is also conceivable that the composition of the graft with respect to the types of mesencephalic DA neurons, from substantia nigra or VTA, and the proportion of nondopaminergic neurons or non-neuronal cells may be a contributing factor. As described above, several properties, e.g., firing pattern, transmitter release, and axonal growth capacity, differ between the two types of mesencephalic DA neuron.53 Finally, the occurrence of GIDs may be induced by inflammatory and immune responses around the graft. In this context, it is interesting to note that in the study of Olanow et al.,23 dyskinesias developed after discontinuation of immunosuppressive therapy, with signs of an inflammatory reaction around the grafts in autopsied cases. These various possibilities need to be explored in further detail in animal models.
CONCLUDING REMARKS
During the past two decades, there has been rapid and remarkable advancements in PD cell therapy research. When transplantation of human embryonic mesencephalic tissue into the striatum of PD patients was first performed in 1987, it was unknown whether grafted neurons could at all survive, grow, and function in the 50- to 60-year-old human brain affected by a chronic neurodegenerative disorder. The clinical trials performed since then have provided evidence that the grafted DA neurons can reinnervate the striatum, release DA, become functionally integrated, and induce symptomatic improvement. The effects of transplantation can be long-lasting, up to at least 10 years, and pronounced, allowing for drug withdrawal. Although the degeneration of the patient's own DA neurons continues, no data have suggested that the disease process compromises the survival of the grafts. From a clinical perspective, however, cell therapy is still in a developmental phase and should only be applied to small groups of patients. Current transplantation procedures have not offered groups of patients any clinical benefits that cannot be obtained with other treatments for PD. However, cell therapy has the potential advantage that it can lead to replacement of those particular neurons that have died, restitute functional synaptic DA release at denervated sites in the striatum, and, in the ideal scenario, reconstruct the nigrostriatal system. If we learn how to generate DA neurons in large numbers from stem cells, and how to implant them and guide their growth for efficient repair of the DA system, there is real hope that we in the future can offer patients effective cell-based treatments to restore brain function in PD.
Acknowledgments
Our own research was supported by grants from the Swedish Research Council, the Michael J. Fox Foundation, and the Söderberg Foundation.
REFERENCES
- 1.Lindvall O, Brundin P, Widner H, Rehncrona S, Gustavii B, Frackowiak R et al. Grafts of fetal dopamine neurons survive and improve motor function in Parkinson's disease. Science 247: 574–577, 1990. [DOI] [PubMed] [Google Scholar]
- 2.Lindvall O, Widner H, Rehncrona S, Brundin P, Odin P, Gustavii B et al. Transplantation of fetal dopamine neurons in Parkinson's disease: one-year clinical and neurophysiological observations in two patients with putaminal implants. Ann Neurol 31: 155–165, 1992. [DOI] [PubMed] [Google Scholar]
- 3.Lindvall O, Sawle G, Widner H, Rothwell JC, Bjorklund A, Brooks D et al. Evidence for long-term survival and function of dopaminergic grafts in progressive Parkinson's disease. Ann Neurol 35: 172–180, 1994. [DOI] [PubMed] [Google Scholar]
