Abstract
Combination of sedatives such as fentanyl and midazolam during bronchoscopy is recommended by American College of Chest Physician due to its favourable drug profile. It improves patient comfort and tolerance, and is commonly given unless contraindicated. We describe a rare case of fentanyl-induced chest wall rigidity syndrome during a routine bronchoscopy with endobronchial ultrasound guided-transbronchial needle aspiration (EBUS-TBNA) in a 55 year old male presenting with a lung mass and mediastinal lymphadenopathy. This was effectively managed with neuromuscular blockade, intubation and reversal agents including naloxone. This rare complication should be effectively managed by all bronchoscopist as it carries significant mortality and morbidity if not recognised early. We review the literature on the occurrence of fentanyl-induced chest wall rigidity and its predisposing risks factors.
Keywords: Lung cancer, Bronchoscopy, Sedation
1. Case report
A 55 year old Chinese male presented to the respiratory clinic for chronic cough for 3 weeks duration associated with haemoptysis. Prior to presentation, he was treated in the community with oral antibiotics without improvement. He had no known past medical history and but he had a significant 20 pack year smoking history. There were no relevant contact exposure or other symptoms to suggest pulmonary tuberculosis. A chest radiograph showed a large right lower zone mass, concerning for malignancy. A computed tomography (CT) thorax confirmed a right middle lobe mass with multiple necrotic mediastinal lymph nodes and liver metastasis (Fig. 1a). Sputum acid fast bacilli (AFB) smears and tuberculosis polymerase chain reaction (TB PCR) were negative.
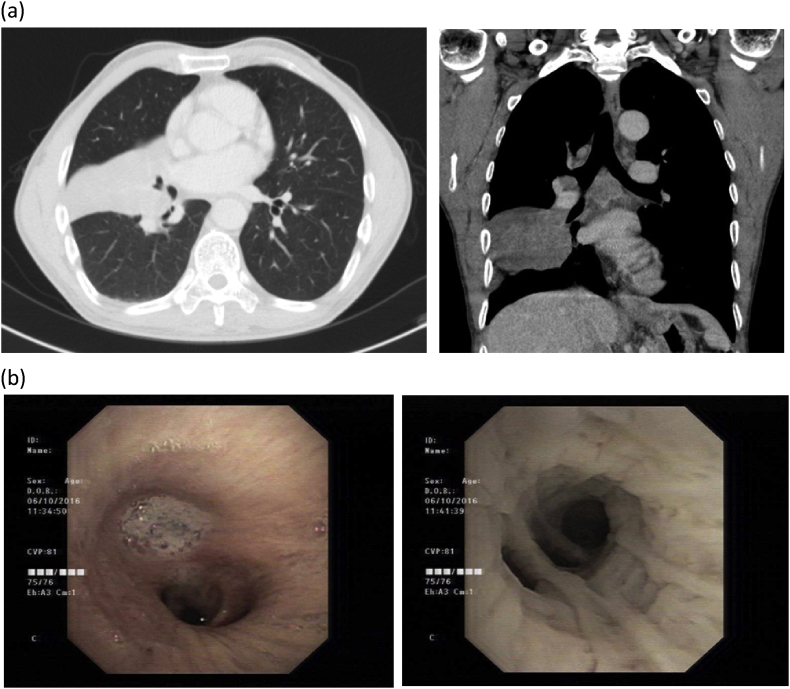
Fig. 1.
(a) Axial and coronal computed tomography (CT) images of the right middle lobe lung mass with sub-carinal lymphadenopathy. (b) Bronchoscopic images of the bronchus intermedius showing mucus secretions in right middle lobe which was suctioned to reveal submucosal tumour infiltration.