- 4.Sawle GV, Bloomfield PM, Bjorklund A, Brooks DJ, Brundin P, Leenders, KL et al. Transplantation of fetal dopamine neurons in Parkinson's disease: PET [18F]6-l-fluorodopa studies in two patients with putaminal implants. Ann Neurol 31: 166–173, 1992. [DOI] [PubMed] [Google Scholar]
- 5.Widner H, Tetrud J, Rehncrona S, Snow B, Brundin P, Gustavii B et al. Bilateral fetal mesencephalic grafting in two patients with parkinsonism induced by 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP). N Engl J Med 327: 1556–1563, 1992. [DOI] [PubMed] [Google Scholar]
- 6.Peschanski M, Defer G, N′Guyen JP, Ricolfi F, Monfort JC, Remy P et al. Bilateral motor improvement and alteration of l-dopa effect in two patients with Parkinson's disease following intrastriatal transplantation of foetal ventral mesencephalon. Brain 117: 487–499, 1994. [DOI] [PubMed] [Google Scholar]
- 7.Freeman TB, Olanow CW, Hauser RA, Nauert GM, Smith DA, Borlongan CV et al. Bilateral fetal nigral transplantation into the postcommissural putamen in Parkinson's disease. Ann Neurol 38: 379–388, 1995. [DOI] [PubMed] [Google Scholar]
- 8.Remy P, Samson Y, Hantraye P, Fontaine A, Defer G, Mangin JF et al. Clinical correlates of [18F]fluorodopa uptake in five grafted parkinsonian patients. Ann Neurol 38: 580–588, 1995. [DOI] [PubMed] [Google Scholar]
- 9.Defer GL, Geny C, Ricolfi F, Fenelon G, Monfort JC, Remy P et al. Long-term outcome of unilaterally transplanted parkinsonian patients. I. Clinical approach. Brain 119: 41–50, 1996. [DOI] [PubMed] [Google Scholar]
- 10.Wenning GK, Odin P, Morrish P, Rehncrona S, Widner H, Brundin P et al. Short- and long-term survival and function of unilateral intrastriatal dopaminergic grafts in Parkinson's disease. Ann Neurol 42: 95–107, 1997. [DOI] [PubMed] [Google Scholar]
- 11.Hagell P, Schrag A, Piccini P, Jahanshahi M, Brown R, Rehncrona S et al. Sequential bilateral transplantation in Parkinson's disease: effects of the second graft. Brain 122: 1121–1132, 1999. [DOI] [PubMed] [Google Scholar]
- 12.Hauser RA, Freeman TB, Snow BJ, Nauert M, Gauger L, Kordower JH et al. Long-term evaluation of bilateral fetal nigral transplantation in Parkinson disease. Arch Neurol 56: 179–187, 1999. [DOI] [PubMed] [Google Scholar]
- 13.Brundin P, Pogarell O, Hagell P, Piccini P, Widner H, Schrag A et al. Bilateral caudate and putamen grafts of embryonic mesencephalic tissue treated with lazaroids in Parkinson's disease. Brain 123: 1380–1390, 2000. [DOI] [PubMed] [Google Scholar]
- 14.Mendez I, Dagher A, Hong M, Hebb A, Gaudet P, Law A et al. Enhancement of survival of stored dopaminergic cells and promotion of graft survival by exposure of human fetal nigral tissue to glial cell line-derived neurotrophic factor in patients with Parkinson's disease. Report of two cases and technical considerations. J Neurosurg 92: 863–869, 2000. [DOI] [PubMed] [Google Scholar]
- 15.Mendez I, Dagher A, Hong M, Gaudet P, Weerasinghe S, McAlister V et al. Simultaneous intrastriatal and intranigral fetal dopaminergic grafts in patients with Parkinson disease: a pilot study. Report of three cases. J Neurosurg 96: 589–596, 2002. [DOI] [PubMed] [Google Scholar]
- 16.Cochen V, Ribeiro MJ, Nguyen JP, Gurruchaga JM, Villafane G, Loc'h C et al. Transplantation in Parkinson's disease: PET changes correlate with the amount of grafted tissue. Mov Disord 18: 928–932, 2003. [DOI] [PubMed] [Google Scholar]
- 17.Piccini P, Brooks DJ, Bjorklund A, Gunn RN, Grasby PM, Rimoldi O et al. Dopamine release from nigral transplants visualized in vivo in a Parkinson's patient. Nat Neurosci 2: 1137–1140, 1999. [DOI] [PubMed] [Google Scholar]
- 18.Freed CR, Greene PE, Breeze RE, Tsai WY, DuMouchel W, Kao R et al. Transplantation of embryonic dopamine neurons for severe Parkinson's disease. N Engl J Med 344: 710–719, 2001. [DOI] [PubMed] [Google Scholar]
- 19.Kordower JH, Freeman TB, Chen EY, Mufson EJ, Sanberg PR, Hauser RA et al. Fetal nigral grafts survive and mediate clinical benefit in a patient with Parkinson's disease. Mov Disord 13: 383–393, 1998. [DOI] [PubMed] [Google Scholar]
- 20.Kordower JH, Freeman TB, Snow BJ, Vingerhoets FJ, Mufson EJ, Sanberg PR et al. Neuropathological evidence of graft survival and striatal reinnervation after the transplantation of fetal mesencephalic tissue in a patient with Parkinson's disease. N Engl J Med 332: 1118–1124, 1995. [DOI] [PubMed] [Google Scholar]
- 21.Kordower JH, Rosenstein JM, Collier TJ, Burke MA, Chen EY, Li JM et al. Functional fetal nigral grafts in a patient with Parkinson's disease: chemoanatomic, ultrastructural, and metabolic studies. J Comp Neurol 370: 203–230, 1996. [DOI] [PubMed] [Google Scholar]
- 22.Hagell P, Brundin P. Cell survival and clinical outcome following intrastriatal transplantation in Parkinson disease. J Neuropathol Exp Neurol 60: 741–752, 2001. [DOI] [PubMed] [Google Scholar]
- 23.Olanow CW, Goetz CG, Kordower JH, Stoessl AJ, Sossi V, Brin MF et al. A double-blind controlled trial of bilateral fetal nigral transplantation in Parkinson's disease. Ann Neurol 54: 403–414, 2003. [DOI] [PubMed] [Google Scholar]
- 24.Playford ED, Jenkins IH, Passingham RE, Nutt J, Frackowiak RS, Brooks DJ. Impaired mesial frontal and putamen activation in Parkinson's disease: a positron emission tomography study. Ann Neurol 32: 151–161, 1992. [DOI] [PubMed] [Google Scholar]
- 25.Piccini P, Lindvall O, Bjorklund A, Brundin P, Hagell P, Ceravolo R et al. Delayed recovery of movement-related cortical function in Parkinson's disease after striatal dopaminergic grafts. Ann Neurol 48: 689–695, 2000. [PubMed] [Google Scholar]
- 26.Cenci MA, Hagell P. Dyskinesias and neural grafting in Parkinson's disease. In: Restorative therapies in Parkinson's disease (Olanow CW, Brundin P, eds). New York: Kluwer Academic/Plenum Publishers (in press).
- 27.Hagell P, Piccini P, Bjorklund A, Brundin P, Rehncrona S, Widner H et al. Dyskinesias following neural transplantation in Parkinson's disease. Nat Neurosci 5: 627–628, 2002. [DOI] [PubMed] [Google Scholar]
- 28.Ma Y, Feigin A, Dhawan V, Fukuda M, Shi Q, Greene P et al. Dyskinesia after fetal cell transplantation for parkinsonism: a PET study. Ann Neurol 52: 628–634, 2002. [DOI] [PubMed] [Google Scholar]
- 29.Lindvall O, Hagell P.Clinical observations after neural transplantation in Parkinson's disease. Prog Brain Res 127: 299–320, 2000. [DOI] [PubMed] [Google Scholar]
- 30.Vitek JL.Deep brain stimulation for Parkinson's disease. A critical re-evaluation of STN versus GPi DBS. Stereotact Funct Neurosurg 78: 119–131, 2002. [DOI] [PubMed] [Google Scholar]
- 31.Braak H, Braak E. Pathoanatomy of Parkinson's disease. J Neurol 247 [Suppl 2]: II3–II10, 2000. [DOI] [PubMed] [Google Scholar]
- 32.Perl DP, Olanow CW, Calne D. Alzheimer's disease and Parkinson's disease: distinct entities or extremes of a spectrum of neurodegeneration? Ann Neurol 44: S19–S31, 1998. [DOI] [PubMed] [Google Scholar]
- 33.Agid Y, Javoy-Agid F, Ruberg M. Biochemistry of neurotransmitter in PD. In: Movement disorders 2 (Marsden CD, Fahn S, eds), pp 166-230. London: Butterworth, 1987.