A bronchoscopy and endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) of the mediastinal lymph nodes was arranged. Initial pre-procedural examination was unremarkable and he was afebrile with normal vital signs and oxygen saturation of 99% on room air. The patient did not have any pre-procedure risk factors for apnoea such as obstructive sleep apnoea (OSA) or short neck. His BMI was 18.9. Topical xylocaine spray 10% was given intra-orally and intra-nasally. Initial 1 mg of intravenous (IV) midazolam and 25 μg of IV fentanyl was given for moderate sedation with cardiac and pulse oximeter monitoring. A flexible bronchoscope was first introduced for airway inspection. Vocal cords was normal in appearance. Except for submucosal infiltration seen in the right middle lobe, there were no other endobronchial lesions seen (Fig. 1b). During inspection, a further 2 mg of IV midazolam was given to maintain adequate sedation. Bronchoalveolar lavage was performed to the right middle lobe with good returns. The flexible bronchoscope was removed and endobronchial ultrasound bronchoscope was introduced. Surveillance endobronchial ultrasound screen showed enlarged sub-carinal and right para-tracheal lymph nodes. Because the patient became agitated, a further IV midazolam 2 mg and IV fentanyl 25 μg was given, closely titrated to maintain moderate sedation. Successful EBUS-TBNA to sub-carinal lymph node was performed. We then proceeded to biopsy the right para-tracheal lymph node but abandoned because patient turned restless again and required a further IV fentanyl 50 μg. 2 minutes later, patient became unconscious and apnoeic. He was rigid and his chest wall movement ceased During the apnoea phase, he had desaturated leading to sinus bradycardia on the cardiac monitor. Bronchoscope was immediately removed and bag-valve-mask ventilation was attempted but ineffective due to chest wall rigidity. 100 mg IV suxamethonium was given for muscle paralysis to allow for endotracheal intubation and ventilation, followed by naloxone and flumazenil to reverse the effects of fentanyl and midazolam respectively. The time interval between the onset of apnoea and successful endotracheal intubation was 2 min. Airway inspection through the endotracheal tube showed no evidence of airway bleeding. Patient was extubated in the endoscopy room after 10 minutes of observation and wearing off of the effect of neuromuscular blockade (suxamethonium). He was closely observed in the recovery room for the next 6 hours during which he was successfully weaned off oxygen and discharged home on the same day.
2. Discussion
Sedation during bronchoscopy including combination of benzodiazepines and opioids are recommended in the American College of Chest Physicians guidelines, due to their synergistic properties and improved patient tolerance of this common procedure. [1] Fentanyl and midazolam are the recommended sedative and analgesic agents due to their short duration and quick onset of action, and are routinely given to improve patient's tolerance unless contraindicated [1]. In our institution we provide moderate sedation with titrated doses of midazolam and fentanyl to achieve this effect under close cardiac and pulse oximeter monitoring, and this is well tolerated in majority of patients. Risks of moderate sedation are known and may include cardiac instability and respiratory depression.
However, fentanyl induced chest wall rigidity is an uncommon complication, especially during sedation for routine bronchoscopy [2] (See Table 1). It was first described by Hamilton and Cullen in 1953 [3]. It primarily results in chest wall and abdominal wall rigidity, also known as the ‘wooden chest syndrome [4]. The reduced chest wall compliance makes rescue assisted ventilation difficult [4]. This may also be contributed by vocal cords or jaw closure resulting in upper airway obstruction [5].
Table 1.
Summary of reported cases of fentanyl-induced chest wall rigidity.
| Cases | Age | Gender | Comorbidities | Procedure/Clinical setting | Total fentanyl dose | Other sedatives | Management | |
|---|---|---|---|---|---|---|---|---|
| 1 | Vaughn et al., 1981 [11] | 22 years | Female | Nil | Dental extraction | 100 mcg, divided doses | Nil | Naloxone |
| 2 | Ackerman et al., 1990 [6] | 19 years | Female | Nil | Dilation and curettage with pudendal block for incomplete abortion | 100 mcg, divided doses | Midazolam 1 mg | Unable to ventilate with bag and mask, Naloxone |