- 34.Sortwell CE, Camargo MD, Pitzer MR, Gyawali S, Collier TJ. Diminished survival of mesencephalic dopamine neurons grafted into aged hosts occurs during the immediate postgrafting interval. Exp Neurol 169: 23–29, 2001. [DOI] [PubMed] [Google Scholar]
- 35.Doucet G, Brundin P, Descarries L, Bjorklund A. Effect of prior dopamine denervation on survival and fiber outgrowth from intrastriatal fetal mesencephalic grafts. Eur J Neurosci 2: 279–290, 1990. [DOI] [PubMed] [Google Scholar]
- 36.Kirik D, Winkler C, Bjorklund A. Growth and functional efficacy of intrastriatal nigral transplants depend on the extent of nigrostriatal degeneration. J Neurosci 21: 2889–2896, 2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yurek DM, Fletcher-Turner A. Temporal changes in the neurotrophic environment of the denervated striatum as determined by the survival and outgrowth of grafted fetal dopamine neurons. Brain Res 931: 126–134, 2002. [DOI] [PubMed] [Google Scholar]
- 38.Carvey PM, Lin DH, Faselis CJ, Notermann JK, Ling ZD. Loss of striatal DA innervation increases striatal trophic activity directed at DA neurons in culture. Exp Neurol 140: 184–197, 1996. [DOI] [PubMed] [Google Scholar]
- 39.Ling ZD, Collier TJ, Sortwell CE, Lipton JW, Vu TQ, Robie HC et al. Striatal trophic activity is reduced in the aged rat brain. Brain Res 856: 301–309, 2000. [DOI] [PubMed] [Google Scholar]
- 40.Yurek DM, Fletcher-Turner A. Lesion-induced increase of BDNF is greater in the striatum of young versus old rat brain. Exp Neurol 161: 392–396, 2000. [DOI] [PubMed] [Google Scholar]
- 41.Zhou J, Pliego-Rivero B, Bradford HF, Stern GM. The BDNF content of postnatal and adult rat brain: the effects of 6-hydroxydopamine lesions in adult brain. Dev Brain Res 97: 297–303, 1996. [DOI] [PubMed] [Google Scholar]
- 42.Yurek DM, Fletcher-Turner A. Differential expression of GDNF, BDNF, and NT-3 in the aging nigrostriatal system following a neurotoxic lesion. Brain Res 891: 228–235, 2001. [DOI] [PubMed] [Google Scholar]
- 43.Björklund A, Stenevi U, Schmidt RH, Dunnett SB, Gage FH. Intracerebral grafting of neuronal cell suspensions. Acta Physiol Scand Suppl 522: 1–48, 1983. [PubMed] [Google Scholar]
- 44.Dunnett SB, Whishaw IQ, Rogers DC, Jones GH. Dopamine-rich grafts ameliorate whole body motor asymmetry and sensory neglect but not independent limb use in rats with 6-hydroxydopamine lesions. Brain Res 415: 63–78, 1987. [DOI] [PubMed] [Google Scholar]
- 45.Mandel RJ, Brundin P, Bjorklund A. The importance of graft placement and task complexity for transplant-induced recovery of simple and complex sensorimotor deficits in dopamine denervated rats. Eur J Neurosci 2: 888–894, 1990. [DOI] [PubMed] [Google Scholar]
- 46.Annett LE, Torres EM, Ridley RM, Baker HF, Dunnett SB. A comparison of the behavioural effects of embryonic nigral grafts in the caudate nucleus and in the putamen of marmosets with unilateral 6-OHDA lesions. Exp Brain Res 103: 355–371, 1995. [DOI] [PubMed] [Google Scholar]
- 47.Dunnett SB, Robbins TW. The functional role of mesotelencephalic dopamine systems. Biol Rev Camb Philos Soc 67: 491–518, 1992. [DOI] [PubMed] [Google Scholar]
- 48.Sloan DJ, Baker BJ, Puklavec M, Charlton HM. The effect of site of transplantation and histocompatibility differences on the survival of neural tissue transplanted to the CNS of defined inbred rat strains. Prog Brain Res 82: 141–152, 1990. [DOI] [PubMed] [Google Scholar]
- 49.Baker-Cairns BJ, Sloan DJ, Broadwell RD, Puklavec M, Charlton HM. Contributions of donor and host blood vessels in CNS allografts. Exp Neurol 142: 36–46, 1996. [DOI] [PubMed] [Google Scholar]
- 50.Brundin P, Barbin G, Strecker RE, Isacson O, Prochiantz A, Bjorklund A. Survival and function of dissociated rat dopamine neurones grafted at different developmental stages or after being cultured in vitro. Brain Res 467: 233–243, 1988. [DOI] [PubMed] [Google Scholar]
- 51.Schultzberg M, Dunnett SB, Bjorklund A, Stenevi U, Hokfelt T, Dockray GJ et al. Dopamine and cholecystokinin immunoreactive neurons in mesencephalic grafts reinnervating the neostriatum: evidence for selective growth regulation. Neuroscience 12: 17–32, 1984. [DOI] [PubMed] [Google Scholar]
- 52.Haque NS, LeBlanc CJ, Isacson O. Differential dissection of the rat E16 ventral mesencephalon and survival and reinnervation of the 6-OHDA-lesioned striatum by a subset of aldehyde dehydrogenase-positive TH neurons. Cell Transplant 6: 239–248, 1997. [DOI] [PubMed] [Google Scholar]
- 53.Isacson O, Björklund LM, Schumacher JM. Toward full restoration of synaptic and terminal function of the dopaminergic system in Parkinson's disease by stem cells. Ann Neurol 53: S135–S146, 2003. [DOI] [PubMed] [Google Scholar]
- 54.Hudson JL, Hoffman A, Stromberg I, Hoffer BJ, Moorhead JW. Allogeneic grafts of fetal dopamine neurons: behavioral indices of immunological interactions. Neurosci Lett 171: 32–36, 1994. [DOI] [PubMed] [Google Scholar]
- 55.Shinoda M, Hudson JL, Stromberg I, Hoffer BJ, Moorhead JW, Olson L. Allogeneic grafts of fetal dopamine neurons: immunological reactions following active and adoptive immunizations. Brain Res 680: 180–195, 1995. [DOI] [PubMed] [Google Scholar]
- 56.Shinoda M, Hudson JL, Stromberg I, Hoffer BJ, Moorhead JW, Olson L. Microglial cell responses to fetal ventral mesencephalic tissue grafting and to active and adoptive immunizations. Exp Neurol 141: 173–180, 1996. [DOI] [PubMed] [Google Scholar]
- 57.Duan WM, Widner H, Bjorklund A, Brundin P. Sequential intrastriatal grafting of allogeneic embryonic dopamine-rich neuronal tissue in adult rats: will the second graft be rejected? Neuroscience 57: 261–274, 1993. [DOI] [PubMed] [Google Scholar]
- 58.Barker RA. Repairing the brain in Parkinson's disease: where next? Mov Disord 17: 233–241, 2002. [DOI] [PubMed] [Google Scholar]
- 59.Schumacher JM, Ellias SA, Palmer EP, Kott HS, Dinsmore J, Dempsey PK et al. Transplantation of embryonic porcine mesencephalic tissue in patients with PD. Neurology 54: 1042–1050, 2000. [DOI] [PubMed] [Google Scholar]
- 60.Watts RL, Freeman TB, Hauser RA, Bakay RA, Ellias SA, Stoessl AJ et al. A double-blind, randomized, controlled, multicenter clinical trial of the safety and efficacy of stereotaxic intrastriatal implantation of fetal porcine ventral mesencephalic tissue (Neurocell™-PD) vs imitation surgery in patients with Parkinson's disease (PD). Parkinsonism Relat Disord 7[Suppl]: S87, 2001. [Google Scholar]
- 61.Lindvall O, Kokaia Z, Martinez-Serrano A. Stem cell therapy for human neurodegenerative disorders—how to make it work. Nat Med 10[Suppl]: S42–S50, 2004. [DOI] [PubMed] [Google Scholar]
- 62.Björklund LM, Sanchez-Pernaute R, Chung S, Andersson T, Chen IY, McNaught KS et al. Embryonic stem cells develop into functional dopaminergic neurons after transplantation in a Parkinson rat model. Proc Natl Acad Sci USA 99: 2344–2349, 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kim JH, Auerbach JM, Rodriguez-Gomez JA, Velasco I, Gavin D, Lumelsky N et al. Dopamine neurons derived from embryonic stem cells function in an animal model of Parkinson's disease. Nature 418: 50–56, 2002. [DOI] [PubMed] [Google Scholar]
- 64.Erdo F, Buhrle C, Blunk J, Hoehn M, Xia Y, Fleischmann B et al. Host-dependent tumorigenesis of embryonic stem cell transplantation in experimental stroke. J Cereb Blood Flow Metab 23: 780–785, 2003. [DOI] [PubMed] [Google Scholar]
- 65.Steece-Collier K, Collier TJ, Danielson PD, Kurlan R, Yurek DM, Sladek JR Jr. Embryonic mesencephalic grafts increase levodopa-induced forelimb hyperkinesia in parkinsonian rats. Mov Disord 18: 1442–1454, 2003. [DOI] [PubMed] [Google Scholar]