| 3 | Viscomi et al., 1997 [16] | Unknown | Female | Multiple psychiatric conditions on haloperidol | Vaginal examination for PV bleed during pregnancy | 150 mcg | Nil | Naloxone |
| 4 | Roy et al., 2003 [13] | 41 years | Female | Depression on venlafexine | Laparotomy for total abdominal hysterectomy and bilateral salpingo-oophorectomy under general anaesthesia | 500 mcg, divided doses | Propofol, rocuronium | Naloxone for delayed chest wall rigidity |
| 5 | Lee et al., 2009 [10] | 58 years | Male | Extensive stage small cell lung cancer | Fentanyl patches for pain relief | 250 mcg/hr topical fentanyl patch | Nil | Naloxone, bag and mask ventilation |
| 6 | Prakash et al., 2010 [14] | 9 month | Male | Nil | Repair of omphalocele under general anaesthesia | 12 mcg | Pedicloryl, inhaled halothane | Failed to ventilate with bag and mask. Vecuronium followed by intubation |
| 7 | Eventov-Friedman et al., 2010 [15] | Preterm infant | Female | Nil | Placental transfer of fentanyl in a preterm delivery | Unknown | Nil | Naloxone |
| 8 | Coruh et al., 2013 [2] | 76 years | Male | Non-small cell lung cancer stage 1A post resection | Bronchoscopy with EBUS-TBNA | 150 mcg, divided doses | Midazolam 4 mg | Bag and mask ventilation, Naloxone |
| 9 | Dimitriou et al., 2014 [4] | 79 years | Male | HTN, CAD | Induction of anaesthesia for hernia repair | 100 mcg bolus | Nil | Failed bag and mask ventilation. Propofol, suxamethonium, intubation |
| 10 | Varghese et al., 2015 [17] | 55 years | Male | Dyslipidaemia | Postoperative analgesia for right shoulder arthroscopic synovectomy and biopsy | 20 mcg bolus, followed by 30 mcg/hr | Nil | Cessation of fentanyl infusion, Naloxone |
| 11 | Current case report | 55 years | Male | Nil | Bronchoscopy with EBUS-TBNA | 100 mcg, divided doses | Midazolam 5 mg | Suxamethonium, intubation, Naloxone |
Ref: HTN: hypertension, CAD: coronary artery disease, mg: milligram, mcg: microgram, EBUS: endobronchial ultrasound, TBNA: transbronchial needle aspiration, PV: per vaginal; EBUS-TBNA: Endobronchial ultrasound-Transbronchial needle aspiration.
The mechanisms are unclear but may be centrally mediated through dopaminergic neurons within the basal ganglia and not due to depression of respiratory drive [4], [6]. Fentanyl may also induce muscle rigidity by activating spinal motor neurons through its actions on the pons [4].
Occurrence of fentanyl induced chest wall rigidity is dependent on the dose and rate administered. When IV fentanyl was administered at a rate of 150 mcg/kg/min in healthy human volunteers, rigidity occurred at a dose of 15 mcg/kg and average 3 minutes after peak fentanyl plasma concentrations, which lasted for 11.5 minutes [7]. Others had also reported chest wall rigidity at lower rates of 30–50 mcg/min with doses of 7.3–8 mcg/kg [8], [9]. Chest wall rigidity had also been described in an advance lung cancer patient receiving fentanyl patches [10].
In our patient, chest wall rigidity occurred after a significantly lower dose of 100 μg IV fentanyl (1.6 μg/kg), given in divided doses. The occurrence at relatively low dose is rare with only very few reported cases [3], [4], [6], [11]. This complication is also unusual in the setting of a routine outpatient bronchoscopy. Our patient had also received total 5 mg IV midazolam in divided doses, which could also potentiate the effect of fentanyl [6]. Conversely, others have also reported that midazolam may attenuate the effect of fentanyl-induced chest wall rigidity [12]. Other described risk factors for fentanyl-induced rigidity include extremes of age, critical illnesses and antidepressants which were not present in our patient [12], [13], [17].
Chest wall rigidity can result in serious complications if not recognised early. Rescue bag and mask ventilation may prove ineffective until appropriate pharmacological treatment is given. Management includes reversal of the effects of fentanyl with naloxone. However, as naloxone has a shorter half-life than fentanyl, it is important that patient are observed closely several hours after naloxone has been administered [6]. Short acting neuromuscular blockade and ventilatory support is also effective to attenuate the effect of fentanyl induced chest wall rigidity [2], [6].
In conclusion, we present a rare complication chest wall rigidity following relatively low dose of fentanyl in a routine bronchoscopy, which was effectively managed with naloxone, neuromuscular blockade and ventilation. All bronchoscopists should be able to recognise this complication and provide appropriate management to prevent life threatening respiratory compromise.
References
- 1.Wahidi M.M., Jain P., Jantz M. American College of Chest Physicians consensus statement on the use of topical anesthesia, analgesia, and sedation during flexible bronchoscopy in adult patients. Chest. 2011;140(5):1342–1350. doi: 10.1378/chest.10-3361. [DOI] [PubMed] [Google Scholar]
- 2.Coruh B., Tonelli M.R., Park D.R. Fentanyl-induced chest wall rigidity. Chest. 2013;143(4):1145–1146. doi: 10.1378/chest.12-2131. [DOI] [PubMed] [Google Scholar]
- 3.Hamilton W.K., Cullen S.C. Effect of levallorphan tartrate upon opiate induced respiratory depression. Anesthesiology. 1953;14(6):550–554. doi: 10.1097/00000542-195311000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Dimitriou V., Zogogiannis I., Liotiri D. Impossible mask ventilation after an unusually low dose fentanyl-induced muscle rigidity in a patient with essential tremor: a case report and review of the literature. Middle East J. Anaesthesiol. 2014;22(6):619–622. [PubMed] [Google Scholar]
- 5.Bennett J.A., Abrams J.T., Van Riper D.F. Difficult or impossible ventilation after sufentanil-induced anesthesia is caused primarily by vocal cord closure. Anesthesiology. 1997;87(5):1070–1074. doi: 10.1097/00000542-199711000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Ackerman W.E., Phero J.C., Theodore G.T. Ineffective ventilation during conscious sedation due to chest wall rigidity after intravenous midazolam and fentanyl. Anesth. Prog. 1990;37(1):46–48. [PMC free article] [PubMed] [Google Scholar]
- 7.Streisand J.B., Bailey P.L., LeMaire L. Fentanyl-induced rigidity and unconsciousness in human volunteers. Incidence, duration, and plasma concentrations. Anesthesiology. 1993;78(4):629–634. doi: 10.1097/00000542-199304000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Grell F.L., Koons R.A., Denson J.S. Fentanyl in anesthesia: a report of 500 cases. Anesth. Analg. 1970;49:523–532. [PubMed] [Google Scholar]
- 9.Waller J.L., Hug C.C., Jr., Nagle D.M. Hemodynamic changes during fentanyl–oxygen anesthesia for aortocoronary bypass operation. Anesthesiology. 1981;55(3):212–217. doi: 10.1097/00000542-198109000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Lee K., Kim J., Jin J.Y. 20th Asia Pacific Cancer Conference. 2009. A case of chest wall rigidity syndrome due fentanyl patch in advanced lung cancer patient; p. 149. [Google Scholar]
- 11.Vaughn R.L., Bennett C.R. Fentanyl chest wall rigidity syndrome-a case report. Anesth. Prog. 1981;28(2):50–51. [PMC free article] [PubMed] [Google Scholar]
- 12.Neidhart P., Burgener M.C., Schwieger I. Chest wall rigidity during fentanyl- and midazolam-fentanyl induction: ventilatory and haemodynamic effects. Acta Anaesthesiol. Scand. 1989;33(1):1–5. doi: 10.1111/j.1399-6576.1989.tb02849.x. [DOI] [PubMed] [Google Scholar]
- 13.Roy S., Fortier L.P. Fentanyl-induced rigidity during emergence from general anesthesia potentiated by venlafaxine. Can. J. Anaesth. 2003;50(1):32–35. doi: 10.1007/BF03020183. [DOI] [PubMed] [Google Scholar]
- 14.Prakash S., Mehra V., Gogia A.R. Fentanyl induced rigidity in an infant. J. Anaesthesiol. Clin. Pharmacol. 2010;26(4):567–568. [PMC free article] [PubMed] [Google Scholar]
- 15.Eventov-Friedman S., Rozin I., Shinwell E.S. Case of chest-wall rigidity in a preterm infant caused by prenatal fentanyl administration. J. Perinatol. 2010;30(2):149–150. doi: 10.1038/jp.2009.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Viscomi C.M., Bailey P.L. Opioid-induced rigidity after intravenous fentanyl. Obstet. Gynecol. 1997;89:822–824. doi: 10.1016/s0029-7844(97)81423-8. [DOI] [PubMed] [Google Scholar]
- 17.Varghese D.M., Remanan George M. A case of breathing difficulty following fentanyl infusion for postoperative analgesia in the ICU. Anaesthesiol. 2015;1(6):7–9. [Google Scholar]